Abstract
The gut microbiota is a vast ensemble of microorganisms inhabiting the mammalian gastrointestinal tract that can impact physiologic and pathologic processes. However, our understanding of the underlying mechanism for the dynamic interaction between host and gut microbiota is still in its infancy. The highly evolved epigenetic modifications allow hosts to reprogram the genome in response to environmental stimuli, which may play a key role in triggering multiple human diseases. In spite of increasing studies in gut microbiota and epigenetic modifications, the correlation between them has not been well elaborated. Here, we review current knowledge of gut microbiota impacts on epigenetic modifications, the major evidence of which centers on DNA methylation and histone modification of the immune system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human gut microbiota is populated with over 100 trillion cells of potentially 100–1000 microbial species [1, 2], which have been shown to be involved in maintenance of human health and pathogenesis of disease [3]. During the past several years, it has been widely demonstrated that the gut microbiota has coevolved with their mammalian host and has established a complex ecosystems [4]. Recent omic-based studies have further facilitated our understanding of dynamic interplay between multiple low molecular weight (LMW) substances produced by gut microbiota and gene expression regulation or posttranslation modification of host [5, 6]. Correspondingly, epigenetics is generally defined as the study of mechanisms that do not modify genomic DNA sequence yet regulate gene expression associated with physiologic and pathologic processes [7]. Furthermore, as epigenetic modifications are reversible depending on environmental stimuli [8], novel therapies that target aberrant epigenetic states and disease are gaining momentum. Here, we will discuss recent clues that implicate influences of gut microbiota on epigenetic modifications.
Epigenetic Modifications
The term epigenetic was first coined by Conrad Waddington for the underlying mechanisms that converted identical genetic information into diverse phenotypes [9]. Interesting epigenetic cases have been identified such as in reproductive status in honeybees [10] and turtle sex determination [11]. Currently, epigenetic modifications are considered to be heritable adaptive mechanisms that regulate gene expression patterns through mitosis and/or meiosis without change in primary DNA sequences [12]. The primary focus of this review is on the two main categories of epigenetic modifications: DNA methylation and histone modifications.
DNA Methylation
DNA methylation involves the transfer of methyl group from S-adenosyl methionine to 5 position of a cytosine pyrimidine ring (m5C), which mostly happens in the context of CpG dinucleotides [13]. The CpG dinucleotides are often clustered in regions called CpG islands [14], defined as sequence ranges of more than 200 bases where a value of observed to statistically expected CpG frequencies is greater than 0.6 and a G + C content is at least 50% [15]. Approximately 60% of gene promoters in human are associated with CpG islands [16] and are generally unmethylated [17]. However, in addition to CpG islands, CpG dinucleotides are predominately methylated [18].
In mammals, DNA methylation is catalyzed by three members of the DNA methyltransferase (DNMT) family: DNMT1, DNMT3a, and DNMT3b [15]. Typically, regulation of DNA methylation on gene expression will have exactly the reverse effect in different gene regions: methylation of gene promoters is in general related to transcriptional silencing [19], while methylation of gene body is often coupled with transcriptional activation [20].
Moreover, DNA methylation does not take place entirely at CpG islands. The term CpG island shores has recently been coined as an additional ingredient of methylation phenomena, referring to regions that flank CpG islands (~2 kb) with lower CpG frequencies [21]. Methylation of CpG island shores is closely related to transcriptional inactivation [15] and is certified to exhibit more specificity among normal tissue types, between cancerous and normal cells [22], thus could be potential candidates for tumor markers. However, to our best knowledge, limited studies focus on methylation of CpG island shores which are influenced by bacteria or by gut microbiota.
Histone Modifications
Histones are proteins that package and order eukaryotic genomes into chromatin, which play an important role in epigenetic regulation with varying covalent modifications [23]. Histones mainly contain five families: H1, H2A, H2B, H3, H4, and H5. Histones H2A, H2B, H3, and H4 are known as core histones to form the nucleosome core representing two H2A–H2B dimers and a H3–H4 tetramer [24]. Histones H1 and H5 are known as the linker histones, histone H1 seals off the nucleosome at the entry and exit locations of the DNA [25], and histone H5 is now recognized as an isoform of histone H1 [26]. All histones are subject to a variety of posttranscriptional modifications, of which the most studied are acetylation and methylation.
Histone acetylation usually takes place on multiple lysine residues located within their N-terminal termini, primarily of histone 3 at lysine 9 (H3K9), lysine 14 (H3K14), lysine 18 (H3K18), lysine 23 (H3K23), histone 4 at lysine 5 (H4K5), lysine8 (H4K8), lysine 12 (H4K12), and lysine16 (H4K16) [27–30]. Histone acetylation and deacetylation is mediated by opposing practices of histone acetyl transferases (HATs) and histone deacetylases (HDACs), respectively [31]. HATs are believed to relax the chromatin structure and allow access for transcription factors, thereby promoting gene expression [32]. Conversely, HDACs promote tighter DNA–histone interaction and repress transcriptional activity [32]. Eighteen currently known HDACs are categorized into four classes depending on their homology with HDACs in yeast and subcellular location. Class I (HDACs 1–3 and 8), II (HDACs 4–7, 9, and 10), and IV (HDACs 11) require zinc for their enzyme activity, while the class III HDACs (sirtuins 1–7) are nicotine adenine dinucleotide (NAD+) dependent [33].
