Abstract
Background
With the increased prevalence of obesity and sarcopenia, those patients with both visceral obesity and sarcopenia were at higher risk of adverse outcomes.
Aim
The aim of this study was to ascertain the combined impact of visceral obesity and sarcopenia on short-term outcomes in patients undergoing colorectal cancer surgery.
Methods
We conducted a prospective study from July 2014 to February 2017. Patients’ demographic, clinical characteristics, physical performance, and postoperative short-term outcomes were collected. Patients were classified into four groups according to the presence of sarcopenia or visceral obesity. Clinical variables were compared. Univariate and multivariate analyses evaluating the risk factors for postoperative complications were performed.
Results
A total of 376 patients were included; 50.8 and 24.5% of the patients were identified as having “visceral obesity” and “sarcopenia,” respectively. Patients with sarcopenia and visceral obesity had the highest incidence of total, surgical, and medical complications. Patients with sarcopenia or/and visceral obesity all had longer hospital stays and higher hospitalization costs. Age ≥ 65 years, visceral obesity, and sarcopenia were independent risk factors for total complications. Rectal cancer and visceral obesity were independent risk factors for surgical complications. Age ≥ 65 years and sarcopenia were independent risk factors for medical complications. Laparoscopy-assisted operation was a protective factor for total and medical complications.
Conclusion
Patients with both visceral obesity and sarcopenia had a higher complication rate after colorectal cancer surgery. Age ≥ 65 years, visceral obesity, and sarcopenia were independent risk factors for total complications. Laparoscopy-assisted operation was a protective factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Around the world, colorectal cancer is the third most malignant disease and the fourth most common cancer cause of death [1, 2]. More than 1.2 million patients are diagnosed with colorectal cancer and more than 600,000 die from the disease per year [3]. Radical resection is still regarded as the best treatment for curable colorectal cancer. However, the complication rate after surgery ranged from 19 to 30%, although an enhanced recovery after surgery program had been implemented for patients with colorectal cancer [4, 5].
Recently, lots of studies focused on the effect of body composition on the prognosis after surgery, such as body fat and muscle mass. Obesity was reported in epidemiological studies as a risk factor for colorectal cancer [6]. Moreover, obesity was presumed to be a risk factor of postoperative complications in many types of abdominal surgery [7]. Visceral obesity was defined as a large accumulation of visceral adipose tissue, which was regarded as a more reliable factor than BMI as an indicator of obesity in Asians [8,9,10]. In addition, many studies demonstrated that visceral obesity negatively affected the outcomes of surgical treatment and resulted in longer operative time, increased intraoperative blood loss, longer hospital stay, and higher morbidity [11,12,13]. Progressive and generalized loss of skeletal muscle mass and strength, known as sarcopenia [14], was identified as a poor prognostic factor for patients with cancer [15,16,17]. Also, it was reported that sarcopenia was associated with the outcomes after colorectal cancer surgery, including postoperative infectious complication and prolonged hospital stay [18, 19]. Most recently, a large-scale prospective study has investigated the impact of different sarcopenia stages on the postoperative outcomes and showed that severe sarcopenia was an independent risk factor for total postoperative complications [20].
With the increased prevalence of obesity and sarcopenia, those patients with both visceral obesity and sarcopenia seemed to be at higher risk of adverse outcomes. A recent study investigated the effect of visceral obesity and sarcopenia on outcomes following pancreatic cancer surgery, indicated that the combination of visceral obesity and sarcopenia was the best predictor of postoperative death [21]. However, to date, there is a lack of evidence of their impacts on outcomes of colorectal cancer surgery. Moreover, most studies only used skeletal muscle mass to define sarcopenia, without including the functional aspect of sarcopenia. The purpose of this prospective study was to ascertain the combined impact of visceral obesity and sarcopenia on short-term outcomes in patients undergoing colorectal surgery for cancer.
