Abstract
Background
Dysphagia, regurgitation, and chest pain are common achalasia, with a variable report of pulmonary symptoms possibly due to micro-aspiration. Pneumatic dilation (PD) may improve pulmonary function. Data on pulmonary dysfunction among achalasia patients are scanty, and the effect of PD is unknown.
Aim
To evaluate pulmonary dysfunction in patients with achalasia based on clinical and radiologic evaluation and spirometry and to study the effect of PD at 1-month follow-up.
Methods
Patients with achalasia (diagnosed using high-resolution manometry and the Chicago classification) were evaluated prospectively by spirometry before (n = 38) and 1 month after PD (n = 31). All patients received a chest X-ray, and patients with respiratory abnormality before PD received high-resolution computed tomography of the thorax.
Results
Of the 38 patients, 17 and 21 had type I and II achalasia, respectively. The respiratory symptoms, such as pharyngeal symptoms [27/38 (71 %) vs. 8/31 (26 %); P = 0.0001], cough [23/38 (60.5 %) vs. 5/31 (16 %), P = 0.0001], and dyspnea [8/38 (21 %) vs. 0/31 (0 %), P = 0.006], improved after treatment with PD. Spirometry showed abnormalities in 17/38 (45 %) patients before and in 8/15 (53 %) after PD. Median FEV1, FVC, PEFR, and percentage of predicted MEF25–75, improved from 78 % (36–85), 74 % (48–100), 62 % (18–72), and 48 % (15–66) before to 83 % (58–94), 86 % (55–99), 69 % (38–81), and 59 % (33–78) after PD, respectively (P < 0.05 for all).
Conclusion
Respiratory symptoms and spirometry abnormalities are common in patients with achalasia and improved after successful PD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Achalasia is one of the most common esophageal motility disorders causing dysphagia [1]. It is characterized by impaired peristalsis in the esophageal body and failure of relaxation of the lower esophageal sphincter (LES). A proportion of patients with achalasia may present primarily with respiratory symptoms, which may cause diagnostic difficulty [2, 3]. Common pulmonary symptoms in achalasia are cough, which is frequently nocturnal, dyspnea, choking, recurrent respiratory infections, wheezing, stridor, and even acute respiratory obstruction [4–10]. Mechanical obstruction leading to stridor and acute tracheal obstruction are serious and life-threatening complications [11]. In addition, pharyngeal and laryngeal symptoms, such as sore throat, globus sensation, and hoarseness, may also occur [12, 13].
Respiratory dysfunction in achalasia may result from micro- and macro-aspiration [4] of the contents of the dilated esophagus. Such aspiration events commonly occur during the night, when the patient is in a supine position. The severity of the pulmonary dysfunction is likely to depend on disease duration, frequency of aspiration episodes, and nature of the aspirated material [14]. Recurrent aspiration episodes over a long period of time may lead to serious consequences, such as diffuse aspiration bronchiolitis, obliterative bronchiolitis, aspiration pneumonia, lung abscess, empyema, and even lung fibrosis, some of which may be irreversible [14–16]. Early detection and appropriate treatment may prevent long-term respiratory morbidity.
Pneumatic dilation (PD), which lowers LES pressure, is a well-established modality for the management of achalasia [17]. Since esophageal emptying is improved after PD [18], it may reduce the risk of aspiration. Timed barium esophagogram (TBE) is a good modality to quantify the response of PD in terms of esophageal emptying [19, 20]. Whether this benefit translates into improvement in respiratory symptoms and lung injury is not fully known. Also, data on respiratory symptoms and the exact pattern of spirometry abnormalities in achalasia are scanty [8, 12]. Moreover, the effect of PD on pulmonary dysfunction is not known. Accordingly, we undertook a study with the following aims: (1) to evaluate the occurrence and spectrum of pulmonary dysfunction in patients with achalasia based on clinical and radiologic evaluations and spirometry and (2) to study the effect of PD on these variables at the 1-month follow-up.