Histone methylation is generally involved in mono-, di-, or tri-methylation of histone 3 at lysine 4 (H3K4), lysine 9 (H3K9), lysine 27 (H3K27), lysine 36 (H3K36), lysine 79 (H3K79), lysine 20 (H3K20), of histone 3 at arginine 2 (H3R2), arginine 8 (H3R8), arginine 17 (H3R17), arginine 26 (H3R26), arginine 128 (H3R128), arginine 129 (H3R129), arginine 131 (H3R131), arginine 134 (H3R134), and methylated arginine 3 in the histone H4 (H4R3), methylated arginine 3 in the histone H2A (H2AR3) [34–46]. The consequences of histone methylation for gene expression are complex, as methylation may have opposite consequences depending on localization and number of methyl groups.
Influences of Gut Microbiota on Epigenetic Modification
An intricate and dynamic relationship exists between the gut microbiota, the immune system and epigenetic modifications [47]. The immune system develops symbiotic relationship with gut microbiota that shapes the diversity and abundance of microbiota [48]. In turn, gut microbiota and induced epigenetic modification is essential for the development and maturation of intestinal mucosal immune system of its hosts [49–53]. As epigenetic modifications of intestinal mucosal immune system mediate cross talk between gut microbiota and the mammalian host, we focus our attention on immune development. Evidence of gut-derived effector molecules effecting host epigenetics are summarized in Table 1.
Influences of Gut Microbiota on DNA Methylation
Many essential micronutrients involved in the process of DNA methylation are associated with gut microbiota. S-adenosylmethionine (SAM) is the primary methyl donor in DNA methylation, which is produced by the biological process called one-carbon metabolism [64]. Folate, choline, methionine, and vitamins B2, B6, and B12 are heavily involved in one-carbon metabolism [65]. It is worth noting that B vitamins also act as cofactors in DNA methylation [66]. Long-term folic acid supplementation before and during pregnancy was associated with higher leptin (LEP) and retinoid X receptor alpha (RXRA) gene cord blood methylation, respectively [67]. Before pregnancy, higher intakes of betaine and methionine were associated with higher cord blood methylation levels of DNMT1 CpG4 and LEP CpG4, respectively. In the second trimester of pregnancy, high methyl group donor intakes (betaine, choline, and folate) were negatively associated with gene specific cord blood methylation (betaine with LEP CpG2; choline with DNMT1 CpG4; and folate with LEP CpG2 and DNMT1 CpG4). In the last trimester of pregnancy, a high intake of choline and folate was associated with higher methylation levels of DNMT1 CpG2 and lower methylation levels of RXRA CpG2, respectively [67]. The authors did not discuss the conflicting results; we hypothesized it may be related to the dynamic process of pregnancy. Hosts must obtain these essential micronutrients exogenously from diet and gut bacteria due to their lack of biosynthesis [54, 56]. The deteriorating gut microbiome and its metabolites will inevitably interfere biochemical process of diet fermentation and thus influence the normal provision of methyl donor for DNA methylation. In addition to global DNA methylation, other bacterial metabolites that relate to DNA methylation are summarized in Table 1.
Many evidences have shown a close relation between gut microbiota and DNA methylation, both in basic researches and clinical findings. The influence of gut microbiome on the epigenetic regulation of host genes has been demonstrated with Toll-like receptor 2 (TLR2)-knockout mice [68, 69], in which the DNA methylation and gene expression in colonic mucosa of wild-type and Tlr2−/− C57BL/6 mice were interrogated. Average DNA methylation in the promoter regions of two genes which related to immune processes, Anpep and Ifit2, increased in Tlr2−/− colonic mucosa. This indicates that alterations in mucosal microbial composition induced by TLR2 deficiency contribute to transcriptomic and epigenomic modifications. Furthermore, repression of the TLR4 gene in intestinal epithelial cells (IECs) through DNA methylation can play a role in maintaining intestinal homeostasis and regulating the mucosal immune system in the gut [70]. Dapito et al. [71] in an elegant series of experiments have demonstrated that TLR4 activation by LPS generated from the intestinal microbiota contributes to hepatocellular carcinoma promotion. Interestingly, Kumar et al. [72] revealed that DNA methylation profiles in blood of pregnant women correlated with gut microbiota patterns. Eight well-matched pregnant women were classified into two groups depending on their dominant gut microbiota, i.e., Bacteroidetes, Proteobacteria, and Firmicutes. Next-generation sequencing of DNA methylomes indicated a clear correlation between predominant phyla and epigenetic patterns. Promoter DNA methylation status of genes in the HighFirm group was functionally associated with genes specifically involved in cardiovascular diseases, lipid metabolism, obesity, and the inflammatory response. This is one of the first studies that underline the association of the gut microbiota with DNA methylation profiles.
Influences of Pathogenic Bacteria on DNA Methylation
Examples of DNA methylation effects of pathogenic bacteria, such as Helicobacter pylori and Klebsiella spp, on the host have also been characterized recently. Chronic inflammation induced by Helicobacter pylori infection is responsible for DNA methylation in gastric mucosae of genes which are closely associated with gastric cancer risk [73]. H. pylori infection induces the inactivation of miR-210 gene expression in the gastric epithelium with chronic inflammation compared with uninfected gastric epithelium, with surprisingly higher rate of CpG methylation within the miR-210 locus in healthy individuals with H. pylori than healthy people without H. pylori [74]. Significantly higher levels of aberrant methylation (5.4- to 303-fold) were present in eight regions of CpG islands in the gastric mucosae of healthy volunteers with H. pylori infection, which strongly indicated that H. pylori infection potently induces aberrant methylation in multiple CpG islands [75]. Similarly, Hp-positive healthy volunteers had a higher level of DNA methylation of three miRNA genes (miR-124a-1, miR-124a-2, and miR-124a-3) in gastric mucosae than Hp-negative individuals, indicating that H. pylori infection can induce DNA methylation of miRNA genes, in addition to protein-coding genes. Infection of immature intestinal epithelial cells with Lactobacillus acidophilus/Bifidobacterium infantis and Klebsiella spp. results in over 200 regions of differential DNA modification [76].
