Abstract
While simple to recommend, diet and lifestyle measures as a first-line therapy for nonalcoholic steatohepatitis (NASH) are hardly a model of successful therapy, as most clinicians can testify. They can be complex to implement, hard to sustain, and of limited efficacy in advanced stages of the disease. The need for specific pharmacotherapy is now acknowledged by practitioners, the pharmaceutical industry, and regulators and is largely expected by patients. The result is a clear move away from products developed second hand for NASH (such as pioglitazone or metformin) or from generic, non-specific hepatoprotectors (such as pentoxifylline, ursodeoxycholic acid, or antioxidants) toward molecules developed and tested specifically for NASH that aim to correct one or several of the pathways of liver injury in this disease. The two most advanced molecules, obeticholic acid and elafibranor, have shown encouraging data on improving hepatic histology. Both compounds appear to clear NASH, with obeticholic acid improving liver fibrosis and elafibranor improving the glycemic and lipid profile. Much larger trials, currently ongoing, will need to confirm these preliminary data and better characterize the safety and tolerability profile. Meanwhile, other compounds are being tested, a few in phase 2b studies (cenicriviroc, aramchol for NASH, and simtuzumab for NASH fibrosis) and many more in earlier, smaller trials. Most of these drug candidates target different pathways, which speaks to the diversity and dynamism of the NASH pipeline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nonalcoholic steatohepatitis (NASH) is becoming the leading cause of chronic liver disease and a major health issue owing to its close association with the worldwide epidemics of obesity and diabetes [1]. A significant proportion of patients can experience disease progression with the occurrence of cirrhosis, hepatocellular carcinoma, and end-stage liver disease [2]. This results in an increase in the overall and liver-related mortality [3, 4]. Patients at risk of disease progression need to be identified as not all individuals with metabolic risk factors will experience disease progression [5]. Prognostic markers have mostly been derived from histological studies and found that the degree of inflammation is the strongest and independent predictor for fibrosis progression [6].
Is There a Need for Pharmacological Therapy?
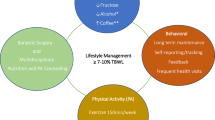
As NASH is a disease that is closely linked to overweight and resulting insulin resistance, the need for pharmacological therapy has been questioned. The mere correction of the predisposing condition through diet and lifestyle measures could be deemed sufficient for treating the ensuing hepatic disease. Weight loss not only corrects the underlying condition that promoted the occurrence of NASH but also improves liver injury itself [7, 8]. Reports from bariatric surgery provided the proof of principle that massive and gradual weight loss improves steatosis and inflammation, clears steatohepatitis, and reverses fibrosis, occasionally even at the cirrhotic stage [9, 10]. Dietary changes and lifestyle modifications are therefore the first-line therapy for patients with NASH. Unfortunately, in many patients, these measures cannot be implemented efficiently or maintained in the long run. Also, many NASH patients have already tried diet and lifestyle modifications repeatedly but unsuccessfully before being referred to the hepatologist. Others have advanced liver disease that would warrant targeted therapy in addition to the treatment of the underlying condition. For these reasons, pharmacological options should be made available at least for some patients with NASH.
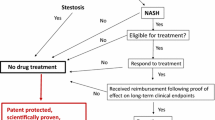
Who Should Be Treated with Pharmacological Agents?
Pharmacological therapy for NASH should be restricted to those individuals with advanced liver disease or at high risk of progression to cirrhosis [11, 12]. Similar to other chronic liver diseases, advanced liver disease can be defined by advanced (i.e., bridging) fibrosis or cirrhosis. What defines high risk of progression is less consensual. Studies with sequential liver biopsies have shown that necroinflammation is the best predictor of progression to fibrosis, a finding corroborated by numerous observations showing that steatohepatitis, and not steatosis, can progress toward advanced liver disease [13]. Thus, patients with NASH and marked hepatocyte injury (ballooning) and inflammation could have a higher risk of disease progression, especially if they already have a moderate amount of fibrosis (perisinusoidal and portal fibrosis) and clinical risk factors for fibrosis, such as age >50 years, male sex, and type 2 diabetes. At the opposite end of the spectrum, patients with isolated steatosis or steatosis and non-specific inflammation are considered at very low risk of fibrosis progression. These patients are not candidates for pharmacological therapy that specifically targets the liver condition.
What Are the Relevant Pharmacological Targets?
Our current understanding of the pathophysiology of NASH is that excessive fat accumulation coexisting with overweight, particularly when localized to visceral adipose tissue, promotes insulin resistance. Uninhibited lipolysis, a consequence of insulin resistance, increases delivery of free fatty acids to the liver [14]. In addition, hyperinsulinemia and the subsequent increase in serum glucose will enhance a maladaptive hepatic lipogenic response and inhibit lipid disposal through beta-oxidation [15]. The resulting increase in intrahepatic flux of numerous lipid species promotes liver damage through multiple lipocytotxic pathways: oxidative stress, mitochondrial dysfunction, apoptosis, free cholesterol toxicity, and endoplasmic reticulum stress [16]. The resulting cell injury and accompanying inflammation (part of which is modulated by cross talk with the inflamed adipose tissue) sets the stage, in the long run, for liver fibrosis to occur.
