Abstract
Background and Aim
Mucosal immune activity may participate in irritable bowel syndrome (IBS) pathogenesis. Mast- and T cell numbers from patients with IBS or ulcerative colitis (UC) and healthy controls were determined.
Methods
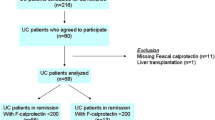
Between November 2007 and May 2012, patients with diarrhea-predominant IBS (D-IBS, n = 83), 49 patients with UC, and 25 healthy controls were recruited. Of the UC group, 28 were in remission and 21 had mildly active UC. Biopsies from each colon segment were subjected to immunohistochemical analysis. The mast cells, intraepithelial lymphocytes (IELs), and lamina proprial lymphocytes (LPLs) were counted.
Results
Compared to the healthy controls, the patients with D-IBS, UC in remission, and mildly active UC had significantly higher mean colorectal mucosal mast-cell, IEL, and LPL counts. Comparison with the colon segments (ascending, transverse, descending, and sigmoid segments) that had once been involved in UC (in the patients with remission) revealed that the D-IBS colons had similar immune-cell counts. However, they had significantly fewer immune cells than the colon segments that presently showed involvement in the patients with mildly-activated UC. The mast-cell and IEL counts were similar in the D-IBS rectums and once-involved UC rectums but significantly higher in the presently-involved UC rectums. However, both the once-involved and presently-involved UC rectums had significantly higher LPL counts than the D-IBS rectums.
Conclusions
Patients with D-IBS had significantly higher colonic mucosal immune-cell counts than healthy controls but had similar counts to patients with UC in remission. The symptoms in both conditions may originate from low-grade inflammation in the colonic mucosa.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Irritable bowel syndrome (IBS) is one of the most common gastrointestinal disorders. It is characterized by abdominal discomfort or pain that is associated with changes in bowel habits and disordered defecation features [1]. Two studies have shown that the intestinal mucosa of patients with IBS is infiltrated by immune cells (i.e., T cells and mast cells), which are activated, as indicated by their production of cytokine, histamine, and proteases [2, 3]. Several other studies have shown that such infiltration is particularly marked in the colonic epithelium and lamina propria, especially in post-infectious IBS (PI-IBS) [4–8]. Thus, the altered bowel physiology and sensory perception of patients with IBS may relate to immune mechanisms [9]. Supporting this notion is that mast-cell histamine and proteases derived from the colonic mucosa of patients with IBS excite rat sensory afferent pathways in vitro and evoke visceral hyperalgesia in mice when administered into the colon [10, 11]. In addition, the severity and frequency of abdominal pain in patients with IBS correlates positively with mast-cell infiltration in close proximity to mucosal nerve fibers [3]. Together, these observations support the hypothesis that immune activity plays a pathogenic role in IBS [12]. However, it should be noted that the findings of gut inflammation in patients with IBS are still being debated and that IBS is still considered to be a disorder of unknown etiology.
Patients frequently report IBS-like symptoms (such as abdominal pain, diarrhea/loose stool, bloating, mucus in stool, and urgency) before they are diagnosed with inflammatory bowel disease (IBD) and microscopic colitis [13, 14]. Moreover, patients with IBD that is in long-standing remission have a two- to threefold higher prevalence of IBS-like symptoms than the normal population [15]. These observations suggest that inflammation may be a common pathophysiological factor that leads to the abdominal symptoms in IBS and IBD. Indeed, it may be that the two diseases represent the opposite ends of a wide spectrum of chronic intestinal inflammatory conditions.
To date, however, the mucosal immune activation of all colonic segments in IBS has been poorly researched. To address this, the mast cell, intraepithelial lymphocyte (IEL), and lamina propria lymphocyte (LPL) counts in colon biopsies from healthy controls and patients with IBS or ulcerative colitis (UC) were determined in the present study. The relationship between the symptoms of the patients with IBS and their colorectal cell counts was also evaluated.
Patients and Methods
Patients
Between November 2007 and May 2012, 83 patients who visited Chung-Ang University Hospital with symptoms that met the Rome III criteria [1] for the diagnosis of diarrhea-predominant IBS (D-IBS) were recruited into the study. During the same period, 49 patients with UC who were undergoing colonoscopy at the same hospital to assess their UC disease activity were recruited. Of these, 28 were in remission and 21 had mild endoscopic activity. In addition, 25 healthy controls who visited the same hospital for a routine health checkup that involved a colonoscopy were recruited during the study period; none had any gastrointestinal complaints.
UC was diagnosed on the basis of clinical, radiological, endoscopic, and histological criteria [16–18]. UC activity was based on the endoscopic subscore in the Mayo score [19]. Patients with UC were judged to be in remission when endoscopy showed near-normal macroscopic findings without erythema, decreased vascularity, and friability. In all patients with UC, the colorectal segments were divided according to the present and past endoscopic findings of the colorectal mucosa into three colon-segment groups: segments whose mucosae were presently involved in the UC (in the patients with mildly active UC), had never been involved, or had once been involved but was now not involved (in the patients with remission).