Influences of Gut Microbiota on Histone Modifications
The gut microbiota plays a role in uptaking and secreting minerals that act as cofactors for enzymes participating in epigenetic regulation, such as cobalt, iodine, selenium, and abovementioned zinc. Furthermore, a wide range of enzymes such as the methyltransferases, acetyltransferases, deacetylases, Bir A ligase, phosphotransferases, kinases, and synthetases are produced by the gut microbiota. Various key energy metabolites including SAM, acetyl-CoA, NAD+, α-KG, and ATP serve as primary cofactors for many enzymes that regulate epigenetic modification [57]. Epicatechin and epigallocatechin-3-gallate (EGCG) can function as histone acetyltransferase (HAT) inhibitor [58, 59], which could be degraded and metabolized by the intestinal microbiota [77]. Similarly, short-chain fatty acids (SCFAs), isothiocyanate, and allyl compounds derived from human gut microflora have been shown to inhibit histone deacetylase (HDAC) activity [78, 79].
Short-chain fatty acids (SCFAs) generated through dietary carbohydrates fermentation by the gut microbiota, many of which in the class Clostridia of Firmicutes phyla, are thought to be mainly responsible for histone modifications. Several promising HDAC inhibitors (HDACi) are presently being evaluated in various stages of clinical trials for the therapy of a wide range of cancer, as well as inflammatory and degenerative disorders [80, 81]. Intriguingly, SCFAs, predominantly acetate, propionate, butyrate, caproate, and valerate have recently attracted considerable attention for their HDAC inhibitory activity [60, 62, 63, 82]. Major SCFAs-producing bacteria and products with the corresponding substrates are listed in Table 2. Schwiertz et al. [84] found elevated SCFA concentrations in overweight and obese subjects with altered gut microbiota compared to healthy controls; they speculate these changes in SCFA may play a role in the development or maintenance of obesity. The affinity of SCFAs to various G protein-coupled receptors (free fatty acid receptors) may be involved in inflammatory conditions, as well as interactions between the gut microbiota and epigenetic regulation [62, 85].
SCFAs, primarily acetate, propionate, and butyrate have recently been revealed for their beneficial effects of histone deacetylase inhibitory activity. Vinicius Andrade-Oliveira et al. [86] evidenced acetate treatment inhibited the activity of HDACs and increased global methylation status in kidney tissue undergoing ischemia and reperfusion injury. Nagendra Singh et al. reported that butyrate and propionate blocked the generation of dendritic cells from bone marrow stem cells; this effect is associated with decreased expression of the transcription factors PU.1 and RelB and is dependent on the ability of these two bacterial metabolites to inhibit histone deacetylases [87]. Butyrate is one of the most potent HDACi which inhibits most HDACs except class III and HDAC 6 and 10 of class II with approximately 80% inhibition of HDAC1/2 and a Ki value of 58 μM [88, 89]. A large number of histone hyperacetylation effects exerted by butyrate have been suggested, which can induce cell differentiation, apoptosis, and inhibit proliferation of tumor cells. In human colon tumor cell lines, butyrate treatment resulted in overexpression of p21WAF1 via hyperacetylation of the gene-associated histones, and arrest of G1 cell cycle [63]. Butyrate blocked human leukemic lymphoblasts in the G2/M phase and caused apoptotic cell death [90], and induced H4 acetylation and myeloid maturation in acute myeloid leukemia (AML) [91] and growth inhibition in human cervical carcinoma and prostate cancer cells [92, 93]. In Bcr/Abl + human leukemia cells, a model of apoptosis induction by butyrate was proposed to involve a coordinated obstruction of the cytoprotective Raf/MEK/ERK pathway in conjunction with the reactive oxygen species-dependent activation of JNK [94]. Also, butyrate-induced histone H3 acetylation and significantly up-regulated expression of Fas, P21, and P27 to induce apoptosis of lymphoma tumor cells [95] and treatment of butyrate led to an increase in histone H3 lysine 9 acetylation (H3K9Ac) levels at the promoter regions of Nos2, Il6, and Il12b [96].
A novel contributory mechanism to the anticarcinogenic effect of butyrate is the down-regulation of the key apoptotic and angiogenesis regulator neuropilin-1 (NRP-1) transcription, which has been shown to promote tumor cell migration and survival in colon cancer in response to vascular endothelial growth factor (VEGF) binding [97]. Butyrate also plays a promising role in inflammatory response by suppressing the nuclear factor κB (NF-κB) activation via inhibition of HDAC [98]. NF-κB regulates the production of pro-inflammatory cytokines involved in early immune inflammatory responses, including IL-1b, IL-2, IL-6, IL-8, IL-12, tumor necrosis factor-alpha (TNF-α), inducible nitric oxide synthase (iNOS), cyclooxygenase-2 (COX-2), intercellular adhesion molecule-1 (ICAM-1), vascular cellular adhesion molecule-1 (VCAM-1), T cell receptor-α (TCR-α), and MHC class II molecules [99–106].
In addition, butyrate as well exerts the anti-inflammatory effect by inhibiting interferon γ (IFN γ) signaling and up-regulating the expression of peroxisome proliferator-activated receptor γ (PPAR γ) [107, 108]. Evidence indicates a role for butyrate in strengthening innate immunity by enhancing the expression of the LL-37 gene, the only cathelicidin-derived peptide expressed in humans, with increased histone acetylation of the cathelicidin promoter and mitogen-activated protein (MAP) kinase signaling [63, 109–111]. What’s more, butyrate induces histone H3 lysine 27 (H3K27) acetylation of the FoxP3 locus and thus promotes differentiation of regulatory T cells in the colon [82].
