Abstract
Background
There is increasing evidence that ischemia–reperfusion injury (IRI) promotes vasculogenesis and tumor outgrowth in the liver. Hepatic IRI is exaggerated by prolongation of ischemia times.
Aims
The aim of this retrospective analysis was to assess the impact of ischemia times on risk of hepatocellular carcinoma (HCC) recurrence after liver transplantation (LT). Subgroup analysis focused on patients with 18F-fluoro-deoxy-glucose (18F-FDG)-avid HCC on pretransplant positron emission tomography (PET).
Methods
A total of 103 liver transplant patients with HCC were included in this study. The impact of cold (CIT), warm (WIT), and total ischemia times (TIT) along with other prognostic variables on posttransplant outcome was analyzed in uni- and multivariate analysis.
Results
Twenty-four patients (23.3 %) developed tumor relapse after LT. Mean durations of CIT (468.0 vs. 375.5 min; P = 0.001), WIT (58.4 vs. 45.7 min; P = 0.001), and TIT (525.8 vs. 422.0 min; P < 0.001) were significantly longer in patients with compared to those without HCC recurrence. In multivariate regression analysis, 18F-FDG-avid HCC (odds ratio [OR] 73.4), WIT >50 min (OR 52.5), alpha-fetoprotein level >400 IU/ml (OR 11.1), and Milan Out status (OR 7.4) were identified as independent predictors of HCC recurrence. In the subgroup of patients with PET-positive HCC, WIT remained the only independent variable to predict HCC recurrence (OR 15.5).
Conclusion
Prolongation of ischemia times promotes the risk of HCC recurrence after LT, especially in patients with unfavorable tumor biology on PET imaging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The implementation of the Milan classification (one tumor nodule up to 5 cm, or up to 3 tumor nodules, each up to 3 cm, no macrovascular tumor infiltration) in 1996 as clinical standard criteria has dramatically improved the outcome of patients with hepatocellular carcinoma (HCC) following liver transplantation (LT). Their adoption produced posttransplant survival rates that were nearly similar to that of patients with non-cancerous liver disease [1]. Since then, important developments in radiologic imaging, locoregional therapies, surgical techniques, and immunosuppressive agents added to further significant improvement of prognosis [2, 3].
To make this treatment option available to a larger number of patients, substantial efforts were made in expanding transplant criteria for HCC [3, 4]. It became clear in this process that extending selection criteria on the basis of tumor macromorphology will be related to an increased risk of tumor recurrence, which appears to be highly questionable given the scarcity of donor organs [2–4]. Biological tumor behavior rather than macromorphology of HCC is currently supposed to determine the limits of indication [5]. Most recently, the metabolic uptake pattern of HCC in 18F-fluoro-deoxy-glucose (18F-FDG) positron emission tomography (PET) was demonstrated to appropriately describe biological tumor aggressiveness and to provide valuable prognostic information in the transplant setting. Therefore, pretransplant PET imaging is increasingly taken into account in liver transplant candidates with HCC [6–9]. It is nowadays well accepted that a subgroup of patients with less aggressive HCC beyond the Milan criteria may benefit from LT [5].
In recent years, circulating tumor cells (CTCs) were increasingly recognized as promoters of recurrent HCC [10, 12]. Surgical stress by ischemia–reperfusion injury (IRI) was shown to trigger up-regulation of several cytokines and, thereby, to support engraftment of CTCs, vasculogenesis, tumor outgrowth, and metastasis in the liver [11–14]. Ischemia–reperfusion damage to the allograft is mainly exaggerated by prolongation of cold (CIT) and warm (WIT) ischemia times [15]. Nonetheless, the impact of ischemia times on risk of tumor relapse in clinical LT has not yet been analyzed in detail.
The aim of our trial was to correlate ischemia times with risk of HCC recurrence and outcome in liver recipients, with a special focus on patients with unfavorable tumor behavior on pretransplant 18F-FDG-PET scanning.
