Abstract
Chronic rejection affects the long-term survival of all solid organ transplants and, among intestinal allografts, occurs in up to 10% of the recipients. The insidious clinical evolution of the chronic allograft enteropathy, the absence of noninvasive biomarkers, and the late endoscopic findings delay its diagnosis. No pharmacological approach has been proven effective, and allograft removal nowadays still represents the only available therapy. The inclusion of the liver in the visceral allograft appears to be the only intervention affecting the development of chronic rejection, as revealed by large-center studies and registry reports. A significant body of evidence emerged from the experimental setting and provided essential knowledge on the complex mechanisms behind the development of chronic allograft enteropathy. More recently, donor-specific antibodies have been suggested as an early, key element in the natural history of chronic allograft enteropathy and several novel approaches, tackling the antibody-mediated graft injury, have gained acceptance in clinical settings and are believed to impact on chronic rejection. The inclusion of a liver allograft is advocated when re-transplanting a sensitized recipient, due to its protective effect against humoral immunity. Multicenter trials are required to understand and tackle chronic rejection, and find the therapeutic answer to this clinical dilemma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rejection (CR) has been recognized as the major cause of late graft loss and reduced late patient survival after intestinal/multivisceral transplantation (ITx), since the early days of the procedure [1,2,3,4]. This phenomenon has been little influenced by the recent immunosuppressive preconditioning protocols [5], and it has been reported in historical reports to affect 10–20% of the intestinal grafts [1,2,3,4]. In spite of its significant impact on the results, this clinical entity is poorly understood, difficult to diagnose, and lacking definitive treatment options. In brief, CR is represented by an enteropathy with an insidious, progressive course lacking early, specific clinical symptoms or mucosal findings at endoscopy.
Diagnosing CR has practical implications as there is an ongoing debate among transplant centers on “whether and when” to perform graft enterectomy in case of irreversible chronic allograft enteropathy (prior or during re-transplantation) [6]. The diagnosis of CR is usually confirmed only in full-thickness biopsies after explanting the failed grafts, which is a radical and often dramatic decision [4, 7]. Hence, reviewing the existing experimental data as well as the available clinical reports may increase our understanding on the etiology of CR, its mechanisms and the opportunities for clinical intervention.
Magnitude of the Problem and Its Clinical Significance
In the largest series of intestinal transplantation published to date, CR has been found as the most important single cause of graft loss among the 245 patients who lost their grafts (30% of all cases) surpassing infections (22%) or the technical complications (8%) [8]. In this cohort of 500 transplants performed in Pittsburgh in both adults and children over a period of 25 years, 15% of the patients developed clinically manifest CR, with the recipients of isolated intestinal grafts running the highest risk. It has to be noted that this unique experience is spanned over several different “immunosuppression eras” which may have influenced significantly both short- and long-term outcome including CR. In a sub-analysis from the same center, performed in 210 pediatric patients, CR has been found as the largest single cause of graft loss after the second year with an overall incidence in excess of 10%. The occurrence of CR in pediatric patients receiving r-ATG induction was found fivefold more common when the intestinal allograft had been transplanted without the liver (8/38 = 21.05% vs. 2/65 = 4.6%, p = 0.017) [9]. In a series of over 300 intestinal transplants from the University of Miami, acute rejection was the leading cause of graft loss (46.8%), whereas chronic rejection accounted for 8 (17%) out of the 47 losses of primary grafts [10].
Newer, medium-sized transplant programs report similar results. In the Italian experience among adult patients, five recipients (10%) of isolated intestinal graft out of 49 patients of intestinal or multivisceral allografts developed CR [11]. Similarly, an Argentinean report indicated that three out of their 42 ITx (7%) were lost for CR [12]. On the other hand, a recent, large single-center report from Indianapolis on 221 intestinal allografts recipients transplanted between 2003 and 2014 reported only 8 enterectomies for CR, thus resulting in a much lower incidence of CR (3,6%) [6]. In brief, most clinical series report an incidence of CR between 5 and 10%. However, given the difficulty in diagnosing CR early and accurately, some cases may have been underdiagnosed (see Table 1).
Diagnostic Criteria
In spite of its frequent occurrence and clinical significance, there is a striking lack of early, well-defined, diagnostic criteria to recognize the patients developing CAE. A recent consensus workshop in Buenos Aires [13] proposed several clinical criteria as suggestive for CAE. Thus, the presence of abdominal pain, abdominal mass or abdominal distension with chronic diarrhea, bowel obstruction, entero-cutaneous fistulas, intolerance to feeding with recurrent emesis, weight loss, protein-losing enteropathy, failure to thrive, or complications at the site of the ostomy should be regarded as signs of CAE. No reliable biomarkers in the feces or serum markers are available, but the workshop suggested a decrease in citrullin and elevated CRP (C-reactive protein)/LPS (lipopolysaccharide)-binding protein ratio as surrogate markers of concomitant loss of graft mass/function and bacterial translocation, respectively, during CR. CT and MRI scan may be supportive to diagnosis, showing thickening of mesentery and/or intestinal wall and a paucity of mesenteric vessels.
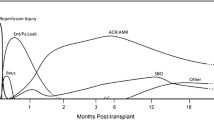
The median time to the diagnosis of CR has been reported to be 39 months with a range of 22–67 months [9]. The frequency increases 2 years after transplantation and reaches a nadir during the third post-transplant year. Endoscopic monitoring may offer some indirect hints: persistent, non-healing, focal mucosal ulcerations often preceded by repeated episodes of ACR (acute cellular rejection) are frequent endoscopic findings in patients with CR [8]. Later, mucosal folds become effaced with pseudomembranes and the bowel appears rigid and fibrotic: Biopsy specimens may show mild ischemic changes, low-grade apoptosis, crypt loss, and very often mild fibrosis of the lamina propria [8].
Frustratingly, mucosal biopsies are often unremarkable, even during overt, refractory intestinal dysfunction. The hallmark of the CR is a patchy, concentric, obstructive vasculopathy of the middle-sized arteries in the submucosa and in the mesentery, but this finding is not sampled on endoscopic biopsies and it has been described on resected specimens or on explanted grafts [4]. In addition to the arteriopathy and the marked intimal hyperplasia, blunting of villi with hyperplastic, branched crypts, and increased fibrosis in the lamina propria have also been reported. The presence of fibrosis in the mucosal biopsies is difficult to interpret as this may be secondary to several causes such as previous episodes of rejection, ischemic injury, prior infections, medication-associated chronic injury or earlier biopsy site [14, 15]—see Fig. 1 (pathologic, endoscopic, and surgical feature of CR).
A case of chronic rejection in a patient receiving an isolated intestinal graft: a graft endoscopy (enteroscopy) showing a mucosa with extensive ulcerations and pseudomembranes, lacking the typical mucosal plications; b the explanted intestinal graft at the time of surgery showing segmental dilatations, adhesions, and sclerosing peritonitis; c the explanted graft indicating a thickened intestinal wall with fibrosis, extensive mucosal ulcerations, and pseudomembranes; d the explanted graft with significant perivascular mesenteric fibrosis; e microphotography revealing absent villi, crypt paucity, and a moderate inflammatory infiltrate (hematoxylin–eosin, magnification ×200—from Liver and Multiorgan Transplant Center in Bologna, Italy, reproduced with authorization of main author Lauro A)
Pathology of Chronic Allograft Enteropathy
Given the insidious clinical development and the uncharacteristic mucosal biopsies, the natural history of CAE in humans is poorly known and much of the information stems from chronically rejecting, explanted grafts. However, several animal studies have shown comprehensive, sequential graft assessment at several time points and provided valuable insight into the development of CR.