Method
Patient
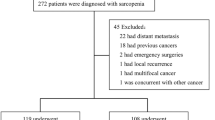
This study was a prospective study. From July 2014 to February 2017, patients who underwent colorectal surgery for cancer at the Gastrointestinal Surgical Department, The First Affiliated Hospital of Wenzhou Medical University, were included. The inclusion criteria included patients who: (1) were ≥ 18 years old; (2) had ASA grade ≤ III; (3) planned to receive elective colorectal surgery for colorectal cancer with curative intent; and (4) had preoperative abdominal computed tomography (CT) scans available for review (no more than 1 month before surgery). Patients were excluded from the study due to (1) undergoing palliative colorectal surgery, emergency surgery; (2) receiving neoadjuvant chemotherapy or radiotherapy; and (3) age less than 18 years. All operations were performed by experienced surgeons who had abundant experience with more than 150 cases of radical colorectal resections for colorectal cancer. Each participant provided written informed consent, and the ethics committee of The First Affiliated Hospital of Wenzhou Medical University approved the protocol for this study.
Data Collection
For each patient, the following parameters were collected: (1) patient characteristics, including age, gender, body mass index (BMI), American Society of Anesthesiology (ASA) grade, hemoglobin concentration (anemia was defined as hemoglobin concentration < 120 g/L in men or < 100 g/L in women), plasma albumin concentration (hypoalbuminemia was defined as a plasma albumin concentration < 35 g/L), comorbidity (calculated by Charlson comorbidity index score) [22], nutritional risk screening 2002 (NRS 2002) scores, history of previous abdominal surgery, total abdominal muscle area (TAMA), visceral fat area (VFA), L3 skeletal muscle index (L3 SMI), tumor location, and TNM stage; (2) operative details, including epidural anesthesia, laparoscopy-assisted operation, combined resection, and surgical duration; and (3) postoperative short-term outcomes, including postoperative complications within 30 days after surgery, postoperative hospital stays, hospitalization costs, and readmissions within 30 days of discharge. Total postoperative complications were defined as those meeting the criterion of grade II or higher according to the Clavien–Dindo classification [23].
Measurement of Muscle Strength and Physical Performance
Preoperative handgrip strength and 6-m usual gait speed were measured as muscle strength and physical performance, respectively, according to the Asian Working Group for Sarcopenia [24]. Once hospitalized, patients were first asked to grip the electronic hand dynamometer (EH101; CAMRY, Guangdong Province, China), using the dominant hand with all of their strength. After that, patients were asked to walk over a 6-m course at their usual speed. Timing was started with the first footfall and stopped when the patient’s first foot completely crossed the 6-m end line. The maximum value of three consecutive tests was recorded.
Quantification of VFA and TAMA
Computed tomography (CT) was used to quantify the abdominal muscle area and visceral fat area. Preoperative abdominal CT scan was routinely available for colorectal cancer patients, generally used to assess tumor location and size and to look for abdominal metastases. A cross-sectional CT image at the inferior aspect of the third lumbar vertebra (L3) was selected for estimating VFA and TAMA as described previously [18, 25]. Predefined Hounsfield unit (HU) thresholds were used for specific tissue demarcation. The Hounsfield unit threshold range of − 29 to + 150 was identified as skeletal muscle and − 150 to − 50 as visceral fat. Tissue boundaries were outlined manually as needed. One trained investigator supervised by a senior radiologist, blinded for the patient and surgical characteristics, analyzed CT images to measure VFA and TAMA with a dedicated processing system (version 3.0.11.3 BN17 32 bit; INFINITT Healthcare Co., Ltd). TAMA was normalized for height (m2) and reported as L3 skeletal muscle index (cm2/m2). The VFA/TAMA ratio was calculated for all patients, and the cutoff values of VFA/TAMA ratio were 1.19 for males and 1.74 for females as previously obtained [20].
Definition of Visceral Obesity and Sarcopenia
Sarcopenia is characterized by low muscle mass, plus low muscle strength or low physical performance [14]. Low muscle mass was defined using predetermined sex-specific L3 skeletal muscle index cutoff values obtained from our previous study: < 40.8 cm2/m2 for men and < 34.9 cm2/m2 for women [26]. Patients with handgrip strength < 26 kg for men and < 18 kg for women were defined as having low muscle strength; patients with 6-m usual gait speed < 0.8 m/s were defined as having low physical performance [24]. Visceral obesity was defined as men with a VFA > 130 cm2 and women with a VFA > 90 cm2, according to the cutoff levels of VFA for metabolic syndrome in the Japanese population [27].