Methods
Study Protocol
Consecutive patients (age ≥18 years) with achalasia were recruited for this prospective study over 1-year period (August 2011 to July 2012). Patients were evaluated using a standard questionnaire (Eckardt’s score) [21]. Esophagogastroduodenoscopy was performed in all patients to rule out esophago-gastric malignancy. The diagnosis and type of achalasia (Chicago classification) [22, 23] was established by high-resolution manometry (HRM) using a 16-channel water-perfused catheter. A pulmonary physician then evaluated all patients with confirmed diagnosis of achalasia for respiratory symptoms, including a spirometry and chest X-ray. Chest computed tomography (CT) with expiratory films was performed in those patients with abnormal spirometry. Esophageal emptying was evaluated by TBE, performed as per a standard protocol [24]. Patients with mega-esophagus (esophageal width >6 cm), pregnant women, chronic smokers, and those with prior history of PD, Heller’s myotomy, significant chronic respiratory illnesses (e.g., asthma, obstructive airway disease), pulmonary tuberculosis) were excluded. Patients were treated by PD according to a standard protocol [25]. Each patient was re-evaluated based on Eckardt’s score, HRM and TBE parameters, respiratory symptoms, chest X-ray (if previous X-ray was abnormal), and spirometry again at 1 month following PD. The study protocol was approved by the Ethics Committee of the Institute, and all patients gave informed consent.
Clinical Evaluation Including Assessment of Pulmonary Symptoms
All patients were evaluated for duration and severity of all symptoms, previous treatment obtained, co-morbid illnesses, and feasibility of PD. Baseline demographics, including prior history of respiratory diseases, were recorded. Dysphagia, chest pain, regurgitation, and weight loss were assessed according to Eckardt’s score (first 3 symptoms scored as 0 = none, 1 = occasional, 2 = daily, 3 = at each meal). Weight loss was scored as 0 = none, 1 = <5 kg, 2 = 5–10 kg, 3 = >10 kg. The maximum possible score was 12, and a score <3 on follow-up was considered to be indicative of clinical response. Respiratory symptoms and signs, such as cough, nocturnal cough, sputum production, dyspnea, recurrent chest infections, wheezing, stridor, acute respiratory obstruction, sore throat, and hoarseness, and the results of the chest physical examination were recorded by a pulmonologist before and after PD; the pulmonologist was unaware of the results of the gastrointestinal evaluation, including Eckardt’s score, esophagogastroduodenoscopy findings, HRM and TBE parameters, and treatment with PD. The same questionnaire for the presence/absence of symptoms and signs was administered before and after PD for qualitative evaluation. Chest X-ray (posterior–anterior view) and spirometry results were obtained in all patients.
High-Resolution Esophageal Manometry
Esophageal manometry was performed using a water perfusion system (G.S. Hebbard system, Australia). Drugs that might interfere with esophageal motility and LES pressure (prokinetics, calcium channel blockers, anti-cholinergics) were discontinued at least 7 days prior to the study. After an overnight fast, an HRM catheter, smeared with lubricating jelly, was passed trans-nasally without any sedation or anaesthesia into the stomach while the patient was in a supine position. Intra-gastric pressure was used as the baseline for all pressure measurements. On HRM, LES was located as a zone of high pressure in the Clouse plot. Patients were given ten wet swallows of 5 mL of water, with a 15–30-s interval between each swallow, to assess esophageal body motility and LES relaxation.
Achalasia was diagnosed on HRM using standard criteria [22]. These patients were further sub-typed according to the dominant characteristics of distal esophageal pressurization (the isobaric contour) after swallowing, set at 30 mmHg and a mean integrated relaxation pressure (IRP) [26]. Type I achalasia was defined as “no distal esophageal” pressurization of >30 mmHg in eight or more of the ten wet swallows; type II as pan-esophageal pressurization to >30 mmHg in at least two of the ten wet swallows; type III (spastic) as preserved fragments of distal peristalsis or premature (spastic) contractions in two or more of the ten swallows [22]. The value of IRP had to be >10 mmHg to diagnose type I achalasia and >15 mmHg to diagnose type II and III achalasia [23].
All manometry analyses were performed using “Trace 1.2” software applied to the data tracings viewed in the color pressure topography mode and referenced to intra-gastric pressure (G.S. Hebbard system, Australia). The same technique was used for both pre- and post-PD manometry.
