Abstract
Background
The Helicobacter pylori eradication rate with standard triple therapy is very low. H. pylori is known to require the nickel-containing metalloenzymes urease and NiFe-hydrogenase to survive at the low pH environment in the stomach.
Aim
To compare the H. pylori eradication rate of a nickel free-diet associated with standard triple therapy and standard triple therapy alone as the first-line regimen.
Methods
Fifty-two sex- and age-matched patients at the first diagnosis of H. pylori infection were randomized 1:1 into two different therapeutic schemes: (1) standard LCA (26 patients): lansoprazole 15 mg bid, clarithromycin 500 mg bid and amoxicillin 1,000 mg bid for 7 days with a common diet; (2) standard LCA plus a nickel free-diet (NFD-LCA) (26 patients). Patients followed 30 days of a nickel-free diet plus a week of lansoprazole 15 mg bid, clarithromycin 500 mg bid and amoxicillin 1,000 mg bid starting from day 15 of the diet.
Results
All patients completed the study. A significantly higher eradication rate was observed in the NFD-LCA group (22/26) versus LCA group (12/26) (p < 0.01). Only a few patients (9 of 52) reported the occurrence of mild therapy-related side effects, without any significant differences between the two groups.
Conclusions
The addition of a nickel-free diet to standard triple therapy significantly increases the H. pylori eradication rate. The reduction of H. pylori urease activity due to the nickel-free diet could expose the bacterium to gastric acid and increase H. pylori's susceptibility to amoxicillin. Further studies are necessary to confirm this preliminary result.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori (H. pylori) is a gram-negative bacterium characterized by specific microbiological features allowing its survival inside the stomach and duodenum, where it represents a major human pathogen. Urease activity is a major feature of all H. pylori strains, conferring resistance to gastric acidity and allowing gastric mucosa colonization [1, 2]. The enzyme urease catalyzes the hydrolysis of urea, which is normally present in the gastric juices, in ammonia and bicarbonate (NH3 and CO2) [3], two strong alkalis that neutralize the hydrochloric acid, maintaining the bacterium's intracellular neutrality. The highest concentration of hydrogen ions in the gastric environment is used by another enzyme, hydrogenase, which oxidizes the molecular hydrogen to produce energy useful for bacterial survival [4] and allowing an efficient colonization of the stomach.
Since H. pylori is able to resist all gastric mucosal protective mechanisms, antibiotics are commonly used in order to eradicate it from the gastroduodenal tract. On this subject, the Mastricht III European Guidelines recommend a combination of proton pump inhibitors (PPIs) or ranitidine bismuth citrate (RBC) with two antibiotics to be chosen from among amoxicillin, clarithromycin or metronidazole for 7–14 days as a first-line regimen. Nevertheless, recent studies have clearly shown that even with the recommended treatment regimens, approximately 20 % of patients fail to obtain H. pylori eradication, and in some countries this phenomenon has reached unacceptable levels [5].
H. pylori treatment failure may be due to different causes, such as bacterial resistance and patient-related factors; although in most cases different factors act simultaneously in reducing antibiotic therapy efficacy in the same patient, the most important is the increased H. pylori resistance to clarithromycin or other antibiotics [5]. Antibiotic resistance rates are increasing worldwide [8], and the cure rate following standard eradication therapies is distinctly lower when either clarithromycin or metronidazole resistance is present [6]. The global clarithromycin resistance rate in Europe increased from 9 % in 1998 [6] to 17.6 % in 2008–2009 [7].
In recent years, several studies have analyzed the molecular and genomic characteristics of H. pylori possibly playing a role in antibiotic resistance. Interestingly, the expression of virulence factors, which are necessary for bacterial infection, is often stimulated at the transcriptional level by some environmental factors, such as metal ions (Fe21, Ni21, Cu21) [8]. On this view, the role of iron and of genes involved in its metabolism has been revealed to be essential in the processes of electron transport, energy metabolism, synthesis of DNA and pathogenesis of H. pylori. Similarly, nickel has a crucial role in activating two enzymes, both necessary for efficient colonization of H. pylori: urease, which is formed by two subunits named UreA and UreB activated by the incorporation of the metal cofactor nickel, and hydrogenase, an enzymes with a [NiFe]-bimetallic center at the active site [9]. The bacterial protein Fur and a homolog of the repressor NikR represent two transcriptional regulators involved in the homeostasis of metals. Fur is involved in the resistance to acidic conditions and in the induction of genes from nickel urease, while NikR could act as a main regulator for the adaptation in acidic conditions by the direct transcriptional activation of the gene ureAB and by activation of other genes regulated by pH through a cascade of transcriptional regulators that involves the Fur repressor.