Statistical Analysis
Continuous variables were presented as means ± standard deviations (SD) (normally distributed variables) or as medians and interquartile ranges (non-normally distributed variables). Continuous normally distributed data were compared using the analysis of variance test. For continuous, non-normally distributed data, the Mann–Whitney U test and Kruskal–Wallis H test were used. Categorical variables are presented as numbers and percentages, which were compared using Pearson’s Chi-square test or Fisher’s exact test. For the test of potential risk factors associated with the outcomes, univariate analyses with clinically relevant parameters were performed. Variables with a value of P < 0.10 in the univariate analyses were included in the subsequent multivariate (logistic regression or Cox proportional hazards regression) analyses. All of the tests were two-sided and considered statistically significant when P values were less than 0.05. Statistical analyses were performed using the SPSS software for Windows (version 22.0 IBM, Armonk, NY, USA) statistical program.
Result
Grouping
From July 2014 to February 2017, a total of 376 patients met the inclusion criteria and took part in the study. Based on the diagnostic criteria, 92 (24.5%) of patients were identified as having “sarcopenia” and 191 (50.8%) of patients were identified as having “visceral obesity,” whereas 134 (35.6%) of patients were identified as “normal.” The patients were classified into four groups according to the presence or absence of sarcopenia or obesity: 134 patients in the non-sarcopenia and non-visceral obesity group (NN group), 51 patients in the sarcopenia and non-visceral obesity group (SC group), 150 patients in the non-sarcopenia and visceral obesity group (VO group), and 41 patients in the sarcopenia and visceral obesity group (SO group).
Clinicopathologic Characteristics
Patient demographic and clinicopathologic characteristics are summarized in Table 1. Among the four groups, the oldest age (P < 0.001), the most decreased L3 SMI (P < 0.001), and the lowest hemoglobin (P = 0.003) were found in SO group; in addition, female make up the majority of patients in SO group (P < 0.001). Patients in VO group had the highest BMI (P < 0.001) and VFA (P < 0.001). Patients in SC group had the lowest BMI (P < 0.001) and albumin (P < 0.001). There were no significant differences in NRS 2002 scores, previous abdominal surgery, tumor location, TNM stage, laparoscopy-assisted operation, and epidural anesthesia among the four groups.
Short-Term Outcomes
As is shown in Table 2, the incidence of total complications was the highest in SO group (12.7 vs 35.3 vs 32.7 vs 46.3%, respectively, P < 0.001). The incidence of surgical complications was 6.7% in NN group, 17.6% in SC group, 28.0% in VO group, and 31.7% in SO group, with a significant difference among the four groups (P < 0.001). For medical complications, the SO group had the highest rate of 24.4%, while the rate was 6.7% in NN group, 23.5% in SC group, and 7.3% in VO group, with significant difference among the four groups (P < 0.001). Patients with sarcopenia or/and visceral obesity all had longer hospital stays and higher hospitalization costs compared with normal patients. Wound infection was the most common surgical complication. Among the medical complications, pulmonary complications were the most frequent. No case of mortality occurred. Moreover, the four groups did not show a significant difference in the surgical durations and readmission rate.
Results of univariate and multivariate analyses for risk factors of total complications were presented in Table 3. In the present study, age ≥ 65 years [OR 2.044 (1.226–3.409); P = 0.006], visceral obesity [OR 2.594 (1.573–4.277); P < 0.001], and sarcopenia [OR 1.822 (1.1–3.020); P = 0.012] were independent risk factors for total complications. As for surgical complications, rectal cancer [OR 1.905 (1.118–3.246); P = 0.018] and visceral obesity [OR 3.837 (2.141–6.874); P < 0.001] were independent risk factors for surgical complications (Table 4). In terms of medical complications, age ≥ 65 years [OR 2.708 (1.214–6.039); P = 0.015] and sarcopenia [OR 3.220 (1.608–6.448); P = 0.001] were independent risk factors for medical complications (Table 5). Laparoscopy-assisted operation was a protective factor for total [OR 0.431 (0.255–0.730); P = 0.002] and medical complications [OR 0.187 (0.070–0.496); P = 0.001] (Tables 3, 5).