Histone modifications of commensal bacteria or probiotics have also been well characterized. High concentrations of butyrate produced by Porphyromonas gingivalis could reactivate latent HIV-1 integrated in the host genome as proviral DNA copies via HDAC inhibition [69, 112]. Bacteroides vulgatus, a commensal of the gut microbiota, can induce acetylation of histone H3 through an inflammatory signaling cascade [113]. Also, B. vulgatus induces inhibition of NF-κB transcriptional activity as well as IL-6 mRNA accumulation mediated by TGF-β1, which in turn induces histone H3 deacetylation via histone deacetylase recruitment at IL-6 promoter [113]. This may contribute to the maintenance of intestinal homeostasis by inhibiting commensal bacteria to activate inflammatory responses in the intestine. Furthermore, Bifidobacterium breve and Lactobacillus rhamnosus GG, representatives of commensal probiotics, diminished the LPS-induced expression of IL-17, IL-23, and CD40 with epigenetic processes involving the inhibition of histone acetylation and the optimal enhancement of DNA methylation [114].
Influences of Pathogenic Bacteria on Histone Modifications
Specific effectors produced by pathogenic bacteria can also induce specific histone modifications. Listeria monocytogenes has been shown to increase IL-8 gene expression by inducing acetylation (lysine 8) of histone H4 and phosphorylation/acetylation (serine 10/lysine 14) of histone H3 globally and at the il8 promoter in human umbilical vein endothelial cells, as well as recruitment of the histone acetylase CREB-binding protein through a nucleotide-binding oligomerization domain 1 (Nod1) proteins-dependent activation of p38 MAPK signaling and NF-κB [69, 115, 116]. Recently, listeriolysin O (LLO)-induced K+ efflux was unveiled as an important signal leading to histone modification [117]. The increased expression of p21WAF1 induced by Helicobacter pylori is associated with the release of HDAC-1 from the p21WAF1 promoter and hyperacetylation of histone H4 [118].
Conclusion
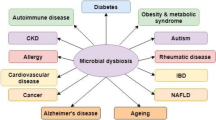
Recent studies and ‘omic’-based technologies suggest that diverse metabolites and signaling molecules produced by gut microbiota may regulate host gene expression through epigenetic modification, explaining a significant part of host–microbiota interactions (Fig. 1). However, we should not stop here; clarifying the underlying molecular mechanisms of these biological processes are still in their infancy and warrant further investigation. Specifically, it needs to be deciphered how DNA methylation or histone modification occurs at specific gene loci. What’s more, novel epigenetic modifications and enzymes which may participate in epigenetic regulation need to be discovered. Continued basic and applied studies are also needed to focus our efforts toward utilizing epigenetic-targeting drugs on microbiota and relevant microbiota-induced cancer and metabolic syndrome, an area that promises exciting preventive and therapeutic applications.
Interaction between gut microbiota and epigenetic modification. The gut microbiota could regulate epigenetic modification with varying energy metabolites and signaling molecules such as minerals, SCFAs, enzymes, and so on. Conversely, epigenetic modification of immune system can also plays a role in intestinal homeostasis. Dash lines indicate elements that remain to be elucidated or elaborated
References
Walsh CJ, Guinane CM, Hill C, Ross RP, O’Toole PW, Cotter PD. In silico identification of bacteriocin gene clusters in the gastrointestinal tract, based on the Human Microbiome Project’s reference genome database. BMC Microbiol. 2015;15:183.
Browne HP, Forster SC, Anonye BO, et al. Culturing of ‘unculturable’ human microbiota reveals novel taxa and extensive sporulation. Nature. 2016;533:543–546.
Karlsson FH, Tremaroli V, Nookaew I, et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498:99–103.
Dobson AJ, Chaston JM, Douglas AE. The Drosophila transcriptional network is structured by microbiota. BMC Genom. 2016;17:975.
Zargar A, Quan DN, Carter KK, et al. Bacterial secretions of nonpathogenic Escherichia coli elicit inflammatory pathways: a closer investigation of interkingdom signaling. MBio. 2015;6:e00025.
Parhar K, Baer KA, Parker K, Ropeleski MJ. Short-chain fatty acid mediated phosphorylation of heat shock protein 25: effects on camptothecin-induced apoptosis. Am J Physiol Gastrointest Liver Physiol. 2006;291:G178–G188.
Rakyan VK, Down TA, Balding DJ, Beck S. Epigenome-wide association studies for common human diseases. Nat Rev Genet. 2011;12:529–541.
Holland ML, Lowe R, Caton PW, et al. Early-life nutrition modulates the epigenetic state of specific rDNA genetic variants in mice. Science. 2016;353:495–498.
Noble D. Conrad Waddington and the origin of epigenetics. J Exp Biol. 2015;218:816–818.
Kucharski R, Maleszka J, Foret S, Maleszka R. Nutritional control of reproductive status in honeybees via DNA methylation. Science. 2008;319:1827–1830.
Patisaul HB, Adewale HB. Long-term effects of environmental endocrine disruptors on reproductive physiology and behavior. Front Behav Neurosci. 2009;3:10.
Blaschke K, Ebata KT, Karimi MM, et al. Vitamin C induces Tet-dependent DNA demethylation and a blastocyst-like state in ES cells. Nature. 2013;500:222–226.