None of the enrolled patients or healthy subjects had undergone major abdominal surgery or had any organic syndrome, asthma, lactose intolerance, food allergy, or other allergic disorders. None of the healthy subjects were taking nonsteroidal anti-inflammatory drugs, or any other anti-inflammatory drugs (including steroids, antihistamines, and mast cell stabilizers). The patients with UC were only given oral and/or topical 5-aminosalicylic acids to treat their mildly active disease or maintain remission.
All study participants provided written informed consent and the study was approved by the Institutional Review Board of the Chung-Ang University Hospital (I2007021(79)).
Colonoscopy and Biopsy Sampling
After bowel preparation with 4 L of polyethylene glycol, all participants underwent colonoscopy. All procedures were performed by the same expert endoscopist. During the colonoscopy of each patient, two mucosal biopsies were obtained from each of the following colon segments: the ascending colon, transverse colon, descending colon, sigmoid colon, and rectum. Given that the colonic mucosa of the healthy controls, patients with D-IBS, and patients with UC in remission were endoscopically normal-looking, the biopsies were taken randomly from each colon segment in these subjects. However, in the patients with mild UC, the biopsies were taken from inflamed areas of the colon unless inflamed areas could not be found; in that case, the biopsies were taken randomly from the endoscopically normal-looking mucosa. All biopsy samples were assessed by the pathologist for the presence of microscopic colitis, including lymphocytic colitis. However, none of the biopsy samples showed evidence of microscopic colitis.
Immunohistochemistry and Quantification of Immune Cells
Biopsy specimens were fixed in buffered 10 % formalin and processed for either H&E histology or immunohistochemistry. Thus, paraffin-embedded specimens were sliced with a microtome into 4-μm-thick sections, which were mounted onto precoated slides (Dako, Glostrup, Denmark). Following dewaxing, the tissue sections were incubated with 0.5 % hydrogen peroxide in methanol at 22 °C for 10 min and washed under running tap water for 15 min. The sections were then incubated with 0.1 % trypsin (Sigma, Pool, UK) and 0.1 % calcium chloride (pH 7.8) for 10 min at 37 °C. Nonspecific binding was blocked by incubation for 15 min in normal rabbit serum that was diluted 1:5 with Tris-buffered saline (TBS; pH 7.6). The slides were then incubated for 18 h at 4 °C with rabbit polyclonal antibodies specific for the T-cell marker CD3 (SP7, 1:150, Thermo Scientific, CA, USA) and with a mouse monoclonal antibody specific for human mast-cell tryptase (CloneAA1, 1:4,000, Thermo Scientific). The slides were immunostained with an automated immunostainer, Techmate 500 Plus, and Techmate reagents (Dako, Carpinteria, CA, USA). For each biopsy, the positively-stained mast cells in three consecutive non-overlapping microscopic fields (i.e., three sections) were counted. Each field was 0.024 mm2 in area. Counting was performed at 400× magnification (Fig. 1). Thus, for each segment (from which two biopsies were taken), the mast cells were counted in a total of six consecutive non-overlapping microscopic fields. Similarly, the IEL and LPL T-cell counts per 100 cells in the epithelium and lamina propria, respectively, were determined in three non-overlapping areas at 400× magnification in each of the two biopsy samples per segment. The counts of the three areas per biopsy were then added together to yield the total counts per 300 cells (Fig. 1). If the two biopsies per segment were too small to yield six consecutive non-overlapping fields, the cells in the maximal number of non-overlapping fields were counted. This occurred in two D-IBS cases (ascending colon), one D-IBS case (transverse colon), and one remission-UC case (ascending colon). However, when the analysis was performed without these slides, similar results were observed. All histological sections were evaluated and cells were counted by an expert pathologist who was unaware of the patient diagnosis and clinical details.
Representative photomicrographs showing tryptase-positive mast cells in the colonic mucosa of a healthy control subject (a), a patient with diarrhea-predominant irritable bowel syndrome (b), CD3+ T cells in the colonic mucosa of a healthy control subject (c), and a patient with mildly active ulcerative colitis (d). ×400 for all images. a, b The black arrows indicate tryptase-stained mast cells. The mast-cell counts were higher in diarrhea-predominant irritable bowel syndrome than in the healthy control group. c, d The black arrows indicate CD3-positive T cells in the lamina propria and the red arrows indicate CD3-positive T cells in the epithelium. The mildly active ulcerative colitis group had significantly higher T-cell counts in both the lamina propria and epithelium than the healthy control group
Symptom Questionnaire
The self-administered questionnaires included the Rome III criteria for IBS and the assessment of the severity of seven symptoms, namely, abdominal pain/discomfort, loose stools, urgency, sense of incomplete evacuation, mucus in stool, bloating, and flatulence. All symptoms were assessed by using a seven-point Likert scale (0–6) [20, 21].