Discussion
In the current study, we prospectively investigate the impact of visceral obesity and sarcopenia on short-term outcomes for patients undergoing colorectal cancer surgery. It revealed that patients with both visceral obesity and sarcopenia had higher incidence of total, surgical, and medical complications, longer hospital stays, and higher hospitalization costs. Age ≥ 65 years, visceral obesity, and sarcopenia were independent risk factors for total complications. For surgical complications, rectal cancer and visceral obesity were independent risk factors. For medical complications, age ≥ 65 years and sarcopenia were independent risk factors. Laparoscopy-assisted operation was a protective factor for total and medical complications. To our knowledge, this is the first study to distinguish the combined influence of visceral obesity and sarcopenia on patients undergoing colorectal cancer surgery.
The data of present study showed the prevalence of visceral obesity was 50.8%, while the previous studies reported this data ranging from 20.4 to 62.6% [8, 11]. The prevalence of sarcopenia in this study was 24.5%, which was comparable to that previously reported [26, 28]. In addition, the prevalence of both visceral obesity and sarcopenia was 10.9%. It may be due to the heterogeneity in study population. This study firstly presented the data of visceral obesity based on the China population. It is interesting to find that there is the highest proportion of females in SO group. We performed a subgroup analysis of postoperative complications based on gender and found the results were consistent with the above-mentioned results. In our study, there were 32 patients (8.5%) diagnosed with obesity according to World Health Organization (WHO) Asian BMI cut points [29]. In the present study, BMI was not correlated with postoperative complications but visceral obesity was. Therefore, BMI does not always reflect the degree of obesity in the visceral cavity because the intra-abdominal fat distribution was individually different, as indicated previously [30].
Many trials had demonstrated that visceral obesity was associated with longer postoperative hospital stays, higher morbidity, and longer operative time. Furthermore, visceral obesity can independently predicted the incidence of overall postoperative complications after elective colorectal surgery [9, 12, 31]. Sarcopenia could impair the ability of daily living, lose independence, and lead to disabilities or a higher risk of death [14]. Also, sarcopenia was proved to be linked with postoperative infections and longer hospital stay and was one of the independent risk factors for complications after surgery for colorectal cancer [18, 19]. A recent study indicated that combination of visceral obesity and sarcopenia was the best predictor of postoperative death after pancreaticoduodenectomy for cancer [21]. For laparoscopic total gastrectomy, the combined state of visceral obesity and sarcopenia was an independent risk factor for the development of surgical site infection [32]. However, these studies only used skeletal muscle mass as the unique parameter to define sarcopenia, without including muscle function and in physical performance. Our previous study had showed that definition of sarcopenia with a functional aspect had a good prediction of postoperative complications [18]. The present study also measured muscle function and physical performance to give a better definition of sarcopenia. Moreover, the data of the combined impact of visceral obesity and sarcopenia on the outcomes of colorectal cancer surgery were limited. This study indicated that the combination of visceral obesity and sarcopenia may have the worst effect on the outcomes in patients undergoing colorectal surgery for cancer and was an indicator of poor prognosis in patients with colorectal cancer.