Most experimental studies assess the grafts after 13 weeks, a time point when CR is considered to be established and the entire spectrum of mucosal, fibrotic, and vascular changes present. In a sequential rodent study spanning over 17 weeks, the earliest change observed was a significant mesenteric inflammation within the first 4 weeks after transplantation, suggesting that the early inflammatory component of chronic rejection began in the mesentery [16]. Loss of goblet cells with the depletion of the Peyer’s patches and the mesenteric lymph nodes are uniformly observed [16,17,18], and other features of chronic rejection, including fibrosis with macrophages in the lamina propria and muscular layer plus arteriosclerosis, were found over the following 5–6 weeks [18]. Increased tissue levels of the inflammatory mediators IL-6, IL-10, and TNF were found after 9 weeks but not after 13 weeks [19]. The changes typically found in the endoscopic mucosal biopsies (flattened and distorted villi, inflamed mucosa, reactive epithelial changes, and fibrosis of the lamina propria between the crypts) occurred only in late, advanced stages [16, 17].
Only a few clinical studies of significant size are available for comparison. In a series of biopsies from 182 human intestinal transplant recipients [20], mucosal fibrosis was observed for the first time after a mean of 7 months post-transplantation and one-third of the intestinal graft recipients had mild or moderate mucosal fibrosis on their graft biopsies 5 years post-transplantation. Although the presence of mucosal fibrosis did not affect patient or graft survival, patients with this kind of lesion were at higher risk of developing chronic allograft enteropathy. Another recent analysis of 26 human small bowel allografts [7], explanted for different causes, found that goblet cell loss and submucosal fibrosis were significantly associated with small bowel explants showing obliterative arteriopathy. The same study inferred that chronic vascular rejection is a common late event in small bowel transplantation where it primarily affects medium-sized and large-sized vessels of the serosa and mesentery.
Pathogenesis of Chronic Rejection: Insights from Experimental and Clinical Observations
The current understanding is that, irrespective of organ, the late graft changes mainly consisting of chronic inflammation and fibrosis and collectively termed “chronic rejection” are induced, maintained and amplified by both the innate and adaptive immunity. However, as with other organs, a main obstacle is the lack of a standardized experimental model reproducing CR identically and the experimental results need to be interpreted cautiously. Different species, strain combinations, and used immunosuppressive protocols thereof render many of the observations only partially relevant but allow glimpses into several of the mechanistic aspects. Fortunately, the clinical evidence grows in parallel with the experimental research and further it contributes to the understanding of this puzzling entity.
While some of the stimuli and mechanisms driving the inflammation may be common to other organs and some may be particular to the intestine, the key question that remains to be answered is if and how these factors can be altered by different therapeutic interventions. For reasons of clarity, the various features developing in the different tissue compartments, and which appear to have different underlying mechanisms and origin, will be discussed separately.
Fibrosis, Arteriopathy, and Mucosal Atrophy
Fibrosis and obliterative arteriopathy are key features during chronic allograft enteropathy. In spite of their preeminence in the tissue, these changes represent late stage of chronic inflammation and share similar mechanisms with the corresponding alterations seen in other types of grafts.
Various types of tissue injury, incurred after transplantation (i.e., ischemia–reperfusion, acute rejection), lead to the breakdown of cell membranes and tissue barriers with the subsequent release of intracellular contents typically hidden from the immune system [21]. Many of these endogenous components are powerful activators of the innate immune system, and the endogenous innate immune activators have been increasingly considered in a variety of experimental models and clinical diseases. The involvement of heat shock proteins (HSPs) and anti-HSP reactivity in the genesis of chronic allograft alterations has been suggested by multiple studies. The immune-dominant nature of HSPs and their immunogenicity has prompted the idea that HSPs might act as autoantigens capable of initiating and perpetuating an inflammatory response. Increased expression of HSP60 and HSP70 has been found during intestinal [22, 23], cardiac [24], or renal acute rejection [25], as well as during chronic rejection of intestinal [26] and cardiac [27] rat allografts. Thus, it might be speculated that an increased or prolonged expression of HSP may promote the expansion of autoreactive, HSP-specific T cell populations and their infiltration into HSP-expressing tissue [27]. This idea is further supported by the finding of HSP-reactive lymphocytes infiltrating renal [25] or cardiac allografts [28]. In addition, experimental evidence indicates the involvement of HSPs in the synthesis and assembly of collagen and in the genesis of interstitial fibrosis. Increases in the synthesis of collagen and HSP47 occurred in a time-dependent fashion during the progression of carbon tetrachloride induced liver fibrosis in rats while, in models of renal fibrosis, synthesis of HSP47 correlated with that of collagen deposition and tissue scarring [29, 30]. Other mechanistic insights, recorded during the tissue remodeling in CR, involve the basic fibroblast growth factor (bFGF) that was found significantly upregulated in failing allografts [31]. The etiology and significance of fibrosis occurring during the intestinal CR remains unclear, but whether it is remodeling and scarring this process will worsen the progressive ischemia driven by the microvascular alterations and will ultimately lead to mucosal atrophy.
The endothelium is the interface between graft and recipient, and it constitutes the first target for the recipient immune response. Damage to the endothelium can be inflicted during leukocyte extravasation into the tissue in the post-reperfusion period, during acute rejection or episodes of enteritis. In addition to the direct and cell-mediated mechanism, the endothelia may be injured through direct donor-specific antibody (DSA), by complement activation, or through DSA-induced recruitment of inflammatory cells [32]. As with other graft types, the involvement of the humoral allo-immunity and circulating donor-specific antibodies (DSA) in the development of the chronic allograft enteropathy has also been recently recognized but the mechanism by which humoral allo-immunity leads to CR is not well understood. The limitations of the animal studies (i.e., experimental design, immunological differences) as well as the location of the principal microvascular changes (outside the reach of endoscopic biopsies) limit drastically the information on the development of the obliterative arteriopathy typical of CAE. Fortunately, new techniques such as the solid phase assay, the growing body of clinical evidence on the DSA role, and the long-term outcome of ITx (as well as data extrapolations from similar settings, particularly kidney transplantation) provide insights on potential causes of late allograft failure and allow for certain mechanistic hypotheses [33,34,35]. The first clinical report on the impact of preformed anti-donor IgG lympho-cytotoxic antibodies on ITx outcome [36] signaled that 23 (18%) of the 124 patients undergoing ITx had preformed anti-donor IgG lympho-cytotoxic antibodies. The authors attributed this relatively high rate of preformed antibodies to the multiple previous abdominal operations and the frequent need for blood transfusions. This study also noted an increased frequency and severity of intestinal acute rejection in ITx patients positive to T cell lympho-cytotoxic crossmatch but no information on long-term outcome was provided. A follow-up study on a larger cohort of 194 adult ITx recipients [33], of which 55 (28%) had a positive crossmatch and 49 (25%) were positive in HLA–DSA, found a relatively high incidence of CR (19%-36 cases) after an average of 21 ± 10 months after transplantation. Overall, the cumulative risk of CR was slightly higher in recipients with a positive crossmatch versus a negative crossmatch. Persistent and de novo HLA–DSA significantly increased the risk of CR and associated graft loss, while the inclusion of the liver was a significant predictor of better outcome. Patients with liver-containing grafts had a higher clearance of the preformed antibodies and lower induction of de novo DSA as well as lower rates of CR.