The human body contains traces of nickel mainly ingested by food, which is mainly concentrated in the pancreas and bone, but also in saliva, sweat and serum. While nickel is naturally abundant in all types of food [10], it does not appear to be essential for humans. Since there is no “competition” for nickel between the host and bacteria, usually high levels of nickel are available for H. pylori.
Based on this observation, we hypothesized that reducing the bioavailability of nickel may significantly impair H. pylori's survival in the gastric environment and increase its susceptibility to the antibiotic therapy. Therefore, we designed a study aimed at comparing the eradication rates of a standard triple therapy obtained in patients following a normal diet and in subjects on a nickel-free diet.
Materials and Methods
Study Design
Eighty-two consecutive patients (38 males, 44 females, mean age 42) were enrolled from January 2011 to January 2012 at our Gastroenterology Division. All patients had been diagnosed for H. pylori infection by the 13C-urea breath test (UBT) for the first time, based on the Maastricht guideline recommendations [5]. After the initial screening, we excluded five patients with a systemic nickel allergy and five subjects with other known food allergies; three patients with drug allergies, two with severe liver disease, two with neoplasms, one with severe kidney failure and 12 who had recently used antimicrobial agents, bismuth compounds, proton pump inhibitors (PPI) or H2 receptor antagonists. We finally enrolled 52 patients (22 males, 30 females, mean age 38 ± 6.) who were randomized 1:1 into two different therapeutic schemes:
-
1.
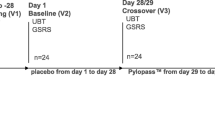
Standard LCA (26 patients): lansoprazole 15 mg bid, clarithromycin 500 mg bid and amoxicillin 1,000 mg bid for 7 days with a common diet (Fig. 1) (according to the Mastricht III Guidelines).
-
2.
Standard LCA plus a nickel free-diet (NFD-LCA) (26 patients): Patients followed a 30-day nickel-free diet plus a week of lansoprazole 15 mg bid, clarithromycin 500 mg bid and amoxicillin 1,000 mg bid starting from day 15 of the diet (Fig. 2).
Compliance and occurrence of adverse effects were assessed by a validated questionnaire, administered at enrollment and at the end of the therapeutic period (day 30) [11]. Written informed consent was obtained for each patient. H. pylori eradication was confirmed by the 13C-urea breath test performed 4 weeks after the end of the therapeutic regimen.
13C-Urea Breath Test
The UBT was performed after a fasting period of at least 6 h. After collection of a baseline sample in a vacutainer vial, a solution containing 75 g of 13C labeled urea and citric acid was administered to the patient. All subjects then sat in the waiting room without eating, drinking or smoking, and exhaled air samples were re-collected 30 min after the ingestion of the above-mentioned solution. Samples were then analyzed by a mass spectrometer allowing the measurement of the amount of 13CO2 in respect to the total expired CO2. We considered all patients in whom the delta over baseline was higher than 3.5 infected by H. pylori.
Patch Tests
All patients underwent a skin-patch test with 5 % nickel sulfate (NiSO4) in petrolatum (Hermal, Hamburg, Germany) in our allergy unit according to the International Contact Dermatitis Research Group Guidelines (ICDRG) [12]. Patch tests were evaluated 48 and 72 h after their application and were considered positive if an eczematous-vesicular reaction occurred at the contact site with the allergen; the intensity was assessed according to the following criteria [13]:
-
(1)
± faint, non-palpable erythema;
-
(2)
+ palpable erythema;
-
(3)
++ strong infiltrate, numerous papules, and vesicles present strong reaction;
-
(4)
+++ coalescing vesicles, bullae or ulceration, and an extreme erythematous reaction.