This brief description suggests that the relevant mechanisms of action for NASH drugs could be: (1) weight loss agents; (2) insulin sensitizers; (3) antidiabetic drugs with antihyperglycemic properties; (4) hepatoprotectants with broad antiinflammatory properties; and (5) antifibrotic drugs. These drugs can therefore be classified into two broad categories: drugs that improve the underlying metabolic conditions that promoted the emergence of NASH and hepatoprotectants that specifically target the mechanisms of hepatic cell injury. As some pathways can be involved in both hepatic inflammation and insulin resistance, some drugs might belong to both categories. Alternatively, combination therapy with molecules that act on distinct metabolic and hepatoprotective pathways could also be envisioned. Depending on how vast the NASH drug pipeline will be, tailored therapy for particular patients could thus become a reality in the near future.
Where Do We Stand with Pharmacological Therapies?
An ideal drug candidate for NASH should reduce hepatic inflammation and liver cell injury, should correct the underlying insulin resistance, and should have antifibrotic effects. However, primarily “anti-NASH” drugs that have no direct antifibrotic effect could, theoretically, result in a subsequent reduction in fibrosis if a sustained resolution of NASH is achieved. Conversely, purely antifibrotic drugs with no anti-NASH activity and no interference with insulin resistance will leave the triggers for fibrogenesis intact. Therefore, even if an antifibrotic is effective, efforts to curb the underlying pro-fibrotic condition must be considered [11]. We will here review some of the novel anti-NASH agents that are now in late stages of drug development. Many other agents are in preclinical phases of development or in early human studies and will not be reviewed here. These agents that target fibrotic pathways, hepatic lipogenesis, endothelial adhesion molecules, apoptosis, miRNA, endotoxin, nuclear receptors, among others, are part of a very diverse and rich pipeline for NASH.
FXR Agonists and Obeticholic Acid
Recent discoveries have identified bile acids as key regulators of liver and metabolic homeostasis. Their action is mediated through nuclear hormone receptors such as the farnesoid X receptor (FXR) and TGR5 [17]. FXR activation results primarily in a reduction in bile acid synthesis from cholesterol by altering expression of a host of genes but mainly by downregulating CYP7A1 [18]. This limits the size of the circulating bile acid pool and promotes choleresis, thus protecting against the toxic accumulation of bile acids. Obeticholic acid (OCA), a first-in-class FXR agonist, is a synthetic bile acid with picomolar agonistic activity on FXR [18]. The bile acid effects have translated into clinical efficacy in patients with primary biliary cirrhosis [19] with a reduction in phosphatase alkaline, a biochemical surrogate for clinical events in the natural history of the disease [20]. Based on these results, it is expected that OCA will be approved for this indication. FXR activation also has a wide range of metabolic effects: inhibition of hepatic neoglucogenesis and hepatic glucose production, reduction in lipogenesis, enhancement of beta-oxidation, and improvement in peripheral insulin sensitivity [21]. Interestingly, FXR activation has also antiinflammatory actions [22] with resultant protection against liver inflammation and fibrosis in experimental models of NASH [23].
A small randomized trial in type 2 diabetic patients with NAFLD showed an improvement in hepatic and muscle insulin sensitivity as measured by the euglycemic clamp, a modest but dose-related weight loss, and a reduction in ALT levels [24]. This study provided the proof of principle of an improvement in insulin sensitivity and possibly NAFLD in humans. It was followed by a much larger trial that tested the oral administration of 25 mg OCA QD versus placebo over 72 weeks of therapy in non-cirrhotic NASH patients [25]. The therapeutic phase of the FLINT trial was stopped early, partly because a preplanned interim analysis showed improved histology in more patients on OCA than on placebo (45 vs. 21 %). The primary endpoint was a two-point reduction in the composite nonalcoholic fatty liver disease score (NAS) without worsening of fibrosis. However, beyond this composite endpoint, OCA was able to significantly improve all histological lesions constitutive of NASH including liver fibrosis. Although the trial was not designed for fibrotic endpoints, there was a significant reduction in the fibrosis score (one stage) in 35 % of OCA-treated patients versus 19 % in the placebo arm. The reduction in fibrosis was observed regardless of the baseline fibrosis stage. The study included patients at high risk of progression (half of the participants had type 2 diabetes) and “non-responders” to vitamin E (20 %). The primary endpoint was reached in secondary analyses of all subgroups of patients. There was a trend in favor of a higher rate of resolution of NASH in the OCA group (22 vs. 13 % in the placebo group) which became significant (19 vs. 8 %, p < 0.05) in a subgroup analysis restricted to patients with well-characterized NASH at baseline. All these data are very encouraging but need to be confirmed in much larger trials as the FLINT trial only included 110 patients per arm. As far as safety and tolerability two issues emerged: pruritus and an increase in LDL cholesterol. Pruritus occurred in 23 % of OCA-treated patients versus 6 % in the placebo group, but discontinuation was very rare (only one patient). It is, however, a concern as the NASH population is overwhelmingly asymptomatic. Further studies will test whether lower doses of OCA reduce the incidence of pruritus. An increase in LDL cholesterol occurred early on therapy, plateaued with continued therapy, and then reversed once the drug was discontinued. Post hoc analyses showed that statins, when initiated during the trial, were able to mitigate the excursion in LDL. Future studies are needed to better characterize alterations in lipid profile and to determine whether this results in an increase in cardiovascular risk, if any. Interestingly, in animal models of atherosclerosis, FXR agonists reduce atherosclerosis and vascular cholesterol load and inflammation. OCA is a very promising molecule for the treatment of NASH, and a large phase 3 trial, the REGENERATE trial (NCT02548351), is ongoing. It is not yet known whether OCA will be effective at the cirrhotic stage. Animal data have shown that in rodents, OCA reduces bacterial translocation by increasing the expression of intestinal tight junction proteins which resulted in a normalization of the endotoxin-TLR4 signaling [26]. Other studies have shown that OCA can reduce the intrahepatic vascular resistance and improving endothelial vasorelaxation by restoring hepatic e-NOS activity [27]. This suggests beneficial effects on portal hypertension which together with reduced risk of infections due to reduced bacterial translocation could result into clinical benefit in cirrhotic patients. This hypothesis will be tested in future trials in cirrhotic patients.