In contrast with the acute rejection, where graft enterocytes are main, early targets for the recipient immune system (with crypt apoptosis and mucosal sloughing as their microscopic hallmarks), mucosal changes are mild and occur late during CR. Thus, the mucosa seems to be among the last compartments featuring significant changes during the progression of CR. Rat intestines presented crypt hyperplasia and scattered necrotic cells in the crypts, sclerosis between the crypts, loss of goblet cells, and only a slight blunting of the villi [18]. These findings were interpreted as secondary to chronic ischemia and to circumstances evolving in reduced mucosal perfusion, well reflecting the findings in human specimens [4, 15]. Much of this prolonged resistance may be due to the high regenerative capacity of the intestine and due to the hyperplastic crypts, but the hypoxic environment will ultimately cause enterocyte shedding and mucosal sloughing which over time would appear as a villous blunting. It is believed that the intestinal stem cells differentiate and repopulate the epithelium with metaplastic-appearing cells. Concomitantly, the fibroblasts in the mucosa and submucosa respond to the chronic hypoxic environment with increased collagen synthesis leading to fibrosis that will gradually worsen the process and lead to mucosal atrophy and ulcerations. [7]. The dysfunctional epithelium and the scattered ulcerations will then promote bacterial translocation and the protein-losing enteropathy.
The mucosal changes do not seem to be the consequence of a leukocyte-mediated injury as several subsets of villus-infiltrating leukocytes (CD4+, CD8+, NK cells) were stationary and did not differ during the development of CR compared with syngeneic transplants used as controls. Instead, ED-1+ macrophages alone increased and differed when comparing grafts developing CR and non-rejecting grafts [17].
The late mucosal alterations can be the result of early events including ischemia–reperfusion or episodes of acute rejection. Thus, it has been suggested that an immunological priming induces chronic rejection after acute rejection, as the fibrosis persisted after the resolution of the acute, transient inflammatory response [37]. In addition, modulating the inflammatory response after ischemia–reperfusion (IR) injury using different TNF-α inhibitors decreased the inflammatory changes after IR injury in all treatment groups in an isogenic transplant model. Besides improved 7-day survival and reducing ischemia reperfusion injury, early infliximab treatment significantly reduced leukocyte infiltration and the development of mesenteric fibrosis over a long-term surveillance period of 6 months [38].
Muscular Layer and Graft Dysmotility
Besides graft fibrosis and inflammation which are also observed in other chronically rejecting organs, intestine has its own manifestation of the CR, namely the dysmotility and hypertrophy of the muscular layer. Experimental data indicate that severe damage to the muscularis and the enteric nervous system occurs before clinical or mucosal changes become apparent [39]. Intestinal smooth muscle hypertrophy and hyperplasia, associated with abnormal contractile and electrical activities, were observed in both rat and dog intestines with CR [40, 41]. These grafts showed a threefold increase in the thickness of the muscularis externa as a result of both smooth muscle hyperplasia and hypertrophy. Muscle strips from these chronically rejecting grafts generated only about 25% of the normal contractile force [41]. The immunological phenomena behind these findings seem to be represented by an infiltration of the muscular layer by NK plus CD5+ leukocytes and a localized production of interferon gamma in both muscularis and mucosa [42].
Part of this muscular hyperplasia seems to have been triggered by the cyclosporine treatment used to prevent the early acute rejection and develop the CR model [43]. Although the loss of myenteric ganglia seems irreversible, a switch to tacrolimus therapy has effectively limited the progression of this subclinical CR phenomenon. The improvement in muscular motility and the reduction in inhibition of neural innervation are probably due to the cessation of infiltrating immunocytes and to the sprouting of remaining myenteric nerves [44].
The origin of this inflammatory process within the muscular layer may be related to the ischemia reperfusion injury in early post-transplant phase. A complex inflammatory milieu has been described in the muscular layer including neutrophil, macrophage, and T cell infiltration as well as the upregulation of nonspecific inflammatory mediators such as IL-6 and MCP-1 [45, 46]. This early inflammatory activation seems to have been better suppressed by tacrolimus compared to sirolimus: Additional infliximab (an anti-TNF antibody) application did not influence the cellular and molecular inflammatory response in the post-acute phase after transplantation [47]. The activated macrophages in the muscular layer induce graft dysmotility and postoperative ileus, mostly through nitric oxide release from iNOS and prostaglandins. Application of infliximab at reperfusion in combination with tacrolimus significantly improved smooth muscle function and reduced lower mRNA expression of the cytokines IL-6, IL-1b, and TNF 1 week after allotransplantation [48]. Taken into consideration together, these findings suggest that the muscular impairment and the ensuing graft dysmotility may be (at least in part) the consequence of early inflammatory events and that its control may require additional targeted interventions apart from the standard antirejection therapy.
Opportunities for Prevention and Intervention
Given the complex and unclear etiology of CAE and our present inability to reach an early diagnosis, the possibilities for prevention and therapeutic intervention are very limited. However, a sizeable body of experimental evidence and an increasing number of clinical reports hint toward the protective effect of several interventions including a simultaneously grafted liver, the central role of immunosuppression, and the beneficial effects of controlling the DSA development after transplantation.
The immune-modulatory and tolerogenic effect of a transplanted liver has been observed almost half a century ago [49], but the immunologic and molecular basis of this phenomenon is still elusive. The ability of a simultaneously grafted liver to prevent or alleviate acute rejection of a second organ from the same donor has been signaled after kidney [50], pancreas [51], or intestinal transplantation [52, 53]. Moreover, liver transplantation (alone or in combination with other organs) can be performed in the presence of positive lymphocytic crossmatch in sensitized recipients [54, 55] although this scenario may result in worse long-term outcomes [56]. Several reports have described beneficial long-term effects of the liver graft on a simultaneously transplanted intestine in both experimental and clinical settings. Accordingly, after brief immunosuppressive course, isolated rat intestinal allografts demonstrated changes corresponding to CR within 100 days, while combined liver-intestinal transplants revealed normal tissue architecture and long-term acceptance (> 150 days) [57]. These experimental observations have been confirmed by several clinical reports. Among the five hundred intestinal transplants reported by Abu Elmagd et al. [8], the cumulative risk of graft loss due to rejection (both acute and chronic) was significantly higher for the isolated intestinal allografts compared with liver-containing grafts (liver–intestine and full multivisceral) with a hazard ratio of 5321. Similarly, liver-containing allografts experienced a significantly better chronic rejection-free survival compared with the liver-free visceral allografts irrespective of “immunosuppressive era”. These findings were confirmed by the most recent registry report based on 2147 transplants performed after 2001 [5]. Part of the protection may be due to liver allograft clearing of preexisting anti-HLA antibodies. In a series of 23 patients undergoing intestinal re-transplantation with a liver-free (n = 13) or a liver-inclusive allograft (n = 10) [58], both patient and graft survival after 1 , 3 , and 5 years were better in the recipients of liver-inclusive allografts. In addition, liver-inclusive re-transplantations were associated with significant clearance of preformed DSA and less development of de novo DSA, whereas the rate and severity of ACR were markedly decreased and CR was not observed.
