Abstract
Background and Aims
The aim of the study was to evaluate the safety of non-anesthesia provider (NAAP)-administered propofol sedation for advanced endoscopic procedures with those of anesthesia provider (AAP).
Methods
PubMed, EMBASE, Cochrane Central Register of Controlled Trials, Scopus, and Web of Science databases were searched for prospective observational trials involving advanced endoscopic procedures. From a total of 519 publications, 26 were identified to meet inclusion criteria (10 AAPs and 16 NAAPs) and were analyzed. Data were analyzed for hypoxia rate, airway intervention rates, endoscopist, and patient satisfaction scores and total propofol administered.
Results
Total number of procedures in NAAP and AAP groups was 3018 and 2374, respectively. Pooled hypoxia (oxygen saturation less than 90 %) rates were 0.133 (95 % CI 0.117–0.152) and 0.143 (95 % CI 0.128–0.159) in NAAP and AAP, respectively. Similarly, pooled airway intervention rates were 0.035 (95 % CI 0.026–0.047) and 0.133 (95 % CI 0.118–0.150), respectively. Pooled patient satisfaction rate, pooled endoscopist satisfaction rate, and mean propofol administered dose for NAAP were 7.22 (95 % CI 7.17–7.27), 6.03 (95 % CI 5.94–6.11), and 251.44 mg (95 % CI 244.39–258.49) in that order compared with 9.82 (95 % CI 9.76–9.88), 9.06 (95 % CI 8.91–9.21), and 340.32 mg (95 % CI 327.30–353.33) for AAP.
Conclusions
The safety of NAAP sedation compared favorably with AAP sedation in patients undergoing advanced endoscopic procedures. However, it came at the cost of decreased patient and endoscopist satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Propofol is a popular sedative for patients undergoing advanced endoscopic procedures. Trials including meta-analyses, comparing the safety and efficacy of sedation with propofol with other agents, have shown the superiority of propofol [1]. Being an anesthetic, it is commonly administered by anesthesiologists (physicians trained to provide anesthesia) or certified nurse anesthetists with or without the supervision of a physician. However, increasingly, anesthesia provider’s (AAP) fees and provider availability have necessitated a rethink in this area of sedation [2]. A common objection from the AAPs and the organizations representing them is that the anesthetic agent propofol is unsafe in the hands of non-anesthesia providers (NAAPs) [3, 4]. Inadequate experience in recognizing and managing an obstructed airway is a commonly cited reason for this objection. The Centers for Medicare & Medicaid Services’ (CMS) sedation guidelines state that propofol administration for deep sedation in Medicare patients and Medicare settings should only be performed by an anesthesiologists [5]. Many prospective observational trials have addressed the safety of NAAP-administered propofol in patients undergoing various endoscopic procedures [6–11]. Large retrospective trials have reported a very low incidence of adverse events, when propofol was administered by NAAPs [12], and gastroenterological professional society published statements and several review articles have spoken about the concept [13–16]. The NAAPs in question are either gastroenterologists themselves or more commonly a certified nurse administering propofol under the guidance of a gastroenterologist. Nevertheless, there is only one published prospective trial comparing the outcome between the two providers [17]. In this study involving 90 patients undergoing colonoscopy, both safety and patient satisfaction were superior in the group administered propofol by the endoscopist. In view of the mounting evidence on the safety of non-anesthesiologist-administered propofol, Federal Drug Administration (FDA) recently approved propofol-based sedation by gastroenterologists using “SEDASYS®,” a computer-assisted personalized sedation (CAPS) system [4].
In the current meta-analysis, we aimed to calculate pooled adverse event rates associated with propofol sedation administered by both anesthesia and NAAPs for advanced upper gastroenterological procedures. A network meta-analysis was not practical, as sedation settings in various individual hospitals show marked variations. Thus, we planned to compare the results of two separate meta-analyses in order to calculate individual sedation-related airway adverse event rates between NAAP-administered and AAP-administered propofol groups.