Timed Barium Esophagogram
The TBE was performed with the same technique [24] in all patients after HRM using 150 mL of 45 % w/v barium suspension (Microbar suspension; Eskay, Mumbai, India). Still images were obtained in the left posterior oblique standing position at 1, 5 and 10 min after completing the swallow (Axiom Icons-R200; Siemens, Munich, Germany). The maximum height and width of the barium column in all these images were measured. The same protocol was used for repeat TBE, done at 1 month after PD.
Spirometry
All patients with achalasia were evaluated by the pulmonologist for pulmonary function tests (PFTs) by spirometry. Spirometry was performed using a dry rolling seal spirometer (model 2010; Ganshorn Medizin Electronic GmbH, Niederlauer, Germany; software version LF 8.5). A minimum of three acceptable and reproducible maneuvers were recorded by an experienced technician using the guidelines of the American Thoracic Society (ATS) [27]. Spirometry indices like forced vital capacity (FVC), forced expiratory ventilation in 1 s (FEV1), FEV1/FVC ratio, mid expiratory flow (MEF25–75), and peak expiratory flow rate (PEFR) were recorded. The pulmonary function of each patient was assessed according to the absolute lung volumes on spirometry in reference to the lower limit of normal (LLN) for that age, height, and gender. The LLN for each of the above variables was calculated as the difference between the predicted value and 1.645-fold the standard error of the estimate of the relevant regression equation [28]. The patients were categorized for pulmonary abnormalities according to the algorithm shown in Fig. 1. Small airway disease was defined as a normal FEV1, FVC and FEV1/FVC ratio in association with a reduction of the MEF25–75 to <60 % of the predicted value. The diffusion capacity of the lung for carbon monoxide (DLCO) was measured by the single breath test (model 2010; Ganshorn Medizin Electronic GmbH; version Power Cube-Diffusion, software LF8) in all patients as per standardized ATS guidelines [29].
Algorithm for the diagnosis of pulmonary function test (PFT) abnormality on spirometry. The simplified algorithm according to American Thoracic Society (ATS) guidelines was used to assess lung function in achalasia patients. It presents classic patterns for various pulmonary disorders. FEV 1 The forced expiratory ventilation in 1 s/forced vital capacity ratio (FEV 1 /FVC) and FVC were considered first in comparison to lower limit of normal (LLN). MEF 25–75 Mid expiratory flow rate
Pneumatic Dilation
After complete baseline evaluation, PD was performed in fasting state using a Rigiflex balloon dilator (Microvasive, Milliford, MA). Most of the PD procedures were performed as daycare procedures under endoscopic guidance without fluoroscopy. Balloon sizes used for initial PD were 30 mm for females and 35 mm for males based on our previous study findings [25]. The dilator was passed into the stomach over a guide wire placed endoscopically. The dilator was positioned under endoscopic vision such that it was placed across the gastro-esophageal junction. The balloon was then inflated for 60 s at 6–8 psi. The patients were observed on the day of dilation for pain, fever, or any complication. A normal diet was allowed commencing on the day following dilation.
Follow-Up
All of the patients were re-evaluated after 1 month of PD in the Luminal Gastroenterology Clinic of the Department of Gastroenterology. Clinical scoring (Eckardt’s score), HRM, and TBE were repeated. The evaluation of respiratory symptoms and spirometry were repeated by the pulmonologist using the same protocol.
Evaluation of Result of Dilation
Clinical response was defined as an Eckardt’s score of <3 at the 1-month follow-up. Response according to HRM and TBE was defined as a “decrease in LES pressure to <22.5 mmHg” and “a more than a 50 % reduction in the barium column on a 5-min film,” respectively, as shown in our previous studies [25, 30].
Statistical Analysis
Continuous unpaired and paired data were compared using the Mann–Whitney U and Wilcoxon rank-sum tests, respectively. Categorical variable were compared using Fisher’s exact test. Data were analyzed using the statistical package SPSS (version 15.0 for Windows; SPSS, Chicago, IL), and P values of <0.05 were considered to be significant.