Donor-specific anti-HLA antibodies are increasingly suggested as one of the factors behind the late graft loss in kidney transplantation. About one-third of the intestinal transplantation seems to harbor or develop anti-HLA antibodies [33, 59]. A prospective study [60] screened for DSA development of 79 intestinal allograft recipients (of which 40 also received a liver) during the first 3 years after transplantation. Twenty-two (28%) patients developed de novo DSA at a median post-transplant period of 3 (1–36) months. De novo DSA occurrence was similar between the liver-inclusive and liver-free allografts, and a fall in preformed DSA levels was seen after transplantation regardless of the presence of liver graft. These results differ slightly from the literature and were obtained after the addition of a single-dose rituximab (150 mg/m 2 body surface area) to the more commonly used thymoglobulin induction. Moreover, the recipients of liver-free allografts also received an IL-2 receptor antibody (basiliximab or daclizumab) in addition to the maintenance immunosuppression. This study also suggests that a more potent induction and maintenance immunosuppression in liver-free transplants may have influenced the dynamics of DSA development and brought it to levels corresponding to liver-inclusive grafts.
Rituximab and plasmapheresis may reduce the concentration of circulating anti-HLA antibodies but both methods are ineffective against antibody-producing plasma cells in the tissues. These cells may be depleted by proteasome inhibitors like bortezomib, and several reports have shown evidence of bortezomib efficacy in the reduction and elimination of DSA after renal and pancreas transplantation [61, 62]. In the area of intestinal transplantation, the use of bortezomib has been limited to isolated cases as salvage therapy during refractory ACR [63,64,65,66] and its routine use in desensitization or treatment remains to be determined.
Fish oil has been long debated as beneficial to CR due to the n-3 polyunsaturated fatty acids (n-3 PUFA) it contains. It has been suggested that n-3 PUFA manifest a variety of putative immune-regulatory effects including the ability to delay cardiac [67] or intestinal [68] acute rejection in rodents. A recent series of studies in rats with intestinal chronic rejection (F344 intestines into Lewis recipients and a 2-week cyclosporine course) found a significantly decreased chronic rejection score and increased postoperative weight gain rate [69], an enhanced recovery of the gut microbiota (with a significant decrease in gut bacterial proportions of E. coli and Bacteroides spp and an increase in Lactobacillaces spp), as well as a maintained epithelial tight junctions integrity with an improved mucosal structure [70]. In the clinical setting, there are no reports on the effect of fish oil on the postoperative course (including CR) after ITx. In spite of the optimism and active ongoing research on the effect of fish oil on the intestinal failure-associated liver fibrosis [71, 72], several randomized controlled trials and meta-analyses could not find consistent, clinically important benefit of fish oil administration after kidney transplantation [73, 74].
Another strategy to mitigate CAE, explored in several experimental studies, is the modulation of the innate immunity (antigen-independent) mainly achieved through TNF-α inhibition. An initial set of observations indicated that an early, brief treatment with a combination of an anti-CD4 non-depleting antibody and etanercept (a TNF-α inhibitor acting as decoy receptor) significantly prolonged long-term graft survival in more than 50% of the recipients of intestinal grafts [75]. These findings were confirmed and expanded using infliximab (a chimeric-monoclonal-anti-TNF-α antibody). A perioperative, single dose of infliximab resulted in lesser pro-inflammatory cytokine levels in the graft, reduced cellular inflammation, and improved smooth muscle contractility early after ITx in rats [48, 76]. An independent group confirmed that a single dose of infliximab improved 7-day survival and ischemia reperfusion injury and reduced the numbers of graft-infiltrating T cells, ED1 monocytes, and macrophages [38]. The long-term effects of the initial injury appeared reduced as well. Interestingly, etanercept revealed a weaker protective effect compared to infliximab. The pro-inflammatory milieu and the intra-graft recruitment of immunocytes from the monocyte–macrophage lineage during IR and acute rejection appear as early events in the development of late changes in other graft types [77]. Hence, the early modulation of the innate immunity and ischemia–reperfusion injury may have also resulted in late improvements, supporting the use of anti-TNF-α agents as additional interventions after intestinal transplantation [78]. Other promising biologic agents such as the neutralizing anti-sonic hedgehog signaling monoclonal antibodies [79] deserve further evaluation.
Discussion
The advent of tacrolimus-based immunosuppression has facilitated dramatic improvements in short-term outcomes for recipients of an intestine allograft. However, the late results of intestinal transplantation continue to be marred by the spectrum of CR or chronic allograft enteropathy, currently representing the main cause of late graft loss.
Experimental studies have provided valuable insights into the natural history of intestinal CR, but its real causes remain unclear. As with other solid organ transplants, CR is likely caused by a combination of several antigen-dependent and independent factors [15, 78, 80,81,82]. However, rodent models have several major limitations including a different immunology and a different response to various doses of immune-suppressants as compared to humans [83, 84]. The different response to the immune-suppressants and the higher doses usually required in rats were the main reasons why the current review did not analyze in detail the plethora of animal studies comparing different regimens of the two main immune-suppressants currently used (cyclosporine and tacrolimus) when evaluating CR. The role of immunosuppression is, however, obvious and undisputed, and it is best illustrated by the difference in results between the different “immunosuppressive eras” [5, 8]. Although the use of tacrolimus for maintenance immunosuppression is universal [10, 12, 85,86,87,88], there are center specific differences in dosage or tolerance induction protocols. Likewise, the use of mammalian target of rapamycin inhibitors (sirolimus, everolimus) either as initial immunosuppressive or as a later switch in patients with impaired renal function or with malignancies varies between different centers [89,90,91,92]. The impact of all these factors on the development of CR is poorly studied, although registry reports indicate a superior graft survival when maintenance immunosuppression is based on sirolimus [5]. Even if the high rate of acute rejection with its serious consequences leaves little room for immunosuppression trials, the increasing evidence on the ability of various biologic agents (belatacept, infliximab, eculizumab) to modulate the immune response after transplantation mandates further consideration.
The role of IR injury in the development of chronic tissue changes has been repeatedly demonstrated [81, 93]. Many of the features encountered after IR injury such as the microvascular and endothelial injury, inflammation in the muscular layer or the macrophage infiltrates are also found in the grafts with CR, supporting a causal relationship between the two entities [17, 41, 48]. Consequently, the various strategies to mitigate IR injury may also curb the development of CR [94].
Humoral immunity will continue to attract interest as both early and late outcomes have been shown to be substantially worse among patients with pre-transplant anti-HLA DSA [33, 36, 95]. However, the mere detection of circulating DSAs is insufficient to indicate a risk for related antibody-mediated complications, as the clinical consequence of DSAs may range from the absence of injury to hyperacute antibody-mediated rejection [96]. These observations suggest that DSA are not equally pathogenic so antibody concentration, antigen availability, IgG subclass composition, and their subsequent complement-binding ability need to be explored [34, 35, 97,98,99]. All these details and their relationship with the outcome need to be assessed to provide a rationale for any aggressive desensitization attempts through plasmapheresis and/or combined liver and intestine transplantation.