Materials and Methods
The medical records of 103 adult (full-size deceased) liver transplant patients between 1996 and 2010 were retrospectively studied (Table 1). The study has been approved by the local ethics committee. Patients with early postoperative mortality (within 30 days from surgical procedure) and recipients of a partial liver allograft were excluded from the analysis. Diagnosis of HCC was established by radiographic staging and determination of alpha-fetoprotein (AFP) levels, but without performing percutaneous tumor biopsy. Listing for LT was based on the Milan criteria [1]. After implementation of the model for end-stage liver disease (MELD) score in the Eurotransplant region in December 2006, patients with HCC meeting the Milan criteria have received regular MELD score upgradings [16]. According to final pretransplant clinical staging by computed tomography (CT) and/or magnetic resonance imaging (MRI), patients were classified as Milan In (HCC meeting the Milan criteria) versus Milan Out (HCC exceeding the Milan criteria). Macromorphologic tumor progression beyond the Milan limits resulted in loss of MELD priority points. These patients were not automatically removed from the waiting list but underwent short-term re-evaluations. They were preferably scheduled for LT by center-based or rescue allocation. Rapid tumor progression, extrahepatic tumor spread, macrovascular tumor invasion, lymph node infiltration, and tumor-related symptoms led to dropout of patients from the waiting list.
All liver transplant candidates with hepatic malignancy underwent additional tumor imaging by 18F-FDG-PET, as previously described [6, 17]. According to the 18F-FDG-uptake patterns on PET, patients were classified as PET+ (18F-FDG uptake of the tumor higher than surrounding normal liver tissue) or PET− (18F-FDG uptake of the tumor comparable to surrounding normal liver tissue) [6, 17].
Based on liver function and tumor topography, patients underwent neoadjuvant locoregional tumor therapy, mainly by transarterial chemoembolization (TACE). All liver transplants were performed without veno-venous bypass by using the piggyback technique [18].
Cold ischemia time was defined as time interval between in situ cold liver flushing during organ retrieval and termination of ex situ cold liver storage.
Warm ischemia time illustrated the time period between termination of cold liver storage and start of portal reperfusion and was thus corresponding with the anastomosis time [19].
Total ischemia time (TIT) was calculated by the sum of CIT and WIT.
Immunosuppressive therapy consisted of a calcineurin inhibitor-based regimen by cyclosporine A (CsA) or tacrolimus (Tac), augmented with azathioprine (AZA) or mycophenolate mofetil (MMF) and prednisone (Table 1).
The posttransplant tumor surveillance program consisted of ultrasonography and AFP level measurement every 3 months. Furthermore, CT/MRI of chest and abdomen were performed every 6 months in the first posttransplant year and minimum yearly thereafter, or in the case of suspected tumor recurrence.
The following parameters and their impact on risk of HCC recurrence were assessed:
Pretransplant (Clinical) Variables:
Donor and recipient age, sex, child status, AFP level, size and number of tumor nodules (radiographic imaging), Milan criteria (radiographic imaging), and PET status.
Perioperative (IRI) Variables:
Donor risk index (DRI), operation time (OT), estimated blood loss (EBL), perioperatively administered red blood cell (RBC) transfusion units, CIT, WIT, TIT, and immunosuppression.
Histopathologic (explant) Variables:
Microvascular (MVI) and lymphovascular invasion (LVI), tumor differentiation (grading), major vessel invasion, and lymph node involvement.
Statistical analyses were performed using the software SPSS 19.0 for Windows. Continuous variables were expressed as mean ± standard deviation (STD) and compared using the Student’s t test. Categorical variables were summarized as frequencies and percentages. They were compared using χ2 test. Overall and recurrence-free survival rates were determined by the Kaplan–Meier method and compared using the log-rank test. Variables being significantly associated with risk of HCC recurrence on univariate assessment (P < 0.05) were entered into a multivariate Cox regression model.
Results
Patient and Tumor Characteristics
Patient and tumor characteristics are listed in Table 1. The predominant underlying liver diseases were alcoholic and postviral hepatitis. Sixty-four patients (62.1 %) underwent locoregional treatment prior to LT. At last pretransplant clinical staging, 63 liver transplant candidates were classified as Milan In (61.2 %), while 40 patients (39.8 %) demonstrated HCC beyond Milan criteria (Milan Out). On pretransplant PET imaging, 37 patients had 18F-FDG-avid HCC (PET+ status; 35.9 %), while 66 patients demonstrated 18F-FDG-non-avid tumors (PET− status; 64.1 %).