Lou S, Lee HM, Qin H, et al. Whole-genome bisulfite sequencing of multiple individuals reveals complementary roles of promoter and gene body methylation in transcriptional regulation. Genome Biol. 2014;15:408.
Thomson JP, Skene PJ, Selfridge J, et al. CpG islands influence chromatin structure via the CpG-binding protein Cfp1. Nature. 2010;464:1082–1086.
Portela A, Esteller M. Epigenetic modifications and human disease. Nat Biotechnol. 2010;28:1057–1068.
Herman JG, Baylin SB. Gene silencing in cancer in association with promoter hypermethylation. N Engl J Med. 2003;349:2042–2054.
Maunakea AK, Nagarajan RP, Bilenky M, et al. Conserved role of intragenic DNA methylation in regulating alternative promoters. Nature. 2010;466:253–257.
Hemmi H, Takeuchi O, Kawai T, et al. A Toll-like receptor recognizes bacterial DNA. Nature. 2000;408:740–745.
Quinonez-Silva G, Davalos-Salas M, Recillas-Targa F, Ostrosky-Wegman P, Aranda DA, Benitez-Bribiesca L. Monoallelic germline methylation and sequence variant in the promoter of the RB1 gene: a possible constitutive epimutation in hereditary retinoblastoma. Clin Epigenetics. 2016;8:1.
Jjingo D, Conley AB, Yi SV, Lunyak VV, Jordan IK. On the presence and role of human gene-body DNA methylation. Oncotarget. 2012;3:462–474.
Savio AJ, Lemire M, Mrkonjic M, et al. MLH1 region polymorphisms show a significant association with CpG island shore methylation in a large cohort of healthy individuals. PLoS ONE. 2012;7:e51531.
Irizarry RA, Ladd-Acosta C, Wen B, et al. The human colon cancer methylome shows similar hypo- and hypermethylation at conserved tissue-specific CpG island shores. Nat Genet. 2009;41:178–186.
Liu X, Wang C, Liu W, et al. Distinct features of H3K4me3 and H3K27me3 chromatin domains in pre-implantation embryos. Nature. 2016;537:558–562.
Banks DD, Gloss LM. Equilibrium folding of the core histones: the H3–H4 tetramer is less stable than the H2A–H2B dimer. Biochemistry. 2003;42:6827–6839.
Daujat S, Zeissler U, Waldmann T, Happel N, Schneider R. HP1 binds specifically to Lys26-methylated histone H1.4, whereas simultaneous Ser27 phosphorylation blocks HP1 binding. J Biol Chem. 2005;280:38090–38095.
Bhasin M, Reinherz EL, Reche PA. Recognition and classification of histones using support vector machine. J Comput Biol. 2006;13:102–112.
Chen ZJ, Pikaard CS. Epigenetic silencing of RNA polymerase I transcription: a role for DNA methylation and histone modification in nucleolar dominance. Genes Dev. 1997;11:2124–2136.
Earley K, Lawrence RJ, Pontes O, et al. Erasure of histone acetylation by Arabidopsis HDA6 mediates large-scale gene silencing in nucleolar dominance. Genes Dev. 2006;20:1283–1293.
Lawrence RJ, Earley K, Pontes O, et al. A concerted DNA methylation/histone methylation switch regulates rRNA gene dosage control and nucleolar dominance. Mol Cell. 2004;13:599–609.
Li X, Qian W, Zhao Y, et al. Antisilencing role of the RNA-directed DNA methylation pathway and a histone acetyltransferase in Arabidopsis. Proc Natl Acad Sci USA. 2012;109:11425–11430.
Dose A, Liokatis S, Theillet FX, Selenko P, Schwarzer D. NMR profiling of histone deacetylase and acetyl-transferase activities in real time. ACS Chem Biol. 2011;6:419–424.
Mahgoub M, Monteggia LM. A role for histone deacetylases in the cellular and behavioral mechanisms underlying learning and memory. Learn Mem. 2014;21:564–568.
Jin K, Li S, Li X, Zhang J, Xu W. Design, synthesis and preliminary biological evaluation of indoline-2,3-dione derivatives as novel HDAC inhibitors. Bioorg Med Chem. 2015;23:4728–4736.
Zhang Z, Shi L, Dawany N, Kelsen J, Petri MA, Sullivan KE. H3K4 tri-methylation breadth at transcription start sites impacts the transcriptome of systemic lupus erythematosus. Clin Epigenetics. 2016;8:14.
Gavin DP, Kusumo H, Zhang H, Guidotti A, Pandey SC. Role of growth arrest and DNA damage-inducible, beta in alcohol-drinking behaviors. Alcohol Clin Exp Res. 2016;40:263–272.
Hou YJ, Zhu CC, Duan X, Liu HL, Wang Q, Sun SC. Both diet and gene mutation induced obesity affect oocyte quality in mice. Sci Rep. 2016;6:18858.
Poulin MB, Schneck JL, Matico RE, et al. Transition state for the NSD2-catalyzed methylation of histone H3 lysine 36. Proc Natl Acad Sci USA. 2016;113:1197–1201.
Zhou L, Holt MT, Ohashi N, et al. Evidence that ubiquitylated H2B corrals hDot1L on the nucleosomal surface to induce H3K79 methylation. Nat Commun. 2016;7:10589.
Sundar IK, Yao H, Rahman I. Oxidative stress and chromatin remodeling in chronic obstructive pulmonary disease and smoking-related diseases. Antioxid Redox Signal. 2013;18:1956–1971.
Huang Y, Chen D, Liu C, Shen W, Ruan Y. Evolution and conservation of JmjC domain proteins in the green lineage. Mol Genet Genomics. 2016;291:33–49.