Changes in the microbiota after intestinal transplantation are an area that recently gained increased attention as intestinal microbiota has been convincingly associated with several human diseases including obesity, diabetes, and inflammation [100, 101]. Several studies indicated a close interplay between microbiota, host immune cells, and the intestine with inflammatory bowel diseases (particularly Crohn’s disease) as noted consequences of its imbalance. In intestinal transplantation, complex alterations in the microbiome have been signaled both during uncomplicated course [102] and in relationship to acute rejection [103]. These alterations may be partly explained by the introduction of oxygen via the ileostomy into the normally anaerobic ileum but also by the exposure to antibiotics because infections are universal in this patient group [10, 104]. During episodes of acute rejection, the proportion of Firmicutes significantly decreased, while Proteobacteria increased. Consequently, it has been suggested that the relative proportions of several bacterial taxa in ileal effluent (particularly Firmicutes) could be used to monitor intestinal rejection [103].
Bacteria closely interact with the host and modulate both the local and the systemic immunity, and nucleotide-binding and oligomerization domain (NOD)-2 protein plays a key role in the sensing of microbial products. Intestinal graft recipients with mutant NOD2 genes have ≈ 100 times higher risk to develop rejection than non-muted patients. Additionally, the CX3CR1(+) myeloid cells of the lamina propria of these patients do not exhibit the characteristic morphological phenotype and fail to express key genes expressed by normal NOD2 (+) cells [105, 106]. Besides the bacterial effects on the intestine, the leakage of bacteria and bacterial products (i.e., LPS) into the recipient may activate numerous cell types including lymphocytes of the endothelia and may favor both acute [107] and chronic rejection [108, 109]. Altogether, these findings indicate intestinal microbiota both as a factor in the pathogenesis of CR as well as a potential opportunity for its monitoring, but more research is mandated.
The effect of humoral and cellular immunity on CR must be further clarified and their role is currently being further developed, so it is worthwhile to devote few lines to recent studies on non-HLA-allo- and autoantibodies (non-HLAabs) and moreover on microchimerism plus tolerance after clinical ITx.
A possible role in CR development was studied for non-HLA-allo- and autoantibodies (non-HLAabs), the immune activity of which has been proven to favor allograft rejection in kidney and heart transplantation. Gerlach et al. [110] have recently described their role in intestinal transplantation on 29 ITx recipients examining the development of anti-Angiotensin II type I receptor antibodies (anti-AT1R) and anti-Endothelin-Type A receptor antibodies (anti-ETAR). Twenty patients developed non-HLAabs (anti-AT1R and/or anti-ETAR): They manifested a higher rate of allograft rejection than controls (80 vs. 55%), especially a higher rate of antibody-mediated rejections (55 vs. 11%, p < 0.01) with detection of donor-specific anti-HLAabs. All rejection episodes in the non-HLAabs group appeared around the time of positive non-HLAabs detection. Their data suggest that antibody-mediated mechanisms, targeting antigens beyond HLA, may trigger and accelerate immune responses and non-HLAabs could enhance rejection and affect long-term allograft survival.
It has been demonstrated that T-regulatory (Tregs) cells could promote the establishment of allogeneic mixed microchimerism as well as the induction of donor-specific tolerance, controlling both acute and chronic rejection and contributing to the protection of allograft from ischemia/reperfusion injury. Ceulemans et al. [111] promoted Tregs-dependent graft-protective mechanisms on 13 consecutive ITx over 15 years through donor-specific blood transfusion (DSBT), avoiding high-dose steroids/calcineurin inhibitors and minimizing reperfusion injury/endotoxin translocation. Early ACR developed in two (15%), while late ACR in three recipients (23%): All were reversible. No CR occurred with mean follow-up of 3.5 years, no DSA were detected and a high frequency of circulating CD4 + CD45RA-Foxp3hi memory Tregs was found (1.8% [1.39–2.21]), comparable to tolerant kidney transplant (KTx) recipients. The authors showed that DSBT, in a low-inflammatory/pro-regulatory environment, activates Tregs at levels similar to tolerant-KTx without causing sensitization, limiting acute and chronic rejection under reduced immunosuppression, and thereby prolonging long-term survival after ITx.
Innate immunity could have a role in microchimerism development and subsequently in graft outcome as well. Innate lymphoid cell (ILC) populations in the human gut and their turnover and subsets after transplantation have recently represented the target of few human studies. Weiner et al. [112] demonstrated that donor-derived ILCs persist long term after transplantation (up to 8 years) in the recipient, while Talayero et al. [113] showed that, different from native intestines, a CD3(−) intraepithelial lymphocytes subset predominates in grafts (significantly higher in patients receiving corticosteroids) during first year after transplantation: Viability of intestinal grafts may depend on the balance among pro-inflammatory and homeostatic roles of different ILC subsets.
Conclusions
CR affects up to 10% of intestinal recipients but its early diagnosis remains elusive and pharmacological therapeutic options are lacking. Nevertheless, important steps have been taken toward understanding the whole phenomenon. At the same time, it has become increasingly obvious that the intestinal transplant community is facing the same dilemma as two decades ago, when it became evident that no blood test could signal acute rejection and a more radical approach represented by frequent mucosal biopsies was needed. As none of the investigations currently in use can diagnose CR at an early stage, novel approaches and strategies need to be identified to diagnose, prevent, and hopefully treat it. Experimental and clinical investigations identified several promising starting points but the low case volume at most centers is currently challenging their clinical translation [114,115,116]. Hence, multicenter collaborations are greatly needed to explore and validate these novel approaches.
Key Messages
-
Chronic rejection occurs in up to 10% of the recipients after intestinal transplant
-
Intestinal biopsies are not helpful in order to diagnose it
-
Allograft removal nowadays still represents the only available therapy
-
Prevention is difficult because of the lack of diagnostic means
-
Liver inclusion seems to reduce the incidence of chronic rejection
-
DSA clearance may help in reducing the impact of it after intestinal transplant
References
Todo S, Tzakis AG, Abu-Elmagd K, et al. Intestinal transplantation in composite visceral grafts or alone. Ann Surg. 1992;216:223–233.
Abu-Elmagd KM, Tzakis A, Todo S, et al. Monitoring and treatment of intestinal allograft rejection in humans. Transplant Proc. 1993;25:1202–1203.
Abu-Elmagd K, Todo S, Tzakis A, et al. Rejection of human intestinal allografts: alone or in combination with the liver. Transplant Proc. 1994;26:1430–1431.
Lee RG, Nakamura K, Tsamandas AC, et al. Pathology of human intestinal transplantation. Gastroenterology. 1996;110:1820–1834.
Grant D, Abu-Elmagd K, Mazariegos G, et al. Intestinal transplant registry report: global activity and trends. Am J Transplant. 2015;15:210–219.
Nagai S, Mangus RS, Anderson E, et al. Intestinal graft failure: should we perform the allograft enterectomy before or with retransplantation? Transplantation. 2017;101:411–420.
Swanson BJ, Talmon GA, Wisecarver JW, et al. Histologic analysis of chronic rejection in small bowel transplantation: mucosal and vascular alterations. Transplantation. 2013;95:378–382.
Abu-Elmagd KM, Costa G, Bond GJ, et al. Five hundred intestinal and multivisceral transplantations at a single center: major advances with new challenges. Ann Surg. 2009;250:567–581.