PPAR Alpha/Delta Agonists and Elafibranor
Another innovative insulin sensitizer is elafibranor, a dual PPARα/δ agonist. PPARs (α, β, and γ) are fatty acid-activated nuclear receptors that have a wide range of physiological actions. PPARδ activation emerged as a potent metabolic regulator that induces hepatic fatty acid β-oxidation, inhibits hepatic lipogenesis [28], reduces hepatic glucose production, and improves hepatic inflammation [29, 30]. PPARα is a major regulator of fatty acid disposal through mitochondrial beta-oxidation, but also has antiinflammatory actions as it inhibits inflammatory genes induced by NF-kB and acute phase response genes induced by IL6 [31]. Combining these two modes of action can thus improve many of the pathways of injury involved in NASH. Animal data confirmed the hepatoprotective effects of GFT505 in dietary models of NASH or fibrosis with, in particular, a reduction in steatosis, hepatic inflammation, and pro-inflammatory genes [32]. Importantly, this compound exhibited antifibrotic properties in fibrosis models that were independent of metabolic and insulin resistance abnormalities [32], thereby suggesting a universal antifibrotic potency in rodents. Elafibranor is a PPAR modulator with preferential activity on PPARα and additional activity on PPARδ, but no PPARγ actions [33]. It undergoes extensive enterohepatic cycling and is liver targeted with little or no muscle action [34]. Human studies performed in abdominally obese, insulin-resistant patients, with or without diabetes, have shown that GFT505 improves hepatic and peripheral insulin sensitivity, dyslipidemia, inflammatory markers, and liver function tests [33, 35].
The results of a large, international, phase IIb trial, the GOLDEN505 trial, have been reported [36]. In this randomized trial, 274 NASH patients received elafibranor 80, 120 mg/day, or placebo for 1 year. While the lower, 80 mg dose did not improve histology, the higher dose was more effective than placebo at inducing NASH resolution without fibrosis worsening. The optimal definition for this histological outcome is still under debate, but these positive results were obtained with a modified, more stringent definition that is consensually emerging. There was no effect on fibrosis (1-year trial duration only) although patients who cleared steatohepatitis (responders) had an improvement in fibrosis after 1 year of therapy, while non-responders did not. This validates the concept that resolution of NASH will be followed by a reversal of fibrosis, a cornerstone of the current surrogate endpoints used in drug development. As anticipated from earlier phase 2 trials, elafibranor improved lipid parameters, glucose homeostasis, and insulin sensitivity as well as systemic inflammatory markers. Remarkably, the cardiometabolic improvement was achieved on top of standard of practice management of the comorbidities in these patients with metabolic syndrome. The drug was well tolerated although a few patients had an increase in creatinine, which was reversible after discontinuation of elafibranor. The increase was less than that observed with fibrates, and similarly to fibrates, it is not expected to be associated with renal insufficiency. This promising molecule needs to be tested in large, phase 3 trials.
Chemokines and Cenicriviroc
Chemokines are chemotactic cytokines specialized in leukocyte recruitment at sites of tissue injury, inflammation, and fibrosis. Chemokines and their receptors form a complex network of redundant ligand complex binding as one receptor may bind different chemokines, but their overall effect is the promotion of local inflammatory and fibrotic response [37]. CCL2 (a.k.a. monocyte chemoattractant protein-1, MCP1) and CCL5 (RANTES) are particularly involved in liver and adipose tissue inflammation and hepatic fibrosis [38–40]. Cenicriviroc (CVC) is a selective inhibitor of CCR2 and CCR5 with nanomolar potency. It was developed initially as an anti-HIV agent as CVC blocks the use of CCR5 as a co-receptor for entry into host cells by HIV. CVC blocks the binding of MCP-1 to CCR2 and of RANTES, macrophage inflammatory protein-1α (MIP-1α), and MIP-1β to CCR5. There is a strong rationale for the use of CVC in NASH. CVC decreases recruitment, migration, and infiltration of pro-inflammatory monocytes to the site of liver injury mainly via CCR2 antagonism, thereby having the potential to reduce chronic liver inflammation. CVC also disrupts co-receptor and cytokine signaling pathways or “cross talk” of intrahepatic immune cells within the inflamed liver via CCR2 and CCR5 antagonism, resulting in decreased Kupffer cell and hepatic stellate cell activation and migration, and therefore reduced fibrogenesis. CVC demonstrated significant antifibrotic effects in diet-induced (mouse model of NASH with streptozotocin and high-fat diet [41]) and chemically induced (rat thioacetamide [TAA] [42]) models of liver fibrosis, as well as in a model of kidney fibrosis. It also reduced lobular inflammation and hepatocyte ballooning in the dietary NASH model. Studies in up to 48 weeks in HIV-infected individuals did not show any safety concern.