Methods
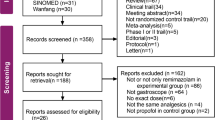
All authors had access to the study data and reviewed and approved the final manuscript. The following databases were used to search for relevant publications during the month of November 2014: PubMed, EMBASE, Cochrane Central Register of Controlled Trials, Scopus, and Web of Science. The medical subject headings (MeSH) used were as follows: endoscopic ultrasound (EUS) propofol, ERCP anesthesia, propofol sedation advanced endoscopic procedures, propofol sedation ERCP, propofol sedation EUS, non-anesthesia provider-administered propofol, endoscopist-administered propofol, and nurse-administered propofol sedation. After deleting the duplicate search results, a total of 519 publications (from 1976 onwards) were analyzed. When the available information was incomplete or conflicting, an effort was made to contact the corresponding author. As illustrated in the flow diagram, 26 trials were included in the final analysis. Of these, 10 trials involved AAP sedation [18–27] and in the remainder of 16 trials included NAAP sedation [28–43], (Fig. 1; Tables 1, 2).
There were no prospective randomized controlled trials directly comparing propofol administration by the two groups of sedation providers at the time of search. As a result, we estimated pooled values of sedation-related parameters to get an indirect comparison between NAAP and AAP groups.
The following criteria were required for a study to be included in the meta-analysis.
-
1.
The data were collected prospectively.
-
2.
All trials involved administration of propofol either as a single agent or along with other sedative/analgesic adjuvants.
-
3.
Trials involved patients undergoing advanced endoscopic procedures only. If the study included both advanced and non-advanced procedures, they were excluded. The advanced procedures included upper EUS, endoscopic retrograde cholangiopancreatography (ERCP), and deep small intestinal enteroscopy.
-
4.
Sedation was provided either by the anesthesiologist or by a certified registered nurse anesthetist (CRNA) under the guidance of an anesthesiologist or a registered nurse guided by a gastroenterologist or a non-anesthesiologist physician.
Data Extraction
A standardized form was used for data documentation. The following data were extracted from the relevant trials: first author of the study, characteristics of population studied, nature of procedures performed, frequency of patients desaturation below 90 %, need for intervention to maintain airway, type of intervention, total propofol dose used, patient/endoscopist satisfaction rate, complications during the procedure, any mortality, or any immediate cardiopulmonary complications. The salient features and findings of the publications analyzed are presented in Tables 1 and 2.
Statistical Analysis
The statistical analysis of the pooled data was performed using Comprehensive Meta-analysis version 2 (Biostat Inc, USA). Meta-analysis was performed initially using fixed-effects modeling and eventually with random-effects methods (after assessment of heterogeneity with fixed modeling). The extent of heterogeneity in between the trials was quantified using the I 2 statistic. Values of I 2 < 40 % were considered unimportant, 40–50 % were considered to represent moderate heterogeneity, and 50–90 % represented high heterogeneity. Results of primary end points (hypoxia and airway intervention rate) were expressed as event rate (per patient) with 95 % CI. Secondary end points that included patient/endoscopist satisfaction scores (both rated at a scale with maxima of 10) were reported as mean with 95 % CI. The resulting pooled value if associated with an alpha error of <5 %, i.e., a “P < 0.05”, was considered statistically significant. Potential publication bias was further evaluated by funnel plot. To account for the high heterogeneity in our analysis, various methods were used. We did a sensitivity analysis by removing single study at a time. Further evaluation of heterogeneity was done by creating possible subgroups. A meta-regression was not possible as the recommended number of trials required for a valid meta-regression (i.e., 10 or more) was not met in any of the subgroups. All values reported for analysis with I 2 more than 40 % are from random-effects modeling only.
Results: Primary End Points
The pooled rates in the AAP group were as follows.
Hypoxia
A total of 16 groups/subgroups reported the required values. The pooled hypoxia rate in AAP group was found to be 0.143 (95 % CI 0.128–0.159). This result, however, showed a significant degree of heterogeneity of 77.24 % (Fig. 2). Further subgroup analysis dividing the included trials into ERCP [13] and non-ERCP [3] had minimal effect on the heterogeneity and brought it down to 75.26 %. Further, a sensitivity analysis (with one study removed at each step) demonstrated that results of Cote et al. contributed most to the heterogeneity; however, its deletion changed the heterogeneity by only 2.4 %.