Nayyar N, Mazariegos G, Ranganathan S, et al. Pediatric small bowel transplantation. Semin Pediatr Surg. 2010;19:68–77.
Selvaggi G, Nishida S, Levi D, et al. Intestinal and multivisceral transplantation at the University of Miami. Clin Transpl. 2009;211–217.
Lauro A, Bagni A, Zanfi C, et al. Mortality after steroid-resistant acute cellular rejection and chronic rejection episodes in adult intestinal transplants: report from a single center in induction/preconditioning era. Transplant Proc. 2013;45:2032–2033.
Ramisch D, Rumbo C, Echevarria C, et al. Long-term outcomes of intestinal and multivisceral transplantation at a single center in Argentina. Transplant Proc. 2016;48:457–462.
Gondolesi, G, Fernandez A, Burghardt K, et al. Meeting Report of the XIV International Small Bowel Transplant Symposium: Summary of Presentations, Workshops, and Debates From a Comprehensive Meeting on Intestinal Failure, Rehabilitation, and Transplantation, Buenos Aires, Argentina, June 10–13, 2015. JPEN J Parenter Enteral Nutr 2017 Apr 1:148607117701696; https://doi.org/10.1177/0148607117701696.
Remotti H, Subramanian S, Martinez M, et al. Small-bowel allograft biopsies in the management of small-intestinal and multivisceral transplant recipients. histopathologic review and clinical correlations. Arch Pathol Lab Med. 2012;136:761–771.
Demetris AJ, Murase N, Lee RG, et al. Chronic rejection. A general overview of histopathology and pathophysiology with emphasis on liver, heart and intestinal allografts. Ann Transplant. 1997;2:27–44.
Orloff SL, Yin Q, Corless CL, et al. A rat small bowel transplant model of chronic rejection: histopathologic characteristics. Transplantation. 1999;68:766–779.
de Bruin RWF, Stein-Oakley AN, Kouwenhoven EA, et al. Functional, histological, and inflammatory changes in chronically rejecting small bowel transplants. Transpl Int. 2000;13:1–11.
Langrehr JM, Banner B, Lee KK, et al. Clinical course, morphology, and treatment of chronically rejecting small bowel allografts. Transplantation. 1993;55:242–250.
Ma H, Wang J, Wang J, et al. Features of chronic allograft rejection on rat small intestine transplantation. Pediatr Transplant. 2007;11:165–172.
Tryphonopoulos P, Weppler D, Nishida S, et al. Mucosal fibrosis in intestinal transplant biopsies correlates positively with the development of chronic rejection. Transplant Proc. 2006;38:1685–1686.
Land WG, Agostinis P, Gasser S, et al. Transplantation and damage-associated molecular patterns (DAMPs). Am J Transplant. 2016;16:3322–3337.
Ogita K, Hopkinson K, Nakao M, et al. Stress responses in graft and native intestine after rat heterotopic small bowel transplantation. Transplantation. 2000;69:2273–2277.
Oltean M, Dindelegan G, Kurlberg G, et al. Intragraft heat shock protein-60 expression after small bowel transplantation in the mouse. Transplant Proc. 2004;36:350–352.
Mehta N, Caroll M, Sykes DE, et al. Heat shock protein 70 expression in native and heterotopically transplanted rat hearts. J Surg Res. 1997;70:151–157.
Trieb K, Dirnhofer S, Krumbock N, et al. Heat shock protein expression in the transplanted human kidney. Transpl Int. 2001;14:281–286.
Wang J, Li Y, Li J. Cell stress response in rat chronic small bowel allograft rejection. Transplant Proc. 2013;45:2539–2542.
Duquesnoy R, Liu K, Fu X, et al. Evidence for heat-shock protein immunity in a rat cardiac allograft model of chronic rejection. Transplantation. 1999;67:156–164.
Moliterno R, Valdivia L, Pan F, et al. Heat shock reactivity of lymphocytes isolated from heterotopic rat cardiac allografts. Transplantation. 1995;59:598–604.
Masuda H, Fukumoto M, Hirayoshi K, et al. Coexpression of the collagen-binding stress protein HSP47 gene and alpha1(I) and alpha1(III) collagen genes in carbon tetrachloride induced rat liver fibrosis. J Clin Investig. 1994;94:2481–2488.
Moriyama T, Kawada N, Ando A, et al. Up-regulation of HSP47 in the mouse kidneys with unilateral ureteral obstruction. Kidney Int. 1998;54:110–119.
Kouwenhoven EA, Stein-Oakley AN, Maguire JA, et al. Increased expression of basic fibroblast growth factor during chronic rejection in intestinal transplants is associated with macrophage infiltrates. Transpl Int. 1999;12:42–49.
Haas M, Sis B, Racusen LC, et al. Banff 2013 meeting report: inclusion of c4d-negative antibody-mediated rejection and antibody-associated arterial lesions. Am J Transplant. 2014;14:272–283.
Abu-Elmagd KM, Wu G, Costa G, et al. Preformed and de novo donor specific antibodies in visceral transplantation: long-term outcome with special reference to the liver. Am J Transplant. 2012;12:3047–3060.
Lee H, Min JW, Kim JI, et al. Clinical significance of HLA-DQ antibodies in the development of chronic antibody-mediated rejection and allograft failure in kidney transplant recipients. Med (Baltim). 2016;95:e3094.
Calp-Inal S, Ajaimy M, Melamed ML, et al. The prevalence and clinical significance of C1q-binding donor-specific anti-HLA antibodies early and late after kidney transplantation. Kidney Int. 2016;89:209–216.
Bond G, Reyes J, Mazariegos G, et al. The impact of positive T-cell lymphocytotoxic crossmatch on intestinal allograft rejection and survival. Transplant Proc. 2000;32:1197–1198.
Pech T, von Websky M, Ohsawa I, et al. Intestinal regeneration, residual function and immunological priming following rescue therapy after rat small bowel transplantation. Am J Transplant. 2012;12:S9–S17.
Gerlach UA, Atanasov G, Wallenta L, et al. Short-term TNF-alpha inhibition reduces short-term and long-term inflammatory changes post-ischemia/reperfusion in rat intestinal transplantation. Transplantation. 2014;97:732–739.
Heeckt PF, Halfter W, Schraut WH, et al. Chronic rejection causes early destruction of the intrinsic nervous system in rat intestinal transplants. Am J Physiol. 1997;273:G413–G421.
Sugitani A, Bauer AJ, Reynolds JC, et al. The effect of small bowel transplantation on the morphology and physiology of intestinal muscle: a comparison of autografts versus allografts in dogs. Transplantation. 1997;63:186–194.
Heeckt PF, Halfter WM, Schraut WH, et al. Small bowel transplantation and chronic rejection alter rat intestinal smooth muscle structure and function. Surgery. 1993;114:449–456.
Su GL, Walgenbach KJ, Heeckt PH, et al. Increased expression of interferon-gamma in a rat model of chronic intestinal allograft rejection. Transplantation. 1996;62:242–248.
Heeckt PF, Halfter WM, Lee KK, et al. Prolonged in vivo administration of cyclosporine causes enteric smooth muscle hyperplasia in normal rat intestine and small bowel grafts. Transplant Proc. 1994;26:1604.
Heeckt PF, Lee KK, Halfter WM, et al. Functional impairment of enteric smooth muscle and nerves caused by chronic intestinal allograft rejection regresses after FK506 rescue. Transplantation. 1995;59:159–164.