Currently, a large randomized phase 2b trial in NASH, the CENTAUR trial (NCT02217475), is ongoing. This trial tests CVC versus placebo over a 2-year period in patients with fibrotic NASH or NASH at high risk of progression [43]. An interim histological analysis at year one will be performed and will allow to understand the benefit of short-term versus prolonged exposure to cenicriviroc both on NASH and on fibrosis.
Fatty Acid–Bile Acid Conjugates and Aramchol
Aramchol is a first-in-class, novel synthetic small molecule produced by conjugating two natural components, a fatty acid, arachidic acid, and a bile acid, cholic acid linked by a stable amide bond. It was initially synthesized to treat gallstones as the saturated fatty acid has cholesterol-solubilizing properties and the bile acid enabled secretion into the bile and entry into the enterohepatic circulation [44]. However, empirical observations of animals fed a high-fat, lithogenic diet documented a strong reduction in liver fat that occurred much earlier than did gallstone dissolution [45]. The antisteatogenic mechanism is probably related to the inhibition of stearoyl-CoA desaturase-1 (SCD1) activity well documented in human liver [46]. This results in decreased synthesis of monounsaturated fatty acids and of triglyceride stores. Moreover, aramchol activates cholesterol efflux by stimulating the ABCA1 transporter, a universal cholesterol efflux pump [47] which can explain the antiatherogenic effects in some animal models [46]. Since liver-specific SCD1 inhibition in rodents reversed hepatic insulin resistance and reduced neoglucogenesis [48], several SCD1 inhibitors were tested as a treatment of diet-induced metabolic complications. However, systemic inhibition of SCD1 resulted in severe skin and eye side effects, and most of them have been discontinued [49]. Aramchol does not induce these side effects possibly because of the liver targeting or the partial and not complete inhibition of SCD1. A small phase 2a study performed in patients with biopsy documented NAFLD tested two doses of aramchol versus placebo over a 3-month period and did not raise any significant safety concern [50]. The higher, 300 mg daily, dose resulted in significant reduction in liver fat as measured by magnetic resonance spectroscopy (MRS). There was also a trend toward an increase in serum adiponectin and an improvement in flow mediated dilation [50], an early marker of endothelial dysfunction in patients with NASH [51].
A large international phase 2b trial is ongoing in patients with histologically documented NASH, high liver fat content measured by MRS, and several features of the metabolic syndrome (NCT 02279524). This trial of one-year duration tests still higher doses of daily aramchol, 400 and 600 mg. The main endpoint is a reduction in liver fat content measured by MRS and histological improvement as secondary endpoints.
Incretin Mimetics and Liraglutide
Among existing therapies for type 2 diabetes, incretin mimetics which are glucagon-like peptide-1 receptor (GLP-1R) agonists hold promise for the treatment of NASH. GLP-1, a peptide product of the L cells of the small intestine and proximal colon, stimulates insulin secretion from the β cells and inhibits glucagon secretion from the α cells in a glucose-dependent manner [52]. GLP-1 also enhances satiety and delays gastric emptying [52]. However, because of their short half-life due to rapid degradation by specific enzymes (such as dipeptidyl peptidase, DPP-IV), native GLP-1 cannot be used as a pharmacological agent. GLP-1R agonists have a much longer half-life than natural GLP-1 allowing either a daily or a once-weekly administration [53]. There seems to be some controversy over the presence of receptors for GLP-1 in hepatocytes and stellate cells. Some studies have shown the presence of a cognate receptor for GLP-1 on human hepatocytes [54]; signaling through these receptors improves hepatic insulin sensitivity [55] by inducing phosphorylation of key signaling pathways [54]. GLP-1 R binding in hepatocytes results in an induction of PPARα and γ expression, which increases disposal of hepatocyte fatty acids by beta-oxidation and lipid export [55, 56]. In vivo studies have confirmed an antisteatogenic effect of exendin in mice [55, 57]. Several potentially beneficial effects have been demonstrated in humans by metabolic studies including the euglycemic clamp: Patients with NAFLD had decreased de novo lipogenesis, decreased adipose tissue lipolysis, and reduced hepatic glucose production upon administration of 1.8 mg liraglutide daily [58]. Moreover, because it induces weight loss, liraglutide at the dose of 3 mg/day [59] is now approved for treatment of obesity or overweight with comorbidities. Other GLP1-R agonists are approved for glycemic control in diabetic patients.