Questionnaire
Each subject received a self-administered questionnaire, slightly modified from de Boer et al. [11], to record the development of symptoms such as nausea, vomiting, abdominal pain, taste disturbances, diarrhea, constipation and skin rash, from nil to severe. Severity scores were assigned as follows: nil (score 0, no side effects), mild (score 1, could be disregarded), moderate (score 2, bad enough to call a physician, but treatment could be continued and was tolerated) and severe (score 3, interfering with activity at work, requiring discontinuation of the therapy).
At enrollment and the end of therapy, each patient completed the validated dyspepsia questionnaire from Buckley et al. [14] to obtain information on gastrointestinal (GI) symptoms (pyrosis, epigastric pain, belching, bloating, halitosis and nausea). A pill count was also assessed at the beginning and end of the therapy.
Nickel-Free Diet
Due to its ubiquitous nature, it is not possible to completely avoid oral intake of nickel. Nevertheless, all foods with a high nickel content, such as apricots, figs, pears, plums, raisins, pineapples, peanuts, cocoa, almonds, walnuts, hazelnuts, lobster, mussels, oysters, mussels, plaice, asparagus, cauliflower, carrots, cabbage, onions, beans, lentils, potatoes, peas, tomatoes, spinach, margarine and corn, were strictly prohibited for 4 weeks [15, 16]. Furthermore, patients were asked to avoid the use of stainless-steel utensils to reduce nickel contamination during cooking.
Statistical Analysis
Both PP and ITT analyses were performed. For the purpose of the analyses, the incidence of side effects was considered a binomial variable (present–absent). Any “side effect” was considered absent if the subject reported the same complaint at the baseline visit as assessed by the questionnaire. To detect differences in H. pylori eradication rates and the incidence of side effects, the χ2 and Fisher exact tests were used.
Results
All patients completed the study; therefore, the intention-to-treat analysis matched the per protocol analysis. A significantly higher eradication rate was obtained in the NFD-LCA group compared to the LCA group (22 of 26 patients vs. 12 of 26 patients; p < 0.01) (Fig. 3).
Overall patient compliance with both eradicating schemes was similar, with all patients completing the prescribed therapy. Both treatments were very well tolerated, and no major side effects were reported. Only a few patients (9 of 52) reported the occurrence of mild therapy-related side effects, without any significant differences between the two groups. Among the LCA group, two patients reported nausea and two diarrhea, while the same side effects were recorded in three and two patients in the NFD-LCA group, respectively.
Discussion
H. pylori infection is the main pathogen of the gastroduodenal tract and a well-recognized cause of several diseases, ranging from chronic gastritis to gastric cancer. While its prevalence is declining in developed countries, it remains an infection with worldwide spread with a definite morbidity and mortality. Recent data have clearly shown that the efficacy of the first-line eradicating regimens is significantly decreased and is far from 80 %, which represents the lower acceptable success rate for an infectious disease. Besides changing the antibiotics or their composition or the duration of the treatment, which in turn may increase the occurrence of side effects, reducing compliance, looking for other strategies able to increase the eradication rates to more acceptable levels has become mandatory.
Our study showed for the first time that a nickel-free diet can increase the H. pylori eradication rate of the standard triple therapy. Interestingly, nickel has been shown to be crucial in H. pylori survival as it is involved in the expression of two enzymes, urease and hydrogenase. While urease is essential for H. pylori's survival against gastric acidity, hydrogenase is fundamental for energy intake. Based on the results of our study, we can hypothesize that a nickel-free diet may increase H. pylori's susceptibility to antibiotics through the depletion of urease and hydrogenase, which in turn are essential for colonization of the gastric mucosa.
An interesting finding of this study is that patients treated with standard clarithromycin-based triple therapy and NFD reported an eradication rate of 84 %, which is higher than the expected 75 %, considering a 25 % primary resistance to clarithromycin. One of the possible explanations is that NFD alone or in combination with amoxicillin may increase the eradication rate, irrespective of clarithromycin resistance. Even though we have no data on this matter, we strongly believe that this may represent an issue to be addressed in the near future.
Another finding of our study is the low eradication rates obtained by the clarithromycin-based triple therapy. There are two possible explanations for this. First, we used a low-dose PPI triple therapy (lansoprazole 15 mg bid), based on previous adopted guidelines, which is known to be associated with reduced eradication rates [17]. Second, since the immigration rate in Rome is very high and most of our patients were immigrants, the eradication rates of a first-line chlaritromycin-based triple therapy in immigrants were lower and comparable to our findings, as demonstrated by an Italian study [18]. In this matter, our original aim was to verify whether an NFD can increase the eradication rate, irrespective of the PPI dosage.