Fujishiro J, Pech TC, Finger TF, et al. Influence of immunosuppression on alloresponse, inflammation and contractile function of graft after intestinal transplantation. Am J Transplant. 2010;10:1545–1555.
Walgenbach KJ, Heeckt PF, Kalff JC, et al. Increase of interleukin-6 in the intestinal mucosa and muscularis following chronic rejection after small bowel transplantation. Transplant Proc. 1998;30:2600.
Pech T, Fujishiro J, Finger T, et al. Effects of immunosuppressive therapy after experimental small bowel transplantation in rats. Transpl Immunol. 2011;25:112–118.
Pech T, Fujishiro J, Finger T, et al. Combination therapy of tacrolimus and infliximab reduces inflammatory response and dysmotility in experimental small bowel transplantation in rats. Transplantation. 2012;93:249–256.
Calne RY, Sells RA, Pena JR, et al. Induction of immunological tolerance by porcine liver allografts. Nature. 1969;223:472–476.
Rasmussen A, Davies HF, Jamieson NV, et al. Combined transplantation of liver and kidney from the same donor protects the kidney from rejection and improves kidney graft survival. Transplantation. 1995;59:919–921.
Wang C, Sun J, Wang L, et al. Combined liver and pancreas transplantation induces pancreas allograft tolerance. Transplant Proc. 1997;29:1145.
Zhong R, He G, Sakai Y, et al. Combined small bowel and liver transplantation in the rat: possible role of the liver in preventing intestinal allograft rejection”. Transplantation. 1991;52:550–552.
Kobayashi E, Kamada N, Enosawa S, et al. Prevention by liver transplantation of the graft-versus-host reaction and allograft rejection in a rat model of small bowel transplantation. Transplantation. 1994;57:177–181.
Nakamura K, Murase N, Becich MJ, et al. Liver allograft rejection in sensitized recipients. Observations in a clinically relevant small animal model. Am J Pathol. 1993;142:1383–1391.
Neumann UP, Lang M, Moldenhauer A, et al. Significance of a T-lymphocytotoxic crossmatch in liver and combined liver-kidney transplantation. Transplantation. 2001;71:1163–1168.
Askar M, Schold JD, Eghtesad B, et al. Combined liver-kidney transplants: allosensitization and recipient outcomes. Transplantation. 2011;91:1286–1292.
Meyer D, Otto C, Rummel C, et al. Tolerogenic effect of the liver for a small bowel allograft. Transpl Int. 2000;13:S123–S126.
Wu G, Cruz RJ. Liver inclusion improves outcomes of intestinal retransplantation in adults. Transplantation. 2015;99:1265–1272.
Gerlach UA, Lachmann N, Sawitzki B, et al. Clinical relevance of the de novo production of anti-HLA antibodies following intestinal and multivisceral transplantation”. Transpl Int. 2013;27:280–289.
Kubal C, Mangus R, Saxena R, et al. Prospective monitoring of donor-specific anti-HLA antibodies after intestine/multivisceral transplantation: significance of de novo antibodies. Transplantation.. 2015;99:e49–e56.
Walsh RC, Everly JJ, Brailey P, et al. Proteasome inhibitor-based primary therapy for antibody-mediated renal allograft rejection. Transplantation. 2010;89:277–284.
Flechner SM, Fatica R, Askar M, et al. The role of proteasome inhibition with bortezomib in the treatment of antibody-mediated rejection after kidney-only or kidney-combined organ transplantation. Transplantation. 2010;90:1486–1492.
Gerlach UA, Schoenemann C, Lachmann N, et al. Salvage therapy for refractory rejection and persistence of donor-specific antibodies after intestinal transplantation using the proteasome inhibitor bortezomib. Transpl Int. 2011;24:e43–e45.
Petit LM, Rabant M, Canioni D, et al. Impacts of donor-specific anti-HLA antibodies and antibody-mediated rejection on outcomes after intestinal transplantation in children. Pediatr Transplant. 2017;. https://doi.org/10.1111/petr.12847.
Island ER, Gonzalez-Pinto IM, Tsai HL, et al. Successful treatment with bortezomib of a refractory humoral rejection of the intestine after multivisceral transplantation. Clin Transpl. 2009:465–469.
Fujiwara S, Wada M, Kudo H, et al. Effectiveness of bortezomib in a patient with acute rejection associated with an elevation of donor-specific HLA antibodies after small-bowel transplantation: case report. Transplant Proc. 2016;48:525–527.
Otto DA, Kahn DR, Hamm MW, et al. Improved survival of heterotopic cardiac allografts in rats with dietary n-3 polyunsaturated fatty acids. Transplantation. 1990;50:193–198.
Ogita K, Suita S, Taguchi T. Effects of omega-3 fatty acids in rat allogenic small intestinal transplantation. Pediatr Surg Int. 2003;19:157–161.
Wang J, Li Y, Li J. Attenuation of rat chronic small bowel allograft rejection by n-3 polyunsaturated fatty acids is associated with reduced expression of graft IL-15. Pediatr Transplant. 2013;17:561–566.
Li Q, Zhang Q, Wang C, et al. Fish oil enhances recovery of intestinal microbiota and epithelial integrity in chronic rejection of intestinal transplant. PLoS ONE. 2011;6:e20460.
Nandivada P, Fell GL, Mitchell PD, et al. Long-term fish oil lipid emulsion use in children with intestinal failure-associated liver disease. J Parenter Enteral Nutr. 2017;41:930–937.
Belza C, Thompson R, Somers GR, et al. Persistence of hepatic fibrosis in pediatric intestinal failure patients treated with intravenous fish oil lipid emulsion. J Pediatr Surg. 2017;52:795–801.
Tatsioni A, Chung M, Sun Y, et al. Effects of fish oil supplementation on kidney transplantation: a systematic review and meta-analysis of randomized, controlled trials. J Am Soc Nephrol. 2005;16:2462–2470.
Lim AK, Manley KJ, Roberts MA, et al. Fish oil treatment for kidney transplant recipients: a meta-analysis of randomized controlled trials. Transplantation. 2007;83:831–838.
Langrehr JM, Gube K, Hammer MH, et al. Short-term anti-CD4 plus anti-TNF-alpha receptor treatment in allogeneic small bowel transplantation results in long-term survival. Transplantation. 2007;84:639–646.
Pech T, Finger T, Fujishiro J, et al. Perioperative infliximab application ameliorates acute rejection associated inflammation after intestinal transplantation. Am J Transplant. 2010;10:2431–2441.
Eugui EM. Fibrogenesis in chronic allograft rejection: underlying mechanisms and pharmacological control. Transplant Proc. 2002;34:2867–2871.
Pascher A, Klupp J. Biologics in the treatment of transplant rejection and ischemia/reperfusion injury: new applications for TNF alpha inhibitors?”. BioDrugs. 2005;19:211–231.
Chen Y, Li X, Tian L, et al. Inhibition of sonic hedgehog signaling reduces chronic rejection and prolongs allograft survival in a rat orthotopic small bowel transplantation model. Transplantation. 2007;83:1351–1357.
Pratschke J, Wilhelm MJ, Laskowski I, et al. Influence of donor brain death on chronic rejection of renal transplants in rats. J Am Soc Nephrol. 2001;12:2474–2481.