Data from large registration trials have shown that diabetic patients treated with liraglutide improved ALT levels and possibly steatosis, measured by CT scan imaging [60]. Taken together, all the above data form a compelling rationale for testing liraglutide in patients with NASH. A British study randomized 52 NASH patients and analyzed 23 of them treated with liraglutide, 1.8 mg/day, and 22 with placebo, in a randomized controlled trial of a 1-year duration [61]. Patients treated with liraglutide experienced more often reversal of NASH (39 vs. 9 %, p < 0.02) and less often progression of fibrosis. There was no significant effect on lobular inflammation and ALT and only a marginally significant effect on hepatocyte ballooning, an indication of the very small sample size of this trial. Hence, these results, although encouraging, especially in the light of the preclinical data and the weight loss effect, clearly need further confirmation before any recommendations can be made.
Antifibrotic Agents: Simtuzumab and Galectin-3 Inhibitors
Since the overall objective when treating NASH patients is to reduce the progression to cirrhosis, antifibrotic drugs that would specifically block liver fibrosis would be an important addition to anti-NASH drugs. There are very few well-conducted trials of antifibrotic agents and those that are available are negative [62–65]. There are very few well-conducted trials of antifibrotic agents and those that are available are negative. Lysyl oxidase and lysyl oxidase like (LOXL) are a family of enzymes expressed and secreted by fibrogenic cells and catalyze oxidative deamination of lysyl and hydroxylysine residues in collagen precursors and elastin [66]. This results in covalent cross-linking of the extracellular matrix, a phenomenon that is believed to greatly contribute to the deposition and stabilization of the hepatic scar [67]. LOXL2, a member of the LOXL family, is upregulated in hepatocytes, and its expression is correlated with collagen deposition in various hepatic fibrotic diseases [68] including steatohepatitis in humans [69]. LOXL2 regulates fibroblast activation, TGF-β signaling, and latent TGF-β activation [69]. Experimental studies have shown that inhibition of LOXL2 with an inhibitory monoclonal antibody results in a reduction in liver and lung fibrosis [69]. Simtuzumab is a humanized monoclonal IgG4 antibody with a long half-life of 10–20 days and can be administered either IV or subcutaneously. It is currently tested in two large, 2-year phase 2b clinical trials in patients with NASH and bridging fibrosis and cirrhotic NASH (NCT01672866 and NCT01672879, respectively). The main endpoint of the non-cirrhotic trial is a reduction in the area of fibrosis assessed by micromorphometry, while that of the cirrhotic study is a reduction in hepatic venous pressure gradient. Both studies are followed by several year extension periods for clinical outcomes.
Galectins are a family of proteins that bind to galactose residues present on glycoproteins from extracellular matrix components (collagens, laminin, fibronectin, integrins, elastin) but also on cell surface proteins such as CD4, CD8, or TGF-beta receptors [70]. Galectin-3, a member of the galectin family expressed at high levels on macrophages, regulates multiple cellular processes including cell adhesion and migration, immune cell function, and inflammation [71]. It is upregulated in hepatic human fibrosis and promotes fibrosis in vitro and in vivo [72]. GR-MD-02, a complex polysaccharide polymer (a galactoarabino-rhamnogalacturonan) is a pharmacological inhibitor of galectin-3 that reduces liver fibrosis and portal hypertension in a thioacetamide model of fibrosis/cirrhosis [73]. The antifibrotic effects were confirmed in a dietary NASH model in diabetic mice where GR-MD-02 prevented accumulation of collagen and reduced stellate cell activation [74]. Remarkably, the drug also improved hepatocyte ballooning and lobular inflammation and reduced fat accumulation; these anti-NASH effects are probably related to a reduction in iNOS, a marker of inflammation, and in CD-36 expressing pro-inflammatory macrophages [74]. A phase I dose-ranging study has shown good safety and tolerability in humans receiving this compound intravenously (NCT01899859). A larger, phase 2a study in NASH patients with cirrhosis and portal hypertension testing intravenous infusions of GR-MD-02 every 2 weeks for 1 year is ongoing (NCT 02462967).
Conclusion
Drug development for NASH has accelerated strongly over the past few years. Earlier studies such as the PIVENS trial have provided the proof of principle that histological improvement and even NASH resolution is possible with drugs such as insulin sensitizers (glitazones) or antioxidants (vitamin E) [75]. Retrospective studies have documented the prognostic significance of histological lesions in NAFLD [76, 77], suggesting that these lesions could be acceptable surrogates of disease control on therapy. Tools for a precise histological description and classification have been refined from the NASH CRN classification [78] to the FLIP/SAF algorithm [79]. Major advances also occurred in the regulatory field. Both the European and the American drug agencies now agree that NASH is a valid indication for therapy and as such it can follow a regulatory path for drug approval. Trial outcomes with clinical and regulatory value have been defined and are currently being used in several large trials of new drugs in NASH [11]. What remains to be done is the discovery and validation of biomarkers that would help diagnose patients at risk of advanced or progressive NASH but also monitor disease progression. Renewed and sustained efforts for drug discovery and dedication from physicians to recruit and complete clinical trials will be key to providing patients with NASH with safe and effective drugs in the near future.