Short Form 36 (SF-36) Questionnaire for Health-Related Quality of Life (HRQOL)
All participants completed the Korean version of the generic SF-36 questionnaire (version 2). This 36-item questionnaire scores eight domains of patient functioning: physical functioning, physical role, bodily pain, general health, vitality, social functioning, emotional role, and mental health [22]. Each subscale was scored from 0 to 100, with higher scores indicating a better health status.
IBS-Quality of Life (QOL) Questionnaire
The patients with D-IBS completed the IBS-QOL questionnaire [23], which has been translated into Korean and validated cross-culturally [24]. This questionnaire consists of 34 IBS-specific QOL items. Patients are asked to choose between descriptive statements using a recall period of the previous 30 days [23]. A five-point Likert response scale was used to assess the degree to which each statement described the feelings of the respondent (not at all, slightly, moderately, quite a bit, and extremely or a great deal). The questionnaire includes eight subscales: dysphoria, interference with activities, body image, health concerns, food avoidance, social reaction, sexual function, and relationships. Each subscale is transformed to a 0–100 scale, where 0 indicates a poor QOL and 100 indicates excellent QOL. All items are summed to calculate the overall score, which is transformed to a 0–100 scale.
Outcome Measures
The primary outcome measure was the number of colonic mucosal immune cells. We hypothesized that patients with D-IBS would have significantly higher colonic mucosal immune-cell counts (namely, mast cells, IELs, and LPLs) than the healthy controls. The secondary outcome measures were (1) comparison of the mucosal immune activity in D-IBS and UC, and (2) the correlation between immune activity and symptoms in D-IBS.
Statistical Analysis
Continuous variables are reported as median with range and/or as mean ± standard deviation (SD). Categorical variables are expressed as relative frequencies. Depending on the distribution, Student’s t test or the Mann–Whitney U test was used to compare the continuous variables and the χ2 or Fisher’s exact test was used (if the numbers were inadequate) to compare the categorical variables. Depending on the distribution, differences between the healthy controls, patients with D-IBS, and patients with UC were evaluated by analysis of variance (ANOVA) or the Kruskal–Wallis test. Correlations between immune activity and other factors, such as scores on the symptom questionnaire, SF-36, and IBS-QOL, were analyzed by Spearman’s rank test and linear regression. All p values were two-sided and p values of <0.05 were considered to indicate statistical significance. All statistical analyses were performed by using the SPSS program, version 18.0 (SPSS Inc, Chicago, IL, USA).
Results
Demographic and Clinical Characteristics of the Patients
As shown in Table 1, 52.0 % (13/25), 55.4 % (46/83), and 71.4 % (35/49) of the control, D-IBS, and UC groups were male, respectively, and their median ages were 40.0 (interquartile range [IQR] 32.0–49.5), 32.0 (IQR 25.5–45.0), and 42 (IQR 29–54) years, respectively. Of the patients with UC in remission and mildly active UC, 75.0 % (21/28) and 66.7 % (14/21) were male, respectively, and their median ages were 41.0 (IQR 25.5–55.3) and 43.0 (IQR 30.3–54.0) years, respectively. Of the 21 patients with mildly active UC, five had extensive colitis, 11 had left-sided colitis, and five had proctitis. Eight of the 83 patients with D-IBS had PI-IBS.
Total Colonic Mast Cell, IEL, and LPL Counts in the D-IBS, Healthy Control, and PI-IBS Groups
As shown in Fig. 2a, the total (all five colorectal segments together) mean (±SD) mast cell, IEL, and LPL counts of the D-IBS group were 33.3 (±15.1), 19.4 (±7.1), and 32.6 (±14.7), respectively. For the healthy controls, these values were 14.8 (±3.6), 10.2 (±3.5), and 19.9 (±4.9), respectively. When these mean control counts were used as cut-offs, 97.6 % (81/83), 92.8 % (77/83), and 81.9 % (68/83) of the patients with D-IBS had higher mast cell, IEL, and LPL counts, respectively. The differences between the D-IBS and healthy control groups in terms of their mean mast cell, IEL, and LPL counts were statistically significant (p < 0.001 for all three cell types). Regarding the eight patients with PI-IBS, their mean (±SD) mast cell, IEL, and LPL counts were 38.4 (±11.4), 22.2 (±6.6), and 35.8 (±14.9), respectively. While these counts were higher than the respective counts for the remaining patients with D-IBS, these differences did not achieve statistical significance (p = 0.105, 0.268, and 0.384, respectively).