Results
Of the 46 consecutive patients with achalasia initially screened, eight were excluded due to secondary achalasia or mega-esophagus or for declining to consent (Fig. 2). Table 1 shows the pre-PD baseline patient characteristics. Of the 38 patient ultimately enrolled in the study, [20 (53 %) males; median age 34.5 years, range 18–62 years] who underwent PD, one required urgent surgery due to perforation. At the 1-month follow-up, 31 patients were re-evaluated for response to PD, respiratory symptoms, and PFTs, and six had been lost to follow-up.
Schematic summary of the protocol and exclusions. Achalasia was confirmed after high-resolution manometry (HRM) in 46 patients. Before pneumatic dilation (PD), 8 patients were excluded from the study for the reasons as shown. After PD, 31 patients were re-assessed after 1 month; 1 patient was excluded from analysis as he required surgery and 6 were lost to follow up. TBE Timed barium esophagogram
Baseline Characteristics
Of the 38 patients entering the study, type I and type II achalasia was diagnosed in 17 (45 %) and 21 (55 %) patients, respectively; no patient had type III achalasia. All patients had an IRP of >15 mmHg (Table 3). There was no significant difference in age, duration of dysphagia, and body mass index between the two patient groups (Table 1). Dysphagia was the most common presenting symptom (100 %) followed by regurgitation, weight loss and chest pain, occurring in 30 (79 %), 18 (47 %), and 11 (29 %) patients, respectively. Median duration of dysphagia was 36 (range 4–180) months. Grade 3 dysphagia was present in most patients in both groups [14/17 (82 %) and 17/21 (81 %) in type I and II, respectively].
Clinical Presentation
Pharyngeal symptoms, such as excessive throat clearing, sore throat, hoarseness and post-nasal drip, were collectively the commonest symptoms occurring in 27 (71 %) patients. The next most common symptom was cough, present in 23 (60.5 %) patients, of which 19 (50 %) had both daytime as well as nocturnal cough. Dyspnea (8/38, 21 %) and wheezing (3/38, 8 %) were the other respiratory symptoms. Abnormal findings on chest auscultation (rhonchi or crepitations) were present in 9/38 (24 %) patients. Regurgitation and respiratory symptoms were more common among type I achalasia patients while chest pain was more frequent in type II achalasia patients (Table 2). The median duration of respiratory symptoms was 12 (range 1–72) months, which was shorter than that of dysphagia (36 months, range 4–180 months).
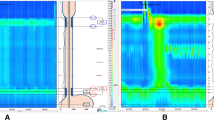
Objective Pulmonary and Esophageal Assessment
Seventeen of the 38 (44.7 %) patients had abnormal spirometry findings before PD; these tended to be commoner among patients with type I (10/17, 59 %) than type II achalasia (7/21, 33 %) (P = 0.09). PFT abnormalities were classified into restrictive (7/38, 18 %), small airway (6/38, 16 %), obstructive (2/38, 5 %), and mixed types (2/38, 5 %). Chest X-rays were normal in all except four of the 38 (10.5 %) patients (Table 3). Radiography findings included right basal consolidation, bilateral, or right-sided non-homogenous opacities. High-resolution CT scans of the thorax were performed in 17 patients who had abnormal PFT; the scans showed abnormal findings in 12 of these patients (70.6 %), inclduing ground glass opacity with mosaic attenuation, centrilobular nodules with a tree-in-bud pattern (Fig. 3), septal thickening with mosaic attenuation, and necrotizing pneumonia (Fig. 4). Tracheal compression with dilated esophagus (Fig. 5) was evident in two patients on the CT scan. The frequency of abnormal findings on the chest X-ray was comparable among patients with type I and II achalasia. Similarly, there was no significant difference in the median height (128 and 109 mm) and width (82 and 35 mm) of the barium column in the TBE at the 5-min film between type I and type II achalasia.
Effect of PD
Following PD, 24/31 (77 %) patients had clinical response (Table 3) as evidenced by a reduction in the Eckardt’s score from a median of 7 (range 4–11) to 2 (0–5). Respiratory abnormalities, such as pharyngeal symptoms, cough, and dyspnea, also improved following successful PD (Table 2). Similarly, abnormal chest auscultatory findings improved in seven of nine patients. Of the 17 patients with abnormal PFT before PD, 15 could be re-assessed at the 1-month follow-up; abnormal PFT normalized in 7/15 (46.7 %) patients. A statistically significant (P < 0.05) improvement occurred in the median FEV1, FVC, PEFR, and MEF25–75 % of the predicted after PD in the patients with baseline PFT abnormality (Table 4). The median percentage of predicted DLCO did not change significantly after PD.