Key Messages
-
NASH is now an established indication for therapy irrespective of the control of associated metabolic comorbidities. Patients with histologically confirmed steatohepatitis and fibrosis are candidates for pharmacotherapy, in association with diet and lifestyle modifications.
-
As current treatment options are limited, new and innovative pharmacological agents are being developed. Obeticholic acid and elafibranor are the most advanced drugs that induced resolution of NASH and for obeticholic acid, an overall improvement in fibrosis.
-
Many other drugs such as chemokine blockers, inhibitors of lipogenesis, and antifibrotics are in various stages of development.
-
New and effective pharmacological agents that improve insulin resistance but also hepatic inflammation and fibrosis need to be identified.
References
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American association for the study of liver diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55:2005–2023.
Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–285.
Ekstedt M, Franzen LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873.
Soderberg C, Stal P, Askling J, et al. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010;51:595–602.
Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53:372–384.
Argo CK, Northup PG, Al-Osaimi AM, Caldwell SH. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J Hepatol. 2009;51:371–379.
Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51:121–129.
Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149:367–378 e365; quiz e314–365.
Dixon JB, Bhathal PS, Hughes NR, O’Brien PE. Nonalcoholic fatty liver disease: improvement in liver histological analysis with weight loss. Hepatology. 2004;39:1647–1654.
Kral JG, Thung SN, Biron S, et al. Effects of surgical treatment of the metabolic syndrome on liver fibrosis and cirrhosis. Surgery. 2004;135:48–58.
Sanyal AJ, Friedman SL, McCullough AJ, Dimick-Santos L. Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: findings and recommendations from an American Association for the Study of Liver Diseases-U.S. Food and Drug Administration Joint Workshop. Hepatology. 2015;61:1392–1405.
Ratziu V, Goodman Z, Sanyal A. Current efforts and trends in the treatment of NASH. J Hepatol. 2015;62:S65–S75.
Ratziu V, Bellentani S, Cortez-Pinto H, Day CP, Marchesini G. A position paper on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53:372–384.
Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: pathophysiology and clinical implications Gastroenterology. 2012;142:711–725 e716.
Neuschwander-Tetri BA. Hepatic lipotoxicity and the pathogenesis of NASH: the central role of nontriglyceride fatty acid metabolites. Hepatology. 2010;52:774–788.
Peverill W, Powell LW, Skoien R. Evolving concepts in the pathogenesis of NASH: beyond steatosis and inflammation. Int J Mol Sci. 2014;15:8591–8638.
Schaap FG, Trauner M, Jansen PL. Bile acid receptors as targets for drug development. Nat Rev Gastroenterol Hepatol. 2014;11:55–67.
Adorini L, Pruzanski M, Shapiro D. Farnesoid X receptor targeting to treat nonalcoholic steatohepatitis. Drug Discov Today. 2012;17:988–997.
Hirschfield GM, Mason A, Luketic V, et al. Efficacy of obeticholic acid in patients with primary biliary cirrhosis and inadequate response to ursodeoxycholic acid. Gastroenterology. 2015;148:e758.
Lammers WJ, van Buuren HR, Hirschfield GM et al. Levels of alkaline phosphatase and bilirubin are surrogate end points of outcomes of patients with primary biliary cirrhosis: an international follow-up study Gastroenterology. 2014;147:1338–1349 e1335; quiz e1315.
Ma K, Saha PK, Chan L, Moore DD. Farnesoid X receptor is essential for normal glucose homeostasis. J Clin Invest. 2006;116:1102–1109.
Wang YD, Chen WD, Wang M, Yu D, Forman BM, Huang W. Farnesoid X receptor antagonizes nuclear factor kappaB in hepatic inflammatory response. Hepatology. 2008;48:1632–1643.
Zhang S, Wang J, Liu Q, Harnish DC. Farnesoid X receptor agonist WAY-362450 attenuates liver inflammation and fibrosis in murine model of non-alcoholic steatohepatitis. J Hepatol. 2009;51:380–388.
Mudaliar S, Henry RR, Sanyal AJ, et al. Efficacy and safety of the farnesoid X receptor agonist obeticholic acid in patients with type 2 diabetes and nonalcoholic fatty liver disease. Gastroenterology. 2013;145:574–582.
Neuschwander-Tetri BA, Loomba R, Sanyal AJ, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet. 2015;85:956–965.
Ubeda M, Lario M, Munoz L et al. Obeticholic acid reduces bacterial translocation, restores intestinal barrier and inhibits inflammation in cirrhotic rats J Hepatol. 2016;in press.
Verbeke L, Farre R, Trebicka J, et al. Obeticholic acid, a farnesoid X receptor agonist, improves portal hypertension by two distinct pathways in cirrhotic rats. Hepatology. 2014;59:2286–2298.
Qin X, Xie X, Fan Y, et al. Peroxisome proliferator-activated receptor-delta induces insulin-induced gene-1 and suppresses hepatic lipogenesis in obese diabetic mice. Hepatology. 2008;48:432–441.
Barish GD, Narkar VA, Evans RM. PPAR delta: a dagger in the heart of the metabolic syndrome. J Clin Invest. 2006;116:590–597.
Bojic LA, Huff MW. Peroxisome proliferator-activated receptor delta: a multifaceted metabolic player. Curr Opin Lipidol. 2013;24:171–177.