Overall and Recurrence-Free Outcome
Current mean survival post-LT was 79.6 ± 46.6 months (range 5–181 months). Overall and recurrence-free survival rates at 1 and 3 years post-LT were 94.6 and 83.9, and 86.2 and 78.3 %, respectively. Twenty-four patients developed HCC recurrence (23.3 %) after a mean of 15.5 months (range 4–55 months). Sixteen of them were Milan Out patients (66.6 %), while eight patients demonstrated tumors meeting the Milan criteria (33.3 %) at final pretransplant radiographic staging.
Eight of 63 patients with Milan In (12.7 %) tumors but 16 of 40 patients with Milan Out HCC (39 %) have developed tumor recurrence (P = 0.001) post-LT.
Recurrence-free survival rates were 91.9 and 87.1 % in Milan In patients and 72.0 and 64.3 % in Milan Out recipients at 1 and 3 years post-LT, respectively (P = 0.001).
Risk Factors for HCC Recurrence
Differences in tumor- and IRI-related variables between patients with and those without HCC recurrence are described in Table 2. Ischemia times were all significantly longer in patients with tumor relapse compared to those without HCC recurrence.
Parameters with a significant influence on risk of HCC recurrence in univariate analysis are listed in Table 3. In multivariate Cox regression analysis, PET+ status, WIT >50 min, AFP level >400 IU/ml, and Milan Out status were identified as independent predictors of HCC recurrence (Table 4).
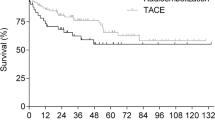
Disease-free survival rates at 1 and 3 years post-LT were 97.2 and 92.8 % in WIT ≤50 min and 61.4 and 42.0 % in WIT >50 min, respectively (Fig. 1). Following LT with WIT ≤50 min, only 6 of 71 patients developed HCC recurrence (8.5 %) compared with 18 of 32 patients after LT with WIT exceeding 50 min (56.3 %; P < 0.001).
Mean time interval to posttransplant HCC recurrence was significantly shorter after extended (12.2 ± 6.8 months) than after limited WIT (25.3 ± 19.7 months; P = 0.02), respectively.
Sixteen of 32 liver recipients developed early HCC recurrence within 12 months after prolonged WIT (50 %) compared with only two of 71 patients (2.8 %) following short-term WIT (P < 0.001).
In the Milan In subpopulation (n = 63), none of 44 patients after limited WIT (0 %) but 8 of 19 patients following extended WIT (42.2 %) were suffering from tumor recurrence (P = 0.001), respectively. In the Milan Out subset, 10 of 13 liver recipients after WIT exceeding 50 min (76.9 %) but only 6 of 27 patients following WIT ≤50 min (22.2 %) have developed post-LT HCC relapse (P = 0.001).
Subanalysis in PET+ Patients
One- and 3-year recurrence-free survival rates were 95.5 and 95.5 % in PET− patients and 68.9 and 45.9 % in patients with 18F-FDG-avid HCC (P < 0.001). Only 3 of 66 PET− patients developed posttransplant HCC recurrence (4.5 %) as compared to 21 of 37 PET+ patients (56.8 %; P < 0.001).
In a subanalysis including PET+ patients (n = 37), total tumor diameter >10 cm (P = 0.047), G3 tumor (P = 0.037), LVI (P = 0.024), AFP level >400 IU/ml (P = 0.047), CIT >400 min (P = 0.044), TIT >500 min (P = 0.033), and WIT >50 min (P < 0.001) were associated with increased risk of HCC recurrence in univariate analysis. In multivariate Cox regression, only WIT >50 min remained as an independent risk factor for HCC recurrence (OR 15.5; 95 % CI 3.0–101.5; P < 0.001).