Repeat chest X-ray normalized only in one of the four patients with baseline abnormality, others had persistence of symptoms as well as radiographic abnormality. The high-resolution CT scan of the thorax was not repeated on follow-up.
Discussion
The results of this study show that pulmonary manifestations are common among patients with achalasia and are prevalent in both type I and type II disease. Common respiratory symptoms among our patient cohort were sore throat, globus sensation, hoarseness, and throat clearing (reported by two-thirds of patients). Other common respiratory symptoms included cough, especially nocturnal, and dyspnea, both of which occurred in more than half of the patients. Previous retrospective studies [31, 32] reported only a 10–12 % prevalence of respiratory symptoms among patients with achalasia, but prospective studies [6, 8, 33] have reported about 50 % prevalence of chronic cough, nocturnal cough, dyspnea, or acute respiratory symptoms. Also, a few case reports [2, 4, 7, 34] have shown the occurrence of respiratory symptoms in achalasia for variable duration and improvement after treatment [8, 33], but none have evaluated whether the type of achalasia was a determining factor for respiratory involvement.
Repeated aspiration of the contents of the dilated esophagus is an important contributory factor in the pathogenesis of respiratory symptoms [2, 4, 15, 35]. Furthermore, dilated esophagus can cause a direct compression of recurrent laryngeal nerve and trachea leading to hoarseness and respiratory symptoms [10, 36, 37]. It was observed that onset of dysphagia (median duration 36 months) preceded respiratory symptoms (median duration 12 months) by about 24 months in both types of achalasia, suggesting that respiratory abnormalities occur later in the course of disease due to chronic aspiration, as described in GERD, [38–40] and other esophageal motility disorders [41]. Aspiration can also result in severe necrotizing infection [42], as occurred in one of our patient who developed lung abscess. We believe that timely diagnosis can prevent these permanent changes and avoid further morbidity.
Regurgitation and respiratory symptoms both tended to be commoner in type I than type II achalasia. Stasis is expected to be more prolonged in type I achalasia, probably due to atonic esophageal body leading to increased risk of aspiration. The difference was not statistically significant for either the stasis, as seen in TBE, or for the prevalence of symptoms, most likely due to small sample size.
We found that PD had a favorable impact on various respiratory symptoms, which is expected due to improved esophageal clearance reducing aspiration. This observation has not been reported in any previously published study. Respiratory symptoms persisted in a few patients after PD despite improvement in dysphagia and esophageal emptying. These patients might have developed chronic changes, which were either irreversible or would take longer to improve after PD.
In our study, functional changes in the lungs were evaluated by spirometry in all patients before PD, which determined the prevalence of PFT abnormalities in achalasia. Functional abnormalities tended to be more prevalent in type I than type II achalasia (59 and 33 %, respectively). Abnormal spirometry was seen in 45 % of the patients, of which restrictive and small airway disease (19 and 16 %, respectively) were the most common dysfunction. Only two previous studies have evaluated functional abnormalities in the lungs in achalasia patients using spirometry [6, 8]. The first of these showed the prevalence of functional abnormality in the lungs to be 20 %; but the authors of this study did not evaluate small airway disease. In our study, those patients suspected to have small airway disease were further evaluated by a high-resolution thorax CT scan, including expiratory film, and were confirmed to have small airway disease. Regarding obstructive airway abnormality, none of the two patients with this pattern in our study showed reversibility with bronchodilators (data not shown), in contrast to results of previous studies, implying that obstruction was not simply because of bronchial hyper-responsiveness.
In our study, PD resulted in normalization of PFT in about half of the patients, demonstrating that PD had a positive impact on pulmonary dysfunction in achalasia. However, this was not statistically significant in terms of number of patients showing improvement, although individual spirometry parameters, namely, FEV1, FVC, PEFR and MEF25–75, showed significant improvement. This is probably due to a reduction in ongoing aspiration. There was resolution of restrictive abnormality only in one patient, while four patients continued to have restrictive changes on spirometry. Since the radiation dose from the chest CT scan is large, high-resolution CT was done only in patients with clinical or spirometry-based pulmonary dysfunction and repeat scanning post-PD was avoided.