Chen H, Zhang C, Sheng Y, Yao S, Liu Z, Zhang T. Frequent SOCS3 and 3OST2 promoter methylation and their epigenetic regulation in endometrial carcinoma. Am J Cancer Res. 2015;5:180–190.
Kim JK, Lim Y, Lee JO, et al. PRMT4 is involved in insulin secretion via the methylation of histone H3 in pancreatic beta cells. J Mol Endocrinol. 2015;54:315–324.
Guertin MJ, Zhang X, Anguish L, et al. Targeted H3R26 deimination specifically facilitates estrogen receptor binding by modifying nucleosome structure. PLoS Genet. 2014;10:e1004613.
Wang CM, Tsai SN, Yew TW, Kwan YW, Ngai SM. Identification of histone methylation multiplicities patterns in the brain of senescence-accelerated prone mouse 8. Biogerontology. 2010;11:87–102.
Pal S, Sif S. Interplay between chromatin remodelers and protein arginine methyltransferases. J Cell Physiol. 2007;213:306–315.
Karkhanis V, Wang L, Tae S, Hu YJ, Imbalzano AN, Sif S. Protein arginine methyltransferase 7 regulates cellular response to DNA damage by methylating promoter histones H2A and H4 of the polymerase delta catalytic subunit gene, POLD1. J Biol Chem. 2012;287:29801–29814.
Obata Y, Furusawa Y, Endo TA, et al. The epigenetic regulator Uhrf1 facilitates the proliferation and maturation of colonic regulatory T cells. Nat Immunol. 2014;15:571–579.
Dimitriu PA, Boyce G, Samarakoon A, Hartmann M, Johnson P, Mohn WW. Temporal stability of the mouse gut microbiota in relation to innate and adaptive immunity. Environ Microbiol Rep. 2013;5:200–210.
Khosravi A, Yanez A, Price JG, et al. Gut microbiota promote hematopoiesis to control bacterial infection. Cell Host Microbe. 2014;15:374–381.
Natoli G. Maintaining cell identity through global control of genomic organization. Immunity. 2010;33:12–24.
O’Shea JJ, Lahesmaa R, Vahedi G, Laurence A, Kanno Y. Genomic views of STAT function in CD4 + T helper cell differentiation. Nat Rev Immunol. 2011;11:239–250.
Peng D, Kryczek I, Nagarsheth N, et al. Epigenetic silencing of TH1-type chemokines shapes tumour immunity and immunotherapy. Nature. 2015;527:249–253.
Allan RS, Zueva E, Cammas F, et al. An epigenetic silencing pathway controlling T helper 2 cell lineage commitment. Nature. 2012;487:249–253.
Yu DH, Gadkari M, Zhou Q, et al. Postnatal epigenetic regulation of intestinal stem cells requires DNA methylation and is guided by the microbiome. Genome Biol. 2015;16:211.
Smallwood T, Allayee H, Bennett BJ. Choline metabolites: gene by diet interactions. Curr Opin Lipidol. 2016;27:33–39.
German AJ, Holden SL, Serisier S, Queau Y, Biourge V. Assessing the adequacy of essential nutrient intake in obese dogs undergoing energy restriction for weight loss: a cohort study. BMC Vet Res. 2015;11:253.
Paul B, Barnes S, Demark-Wahnefried W, et al. Influences of diet and the gut microbiome on epigenetic modulation in cancer and other diseases. Clin Epigenetics. 2015;7:112.
Choi KC, Jung MG, Lee YH, et al. Epigallocatechin-3-gallate, a histone acetyltransferase inhibitor, inhibits EBV-induced B lymphocyte transformation via suppression of RelA acetylation. Cancer Res. 2009;69:583–592.
Lee YH, Kwak J, Choi HK, et al. EGCG suppresses prostate cancer cell growth modulating acetylation of androgen receptor by anti-histone acetyltransferase activity. Int J Mol Med. 2012;30:69–74.
Le Roy T, Llopis M, Lepage P, et al. Intestinal microbiota determines development of Nonalcoholic fatty liver disease in mice. Gut. 2013;62:1787–1794.
Macfarlane S, Macfarlane GT. Regulation of short-chain fatty acid production. Proc Nutr Soc. 2003;62:67–72.
Remely M, Aumueller E, Merold C, et al. Effects of short chain fatty acid producing bacteria on epigenetic regulation of FFAR3 in type 2 diabetes and obesity. Gene. 2014;537:85–92.
Canani RB, Costanzo MD, Leone L, Pedata M, Meli R, Calignano A. Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J Gastroenterol. 2011;17:1519–1528.
Walker AK, Jacobs RL, Watts JL, et al. A conserved SREBP-1/phosphatidylcholine feedback circuit regulates lipogenesis in metazoans. Cell. 2011;147:840–852.
Oster M, Nuchchanart W, Trakooljul N, et al. Methylating micronutrient supplementation during pregnancy influences foetal hepatic gene expression and IGF signalling and increases foetal weight. Eur J Nutr. 2016;55:1717–1727.
Yamada K, Gherasim C, Banerjee R, Koutmos M. Structure of human B12 trafficking protein CblD reveals molecular mimicry and identifies a new subfamily of nitro-FMN reductases. J Biol Chem. 2015;290:29155–29166.
Mischke M, Plosch T. More than just a gut instinct-the potential interplay between a baby’s nutrition, its gut microbiome, and the epigenome. Am J Physiol Regul Integr Comp Physiol. 2013;304:R1065–R1069.
Kellermayer R, Dowd SE, Harris RA, et al. Colonic mucosal DNA methylation, immune response, and microbiome patterns in Toll-like receptor 2-knockout mice. FASEB J. 2011;25:1449–1460.