The result of multivariate analyses showed that both visceral obesity and sarcopenia were risk factors for total complication, while visceral obesity was a risk factor for surgical complication and sarcopenia was a risk factor for medical complication. Surgery in obese patients was generally considered to be difficult due to the presence of excess intra-abdominal fat tissue, while it is correlated with visceral obesity. It is well known that performing colorectal surgery on obese patients requires more careful effort because of the need to manipulate overly bulky mesenteries, obscure surgical views, and difficulties of identifying adequate surgical planes and normal vasculature. Also, the massive and fragile fat tissue can be easily torn, further decreased precision of surgery [33]. In addition, visceral obesity was correlated with insulin resistance, decreased oxygen tension within surgical wounds, prolonged operative times, and increased operative blood loss, resulting in raising the incidence of wound infection [32]. In the present study, result showed that wound infection was the most common surgical complication; patients only with visceral obesity had a higher incidence of surgical complications and consequently had longer hospital stays and higher costs compared with normal patients. Therefore, visceral obesity seemed to be a suitable indicator of surgical complications after colorectal cancer surgery. In terms of sarcopenia, it serves as a reflection of poor nutritional status, which can be associated with an increased postoperative complication rate [34]. In recent years, sarcopenia was demonstrated to be a poor prognostic factor for various cancers and impact clinical outcomes after surgery [35, 36]. Sarcopenia is described as a global phenomenon, resulting in impairment of multiple physiologic parameters resulting in a decreased ability to respond to stressors, especially the status of cancer and surgical strike [19, 37]. In this study, patients only with sarcopenia had a lowest BMI and albumin, which were both common indexes to evaluate nutritional status. Nutritional status is always correlated with the postoperative outcomes. Patients only with sarcopenia also had a higher incidence of medical complications and longer hospital stays and higher costs according to the result of the present study. Thus, sarcopenia was shown to be a strong risk factor for medical complications. However, high VFA/TAMA ratio was not identified as an independent risk factor for total complications, which means VFA/TAMA ratio may not representative for diagnoses of combined state of measurement of both visceral obesity and sarcopenia. Therefore, preoperative measurement of visceral fat and skeletal muscle mass and independent diagnoses for visceral obesity and sarcopenia could be more comprehensive predictions of postoperative complications. Before surgery, surgeons can easily get this information to have a better understanding of patients’ nutritional status and intra-abdominal anatomic conditions, to predict surgical difficulties and outcomes.
The results of the present study strongly suggested that patients should receive preoperative diagnosis and treatment of sarcopenia and visceral obesity in order to improve postoperative complications. A number of studies indicated physical exercise was one of the treatments for sarcopenia [38]. In addition, studies suggested a beneficial effect of physical exercise on abdominal fat accumulation [39]. So exercise therapy can be one of the interventions between cancer diagnosis and definitive surgical treatment. Pre-habilitation, such as preoperative exercise, has been suggested as a method to reduce postoperative complications [40]. Currently, multi-model pre-habilitation including exercise therapy, nutritional supplementation and hematinic optimization before surgery is not widely adopted [41]. Further studies should pay more attention to this issue.
Patients with rectal cancer had a much higher incidence of surgical complications compared to those with colon cancer in this study. On the one side, the total mesorectal excision (TME) surgery has been regarded as the standard operative mode for rectal cancer, which needs sharp dissection from the pelvic structures. On the other side, it could be technically challenging to give operative procedure with narrow pelvic exposure and distortion of “holy plane.” These potential reasons may raise the difficulty of rectal cancer surgery. In addition, laparoscopic surgery for colorectal cancer can be a protective factor for total postoperative complications. However, concerns remained about the safety and feasibility of laparoscopic surgery for rectal cancer. A randomized clinical trial was unable to establish non-inferiority of laparoscopic surgery for T1–T3 rectal tumors compared with open surgery, although the overall quality of laparoscopic surgery was extremely high [42]. Further prospective studies with long-term follow-ups are required to solve this problem.
Age ≥ 65 years was another risk factor for total and medical complications after colorectal cancer surgery. As we know, elderly patients often have a declined reserve capacity and a high incidence of comorbidity. Age was an independent risk factor for postoperative mortality and morbidity [43]. There is a challenge from the increasing proportion of elderly patients diagnosed with colorectal cancer in China. Because of this, a specific perioperative support with individualized treatment plans should be recommended for elderly patients with colorectal cancer.
There were some limitations in this study. First, this was a single-center study. However, the data can be representative as our department is the largest center of colorectal cancer in the south of Zhejiang Province. In addition, this study included only Chinese patients. As the body composition differs from distinct regions, the result of this study may not be applicable to other biogeographic ethnic groups, especially western population. Further multicenter studies are needed to validate the conclusions of this study. Second, long-term outcomes were not reported in this study. A recent study reported that visceral obesity was significantly associated with decreased metastatic lymph node ratio and better overall survival for colorectal cancer [44], so long-term follow-ups are needed in future studies to investigate the relationship between visceral obesity and disease-free survival rate or the loco-regional recurrence rate after surgery for colorectal cancer.