Tullius SG, Heemann U, Hancock WW, et al. Long-term kidney isografts develop functional and morphologic changes that mimic those of chronic allograft rejection. Ann Surg. 1994;220:425–432.
Tullius SG, Nieminen M, Bechstein WO. Contribution of early acute rejection episodes to chronic rejection in a rat kidney retransplantation model. Kidney Int. 1998;53:465–472.
Langrehr JM, Hoffman RA, Demetris AJ, et al. Evidence that indefinite survival of small bowel allografts achieved by a brief course of cyclosporine or FK506 is not due to systemic hyporesponsiveness. Transplantation. 1992;54:505–510.
Nakao A, Nalesnik MA, Ishikawa T, et al. Chimerism and tolerance in rat recipients of intestinal allografts from ALS-treated donors with and without adjunct naïve-donor-strain bone-marrow cells. Transplantation. 2003;75:1575–1581.
Zanfi C, Lauro A, Cescon M, et al. Comprehensive surgical intestinal rescue and transplantation program in adult patients: Bologna experience. Transplant Proc. 2010;42:39–41.
Dopazo C, Gupte GL, Sharif K, et al. Combined liver-intestine grafts compared with isolated intestinal transplantation in children: a single-center experience. Transplantation. 2012;94:859–865.
Varkey J, Simrén M, Jalanko H, et al. Fifteen years’ experience of intestinal and multivisceral transplantation in the Nordic countries. Scand J Gastroenterol. 2015;50:278–290.
Farmer DG, Kattan OM, Wozniak LJ, et al. Incidence, timing, and significance of early hypogammaglobulinemia after intestinal transplantation. Transplantation. 2013;95:1154–1159.
Fishbein TM, Florman S, Gondolesi G, et al. Intestinal transplantation before and after the introduction of sirolimus. Transplantation. 2002;73:1538–1542.
Andres AM, Lopez Santamaría M, Ramos E, et al. The use of sirolimus as a rescue therapy in pediatric intestinal transplant recipients. Pediatr Transplant. 2010;14:931–935.
Herlenius G, Fägerlind M, Krantz M, et al. Chronic kidney disease–a common and serious complication after intestinal transplantation. Transplantation. 2008;86:108–113.
Lauro A, Dazzi A, Ercolani G, et al. Rejection episodes and 3-year graft survival under sirolimus and tacrolimus treatment after adult intestinal transplantation. Transplant Proc. 2007;39:1629–1631.
Morini S, Elias G, Brown M, et al. Chronic morpho-functional damage as a consequence of transient ischemia/reperfusion injury of the small bowel. Histol Histopathol. 2010;25:277–286.
Oltean M, Churchill TA. Organ-specific solutions and strategies for the intestinal preservation. Int Rev Immunol. 2014;33:234–244.
Cheng EY, Kaneku H, Farmer DG. The role of donor-specific antibodies in intestinal transplantation: experience at the University of California Los Angeles and Literature Review. Clin Transpl. 2014;153–159.
Tait BD, Süsal C, Gebel HM, et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation. 2013;95:19–47.
Crespo M, Torio A, Mas V, et al. Clinical relevance of pretransplant anti-HLA donor-specific antibodies: does C1q-fixation matter? Transpl Immunol. 2013;29:28–33.
Yell M, Muth BL, Kaufman DB, et al. C1q binding activity of de novo donor-specific HLA antibodies in renal transplant recipients with and without antibody-mediated rejection. Transplantation. 2015;99:1151–1155.
Freitas MC, Rebellato LM, Ozawa M, et al. The role of immunoglobulin-G subclasses and C1q in de novo HLA-DQ donor-specific antibody kidney transplantation outcomes. “. Transplantation. 2013;95:1113–1119.
Karlsson F, Tremaroli V, Nielsen J, et al. Assessing the human gut microbiota in metabolic diseases. Diabetes. 2013;62:3341–3349.
Schrumpf E, Kummen M, Valestrand L, et al. The gut microbiota contributes to a mouse model of spontaneous bile duct inflammation. J Hepatol. 2017;66:382–389.
Hartman AL, Lough DM, Barupal DK, et al. Human gut microbiome adopts an alternative state following small bowel transplantation. Proc Natl Acad Sci USA. 2009;106:17187–17192.
Oh PL, Martínez I, Sun Y, et al. Characterization of the ileal microbiota in rejecting and nonrejecting recipients of small bowel transplants. Am J Transplant. 2012;12:753–762.
Oltean M, Herlenius G, Gäbel M, et al. Infectious complications after multivisceral transplantation in adults. Transplant Proc. 2006;38:2683–2685.
Fishbein T, Novitskiy G, Mishra L, et al. NOD2-expressing bone marrow-derived cells appear to regulate epithelial innate immunity of the transplanted human small intestine. Gut. 2008;57:323–330.
Lough D, Abdo J, Guerra-Castro JF, et al. Abnormal CX3CR1+ lamina propria myeloid cells from intestinal transplant recipients with NOD2 mutations. Am J Transplant. 2012;12:992–1003.
Kawai M, Kitade H, Koshiba T, et al. Intestinal ischemia reperfusion and lipopolysaccharide transform a tolerogenic signal into a sensitizing signal and trigger rejection. Transplantation. 2009;87:1464–1467.
Heemann UW, Tullius SG, Schmid C, et al. Infection-associated cellular activation accelerates chronic renal allograft rejection in rats. Transpl Int. 1996;9:137–140.
Nagano H, Nadeau KC, Kusaka M, et al. Infection-associated macrophage activation accelerates chronic renal allograft rejection in rats. Transplantation. 1997;64:1602–1605.
Gerlach UA, Lachmann N, Ranucci G, et al. Non-HLA antibodies may accelerate immune responses after intestinal and multivisceral transplantation. Transplantation. 2017;101:141–149.
Ceulemans LJ, Braza F, Monbaliu D, et al. The Leuven immunomodulatory protocol promotes T-regulatory cells and substantially prolongs survival after first intestinal transplantation. Am J Transplant. 2016;16:2973–2985.
Weiner J, Zuber J, Shonts B, et al. Long-term persistence of innate lymphoid cells in the gut after intestinal transplantation. Transplantation. 2017;101:2449–2454.
Talayero P, Mancebo E, Calvo-Pulido J, et al. Innate lymphoid cells groups 1 and 3 in the epithelial compartment of functional human intestinal allografts. Am J Transplant. 2016;16:72–82.
Gangemi A, Tzvetanov I, Beatty E, et al. Lessons learned in pediatric small bowel and liver transplantation from living-related donors. Transplantation. 2009;87:1027–1030.
Ceulemans LJ, Monbaliu D, De Roover A, et al. Belgian multicenter experience with intestinal transplantation. Transpl Int. 2015;28:1362–1370.
Lauro A, Panaro F, Iyer KR. An overview of EU and USA intestinal transplant current activity. J Visc Surg. 2017;154:105–114.
Acknowledgments
We wish to thank Ms. Claudia Cirillo for her English language editing of our text.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lauro, A., Oltean, M. & Marino, I.R. Chronic Rejection After Intestinal Transplant: Where Are We in Order to Avert It?. Dig Dis Sci 63, 551–562 (2018). https://doi.org/10.1007/s10620-018-4909-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-4909-7