Takahashi K. Influence of bacteria on epigenetic gene control. Cell Mol Life Sci. 2014;71:1045–1054.
Takahashi K, Sugi Y, Nakano K, et al. Epigenetic control of the host gene by commensal bacteria in large intestinal epithelial cells. J Biol Chem. 2011;286:35755–35762.
Dapito DH, Mencin A, Gwak GY, et al. Promotion of hepatocellular carcinoma by the intestinal microbiota and TLR4. Cancer Cell. 2012;21:504–516.
Kumar H, Lund R, Laiho A, et al. Gut microbiota as an epigenetic regulator: pilot study based on whole-genome methylation analysis. MBio. 2014;5:e02113–e02114.
Nakajima T, Enomoto S, Yamashita S, et al. Persistence of a component of DNA methylation in gastric mucosae after Helicobacter pylori eradication. J Gastroenterol. 2010;45:37–44.
Kiga K, Mimuro H, Suzuki M, et al. Epigenetic silencing of miR-210 increases the proliferation of gastric epithelium during chronic Helicobacter pylori infection. Nat Commun. 2014;5:4497.
Maekita T, Nakazawa K, Mihara M, et al. High levels of aberrant DNA methylation in Helicobacter pylori-infected gastric mucosae and its possible association with gastric cancer risk. Clin Cancer Res. 2006;12:989–995.
Cortese R, Lu L, Yu Y, Ruden D, Claud EC. Epigenome-microbiome crosstalk: a potential new paradigm influencing neonatal susceptibility to disease. Epigenetics. 2016;11:205–215.
van’t Slot G, Humpf HU. Degradation and metabolism of catechin, epigallocatechin-3-gallate (EGCG), and related compounds by the intestinal microbiota in the pig cecum model. J Agric Food Chem. 2009;57:8041–8048.
Rungapamestry V, Rabot S, Fuller Z, Ratcliffe B, Duncan AJ. Influence of cooking duration of cabbage and presence of colonic microbiota on the excretion of N-acetylcysteine conjugates of allyl isothiocyanate and bioactivity of phase 2 enzymes in F344 rats. Br J Nutr. 2008;99:773–781.
Ciarlo E, Heinonen T, Herderschee J, et al. Impact of the microbial derived short chain fatty acid propionate on host susceptibility to bacterial and fungal infections in vivo. Sci Rep. 2016;6:37944.
Hichino A, Okamoto M, Taga S, et al. Down-regulation of claudin-2 expression and proliferation by epigenetic inhibitors in human lung adenocarcinoma A549 cells. J Biol Chem. 2017;292:2411–2421.
Haldar S, Dru C, Mishra R, et al. Histone deacetylase inhibitors mediate DNA damage repair in ameliorating hemorrhagic cystitis. Sci Rep. 2016;6:39257.
Arpaia N, Campbell C, Fan X, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature. 2013;504:451–455.
Wostmann BS, Larkin C, Moriarty A, Bruckner-Kardoss E. Dietary intake, energy metabolism, and excretory losses of adult male germfree Wistar rats. Lab Anim Sci. 1983;33:46–50.
Schwiertz A, Taras D, Schafer K, et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring). 2010;18:190–195.
Li G, Su H, Zhou Z, Yao W. Identification of the porcine G protein-coupled receptor 41 and 43 genes and their expression pattern in different tissues and development stages. PLoS ONE. 2014;9:e97342.
Andrade-Oliveira V, Amano MT, Correa-Costa M, et al. Gut bacteria products prevent AKI induced by ischemia–reperfusion. J Am Soc Nephrol. 2015;26:1877–1888.
Singh N, Thangaraju M, Prasad PD, et al. Blockade of dendritic cell development by bacterial fermentation products butyrate and propionate through a transporter (Slc5a8)-dependent inhibition of histone deacetylases. J Biol Chem. 2010;285:27601–27608.
Davie JR. Inhibition of histone deacetylase activity by butyrate. J Nutr. 2003;133:2485S–2493S.
Cousens LS, Gallwitz D, Alberts BM. Different accessibilities in chromatin to histone acetylase. J Biol Chem. 1979;254:1716–1723.
Bernhard D, Ausserlechner MJ, Tonko M, et al. Apoptosis induced by the histone deacetylase inhibitor sodium butyrate in human leukemic lymphoblasts. FASEB J. 1999;13:1991–2001.
Gozzini A, Rovida E, Dello Sbarba P, Galimberti S, Santini V. Butyrates, as a single drug, induce histone acetylation and granulocytic maturation: possible selectivity on core binding factor-acute myeloid leukemia blasts. Cancer Res. 2003;63:8955–8961.
Finzer P, Stohr M, Seibert N, Rosl F. Phenylbutyrate inhibits growth of cervical carcinoma cells independent of HPV type and copy number. J Cancer Res Clin Oncol. 2003;129:107–113.
Kuefer R, Hofer MD, Altug V, et al. Sodium butyrate and tributyrin induce in vivo growth inhibition and apoptosis in human prostate cancer. Br J Cancer. 2004;90:535–541.
Yu C, Subler M, Rahmani M, et al. Induction of apoptosis in BCR/ABL + cells by histone deacetylase inhibitors involves reciprocal effects on the RAF/MEK/ERK and JNK pathways. Cancer Biol Ther. 2003;2:544–551.
Wei W, Sun W, Yu S, Yang Y, Ai L. Butyrate production from high-fiber diet protects against lymphoma tumor. Leuk Lymphoma. 2016;57:2401–2408.
Chang PV, Hao L, Offermanns S, Medzhitov R. The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc Natl Acad Sci USA. 2014;111:2247–2252.