Pawlak M, Lefebvre P, Staels B. Molecular mechanism of PPARalpha action and its impact on lipid metabolism, inflammation and fibrosis in non-alcoholic fatty liver disease. J Hepatol. 2015;62:720–733.
Staels B, Rubenstrunk A, Noel B, et al. Hepatoprotective effects of the dual peroxisome proliferator-activated receptor alpha/delta agonist, GFT505, in rodent models of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Hepatology. 2013;58:1941–1952.
Cariou B, Zair Y, Staels B, Bruckert E. Effects of the new dual PPAR alpha/delta agonist GFT505 on lipid and glucose homeostasis in abdominally obese patients with combined dyslipidemia or impaired glucose metabolism. Diabetes Care. 2011;34:2008–2014.
Staels B, Rubenstrunk A, Noel B, et al. Hepato-protective effects of the dual PPARalpha/delta agonist GFT505 in rodent models of NAFLD/NASH. Hepatology. 2013;58:1941–1952.
Cariou B, Hanf R, Lambert-Porcheron S, et al. Dual peroxisome proliferator-activated receptor alpha/delta agonist GFT505 improves hepatic and peripheral insulin sensitivity in abdominally obese subjects. Diabetes Care. 2013;36:2923–2930.
Ratziu V, Harrison S, Franque S et al. Elafibranor, an agonist of the peroxisome proliferator-activated receptor alpha and delta, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. 2016;in press.
Berres ML, Koenen RR, Rueland A, et al. Antagonism of the chemokine Ccl5 ameliorates experimental liver fibrosis in mice. J Clin Invest. 2010;120:4129–4140.
Zimmermann HW, Tacke F. Modification of chemokine pathways and immune cell infiltration as a novel therapeutic approach in liver inflammation and fibrosis. Inflamm Allergy Drug Targets. 2011;10:509–536.
Miura K, Yang L, van Rooijen N, Ohnishi H, Seki E. Hepatic recruitment of macrophages promotes nonalcoholic steatohepatitis through CCR2. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1310–G1321.
Baeck C, Wehr A, Karlmark KR, et al. Pharmacological inhibition of the chemokine CCL2 (MCP-1) diminishes liver macrophage infiltration and steatohepatitis in chronic hepatic injury. Gut. 2012;61:416–426.
Lefebvre E, Hashiguchi T, Jenkins H, et al. Anti-fibrotic and anti-inflammatory activity of the dual CCR2 and CCR5 antagonist cenicriviroc in a mouse model of NASH. Hepatology. 2013;58:221A–222A.
Hong F, Chou H, Friedman SL. Significant anti-fibrotic activity of cenicriviroc, a dual CCR2/CCR5 antagonist, in a rat model of thioacetamide-induced liver fibrosis and cirrhosis. Hepatology. 2013;58:S1.
Friedman SL, Sanyal A, Goodman Z et al. Efficacy and safety study of cenicriviroc for the treatment of non-alcoholic steatohepatitis in adult subjects with liver fibrosis: CENTAUR Phase 2b study design. Contemp Clin Trials. 2016;in press.
Gilat T, Somjen GJ, Mazur Y, et al. Fatty acid bile acid conjugates (FABACs)—new molecules for the prevention of cholesterol crystallisation in bile. Gut. 2001;48:75–79.
Gilat T, Leikin-Frenkel A, Goldiner I, et al. Prevention of diet-induced fatty liver in experimental animals by the oral administration of a fatty acid bile acid conjugate (FABAC). Hepatology. 2003;38:436–442.
Leikin-Frenkel A, Gonen A, Shaish A, et al. Fatty acid bile acid conjugate inhibits hepatic stearoyl coenzyme A desaturase and is non-atherogenic. Arch Med Res. 2010;41:397–404.
Goldiner I, van der Velde AE, Vandenberghe KE, et al. ABCA1-dependent but apoA-I-independent cholesterol efflux mediated by fatty acid–bile acid conjugates (FABACs). Biochem J. 2006;396:529–536.
Gutierrez-Juarez R, Pocai A, Mulas C, et al. Critical role of stearoyl-CoA desaturase-1 (SCD1) in the onset of diet-induced hepatic insulin resistance. J Clin Invest. 2006;116:1686–1695.
Powell DA. An overview of patented small molecule stearoyl coenzyme-A desaturase inhibitors (2009–2013). Expert Opin Ther Pat. 2014;24:155–175.
Safadi R, Konikoff FM, Mahamid M, et al. The fatty acid–bile acid conjugate aramchol reduces liver fat content in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2014;12:e2081.
Villanova N, Moscatiello S, Ramilli S, et al. Endothelial dysfunction and cardiovascular risk profile in nonalcoholic fatty liver disease. Hepatology. 2005;42:473–480.
Mells JE, Anania FA. The role of gastrointestinal hormones in hepatic lipid metabolism. Semin Liver Dis. 2013;33:343–357.
Garber AJ. Long-acting glucagon-like peptide 1 receptor agonists: a review of their efficacy and tolerability. Diabetes Care. 2011;34:S279–S284.