The strength of our study includes objective evaluation of pulmonary symptoms by spirometry along with DLCO, chest X-ray, and high-resolution chest CT scan as required. Also, we re-assessed pulmonary symptoms and spirometry following PD to study the effect of treatment. The limitations of our study include a small number of patients for subgroup analysis and post-treatment follow-up evaluation and short-term follow-up. A body plethysmography is another option to better delineate the respiratory dysfunction.
We excluded patients with mega-esophagus; dysphagia and esophageal emptying are less likely to respond to PD in such patients and, hence, the respiratory dysfunction. Exclusion of these patients might have resulted in an overestimation of the improvement in pulmonary dysfunction, but their inclusion would have underestimated the response. Moreover, these patients are better treated by surgery rather than PD.
The benefit of treatment in this study was reflected by improvement in the clinical and functional pulmonary parameters after PD. Thus, treatment with PD is valuable option for achalasia without any increase in mortality; in addition, complications are infrequent. Based on our data, we conclude that functional pulmonary dysfunction occurs in about half of the patients with achalasia and that timely treatment could lead to reversal. We therefore recommend respiratory evaluation of patients with achalasia in routine and timely management before permanent pulmonary changes occur.
References
Castell DO. Motor disorders of the esophagus. N Engl J Med. 1979;301:1124.
Mehdi NF, Weinberger MM, Abu-Hasan MN. Achalasia: unusual cause of chronic cough in children. Cough. 2008;4:6.
Al-Abdoulsalam T, Anselmo MA. An 11-year-old male patient with refractory asthma and heartburn. Can Respir J. 2011;18:81–83.
Akritidis N, Gousis C, Dimos G, Paparounas K. Fever, cough, and bilateral lung infiltrates. Achalasia associated with aspiration pneumonia. Chest. 2003;123:608–612.
Bello CT, Lewin JR, Norris CM, Farrar GE Jr. Achalasia (cardiospasm); report of a case with extreme and unusual manifestations. Ann Intern Med. 1950;32:1184–1190.
Makharia GK, Seith A, Sharma SK, et al. Structural and functional abnormalities in lungs in patients with achalasia. Neurogastroenterol Motil. 2009;21:603–608.
Muralidharan S, Jairaj PS, Periyanayagam WJ, John S. Achalasia cardia: a review of 100 cases. Aust N Z J Surg. 1978;48:167–170.
Parshad R, Devana SK, Panchanatheeswaran K, et al. Clinical, radiological and functional assessment of pulmonary status in patients with achalasia cardia before and after treatment. Eur J Cardiothorac Surg. 2012;42:e90–e95.
Chegar BE, Emko P. Bilateral vocal cord paralysis secondary to esophageal compression. Am J Otolaryngol. 2004;25:361–363.
Wickramasinghe LS, Chowdhury CR, Pillai SS, Ghosh S. Distended oesophagus as a cause of bilateral recurrent laryngeal nerve palsy. Postgrad Med J. 1988;64:958–959.
Miyamoto S, Konda Y, Matsui M, et al. Acute airway obstruction in a patient with achalasia. Intern Med. 2011;50:2333–2336.
Sinan H, Tatum RP, Soares RV, et al. Prevalence of respiratory symptoms in patients with achalasia. Dis Esophagus. 2011;24:224–228.
Farkkila MA, Ertama L, Katila H, et al. Globus pharyngis, commonly associated with esophageal motility disorders. Am J Gastroenterol. 1994;89:503–508.
Lee JS, Collard HR, Raghu G, et al. Does chronic microaspiration cause idiopathic pulmonary fibrosis? Am J Med. 2010;123:304–311.
Matsuse T, Oka T, Kida K, Fukuchi Y. Importance of diffuse aspiration bronchiolitis caused by chronic occult aspiration in the elderly. Chest. 1996;110:1289–1293.
Gimenez A, Franquet T, Erasmus JJ, Martinez S, Estrada P. Thoracic complications of esophageal disorders. Radiographics. 2002;22:S247–S258.