Airway Intervention
Eleven groups/subgroups reported the airway intervention rate during the procedures. The pooled intervention rate was found to be 0.133 (95 % CI 0.118–0.150) with P < 0.001. The heterogeneity was found to be very high at 89.02 % (Fig. 3). Sensitivity analysis performed after removing the study contributing most to heterogeneity (Cote et al.) brought this down to 68.54 %, suggesting significant methodological variations among the sedation providers. On removing subgroups involving non-ERCP procedures (three participants of 11), the heterogeneity was reduced to 65.50 %.
The pooled values in the in NAAP group were as follows.
Hypoxia
A total of 19 participant trials/subgroups reported the incidence of hypoxia during the procedures. The pooled hypoxia rate was found to be 0.133 (95 % CI 0.117–0.152) with a P < 0.001. The heterogeneity was found to be 92.95 % (Fig. 4). On step-by-step single study removal, heterogeneity dropped to 84.83 % by removing Angsuwatcharakon et al. subgroup that was contributing most to the heterogeneity. Further, by removing trials from the non-ERCP group (five trials), the heterogeneity only decreased to 90.31 %.
Airway Intervention
Airway intervention rates were documented in 15 of the included subgroups. Pooled intervention rate was found to be 0.035 (95 % CI 0.026–0.047) with P < 0.001. This was associated with a heterogeneity of 76.02 % (Fig. 5). For reduction in heterogeneity, one study exclusion was performed at a time and study by Fatima et al. was found to contribute most to the heterogeneity. On its removal, the I 2 value dropped only marginally to 69.57 %. Five trials involving non-ERCP procedures were excluded to further analyze the effect on heterogeneity, and I 2 values after this exclusion were found to be 59.65 %.
Results: Secondary End Points
Both the above groups were also analyzed for pooled rate of the following parameters as explorative objectives, resulting in the following findings.
AAP Group
Patient Satisfaction
Six trials reported patient satisfaction scores recorded after the procedural sedation. On a scale of 1–10, mean pooled patient satisfaction scores were found to be 9.82 (95 % CI 9.76–9.88) with a P value <0.001. The heterogeneity for this pooled analysis was 89.72 % (Fig. 6a)
Endoscopist Satisfaction
Six trials reported the mean scores. Pooled mean value was found to be 9.06 (95 % CI 8.91–9.21) (on a scale of 1–10) with P < 0.001 and a heterogeneity of 79.28 % (Fig. 6b)
Mean Propofol Administered
Ten trials reported the amount of propofol administered with a mean of 340.32 mg (95 % CI 327.30–353.33) I 2 = 95.88 % (Fig. 8).
NAAP Group
Patient Satisfaction Scores
Mean pooled patient satisfaction score was found to be 7.22 (95 % CI 7.17–7.27) with a heterogeneity of 99.88 % reported in eight of the trials (Fig. 7a).
Endoscopist Satisfaction Scores
Five trials reported the mean endoscopist satisfaction scores on a scale of 1–10. Pooled satisfaction score was found to be 6.03 (95 % CI 5.94–6.11) with P < 0.001. The heterogeneity of this analysis was 98.98 % (Figs. 7b, 8).
Mean Propofol Administered
Fourteen trials reported the amount of propofol administered with a mean of 251.44 mg (95 % CI 244.39–258.49), I 2 99.08 % (Fig. 9).
34.38 percent of the patients in AAP group and 37.1 percent in NAAP group were of American Society of Anesthesiologists (ASAs) class 3–4. Although a quantitative analysis was not possible, the patients data in terms of both age and ASA physical status were similar in both groups.
For assessment of publication bias, Egger’s regression test was used for the reporting of hypoxia (primary end point) in both the NAAP and AAP groups. For AAP group, the intercept at X-axis was found to be −0.21 (95 % CI −1.93 to 1.51) with a P value of 0.796, i.e., a statistically significant bias was unlikely in AAP group. Similarly, for NAAP the intercept at X-axis was at −4.69 (95 % CI 0.33 to −9.73) with a P value of 0.065; as a result publication bias was unlikely in this group as well. The funnel plots of standard error by logit event rate for AAP and NAAP (both showing symmetrical distribution) are shown in Figs. 10 and 11, respectively.