Conclusion
In conclusion, despite these limitations, the present study demonstrated that patients with both visceral obesity and sarcopenia had a higher postoperative complication rate, longer hospital stays and higher hospitalization costs after surgery for colorectal cancer. Moreover, age ≥ 65 years, visceral obesity, and sarcopenia were independent risk factors for total postoperative complications. Rectal cancer and visceral obesity were independent risk factors for surgical complications. Age ≥ 65 years and sarcopenia showed a significant association with medical complications. Laparoscopy-assisted operation was a protective factor. Assessing visceral fat and muscle areas before surgery could provide useful information to surgeon for a better preparation to reduce the risks of operation.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet. 2014;383:1490–1502.
Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2013;56:667–678.
Zhao JH, Sun JX, Huang XZ, et al. Meta-analysis of the laparoscopic versus open colorectal surgery within fast track surgery. Int J Colorectal Dis. 2016;31:613–622.
Ma Y, Yang Y, Wang F, et al. Obesity and risk of colorectal cancer: a systematic review of prospective studies. PLoS ONE. 2013;8:e53916.
Scheidbach H, Benedix F, Hugel O, Kose D, Kockerling F, Lippert H. Laparoscopic approach to colorectal procedures in the obese patient: risk factor or benefit? Obes Surg. 2008;18:66–70.
Kang J, Baek SE, Kim T, et al. Impact of fat obesity on laparoscopic total mesorectal excision: more reliable indicator than body mass index. Int J Colorectal Dis. 2012;27:497–505.
Watanabe J, Tatsumi K, Ota M, et al. The impact of visceral obesity on surgical outcomes of laparoscopic surgery for colon cancer. Int J Colorectal Dis. 2014;29:343–351.
Rickles AS, Iannuzzi JC, Mironov O, et al. Visceral obesity and colorectal cancer: are we missing the boat with BMI? J Gastrointest Surg. 2013;17:133–143. (discussion p 143).
Yamamoto N, Fujii S, Sato T, et al. Impact of body mass index and visceral adiposity on outcomes in colorectal cancer. Asia Pac J Clin Oncol. 2012;8:337–345.
Cakir H, Heus C, van der Ploeg TJ, Houdijk AP. Visceral obesity determined by CT scan and outcomes after colorectal surgery; a systematic review and meta-analysis. Int J Colorectal Dis. 2015;30:875–882.
Balentine CJ, Enriquez J, Fisher W, et al. Intra-abdominal fat predicts survival in pancreatic cancer. J Gastrointest Surg. 2010;14:1832–1837.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–423.
Wang SL, Zhuang CL, Huang DD, et al. Sarcopenia Adversely Impacts Postoperative Clinical Outcomes Following Gastrectomy in Patients with Gastric Cancer: A Prospective Study. Ann Surg Oncol. 2016;23:556–564.
Fukuda Y, Yamamoto K, Hirao M, et al. Sarcopenia is associated with severe postoperative complications in elderly gastric cancer patients undergoing gastrectomy. Gastric Cancer. 2016;19:986–993.
Psutka SP, Carrasco A, Schmit GD, et al. Sarcopenia in patients with bladder cancer undergoing radical cystectomy: impact on cancer-specific and all-cause mortality. Cancer. 2014;120:2910–2918.
Huang DD, Wang SL, Zhuang CL, et al. Sarcopenia, as defined by low muscle mass, strength and physical performance, predicts complications after surgery for colorectal cancer. Colorectal Dis. 2015;17:O256–O264.
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE. Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer. 2012;107:931–936.
Huang DD, Zhou CJ, Wang SL, et al. Impact of different sarcopenia stages on the postoperative outcomes after radical gastrectomy for gastric cancer. Surgery. 2017;161:680–693.
Pecorelli N, Carrara G, De Cobelli F, et al. Effect of sarcopenia and visceral obesity on mortality and pancreatic fistula following pancreatic cancer surgery. Br J Surg. 2016;103:434–442.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196.
Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101.
Malietzis G, Currie AC, Athanasiou T, et al. Influence of body composition profile on outcomes following colorectal cancer surgery. Br J Surg. 2016;103:572–580.
Zhuang CL, Huang DD, Pang WY, et al. Sarcopenia is an Independent Predictor of Severe Postoperative Complications and Long-Term Survival After Radical Gastrectomy for Gastric Cancer: Analysis from a Large-Scale Cohort. Medicine (Baltimore). 2016;95:e3164.