Average mast cell, IEL, and LPL counts of the HC, D-IBS, UCR, and UCMA groups. Total cell counts (a). Average cell counts in various segments of the colon in the HC (b), D-IBS (c), UCR (d), and UCMA (e) groups. The D-IBS, UCR, and UCMA groups had significantly higher mean mucosal mast cell, IEL, and LPL counts in all colon segments than the healthy control group (all p values <0.001). Of the various colon segments, the healthy controls had significantly higher mean mast cell and IEL counts in the rectum than in other segments of the colon (p < 0.001). The colon segments of the D-IBS group did not differ in terms of mast cell, IEL, and LPL counts. The rectum of the UCR and UCMA groups had significantly higher LPL counts than the other segments of the colon (p < 0.001). HCs healthy controls, D-IBS diarrhea-predominant irritable bowel syndrome, UCR ulcerative colitis in remission, UCMA ulcerative colitis with mild activity, AC ascending colon, TC descending colon, DC descending colon, SC sigmoid colon, RE rectum, IEL intraepithelial lymphocyte, LPL lamina propria lymphocyte
Mucosal Mast- and T-Cell Counts in the Different Colorectal Segments of the Healthy Control, D-IBS, and UC Groups
In the healthy controls, the rectum had significantly higher mean mast cell and IEL counts than the other segments of the colon (p < 0.001) but none of the segments differed in terms of mean LPL counts (Fig. 2b). In the D-IBS group, none of the segments differed in terms of mast cell, IEL, and LPL counts (Fig. 2c). Analysis of the patients with UC in remission and mildly active UC revealed that in both subgroups, the rectum also had significantly higher LPL counts than the other segments (p < 0.001 for both subgroups; Fig. 2d, e).
Mucosal Mast-and T-Cell Counts in the Rectum Versus Other Colorectal Segments
Since none of the colon segments apart from the rectum differed in terms of mast cell, IEL, and LPL counts for any of the patient groups, the average immune-cell counts of the ascending, transverse, descending, and sigmoid colon segments together in each patient group were calculated. The D-IBS and healthy control groups were then compared in terms of their colonic (i.e., containing four segments) and rectal mast cell (Table 2), IEL (Table 3), and LPL (Table 4) counts. The D-IBS group had significantly higher mast cell, IEL, and LPL counts in the colon than the healthy controls (p < 0.001 for all three comparisons). However, while the D-IBS group also had significantly higher LPL counts in the rectum than the healthy controls (p = 0.004), the two groups did not differ in terms of mast cells (p = 0.087) or IELs (p = 0.394) in the rectum.
The patients with UC were also compared to the healthy controls and patients with D-IBS in terms of colonic and rectal immune-cell counts (Tables 2, 3, 4). However, in the patients with UC in remission or mildly active UC, not all of the colon segments had once been involved with the UC or were presently involved, respectively.
Compared to the healthy control colons, the uninvolved, once-involved, and presently-involved UC colons had significantly higher mast cell and IEL counts (p < 0.001 for all comparisons). The LPL counts were also higher in the uninvolved and presently-involved (both p < 0.001) colons but not the once-involved colons (p = 0.106).
Compared to the healthy control rectums, the presently-involved UC rectums had higher mast cell, IEL, and LPL counts (p < 0.001 for all comparisons) and the once-involved rectums had higher LPL (p = 0.003) but similar mast cell (p = 0.087) and IEL (p = 0.394) counts.
Comparison of the D-IBS colons to the colon UC subgroups revealed that the uninvolved UC colons had fewer mast cells (p = 0.010) and more IELs (p = 0.001) than the D-IBS colons but similar LPL counts (p = 0.669). The once-involved colons had significantly lower LPLs than the D-IBS colons (p = 0.023) but similar mast cell (p = 0.301) and IEL (p = 0.731) counts. The presently-involved colons had more mast cells (p = 0.002), IELs (p < 0.001), and LPLs (p < 0.001) than the D-IBS colons.
The once-involved UC rectums had similar mast cell (p = 0.981) and IEL (p = 0.554) counts but significantly more LPLs (p = 0.033) than the D-IBS rectums. The presently-involved UC rectums had more mast cells (p = 0.038), IELs (p < 0.001), and LPLs (p < 0.001) than the D-IBS rectums.
Comparisons between the UC colon subgroups revealed that the never-involved colons had similar mast cell (p = 0.471) and IEL (p = 0.050) numbers but more LPLs (p = 0.033) than the once-involved colons. The never-involved colons also had fewer mast cells (p < 0.001), IELs (p = 0.003), and LPLs (p = 0.002) than the presently-involved colons. The once-involved colons had fewer masts cells (p = 0.006), LPLs (p < 0.001), and LPLs (p < 0.001) than the presently-involved colons. Comparison of the UC rectum subgroups revealed that the once-involved rectums had similar mast cell (p = 0.141) but higher IEL (p < 0.001) and LPL (p = 0.001) counts than the presently-involved rectums.