Yu DC, Waby JS, Chirakkal H, Staton CA, Corfe BM. Butyrate suppresses expression of neuropilin I in colorectal cell lines through inhibition of Sp1 transactivation. Mol Cancer. 2010;9:276.
Khan S, Jena G. The role of butyrate, a histone deacetylase inhibitor in diabetes mellitus: experimental evidence for therapeutic intervention. Epigenomics. 2015;7:669–680.
Rao P, Hayden MS, Long M, et al. IkappaBbeta acts to inhibit and activate gene expression during the inflammatory response. Nature. 2010;466:1115–1119.
Tay S, Hughey JJ, Lee TK, Lipniacki T, Quake SR, Covert MW. Single-cell NF-kappaB dynamics reveal digital activation and analogue information processing. Nature. 2010;466:267–271.
Wang KS, Li J, Wang Z, et al. Artemisinin inhibits inflammatory response via regulating NF-kappaB and MAPK signaling pathways. Immunopharmacol Immunotoxicol. 2017;39:28–36.
Liu W, Sun Y, He Y, et al. IL-1beta impedes the chondrogenic differentiation of synovial fluid mesenchymal stem cells in the human temporomandibular joint. Int J Mol Med. 2016;39:317–326.
Wang B, Liao PP, Liu LH, Fang X, Li W, Guan SM. Baicalin and geniposide inhibit the development of atherosclerosis by increasing Wnt1 and inhibiting dickkopf-related protein-1 expression. J Geriatr Cardiol. 2016;13:846–854.
Yang JX, Pan YY, Ge JH, et al. Tanshinone II A attenuates TNF-alpha-induced expression of VCAM-1 and ICAM-1 in endothelial progenitor cells by blocking activation of NF-kappaB. Cell Physiol Biochem. 2016;40:195–206.
Chang X, Zhu A, Liu F, et al. Role of NF-kappaB activation and Th1/Th2 imbalance in pulmonary toxicity induced by nano NiO. Environ Toxicol. 2016;32:1354–1362.
Deng QW, Yang H, Yan FL, et al. Blocking sympathetic nervous system reverses partially stroke-induced immunosuppression but does not aggravate functional outcome after experimental stroke in rats. Neurochem Res. 2016;41:1877–1886.
He YW, Wang HS, Zeng J, et al. Sodium butyrate inhibits interferon-gamma induced indoleamine 2,3-dioxygenase expression via STAT1 in nasopharyngeal carcinoma cells. Life Sci. 2013;93:509–515.
Gao Z, He Q, Peng B, Chiao PJ, Ye J. Regulation of nuclear translocation of HDAC3 by IkappaBalpha is required for tumor necrosis factor inhibition of peroxisome proliferator-activated receptor gamma function. J Biol Chem. 2006;281:4540–4547.
Hase K, Murakami M, Iimura M, et al. Expression of LL-37 by human gastric epithelial cells as a potential host defense mechanism against Helicobacter pylori. Gastroenterology. 2003;125:1613–1625.
Schauber J, Svanholm C, Termen S, et al. Expression of the cathelicidin LL-37 is modulated by short chain fatty acids in colonocytes: relevance of signalling pathways. Gut. 2003;52:735–741.
Steinmann J, Halldorsson S, Agerberth B, Gudmundsson GH. Phenylbutyrate induces antimicrobial peptide expression. Antimicrob Agents Chemother. 2009;53:5127–5133.
Imai K, Ochiai K, Okamoto T. Reactivation of latent HIV-1 infection by the periodontopathic bacterium Porphyromonas gingivalis involves histone modification. J Immunol. 2009;182:3688–3695.
Haller D, Holt L, Kim SC, Schwabe RF, Sartor RB, Jobin C. Transforming growth factor-beta 1 inhibits non-pathogenic Gram negative bacteria-induced NF-kappa B recruitment to the interleukin-6 gene promoter in intestinal epithelial cells through modulation of histone acetylation. J Biol Chem. 2003;278:23851–23860.
Ghadimi D, Helwig U, Schrezenmeir J, Heller KJ, de Vrese M. Epigenetic imprinting by commensal probiotics inhibits the IL-23/IL-17 axis in an in vitro model of the intestinal mucosal immune system. J Leukoc Biol. 2012;92:895–911.
Schmeck B, Beermann W, van Laak V, et al. Intracellular bacteria differentially regulated endothelial cytokine release by MAPK-dependent histone modification. J Immunol. 2005;175:2843–2850.
Opitz B, Puschel A, Beermann W, et al. Listeria monocytogenes activated p38 MAPK and induced IL-8 secretion in a nucleotide-binding oligomerization domain 1-dependent manner in endothelial cells. J Immunol. 2006;176:484–490.
Hamon MA, Cossart P. K+ efflux is required for histone H3 dephosphorylation by Listeria monocytogenes listeriolysin O and other pore-forming toxins. Infect Immun. 2011;79:2839–2846.
Xia G, Schneider-Stock R, Diestel A, et al. Helicobacter pylori regulates p21(WAF1) by histone H4 acetylation. Biochem Biophys Res Commun. 2008;369:526–531.
Acknowledgments
We thank Haiyang Hu for figure preparation. This study was supported by the Key Program of the National Natural Science Foundation of China (No. 81330011) and the National Basic Research Program of China (973 Program) (No. 2013CB531401).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ye, J., Wu, W., Li, Y. et al. Influences of the Gut Microbiota on DNA Methylation and Histone Modification. Dig Dis Sci 62, 1155–1164 (2017). https://doi.org/10.1007/s10620-017-4538-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4538-6