In this subset, recurrence-free survival rates at 1 and 3 years post-LT were 89.7 and 73.9 % in WIT ≤50 min, and 43.9 and 18.8 % in WIT >50 min (P < 0.001; Fig. 2a). In patients with 18F-FDG-non-avid HCC (n = 66), disease-free survival probabilities at 1 and 3 years post-LT were 100 and 100, and 80 and 80 % in WIT ≤ versus WIT >50 min, respectively (P < 0.001, Fig. 2b).
a In the subset of PET+ patients, 1- and 3-year recurrence-free survival rates were 89.7 and 73.9 % after LT with WIT ≤50 min, and 43.9 and 18.8 % following LT with WIT >50 min (P < 0.001). b In the subpopulation of PET− patients, posttransplant recurrence-free survival rates at 1 and 3 years post-LT were 100 and 100 % in WIT ≤50 min, and 80 and 80 % in WIT >50 min (P = 0.001)
Discussion
The present study demonstrates that prolongation of ischemia times is associated with a significantly increased risk of HCC recurrence in liver transplant patients. Apart from other clinical variables, such as AFP level, PET, and Milan status, WIT was identified as independent predictor of tumor-specific outcome, which is another novel result of our trial.
In order to improve prognosis of liver transplant patients with HCC, different pre- and posttransplant clinical approaches have been established in recent years [2–5]. It was only recently that the clinical relevance of surgical stress to promote tumor recurrence or metastasis moved into the focus of interest [10–13].
Surgical trauma by IRI is a very complex network of diverse molecular mechanisms and cellular interactions that are not yet fully understood [15, 20]. It consists of two sequential periods. Cold IRI is induced by cold organ flushing during retrieval operation and is maintained by cold liver storage. Warm IRI develops during in situ allograft revascularization. Although initial cellular targets of both IRI types might be different, they share a common mechanism in disease etiology, which is best described as inflammatory innate immune activation [15, 20]. It is characterized by activation of Kupffer cells and neutrophils, production of cyto- and chemokines, expression of adhesion molecules, and infiltration of circulating lymphocytes and monocytes [15, 20, 21]. The extent of IRI is exaggerated by prolongation of ischemia times and may result in elevated liver enzymes, biliary strictures, and impaired allograft function. Targeting IRI-related mechanisms is thus an important aspect in preventing early allograft failure, especially in the context of using marginal donor livers [15, 20].
There is accumulating evidence from experimental studies that molecular mechanisms of IRI are substantially involved in tumor vasculogenesis and engraftment of CTCs [10–14, 20–25]. Clinical data in this context are rare and inconsistent. Hepatic pedicle clamping did not adversely affect tumor-related survival in liver resection [26, 27]. However, liver allografts are exposed to a long-term surgical trauma by a sequence of CIT and WIT, which is in contrast to short-term warm vascular clamping during hepatectomy. Furthermore, risk of tumor recurrence is promoted by immunosuppressive therapy in the transplant setting, but not in case of liver resection. Partial liver allografts are by nature exposed to an intensified surgical stress induced by “small-for-size graft damage,” in addition to IRI [24]. Higher HCC recurrence rates after living donor liver transplantation as compared to deceased donor LT should thus be expected. However, currently available findings are inconclusive [28–31]. In contrast, recent results of LT using donors after cardiac death (DCD) provided some clinical evidence of a carcinogenic effect of IRI [32, 33]. Contrary to conventional donors after brain death (DBD), DCD liver allografts are subject to an additional WIT during the agonal period [32]. Therefore, these organs are susceptible to an intensified IRI, which may result in higher rates of hepatocellular dysfunction, biliary tract injury, and liver re-transplantation [32]. Croome et al. showed superior survival after LT for HCC by using DBD livers as compared to DCD allografts, which was beyond inherent inferiority related to DCD organs [33]. And just recently, Nagai and colleagues identified ischemia times as independent risk factors for post-LT HCC recurrence in tumors with vascular invasion [34].
Results of our study underline the prognostic importance of surgical stress in liver transplant patients with malignancy. Ischemia times were all significantly longer in patients with as compared to those without tumor relapse (Table 2). Prolonged WIT was identified as an independent predictor of tumor relapse (Table 4), and HCC recurrences occurred much earlier after extended than after limited WIT in our series. Moreover, early post-LT maximum AST levels were significantly higher in recipients with recurrent HCC (Table 2), which seems to emphasize on the association between IRI and carcinogenesis.