Please note that the comparison values are presented with their 95 % CI (denoting values pertaining to whole of the population) rather than a single value, which would have accounted only for the study group.
Interestingly, the absence of overlap of 95 % CI values for these population-based results itself indirectly suggests that the values in the actual population are statistically different; however, in the absence of trials making direct comparisons and given the limitations of indirect meta-analysis, a “P” value comparison cannot be made.
Discussion
The main findings of the study are as follows:
-
1.
The pooled hypoxia rates in patients undergoing advanced endoscopic procedures sedated with propofol were similar, irrespective of the provider administering it.
-
2.
Airway interventions (such as jaw thrust, chin lift, mask ventilation, and endotracheal intubation) and airway intervention rates were higher in the patient groups administered propofol by AAPs.
-
3.
However, both patient satisfaction and endoscopist satisfaction were better when propofol was given by AAPs.
-
4.
Anesthesia providers administered higher doses of propofol, although the precise nature and complexity of the procedures were unknown.
In clinical trial settings, propofol can be administered safety by NAAPs, during the conduct of advanced endoscopic procedures. However, the practice is associated with decreased patient and endoscopist satisfaction.
Similarly, the safety of propofol administration in the hands of NAAPs was demonstrated in a very large retrospective study by Rex et al. [12]. Although frequently cited, the study is also criticized for two reasons. Firstly, it is a retrospective study with the expected limitations. Secondly, some of the data used were based on the recollection of the participating centers, instead of a formal record. In spite of these shortcomings, the large number of the patients in the study, diversity of the procedures, and the global nature of the data cannot be ignored.
Can our findings be applied more generally to make recommendations? The gastroenterologists involved in the non-anesthesia provider-administered propofol trials might represent a subgroup of very competent physicians with dedication to the area of sedation. Their other publications in the area would support such a hypothesis. However, a similar argument can be made for the anesthesiologist-administered or anesthesiologist-supervised trials. It is commonly a group of dedicated AAPs who undertake sedation responsibilities during these procedures [44]. It is plausible that the AAPs were more apt to institute airway support interventions biasing their results. Another consideration is that in the NAAP sedation group, the gastroenterologists were more “in tune” with the nuances and duration of the procedures resulting in lower propofol requirements and vis-a-vis fewer airway support interventions.
Another possible consideration is that drawing from their experience and owing to their comfort with airway management and rescue, higher doses of propofol were administered by the AAPs. This observation is strengthened by the finding of more frequent airway manipulations (chin lift, jaw thrust, endotracheal intubations, additional airway devices, and procedure interruptions) in the AAP group. As a group, AAPs tend to provide deeper sedation [45]. This has been demonstrated by using electroencephalogram-based brain function monitor. In a study involving 87 adults undergoing colonoscopy (unpublished) in the Hospital of the University of Pennsylvania, approximately half were provided propofol sedation, by a small group of nurse anesthetists, and the remaining were given midazolam–fentanyl by the endoscopy nurse under the guidance of the endoscopist. Unlike the midazolam–fentanyl group, all the patients in the propofol group spent significant period of their procedure in general anesthesia and even deep general anesthesia. In patients undergoing colonoscopy, it is easy to prevent hypoxemia by mask ventilation. However, mask ventilation is not feasible while sustaining upper GI endoscopy without procedure interruption and endoscope withdrawal. The need for endotracheal intubation and procedure interruption and cancellation was high in AAP-administered propofol group, while absent in non-anesthesia propofol group.
It is also possible that the gastroenterologists expect deeper degree of sedation to the point of general anesthesia when propofol is administered by AAPs. They might be willing to perform the procedure with suboptimal sedation when propofol is administered under their own supervision. The increased endoscopist satisfaction scores in the AAP group might support such a hypothesis. Frequent use of adjuvants such as midazolam and fentanyl in the AAP might have contributed to increased patient satisfaction. By virtue of their experience and expertise in managing the airway, AAPs might err toward deeper sedation, which is associated with greater patient and endoscopist satisfaction.