Gupta NA, Mells J, Dunham RM, et al. Glucagon-like peptide-1 receptor is present on human hepatocytes and has a direct role in decreasing hepatic steatosis in vitro by modulating elements of the insulin signaling pathway. Hepatology. 2010;51:1584–1592.
Mells JE, Fu PP, Sharma S, et al. Glp-1 analog, liraglutide, ameliorates hepatic steatosis and cardiac hypertrophy in C57BL/6 J mice fed a Western diet. Am J Physiol Gastrointest Liver Physiol. 2012;302:G225–G235.
Svegliati-Baroni G, Saccomanno S, Rychlicki C, et al. Glucagon-like peptide-1 receptor activation stimulates hepatic lipid oxidation and restores hepatic signalling alteration induced by a high-fat diet in nonalcoholic steatohepatitis. Liver Int. 2011;31:1285–1297.
Ding X, Saxena NK, Lin S, Gupta NA, Anania FA. Exendin-4, a glucagon-like protein-1 (GLP-1) receptor agonist, reverses hepatic steatosis in ob/ob mice. Hepatology. 2006;43:173–181.
Armstrong MJ, Hull D, Guo K, et al. Glucagon-like peptide 1 decreases lipotoxicity in non-alcoholic steatohepatitis. J Hepatol. 2016;64:399–408.
Pi-Sunyer X, Astrup A, Fujioka K, et al. A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. N Engl J Med. 2015;373:11–22.
Armstrong MJ, Houlihan DD, Rowe IA, et al. Safety and efficacy of liraglutide in patients with type 2 diabetes and elevated liver enzymes: individual patient data meta-analysis of the LEAD program. Aliment Pharmacol Ther. 2013;37:234–242.
Armstrong MJ, Gaunt P, Aithal GP, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387:679–690.
Di Bisceglie AM, Shiffman ML, Everson GT, et al. Prolonged therapy of advanced chronic hepatitis C with low-dose peginterferon. N Engl J Med. 2008;359:2429–2441.
McHutchison J, Goodman Z, Patel K et al. Farglitazar lacks antifibrotic activity in patients with chronic hepatitis C infection Gastroenterology. 2010;138:1365–1373, 1373 e1361–1362.
Pockros PJ, Jeffers L, Afdhal N, et al. Final results of a double-blind, placebo-controlled trial of the antifibrotic efficacy of interferon-gamma1b in chronic hepatitis C patients with advanced fibrosis or cirrhosis. Hepatology. 2007;45:569–578.
Poynard T, Bruix J, Schiff ER, et al. Improved inflammatory activity with peginterferon alfa-2b maintenance therapy in non-cirrhotic prior non-responders: a randomized study. J Hepatol. 2013;58:452–459.
Kagan HM, Li W. Lysyl oxidase: properties, specificity, and biological roles inside and outside of the cell. J Cell Biochem. 2003;88:660–672.
Kagan HM. Lysyl oxidase: mechanism, regulation and relationship to liver fibrosis. Pathol Res Pract. 1994;190:910–919.
Vadasz Z, Kessler O, Akiri G, et al. Abnormal deposition of collagen around hepatocytes in Wilson’s disease is associated with hepatocyte specific expression of lysyl oxidase and lysyl oxidase like protein-2. J Hepatol. 2005;43:499–507.
Barry-Hamilton V, Spangler R, Marshall D, et al. Allosteric inhibition of lysyl oxidase-like-2 impedes the development of a pathologic microenvironment. Nat Med. 2010;16:1009–1017.
Yang RY, Rabinovich GA, Liu FT. Galectins: structure, function and therapeutic potential. Expert Rev Mol Med. 2008;10:e17.
Henderson NC, Sethi T. The regulation of inflammation by galectin-3. Immunol Rev. 2009;230:160–171.
Henderson NC, Mackinnon AC, Farnworth SL, et al. Galectin-3 regulates myofibroblast activation and hepatic fibrosis. Proc Natl Acad Sci USA. 2006;103:5060–5065.
Traber PG, Chou H, Zomer E, et al. Regression of fibrosis and reversal of cirrhosis in rats by galectin inhibitors in thioacetamide-induced liver disease. PLoS One. 2013;8:e75361.
Traber PG, Zomer E. Therapy of experimental NASH and fibrosis with galectin inhibitors. PLoS One. 2013;8:e83481.
Sanyal AJ, Chalasani N, Kowdley KV, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362:1675–1685.
Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, associates with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–397.
Younossi ZM, Stepanova M, Rafiq N, et al. Pathologic criteria for nonalcoholic steatohepatitis: Interprotocol agreement and ability to predict liver-related mortality. Hepatology. 2011;53:1874–1882.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321.
Bedossa P. Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease. Hepatology. 2014;60:565–575.
Acknowledgments
Funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) under Grant Agreement No. HEALTH-F2-2009-241762 for the Project FLIP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Consultancy for Astra-Zeneca, Boehringer-Ingelheim, Galmed, Genfit, Gilead, Immuron, Intercept, Roche-Genentech, Tobira for VR.
Rights and permissions
About this article
Cite this article
Ratziu, V. Novel Pharmacotherapy Options for NASH. Dig Dis Sci 61, 1398–1405 (2016). https://doi.org/10.1007/s10620-016-4128-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4128-z