Although our study is hampered by a rather small sample size, a large study period, and its retrospective character, there are some interesting clinical implications that may be drawn from our data.
First, ischemia times should be reduced to a minimum, not only for reasons of allograft function but for tumor-specific considerations as well. This seems to have paramount importance for patients with 18F-FDG-avid tumors on pretransplant PET scanning (Fig. 2a), since extended WIT remained the only independent predictor of HCC recurrence in this special subpopulation.
Several transplant groups have recently described 18F-FDG-PET as useful diagnostic tool for identifying HCC with aggressive biological behavior [5–9]. Its prognostic significance seems to be triggered by a high correlation of increased FDG uptake with the presence of MVI and low tumor differentiation, which are both major determinants of posttransplant outcome [5–9, 17]. Currently available data suggest that patients with 18F-FDG-non-avid HCC are appropriate liver transplant candidates, independent from meeting the Milan criteria [5–9, 17]. However, experiences with PET evaluation in this context are still limited, and 18F-FDG-uptake data are not yet for standard incorporated into the selection process prior to LT [5]. Thus, patients with 18F-FDG-avid HCC may not automatically be excluded from LT. Instead, additional prognostic variables have to be identified.
The unfavorable impact of extended WIT on tumor-related outcome was particularly evident in patients with 18F-FDG-avid HCC (Fig. 2a), but less serious in PET− recipients (Fig. 2b). Tumor recurrence rates were 20 % in PET− recipients, but 88.2 % in PET+ patients following LT with extended WIT (P < 0.001). It has been recently demonstrated that the presence of unfavorable histopathologic features may be associated with higher blood levels of CTCs as compared to less aggressive tumors [35]. We therefore suppose the exaggerated risk of tumor relapse in PET+ versus PET− patients following extended WIT (Fig. 2a, b) to be triggered by higher amounts of circulating HCC cells. However, we have not performed CTC measurements, which is a drawback of our trial.
In contrast, patients with 18F-FDG-avid HCC were able to achieve an acceptable recurrence-free survival rate of 73.9 % at 3 years, if WIT remained limited (Fig. 2a). To our opinion, this outcome result would, in retrospect, not have been justified their exclusion from LT.
Although recommended by our data, additional reduction of ischemia times might be difficult in clinical reality. Cold ischemia time is mainly determined by logistic factors, such as location of retrieval operation and availability of operation facilities and staff. Warm ischemia time is less variable than CIT, but may be influenced by allograft size, the vessels’ anatomical structure, and, not least, the surgeons’ experiences. Apart from that, acceptance of a liver allograft is rather determined by medical priorities than by calculated ischemia times. Nevertheless, our data strongly suggest that expected ischemia times should play an important role in individual decision making, especially in patients with unfavorable tumor biology.
Second, targeting molecular mechanisms of hepatic IRI not only might improve allograft function but possibly reduces the risk of HCC recurrence. Post-LT maximum AST levels were significantly higher following WIT >50 min (618.5 IU/ml) than after limited WIT (366.2 IU/ml; P < 0.001), which stresses the correlation between ischemia times and IRI in our study. There are numerous experimental and clinical studies on pharmacological strategies for limiting hepatic IRI without, however, yet focusing on their possible anticancer efficacies [21].
And third, our data seem to implicate that, along with other clinical and histopathologic variables, ischemia times should be incorporated into the assessment of the patients’ individual oncological risk profile following LT. This, however, has to be further analyzed in a prospective approach.
In conclusion, results of our trial demonstrate that ischemia times are important risk factors for HCC recurrence following LT. Prolonged warm ischemia time was identified as an independent promoter of HCC recurrence, especially in patients with unfavorable tumor biology on pretransplant PET imaging. There should be attempts to further minimize ischemia times for improving outcome in liver transplant patients with HCC.