Oka R, Kobayashi J, Yagi K, et al. Reassessment of the cutoff values of waist circumference and visceral fat area for identifying Japanese subjects at risk for the metabolic syndrome. Diabetes Res Clin Pract. 2008;79:474–481.
Peng P, Hyder O, Firoozmand A, et al. Impact of sarcopenia on outcomes following resection of pancreatic adenocarcinoma. J Gastrointest Surg. 2012;16:1478–1486.
Organization WH. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; 2000.
Bouchard C, Despres JP, Mauriege P. Genetic and nongenetic determinants of regional fat distribution. Endocr Rev. 1993;14:72–93.
Tsujinaka S, Konishi F, Kawamura YJ, et al. Visceral obesity predicts surgical outcomes after laparoscopic colectomy for sigmoid colon cancer. Dis Colon Rectum. 2008;51:1757–1765. (discussion 1765-1757).
Nishigori T, Tsunoda S, Okabe H, et al. Impact of Sarcopenic Obesity on Surgical Site Infection after Laparoscopic Total Gastrectomy. Ann Surg Oncol. 2016;23:524–531.
Kim KH, Kim MC, Jung GJ, Kim HH. The impact of obesity on LADG for early gastric cancer. Gastric Cancer. 2006;9:303–307.
Prado CM, Heymsfield SB. Lean tissue imaging: a new era for nutritional assessment and intervention. JPEN J Parenter Enteral Nutr. 2014;38:940–953.
Reisinger KW, van Vugt JL, Tegels JJ, et al. Functional compromise reflected by sarcopenia, frailty, and nutritional depletion predicts adverse postoperative outcome after colorectal cancer surgery. Ann Surg. 2015;261:345–352.
Wagner D, DeMarco MM, Amini N, et al. Role of frailty and sarcopenia in predicting outcomes among patients undergoing gastrointestinal surgery. World J Gastrointest Surg. 2016;8:27–40.
Miyamoto Y, Baba Y, Sakamoto Y, et al. Sarcopenia is a Negative Prognostic Factor After Curative Resection of Colorectal Cancer. Ann Surg Oncol. 2015;22:2663–2668.
Marzetti E, Calvani R, Tosato M, et al. Physical activity and exercise as countermeasures to physical frailty and sarcopenia. Aging Clin Exp Res. 2017;29:35–42.
Riechman SE, Schoen RE, Weissfeld JL, Thaete FL, Kriska AM. Association of physical activity and visceral adipose tissue in older women and men. Obes Res. 2002;10:1065–1073.
Yamamoto K, Nagatsuma Y, Fukuda Y, et al. Effectiveness of a preoperative exercise and nutritional support program for elderly sarcopenic patients with gastric cancer. Gastric Cancer. 2017;20:913–918.
Bolshinsky V, Li MH, Ismail H, Burbury K, Riedel B, Heriot A. Multimodal Prehabilitation Programs as a Bundle of Care in Gastrointestinal Cancer Surgery: A Systematic Review. Dis Colon Rectum. 2018;61:124–138.
Stevenson AR, Solomon MJ, Lumley JW, et al. Effect of Laparoscopic-Assisted Resection vs Open Resection on Pathological Outcomes in Rectal Cancer: The ALaCaRT Randomized Clinical Trial. JAMA. 2015;314:1356–1363.
Tran TB, Worhunsky DJ, Squires MH 3rd, et al. Outcomes of Gastric Cancer Resection in Octogenarians: A Multi-institutional Study of the U.S. Gastric Cancer Collaborative. Ann Surg Oncol. 2015;22:4371–4379.
Park SW, Lee HL, Doo EY, et al. Visceral Obesity Predicts Fewer Lymph Node Metastases and Better Overall Survival in Colon Cancer. J Gastrointest Surg. 2015;19:1513–1521.
Acknowledgments
This study was supported by the clinical nutriology area of the medical support discipline of Zhejiang Province (No. 11-ZC24).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, WZ., Chen, XD., Ma, LL. et al. Impact of Visceral Obesity and Sarcopenia on Short-Term Outcomes After Colorectal Cancer Surgery. Dig Dis Sci 63, 1620–1630 (2018). https://doi.org/10.1007/s10620-018-5019-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5019-2