The reasons for the extensive use of AAPs to administer propofol in GI endoscopy might be other than safety concerns. Many gastroenterologists might be unwilling to shoulder additional responsibility. Rarely, a need for converting to general anesthesia may arise. The gastroenterologists may not be provided with additional remuneration to shoulder the responsibility of administering propofol.
Limitations of the Study
The most important limitation of this study is “indirect comparison of pooled estimates between NAAP and AAP.” Additionally, the present analysis suffers a significant degree of heterogeneity in almost all reported pooled values. Despite making subgroups for sensitivity analysis, we were unable to significantly improve the heterogeneity. However, to balance this variability, all values reported are from random-effects modeling. Although it widened our confidence intervals, all values remained statistically significant, maintaining the strength of evidence. This heterogeneity is probably due to variations in the technique of propofol administration, both within the groups and among the different centers where trials were carried out. None of the trials reported the expertise of sedation provider or the quality of endoscopy suite setup, and thus, any comparison to eliminate heterogeneity arising from these variations could not be made. A preference for co-administration of adjuvants was a consistent feature of AAP groups, while propofol alone was preferentially administered in NAAP groups; however, due to inconsistent reporting, this factor could not be compared. Additionally, duration of the procedure and the context of the study were not accounted for.
The reported data on blood pressure and heart rate were inconsistent and the definitions varied. As a result, pooled comparison was not possible. Given the higher doses of propofol and frequent use of adjuvants, it is realistic to expect more frequent and greater degrees of hypotension and bradycardia episodes in the AAP group. Such episodes could be preempted in susceptible individuals by administering appropriate medications, thus limiting the value of hemodynamic data.
Another limitation of the present analysis is that some studies like Mazinkov et al. 2011 had three subgroups (remifentanil group, alfentanyl high-dose group, and alfentanyl low-dose group), and these were analyzed individually as separate representation in the statistics. We were able to extract independent data for such individual groups in the study; however, possible violation of methodological individuality cannot be negated with absolute certainty.
Conclusion
Although gastroenterologists with an interest in sedation can administer propofol safely for advanced endoscopic procedures, the practice is associated with reduced patient and endoscopist satisfaction. As satisfaction is important for patient compliance and successful completion of the procedures, the gastroenterologists interested in providing propofol sedation for advanced procedures should undergo training in deep sedation and airway management.
References
Sethi S, Wadhwa V, Thaker A, et al. Propofol versus traditional sedative agents for advanced endoscopic procedures: a meta-analysis. Dig Endosc. 2014;26:515–524.
Dumonceau J-M. Nonanesthesiologist administration of propofol: it’s all about money. Endoscopy. 2012;44:453–455.
Goudra BG, Singh PM. SEDASYS, sedation, and the unknown. J Clin Anesth. 2014;26:334–336.
Goudra BG, Singh PM, Chandrasekhara V. SEDASYS®, airway, oxygenation, and ventilation: anticipating and managing the challenges. Dig Dis Sci. 2014;59:920–927.
Clarification of the interpretative guidelines for the anaesthesia services condition of participation and revised hospital anaesthesia guidelines-state operations manual (SOM) Appendix A, S&C-10-09-Hospital. CMS publication no. 100-07.
Rex DK, Overley C, Kinser K, et al. Safety of propofol administered by registered nurses with gastroenterologist supervision in 2000 endoscopic cases. Am J Gastroenterol. 2002;97:1159–1163.
Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C. Safety of propofol for conscious sedation during endoscopic procedures in high-risk patients-a prospective, controlled study. Am J Gastroenterol. 2003;98:1751–1757.
Külling D, Rothenbühler R, Inauen W. Safety of nonanesthetist sedation with propofol for outpatient colonoscopy and esophagogastroduodenoscopy. Endoscopy. 2003;35:679–682.
Sieg A, bng-Study-Group, Beck S, et al. Safety analysis of endoscopist-directed propofol sedation: a prospective, national multicenter study of 24 441 patients in German outpatient practices. J Gastroenterol Hepatol. 2014;29:517–523.
Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C. Risk stratification and safe administration of propofol by registered nurses supervised by the gastroenterologist: a prospective observational study of more than 2000 cases. Gastrointest Endosc. 2003;57:664–671.
Sieg A. Propofol sedation in outpatient colonoscopy by trained practice nurses supervised by the gastroenterologist: a prospective evaluation of over 3000 cases. Z Gastroenterol. 2007;45:697–701.
Rex DK, Deenadayalu VP, Eid E, Imperiale TF, Walker JA, Sandhu K, et al. Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology. 2009;137:1229–1237; quiz 1518–1519.
Chen SC, Rex DK. Review article: registered nurse-administered propofol sedation for endoscopy. Aliment Pharmacol Ther. 2004;19:147–155.
Rex DK. Endoscopist-directed propofol. Tech Gastrointest Endosc. 2009;11:177–180.
Cohen LB, Dubovsky AN, Aisenberg J, Miller KM. Propofol for endoscopic sedation: a protocol for safe and effective administration by the gastroenterologist. Gastrointest Endosc. 2003;58:725–732.
Vargo JJ, Cohen LB, Rex DK, Kwo PY. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastrointest Endosc. 2009;70:1053–1059.
Poincloux L, Laquière A, Bazin J-E, et al. A randomized controlled trial of endoscopist vs. anaesthetist-administered sedation for colonoscopy. Dig Liver Dis. 2011;43:553–558.
Paspatis G, Chainaki I, Manolaraki M, et al. Efficacy of bispectral index monitoring as an adjunct to propofol deep sedation for ERCP: a randomized controlled trial. Endoscopy. 2009;41:1046–1051.
Paspatis GA, Manolaraki MM, Vardas E, Theodoropoulou A, Chlouverakis G. Deep sedation for endoscopic retrograde cholangiopancreatography: intravenous propofol alone versus intravenous propofol with oral midazolam premedication. Endoscopy. 2008;40:308–313.
Coté GA, Hovis RM, Ansstas MA, et al. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol.. 2010;8:137–142.
Fanti L, Agostoni M, Arcidiacono PG, et al. Target-controlled infusion during monitored anesthesia care in patients undergoing EUS: propofol alone versus midazolam plus propofol. A prospective double-blind randomised controlled trial. Dig Liver Dis. 2007;39:81–86.
Mazanikov M, Udd M, Kylänpää L, et al. Patient-controlled sedation for ERCP: a randomized double-blind comparison of alfentanil and remifentanil. Endoscopy. 2012;44:487–492.
Mazanikov M, Udd M, Kylänpää L, et al. A randomized comparison of target-controlled propofol infusion and patient-controlled sedation during ERCP. Endoscopy. 2013;45:915–919.
Kongkam P, Rerknimitr R, Punyathavorn S, et al. Propofol infusion versus intermittent meperidine and midazolam injection for conscious sedation in ERCP. J Gastrointest Liver Dis. 2008;17:291–297.
Barnett SR, Berzin T, Sanaka S, Pleskow D, Sawhney M, Chuttani R. Deep sedation without intubation for ERCP is appropriate in healthier, non-obese patients. Dig Dis Sci. 2013;58:3287–3292.
Berzin TM, Sanaka S, Barnett SR, et al. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011;73:710–717.
Mazanikov M, Udd M, Kylänpää L, et al. Patient-controlled sedation with propofol and remifentanil for ERCP: a randomized, controlled study. Gastrointest Endosc. 2011;73:260–266.
Redondo-Cerezo E, Sánchez-Robaina A, Martínez Cara JG, et al. Gastroenterologist-guided sedation with propofol for endoscopic ultrasonography in average-risk and high-risk patients: a prospective series. Eur J Gastroenterol Hepatol. 2012;24:506–512.
Lee CK, Lee S-H, Chung I-K, et al. Balanced propofol sedation for therapeutic GI endoscopic procedures: a prospective, randomized study. Gastrointest Endosc. 2011;73:206–214.