Abbreviations
- IRI:
-
Ischemia–reperfusion injury
- HCC:
-
Hepatocellular carcinoma
- LT:
-
Liver transplantation
- 18F-FDG:
-
18F-Fluoro-deoxy-glucose
- PET:
-
Positron emission tomography
- CIT:
-
Cold ischemia time
- WIT:
-
Warm ischemia time
- TIT:
-
Total ischemia time
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- AFP:
-
Alpha-fetoprotein
- HR:
-
Hazard ratio
- MELD:
-
Model for end-stage liver disease
- TACE:
-
Transarterial chemoembolization
- CsA:
-
Cyclosporine A
- Tac:
-
Tacrolimus
- AZA:
-
Azathioprine
- MMF:
-
Mycophenolate mofetil
- DRI:
-
Donor risk index
- OT:
-
Operation time
- EBL:
-
Estimated blood loss
- RBC:
-
Red blood cell
- MVI:
-
Microvascular invasion
- LVI:
-
Lymphovascular invasion
- STD:
-
Standard deviation
- CTC(s):
-
Circulating tumor cell(s)
- DCD:
-
Donor after cardiac death
- DBD:
-
Donor after brain death
- AST:
-
Aspartate aminotransferase
References
Mazzaferro V, Bhoori S, Sposito C, et al. Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transplant. 2011;17:44–57.
Ishizaki Y, Kawasaki S. The evolution of liver transplantation for hepatocellular carcinoma (past, present, and future). J Gastroenterol. 2008;43:18–26.
Koschny R, Schmidt J, Ganten TM. Beyond Milan criteria–chances and risks of expanding transplantation criteria for HCC patients with liver cirrhosis. Clin Transplant. 2009;23:49–60.
Cheah YL, Chow P. Liver transplantation for hepatocellular carcinoma: an appraisal of current controversies. Liver Cancer. 2012;1:183–189.
Kornberg A. Liver transplantation for hepatocellular carcinoma beyond Milan criteria: multidisciplinary approach to improve outcome. ISRN Hepatology 2014, Article ID 706945.
Kornberg A, Freesmeyer M, Bärthel E, et al. 18F-FDG-uptake of hepatocellular carcinoma on PET predicts microvascular tumor invasion in liver transplant patients. Am J Transplant. 2009;9:592–600.
Lee JW, Paeng JC, Kang KW, et al. Prediction of tumor recurrence by 18F-FDG PET in liver transplantation for hepatocellular carcinoma. J Nucl Med. 2009;50:682–687.
Lee SD, Kim SH, Kim YK, et al. (18)F-FDG-PET/CT predicts early tumor recurrence in living donor liver transplantation for hepatocellular carcinoma. Transpl Int. 2013;26:50–60.
Cho Y, Lee DH, Lee YB, et al. Does 18F-FDG positron emission tomography-computed tomography have a role in initial staging of hepatocellular carcinoma? PLoS ONE. 2014;9:e105679.
Zhang J, Shi ZL, Yang X, Yin ZF. Targeting of circulating hepatocellular carcinoma cells to prevent postoperative recurrence and metastasis. World J Gastroenterol. 2014;20:142–147.
Toso C, Mentha G, Majno P. Liver transplantation for hepatocellular carcinoma: five steps to prevent recurrence. Am J Transplant. 2011;11:2031–2035.
van der Bilt JD, Kranenburg O, Nijkamp MW, et al. Ischemia/reperfusion accelerates the outgrowth of hepatic micrometastases in a highly standardized murine model. Hepatology. 2005;42:165–175.
van der Bilt JD, Kranenburg O, Borren A, van Hillegersberg R, Borel RIH. Ageing and hepatic steatosis exacerbate ischemia/reperfusion-accelerated outgrowth of colorectal micrometastases. Ann Surg Oncol. 2008;15:1392–1398.
Tsuchiya Y, Sawada S, Yoshioka I, et al. Increased surgical stress promotes tumor metastasis. Surgery. 2003;133:547–555.
Teoh NC. Hepatic ischemia reperfusion injury: contemporary perspectives on pathogenic mechanisms and basis for hepatoprotection—the good, bad and deadly. J Gastroenterol Hepatol. 2011;26:180–187.
Roayaie K, Feng S. Allocation policy for hepatocellular carcinoma in the MELD era: room for improvement? Liver Transplant. 2007;13:36–43.
Kornberg A, Küpper B, Tannapfel A, et al. Patients with non-[18 F]fludeoxyglucose-avid advanced hepatocellular carcinoma on clinical staging may achieve long-term recurrence-free survival after liver transplantation. Liver Transplant. 2012;18:53–61.