Symptoms and HRQOL in the Groups
The D-IBS and total UC groups had significantly higher mean ± SD overall symptom questionnaire scores (20.0 ± 6.9 and 16.8 ± 8.8, respectively) than the healthy controls (6.7 ± 2.9; both p < 0.001). The D-IBS and UC groups did not differ in terms of overall symptom scores. Figure 3a shows the scores of the seven symptoms for each group. Apart from one exception, the two patient groups differed significantly from the healthy controls in all seven scores; the exception was that the UC and healthy control groups did not differ in loose stool scores. The two patient groups did not differ significantly in any of the symptoms except for abdominal pain/discomfort, which was higher in the D-IBS group (3.3 ± 1.2) than in the UC group (2.6 ± 1.4; p = 0.043).
Symptom scale scores in the D-IBS, UC, and HC groups (a) and Short Form-36 scale scores (b) in the D-IBS, UC, and HC groups. a *p < 0.05 HC versus D-IBS and UC, p < 0.05 UC versus D-IBS; † p < 0.05 HC versus D-IBS; ‡ p < 0.05 HC versus D-IBS and UC; § p < 0.05 HC versus D-IBS and UC; ∥ p < 0.05 HC versus D-IBS and UC; ¶ p < 0.05 HC versus D-IBS and UC; # p < 0.05 HC versus D-IBS and UC. b *p < 0.05 HC versus D-IBS and UC; † p < 0.05 HC versus D-IBS and UC; ‡ p < 0.05 HC versus D-IBS and UC; § p < 0.05 HC versus D-IBS and UC; ∥ p < 0.05 HC versus D-IBS and UC; ¶ p < 0.05 HC versus D-IBS and UC; # p < 0.05 HC versus D-IBS and UC. HCs healthy controls, D-IBS diarrhea-predominant irritable bowel syndrome, UC ulcerative colitis
Figure 3b shows the SF-36 results of the three groups. The D-IBS and UC groups had significantly lower scores than the healthy controls in all domains (all p < 0.05) except physical functioning. The two patient groups did not differ in terms of any of the SF-36 domains.
Correlation Between Mucosal Immune Infiltration in D-IBS and Symptoms and QOL (SF-36 and IBS-QOL)
The IBS symptoms and SF-36 scores of the patients with D-IBS did not correlate with their mean mast cell, IEL, and LPL counts of the entire colon. While their LPL counts in the entire colon correlated positively with interference with activity (r s = 0.470, p = 0.010) and food avoidance (r s = 0.333, p = 0.040) on the IBS-QOL, there were no other relationships between mucosal immune-cell counts and IBS-QOL domain scores, including the mean overall score (data not shown).
Discussion
Several studies have found associations between IBS and immune activity in the colon, as reflected by increased numbers and/or frequencies of mast cells and T cells in the colonic mucosa [2, 25–28]. Patients with UC also frequently exhibit IBS-like symptoms before being diagnosed with UC [13]. To date, however, the role immune cells play in IBS and UC pathogenesis is poorly understood. Moreover, studies comparing the colonic immune-cell infiltration in patients with IBS to that in healthy controls and patients with UC have not been performed. To address this lack, the present study was performed. We showed that patients with D-IBS, UC in remission, and mildly active UC had significantly more mucosal mast cells, IELs, and LPLs in their colorectal mucosa than healthy controls. Moreover, the patients with UC in remission had comparable colorectal immune-cell counts to the patients with D-IBS. However, the patients with mildly active UC had higher colorectal immune-cell infiltration than either the patients with UC in remission or D-IBS. Thus, although the endoscopic findings of the patients with D-IBS and UC in remission were negative, our immunohistochemical analyses showed that there was microscopic inflammation in the colorectal tissues of these patients. This suggests that immune activity, such as that generated by colorectal mucosal mast cells and T cells, may contribute to D-IBS-related symptoms. Supporting this notion indirectly is that it is already known that UC associates with chronic inflammation, even when the disease improves. Thus, the fact that D-IBS and UC in remission are similar in terms of colorectal immune-cell numbers supports the idea that chronic low-grade inflammation also participates in the pathophysiology of IBS.