Von Delius S, Salletmaier H, Meining A, et al. Bispectral index monitoring of midazolam and propofol sedation during endoscopic retrograde cholangiopancreatography: a randomized clinical trial (the EndoBIS study). Endoscopy. 2012;44:258–264.
Lee TH, Lee CK, Park S-H, et al. Balanced propofol sedation versus propofol monosedation in therapeutic pancreaticobiliary endoscopic procedures. Dig Dis Sci. 2012;57:2113–2121.
Khan HA, Umar M, Tul-Bushra H, Nisar G, Bilal M, Umar S. Safety of non-anaesthesiologist-administered propofol sedation in ERCP. Arab J Gastroenterol. 2014;15:32–35.
Riphaus A, Geist C, Schrader K, Martchenko K, Wehrmann T. Intermittent manually controlled versus continuous infusion of propofol for deep sedation during interventional endoscopy: a prospective randomized trial. Scand J Gastroenterol. 2012;47:1078–1085.
Dewitt J, McGreevy K, Sherman S, Imperiale TF. Nurse-administered propofol sedation compared with midazolam and meperidine for EUS: a prospective, randomized trial. Gastrointest Endosc. 2008;68:499–509.
Angsuwatcharakon P, Rerknimitr R, Ridtitid W, et al. Cocktail sedation containing propofol versus conventional sedation for ERCP: a prospective, randomized controlled study. BMC Anesthesiol. 2012;12:20.
García-Suárez C, López-Rosés L, Olivencia P, et al. Sedation with propofol controlled by endoscopists during percutaneous endoscopic gastrostomy. Rev Esp Enferm Dig. 2010;102:249–256.
Wehrmann T, Grotkamp J, Stergiou N, et al. Electroencephalogram monitoring facilitates sedation with propofol for routine ERCP: a randomized, controlled trial. Gastrointest Endosc. 2002;56:817–824.
Yusoff IF, Raymond G, Sahai AV. Endoscopist administered propofol for upper-GI EUS is safe and effective: a prospective study in 500 patients. Gastrointest Endosc. 2004;60:356–360.
Fatima H, DeWitt J, LeBlanc J, Sherman S, McGreevy K, Imperiale TF. Nurse-administered propofol sedation for upper endoscopic ultrasonography. Am J Gastroenterol. 2008;103:1649–1656.
Vargo JJ, Zuccaro G, Dumot JA, et al. Gastroenterologist-administered propofol versus meperidine and midazolam for advanced upper endoscopy: a prospective, randomized trial. Gastroenterology. 2002;123:8–16.
Riphaus A, Stergiou N, Wehrmann T. Sedation with propofol for routine ERCP in high-risk octogenarians: a randomized, controlled study. Am J Gastroenterol. 2005;100:1957–1963.
Schilling D, Rosenbaum A, Schweizer S, Richter H, Rumstadt B. Sedation with propofol for interventional endoscopy by trained nurses in high-risk octogenarians: a prospective, randomized, controlled study. Endoscopy. 2009;41:295–298.
Wehrmann T, Kokabpick S, Lembcke B, Caspary WF, Seifert H. Efficacy and safety of intravenous propofol sedation during routine ERCP: a prospective, controlled study. Gastrointest Endosc. 1999;49:677–683.
Goudra BG, Singh PM, Sinha AC. Anesthesia for ERCP: impact of anesthesiologist’s experience on outcome and cost. Anesthesiol Res Pract. 2013;2013:570518.
Goudra BG, Singh PM, Manjunath A, Reihmer J. Sedation spectrum in patients undergoing advanced gastrointestinal (GI) endoscopic procedures with propofol, presented at the annual meeting of International Society of Anesthetic Pharmacology, San Fransisco October 11th 2013.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goudra, B.G., Singh, P.M., Gouda, G. et al. Safety of Non-anesthesia Provider-Administered Propofol (NAAP) Sedation in Advanced Gastrointestinal Endoscopic Procedures: Comparative Meta-Analysis of Pooled Results. Dig Dis Sci 60, 2612–2627 (2015). https://doi.org/10.1007/s10620-015-3608-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3608-x