Conclusions
In conclusion, our study shows for the first time that an NFD significantly enhances the eradication rate of a standard anti-H. pylori triple therapy, possibly by depleting the enzymes urease and hydrogenase, reducing H. pylori's survival. Considering the importance of this issue and the small number of patients enrolled in our study, further studies are needed in order to confirm our findings and to assess the effect of NFD on the efficacy of each single antibiotic composing the standard eradication treatment.
References
Bijlsma JJ, Lie-A-Ling M, Nootenboom IC, et al. Identification of loci essential for the growth of Helicobacter pylori under acidic conditions. J Infect Dis. 2000;182:1566–1569.
Stingl K, Altendorf K, Bakker EP. Acid survival of Helicobacter pylori: how does urease activity trigger cytoplasmic pH homeostasis? Trends Microbiol. 2002;10:70–74.
Sachs G, Scott DR, Wen Y. Gastric infection by Helicobacter pylori. Curr Gastroenterol Rep. 2011;13:540–546.
Maier RJ, Fu C, Gilbert J, et al. Hydrogen uptake hydrogenase in Helicobacter pylori. FEMS Microbiol Lett. 1996;141:71–76.
Malfertheiner P, Megraud F, O’Morain C, et al. Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 2007;56:772–781.
Glupczynski Y, Mégraud F, Lopez-Brea M, Andersen LP. European multicentre survey of in vitro antimicrobial resistance in Helicobacter pylori. Eur J Clin Microbiol Infect Dis. 2001;20:820–823.
Megraud F, Coenen S, Versporten A, et al. Helicobacter pylori resistance to antibiotics in Europe and its relationship to antibiotic consumption. Gut. 2013;62:34–42.
Bury-Moné S, Thiberge JM, Contreras M, et al. Responsiveness to acidity via metal ion regulators mediates virulence in the gastric pathogen Helicobacter pylori. Mol Microbiol. 2004;53:623–638.
Burne RA, Chen YY. Bacterial ureases in infectious diseases. Microbes Infect. 2000;2:533–542.
Denkhaus E, Salnikow K. Nickel essentiality, toxicity, and carcinogenicity. Crit Rev Oncol Hematol. 2002;42:35–56.
de Boer WA, Thys JC, Borody TJ, et al. Proposal for use of a standard side effect scoring system in studies exploring Helicobacter pylori treatment regimens. Eur J Gastroenterol Hepatol. 1996;8:641–643.
Calnan CD, Fregert S, Magnusson B. The international contact dermatitis research group. Cutis. 1976;18:708–710.
Czarnobilska E, Jenner B, Kaszuba-Zwoinska J et al. Contact allergy to nickel: patch test score correlates with IL-5, but not with IFN-gamma nickel-specific secretion by peripheral blood lymphocytes. Ann Agric Environ Med. 2009;16:37–41, 51.
Buckley MJ, Scanlon C, McGurgan P, O’Morain CA. A validated dyspepsia symptom score. Ital J Gastroenterol Hepatol.. 1997;29:495–500.
Minelli M, Schiavino D, Musca F, et al. Oral hyposensitization to nickel induces clinical improvement and a decrease in TH1 and TH2 cytokines in patients with systemic nickel allergy syndrome. Int J Immunopathol Pharmacol. 2010;23:193–201.
Schiavino D, Nucera E, Alonzi C, et al. A clinical trial of oral hyposensitization in systemic allergy to nickel. Int J Immunopathol Pharmacol. 2006;19:593–600.
Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht IV/florence consensus report. Gut. 2012;61:646–664.
Gatta L, Di Mario F, Vaira D, et al. Helicobacter pylori eradication: are we really all equal? A controlled study in native and immigrant population. Intern Emerg Med. 2011;6:35–39.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Campanale, M., Nucera, E., Ojetti, V. et al. Nickel Free-Diet Enhances the Helicobacter pylori Eradication Rate: A Pilot Study. Dig Dis Sci 59, 1851–1855 (2014). https://doi.org/10.1007/s10620-014-3060-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3060-3