Mucosal mast cells are widely distributed throughout the body and several studies have shown that higher mast cell numbers and activation are associated with inflammatory diseases in the colon [29–31]. While two studies have failed to detect immune-cell count changes in different intestinal segments of patients with IBS [2, 32], several other studies have shown that there is increased infiltration of mast cells in the terminal ileum [33], cecum [34], and proximal descending colon [3] of these patients. This increase in mast cells is believed to contribute to the symptoms and changes in bowel physiology seen in IBS [2, 3, 9]. Similarly, patients with UC have higher numbers of mast cells in the colonic mucosa than normal controls; moreover, this increase associates with greater bowel sensitivity and IBS-like symptoms [35, 36]. However, to our knowledge, the colorectal mast-cell counts of patients with IBS and UC and healthy controls have not been compared directly. We found that compared to healthy controls, the UC and D-IBS groups had higher numbers of colonic mast cells in all segments of the colon. A closer analysis of the colon segments of the UC group revealed that compared to the healthy control colons, the never-involved, once-involved, and presently-involved colonic segments of the patients with UC also had higher mast-cell numbers. Moreover, the mean mast-cell counts of the D-IBS colons were higher than those in the never-involved UC colonic segments, similar to those in the once-involved UC colonic segments, and lower than those in the presently-involved UC colonic segments. Thus, immune-system activation by mast cells associates with symptoms in D-IBS and IBS-like symptoms in UC, even when the mucosa appears normal and lacks gross inflammation, such as erythema, decreased vascularity, and friability.
Several studies have shown that in patients with IBS, innate immune-system cells secrete higher levels of proinflammatory cytokines, including interleukin (IL)-1β, tumor necrosis factor (TNF)-α, IL-8, and IL-6, than the controls [37, 38]. Such changes in the innate immune-system can alter the response of the adaptive immune-system, namely, T cells and B cells. Numerous studies have found that the colons of patients with IBS, including patients with PI-IBS, have higher mucosal T-cell counts than healthy controls [2, 3, 5, 6, 39, 40]. In particular, it was shown that patients with IBS have higher numbers of lamina propria CD3+ and CD8+ T cells [2] and intraepithelial lymphocytes than healthy controls [41]. Two studies also showed that patients with UC in remission have higher colonic mucosal T-cell counts than normal controls [42, 43]. However, the T-cell counts in the epithelium and lamina propria of the entire colon of patients with UC have not yet been reported. Moreover, only one study compared the colonic T-cell counts of patients with UC and patients with IBS [2]. We found that the patients with D-IBS, UC in remission, and mildly active UC generally had higher T-cell counts in the epithelium and lamina propria than the healthy controls in nearly all colon segments. Moreover, D-IBS colons (the ascending, transverse, descending, and sigmoid segments) had similar or higher LPL counts than the never-involved and the once-involved UC colons but significantly lower LPL counts than the mildly-activated UC colons. Moreover, in the rectal mucosa, the D-IBS group had a lower LPL count than both the once-involved and presently-involved UC subgroups. The presently-involved UC colons also had higher LPL counts than the once-involved UC colons. The rectal LPL-based inflammation seen in the patients with D-IBS and UC, even those with UC in remission, was usually severe. Thus, although the etiology of the inflammatory changes in D-IBS is unclear, it may involve T cells. IELs are intraepithelial inflammatory cells, while mast cells and lamina propria lymphocytes are subepithelial inflammatory cells linked by cytokine. In our study, we investigated the immune activation of both the intraepithelial and subepithelial layers of the colon.
IBS is a functional gastrointestinal disorder that is characterized by abdominal pain or discomfort and is associated with alterations in stool form or frequency. UC is a chronic inflammatory organic disorder of the gastrointestinal tract of unknown etiology that causes bowel-related symptoms, including abdominal pain and diarrhea. IBS and UC are chronic diseases that present with similar symptoms and significantly reduced QOL compared to healthy controls [44–47]. Both share a symptom complex involving abdominal pain and altered bowel habits. Indeed, IBS-like symptoms are frequently reported in UC [46–48]. The present study showed that the D-IBS and UC abdominal symptom and HRQOL scores were generally similar and differed significantly from the scores of healthy patients. However, patients with D-IBS did have higher abdominal pain/discomfort scores than the patients with UC (3.1 ± 1.5 vs. 1.9 ± 1.6, p = 0.005). These observations support previous findings by other investigators [44–46] that showed (1) patients with D-IBS have severe symptoms and a lower QOL than healthy controls and that (2) the symptoms of patients with UC, whether they have mildly active UC or UC in remission, are similar to those of patients with D-IBS, except that they have less abdominal pain/discomfort, which is a predominant symptom in IBS.
In the present study, the correlations between mucosal immune-cell activity and the symptoms and QOL (SF-36 and IBS-QOL) in D-IBS were also assessed. Contrary to our expectations, the average mast cell, IEL, and LPL immune-cell counts throughout the entire colon did not correlate with the IBS symptoms. This suggests that symptom severity may be independent of mast- and T-cell counts. Instead, symptom severity may be affected by other factors, such as proinflammatory mediators that are involved in the disease.
This study had several limitations. The sample size was relatively small and the evaluation was limited to two immune cells, namely, mast cells and T cells. There are many other immune cells, such as neutrophils and macrophages, which are involved in the innate immune-system and that could be associated with IBS. Further studies that analyze the association between D-IBS pathophysiology and other immune cells are warranted.