Parrilla P, Sanchez-Bueno F, Figueras J, et al. Analysis of the complications of the piggy-back technique in 1112 liver transplants. Transplantation. 1999;31:2388–2389.
Ijtsma AJ, van der Hilst CS, de Boer MT, et al. The clinical relevance of the anhepatic phase during liver transplantation. Liver Transplant. 2009;15:1050–1055.
Klune JR, Tsung A. Molecular biology of liver ischemia/reperfusion injury: established mechanisms and recent advancements. Surg Clin N Am. 2010;90:665–677.
Zhai Y, Petrowsky H, Hong JC, Busuttil RW, Kupiec-Weglinski JW. Ischemia-reperfusion injury in liver transplantation—from bench to bedside. Nat Rev Gastroenterol Hepatol. 2013;10:79–89.
Lim C, Broqueres-You D, Brouland JP, et al. Hepatic ischemia-reperfusion increases circulating bone-marrow-derived progenitor cells and tumor growth in a mouse model of colorectal liver metastases. J Surg Res. 2013;184:888–897.
Doi K, Horiuchi T, Uchinami M, et al. Hepatic ischemia-reperfusion injury promotes liver metastasis of colon cancer. J Surg Res. 2002;105:243–247.
Shih KC, Man K. Small-for-size liver graft injury—impact on tumor behaviour. Transplant Rev. 2010;24:1–10.
Oldani G, Crowe LA, Orci LA, et al. Pre-retrieval reperfusion decreases cancer recurrence after rat ischemic liver graft transplantation. J Hepatol. 2014;61:278–285.
Xia F, Lau WY, Xu Y, Wu L, Qian C, Bie P. Does hepatic ischemia–reperfusion injury induced by hepatic pedicle clamping affect survival after partial hepatectomy for hepatocellular carcinoma? World J Surg. 2013;37:192–201.
Giuliante F, Ardito F, Pulitano C, et al. Does hepatic pedicle camping affect disease-free survival following liver resection for colorectal metastases? Ann Surg. 2010;252:1020–1026.
Lo CM, Fan ST, Liu CL, Chan SC, Ng IO, Wong J. Living donor versus deceased donor liver transplantation for early irresectable hepatocellular carcinoma. Br J Surg. 2007;94:78–86.
Fisher RA, Kulik LM, Freise CE, et al. Hepatocellular carcinoma recurrence and death following living and deceased donor liver transplantation. Am J Transplant. 2007;7:1601–1608.
Ling C, Ng KTP, Shao Y, et al. Posttransplant endothelial progenitor cell mobilization via CXCL10/CXCR3 signaling promotes liver tumor growth. J Hepatol. 2014;60:103–109.
Liang W, Wu L, Ling X, et al. Living donor liver transplantation versus deceased donor liver transplantation for hepatocellular carcinoma: a meta-analysis. Liver Transpl. 2012;18:1226–1236.
Monbaliu D, Pirenne J, Talbot D. Liver transplantation using Donation after Cardiac Death donors. J Hepatol. 2012;56:474–485.
Croome KP, Wall W, Chandok N, Beck G, Marotta P, Hernandez-Alejandro R. Inferior survival in liver transplant recipients with hepatocellular carcinoma receiving donation after cardiac death liver allografts. Liver Transpl. 2013;19:1214–1223.
Nagai S, Yoshida A, Facciuto M, et al. Ischemia time impacts recurrence of hepatocellular carcinoma following liver transplantation. Hepatology. 2014. doi:10.1002/hep.27358.
Xu W, Cao L, Chen L, et al. Isolation of circulating tumor cells in patients with hepatocellular carcinoma using a novel cell separation strategy. Clin Cancer Res. 2011;17:3783–3793.
Acknowledgments
The authors have no financial support to declare.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kornberg, A., Witt, U., Kornberg, J. et al. Extended Ischemia Times Promote Risk of HCC Recurrence in Liver Transplant Patients. Dig Dis Sci 60, 2832–2839 (2015). https://doi.org/10.1007/s10620-015-3541-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3541-z