Ghoshal UC, Kumar S, Saraswat VA, et al. Long-term follow-up after pneumatic dilation for achalasia cardia: factors associated with treatment failure and recurrence. Am J Gastroenterol. 2004;99:2304–2310.
Vaezi MF, Baker ME, Richter JE. Assessment of esophageal emptying post-pneumatic dilation: use of the timed barium esophagram. Am J Gastroenterol. 1999;94:1802–1807.
de Oliveira JM, Birgisson S, Doinoff C, et al. Timed barium swallow: a simple technique for evaluating esophageal emptying in patients with achalasia. Am J Roentgenol (AJR). 1997;169:473–479.
Gupta M, Ghoshal UC, Verma A. Timed barium esophagogram and high resolution manometry for assessment of response to pneumatic dilation for achalasia cardia: a comparative study [abstract]. J Gasteroenterol Hepatol. 2012;27:58.
Eckardt AJ, Eckardt VF. Current clinical approach to achalasia. World J Gastroenterol. 2009;15:3969–3975.
Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24:57–65.
Lin Z, Kahrilas PJ, Roman S, et al. Refining the criterion for an abnormal integrated relaxation pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil. 2012;24:e356–e363.
Neyaz Z, Gupta M, Ghoshal UC. How to perform and interpret timed barium esophagogram. J Neurogastroenterol Motil. 2013;19:251–256.
Ghoshal UC, Rangan M, Misra A. Pneumatic dilation for achalasia cardia: reduction in lower esophageal sphincter pressure in assessing response and factors associated with recurrence during long-term follow up. Dig Endosc. 2011;24:7–15.
Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526–1533.
Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968.
Aggarwal AN, Gupta D, Behera D, Jindal SK. Comparison of fixed percentage method and lower confidence limits for defining limits of normality for interpretation of spirometry. Respir Care. 2006;51:737–743.
Macintyre N, Crapo RO, Viegi G, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26:720–735.
Vaezi MF, Baker ME, Achkar E, Richter JE. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut. 2002;50:765–770.
Plummer H, Vinson P. Cardiospasm: a report of 301 cases. Med Clin N Am. 1921;5:355–369.
Vinson P. Diagnosis and treatment of cardiospasm. JAMA. 1924;40:859–861.
Khandelwal S, Petersen R, Tatum R, et al. Improvement of respiratory symptoms following Heller myotomy for achalasia. J Gastrointest Surg. 2011;15:235–239.
Robinson GV, Kanji H, Davies RJ, Gleeson FV. Selective pulmonary fat aspiration complicating oesophageal achalasia. Thorax. 2004;59:180.
Smith Hammond C. Cough and aspiration of food and liquids due to oral pharyngeal dysphagia. Lung. 2008;186:S35–S40.
Chapman S, Weller PH, Campbell CA, Buick RG. Tracheal compression caused by achalasia. Pediatr Pulmonol. 1989;7:49–51.
Givan DC, Scott PH, Eigen H, Grosfeld JL, Clark JH. Achalasia and tracheal obstruction in a child. Eur J Respir Dis. 1985;66:70–73.
Savarino E, Bazzica M, Zentilin P, et al. Gastroesophageal reflux and pulmonary fibrosis in scleroderma: a study using pH-impedance monitoring. Am J Respir Crit Care Med. 2009;179:408–413.
Katz PO, Lehrer JK. GERD and interstitial lung disease. Cause, effect, or true true and unrelated? Dig Liver Dis. 2006;38:885–886.
Teramoto S, Ouchi Y. A possible pathologic link between chronic cough and sleep apnea syndrome through gastroesophageal reflux disease in older people. Chest. 2000;117:1215–1216.
Olsen AM. The spectrum of aspiration pneumonitis. Ann Otol Rhinol Laryngol. 1970;79:875–888.
Franquet T, Gimenez A, Roson N, et al. Aspiration diseases: findings, pitfalls, and differential diagnosis. Radiographics. 2000;20:673–685.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gupta, M., Ghoshal, U.C., Jindal, S. et al. Respiratory Dysfunction Is Common in Patients with Achalasia and Improves After Pneumatic Dilation. Dig Dis Sci 59, 744–752 (2014). https://doi.org/10.1007/s10620-013-2971-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2971-8