Notwithstanding these limitations, this prospective study involved an exhaustive assessment of the two cell types throughout the colon in not only D-IBS but also UC (both in remission and mildly active disease) and healthy controls. This is the first time such comparisons have been performed. The study showed that while patients with D-IBS had significantly higher mucosal mast cell, IEL, and LPL counts than healthy controls, they were comparable to patients with UC in remission. Thus, even though the endoscopic findings of D-IBS were negative, there was ample evidence of immune-cell activity in the colon. This was also true for UC in remission. This supports the notion that the symptoms in patients with IBS and UC in endoscopic remission associate with low-grade mucosal and submucosal inflammation.
References
Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491.
Cremon C, Gargano L, Morselli-Labate AM, et al. Mucosal immune activation in irritable bowel syndrome: gender-dependence and association with digestive symptoms. Am J Gastroenterol. 2009;104:392–400.
Barbara G, Stanghellini V, De Giorgio R, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126:693–702.
Wang LH, Fang XC, Pan GZ. Bacillary dysentery as a causative factor of irritable bowel syndrome and its pathogenesis. Gut. 2004;53:1096–1101.
Dunlop SP, Jenkins D, Spiller RC. Distinctive clinical, psychological, and histological features of postinfective irritable bowel syndrome. Am J Gastroenterol. 2003;98:1578–1583.
Spiller RC, Jenkins D, Thornley JP, et al. Increased rectal mucosal enteroendocrine cells, T lymphocytes, and increased gut permeability following acute Campylobacter enteritis and in post-dysenteric irritable bowel syndrome. Gut. 2000;47:804–811.
Lee KJ, Kim YB, Kim JH, Kwon HC, Kim DK, Cho SW. The alteration of enterochromaffin cell, mast cell, and lamina propria T lymphocyte numbers in irritable bowel syndrome and its relationship with psychological factors. J Gastroenterol Hepatol. 2008;23:1689–1694.
Wheatcroft J, Wakelin D, Smith A, Mahoney CR, Mawe G, Spiller R. Enterochromaffin cell hyperplasia and decreased serotonin transporter in a mouse model of postinfectious bowel dysfunction. Neurogastroenterol Motil. 2005;17:863–870.
Park JH, Rhee PL, Kim HS, et al. Mucosal mast cell counts correlate with visceral hypersensitivity in patients with diarrhea predominant irritable bowel syndrome. J Gastroenterol Hepatol. 2006;21:71–78.
Barbara G, Wang B, Stanghellini V, et al. Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome. Gastroenterology. 2007;132:26–37.
Cenac N, Andrews CN, Holzhausen M, et al. Role for protease activity in visceral pain in irritable bowel syndrome. J Clin Invest. 2007;117:636–647.
Barbara G, De Giorgio R, Stanghellini V, Cremon C, Corinaldesi R. A role for inflammation in irritable bowel syndrome? Gut. 2002;51:i41–i44.
Burgmann T, Clara I, Graff L, et al. The Manitoba Inflammatory Bowel Disease Cohort Study: prolonged symptoms before diagnosis—how much is irritable bowel syndrome? Clin Gastroenterol Hepatol. 2006;4:614–620.
Limsui D, Pardi DS, Camilleri M, et al. Symptomatic overlap between irritable bowel syndrome and microscopic colitis. Inflamm Bowel Dis. 2007;13:175–181.
Simren M, Axelsson J, Gillberg R, Abrahamsson H, Svedlund J, Bjornsson ES. Quality of life in inflammatory bowel disease in remission: the impact of IBS-like symptoms and associated psychological factors. Am J Gastroenterol. 2002;97:389–396.
Choi CH, Jung SA, Lee BI, Lee KM, Kim JS, Han DS. Diagnostic guideline of ulcerative colitis. Korean J Gastroenterol. 2009;53:145–160.
Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults (update): American College of Gastroenterology. Practice Parameters Committee. Am J Gastroenterol. 2004;99:1371–1385.
Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105:501-523; quiz 524.
Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987;317:1625–1629.
O’Mahony L, McCarthy J, Kelly P, et al. Lactobacillus and bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology. 2005;128:541–551.
Veldhuyzen van Zanten SJ, Talley NJ, Bytzer P, Klein KB, Whorwell PJ, Zinsmeister AR. Design of treatment trials for functional gastrointestinal disorders. Gut. 1999;45:II69-77.
Ware JE Jr. Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483.
Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43:400–411.
Park JM, Choi MG, Oh JH, et al. Cross-cultural validation of Irritable Bowel Syndrome Quality of Life in Korea. Dig Dis Sci. 2006;51:1478–1484.
Ohman L, Isaksson S, Lindmark AC, et al. T-cell activation in patients with irritable bowel syndrome. Am J Gastroenterol. 2009;104:1205–1212.
Vivinus-Nebot M, Dainese R, Anty R, et al. Combination of allergic factors can worsen diarrheic irritable bowel syndrome: role of barrier defects and mast cells. Am J Gastroenterol. 2012;107:75–81.
De Silva AP, Nandasiri SD, Hewavisenthi J, et al. Subclinical mucosal inflammation in diarrhea-predominant irritable bowel syndrome (IBS) in a tropical setting. Scand J Gastroenterol. 2012;47:619–624.
Bashashati M, Rezaei N, Bashashati H, et al. Cytokine gene polymorphisms are associated with irritable bowel syndrome: a systematic review and meta-analysis. Neurogastroenterol Motil. 2012;24:1102-e1566.
Yamagata K, Tanaka M, Kudo H. A quantitative immunohistochemical evaluation of inflammatory cells at the affected and unaffected sites of inflammatory bowel disease. J Gastroenterol Hepatol. 1998;13:801–808.
Quist RG, Ton-Nu HT, Lillienau J, Hofmann AF, Barrett KE. Activation of mast cells by bile acids. Gastroenterology. 1991;101:446–456.
Gui XY. Mast cells: a possible link between psychological stress, enteric infection, food allergy and gut hypersensitivity in the irritable bowel syndrome. J Gastroenterol Hepatol. 1998;13:980–989.
El-Salhy M, Gundersen D, Hatlebakk JG, Hausken T. Low-grade inflammation in the rectum of patients with sporadic irritable bowel syndrome. Mol Med Rep. 2013;7:1081–1085.
Weston AP, Biddle WL, Bhatia PS, Miner PB Jr. Terminal ileal mucosal mast cells in irritable bowel syndrome. Dig Dis Sci. 1993;38:1590–1595.
O’Sullivan M, Clayton N, Breslin NP, et al. Increased mast cells in the irritable bowel syndrome. Neurogastroenterol Motil. 2000;12:449–457.
Nishida Y, Murase K, Isomoto H, et al. Different distribution of mast cells and macrophages in colonic mucosa of patients with collagenous colitis and inflammatory bowel disease. Hepatogastroenterology. 2002;49:678–682.
van Hoboken EA, Thijssen AY, Verhaaren R, et al. Symptoms in patients with ulcerative colitis in remission are associated with visceral hypersensitivity and mast cell activity. Scand J Gastroenterol. 2011;46:981–987.
Liebregts T, Adam B, Bredack C, et al. Immune activation in patients with irritable bowel syndrome. Gastroenterology. 2007;132:913–920.
Dinan TG, Quigley EM, Ahmed SM, et al. Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? Gastroenterology. 2006;130:304–311.
Chadwick VS, Chen W, Shu D, et al. Activation of the mucosal immune system in irritable bowel syndrome. Gastroenterology. 2002;122:1778–1783.
Dunlop SP, Jenkins D, Neal KR, Spiller RC. Relative importance of enterochromaffin cell hyperplasia, anxiety, and depression in postinfectious IBS. Gastroenterology. 2003;125:1651–1659.
Arevalo F, Aragon V, Montes P, Guzman E, Monge E. Increase of intraepithelial lymphocytes in patients with irritable bowel syndrome. Rev Gastroenterol Peru. 2011;31:315–318.
Reichman-Warmusz E, Kurek J, Gabriel A, et al. Tissue hemostasis and chronic inflammation in colon biopsies of patients with inflammatory bowel disease. Pathol Res Pract. 2012;208:553–556.
Dai SX, Wu G, Zou Y, et al. Balance of CD8(+)CD28 (+)/CD8 (+)CD28 (−) T lymphocytes is vital for patients with ulcerative colitis. Dig Dis Sci. 2013;58:88–96.
Cho HS, Park JM, Lim CH, et al. Anxiety, depression and quality of life in patients with irritable bowel syndrome. Gut Liver. 2011;5:29–36.
Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119:654–660.
Whitehead WE, Burnett CK, Cook EW III, Taub E. Impact of irritable bowel syndrome on quality of life. Dig Dis Sci. 1996;41:2248–2253.
Drossman DA, Patrick DL, Mitchell CM, Zagami EA, Appelbaum MI. Health-related quality of life in inflammatory bowel disease. Functional status and patient worries and concerns. Dig Dis Sci. 1989;34:1379–1386.
Bercik P, Verdu EF, Collins SM. Is irritable bowel syndrome a low-grade inflammatory bowel disease? Gastroenterol Clin N Am. 2005;34:235–245, vi–vii.
Acknowledgments
The authors confirm that they have no financial arrangements with anyone in relation to this work.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ji Yong Ahn and Kyung Hun Lee contributed equally to this article.
Rights and permissions
About this article
Cite this article
Ahn, J.Y., Lee, K.H., Choi, C.H. et al. Colonic Mucosal Immune Activity in Irritable Bowel Syndrome: Comparison with Healthy Controls and Patients with Ulcerative Colitis. Dig Dis Sci 59, 1001–1011 (2014). https://doi.org/10.1007/s10620-013-2930-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2930-4