Abstract
Background
The immunosuppressive potential of anti-tumor necrosis factor (TNF) in exacerbating chronic hepatitis C virus (HCV) infection has been a major concern. We aim to critically analyze the impact of anti-TNF on the course of chronic HCV infection in patients with concurrent inflammatory bowel disease (IBD) and HCV infection.
Materials and Methods
Patients with diagnosis of IBD and HCV were identified retrospectively through the University of Pennsylvania Health System electronic database. Data assessed included demographics, duration of IBD and HCV infection, HCV RNA levels, HCV genotype, liver histology, hepatic biochemical tests (HBT) and IBD disease activity index.
Results
A total of 4,274 IBD and 3,523 HCV patients were identified from 10/1998 to 05/2010. Thirty-seven patients had concurrent HCV infection and IBD, of which 23 patients were eligible (61 % CD; 39 % UC). Five patients (22 %) received anti-TNF therapy (infliximab). Two patients received pegylated interferon and ribavirin (both were non-responders). Overall, three patients had clinical remission and one patient had clinical response to infliximab. When compared to baseline, one patient had HBT improvement, three patients remained stable and one patient had HBT elevation, which was likely due to progressive liver disease in view of HIV co-infection.
Conclusion
This represents the first critical analysis assessing the impact of anti-TNF therapy on the course of chronic HCV in IBD patients. Concurrent HCV infection in IBD patients is uncommon. Treatment of IBD with infliximab in HCV patients did not result in flares in hepatic biochemical tests while there was an improvement in the IBD disease activity score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anti-tumor necrosis factor (anti-TNF) therapy has been shown to be highly efficacious in the treatment of inflammatory bowel disease (IBD). Anti-TNF agents such as infliximab, adalimumab and certolizumab were approved by the US Food and Drug Administration (FDA) as induction and maintenance agents for patients with moderate to severe Crohn’s disease (CD), patients who are refractory to conventional therapies, or as alternative therapies in patients who lost responses or became intolerant to previous therapy with infliximab. Infliximab is the sole anti-TNF agent to date that was approved for use in patients with ulcerative colitis (UC) [1, 2]. It is well recognized that these therapies increase the susceptibility of patients to various non-opportunistic and opportunistic infections [3, 4]. Nevertheless, data are limited on the relationship between anti-TNF therapy and the risk of chronic viral infection or latent viral reactivation. Hepatitis C virus (HCV) is one of the common viral infections in United States. It affects almost 170–200 million people worldwide [5]. There have been concerns about the use of anti-TNFs agents in this patient population as the effect of immunosuppression may ultimately lead to HCV replications and worsening of liver disease. However, various studies demonstrated that patients with chronic HCV infections have increase TNF-α productions [6–8] which may play a role in liver injury; further a lack of response to antiviral therapy has been associated with elevated TNF-α levels [9, 10]. Thus, TNF inhibitions may result in beneficial outcome for HCV treatment. There are also case reports and case series, mainly in those with rheumatologic diseases, documenting the use of other anti-TNF agents (e.g. etanercept) in patients with concurrent HCV infections. The hepatic biochemical tests and post-treatment viral replications remained stable in these studies [11, 12]. However, there are a scarcity of data regarding the treatment with anti-TNF agents in patients with both IBD and chronic HCV infections. As the indications for anti-TNF agents evolve, safety consideration regarding their use in patients infected with HCV is becoming more important. Therefore the aim of this study was to critically analyze the impact of anti-TNF treatment on the course of chronic HCV infection in patients with IBD and HCV infections at a single center, and to perform a systematic review of the literature. We hypothesized that treatment with anti-TNF agents did not exacerbate the course of chronic HCV infection in patients with IBD and chronic HCV infections.
Materials and Methods
The electronic medical database (EPIC® Verona, Wisconsin) of the University of Pennsylvania Health System was retrospectively reviewed from October 1998 to May 2010, in a systematic order, to identify patients with concurrent diagnosis of IBD and HCV infections. The following ICD-9 codes used in our search were UC: 556.0–556.9; CD: 555.0–555.2 and 555.9; HCV infection: 070.41, 070.44, 070.51, 070.54, 070.70, and 070.71. The diagnoses of IBD and chronic HCV infection were verified and documented by members of the Gastroenterology Faculty of the University of Pennsylvania Health System.
Data were collected on patients’ demographics (sex, race, age), duration of HCV infection, possible mode of HCV transmission, HCV RNA viral loads, HCV genotype, hepatic biochemical test results (HBT), both pre and post anti-TNF therapy, liver histology, HCV treatment (pegylated inteferon and ribavirin), IBD subtype (CD or UC), IBD clinical activity index, both pre and post anti-TNF therapy (Harvey–Bradshaw Index (HBI) for CD [13] and partial Mayo Score for UC [14, 15], medical co-morbidity, HIV status and alcohol consumption.
The clinical activity of CD was measured using the HBI score. It was calculated by the sum of five components based on the data obtained from patient’s medical records [13]. Clinical response was defined as a reduction in HBI score of three points or more from baseline. Clinical remission was defined as an HBI score of four points or less based on established criteria determined from previous clinical trials [16].
The clinical activity of UC was measured using the partial Mayo score. It was calculated by the sum of three components based on the data obtained from patient’s medical records [14, 15]. Clinical response was defined as a reduction in partial Mayo score of three points or less from baseline. Clinical remission was defined as a partial Mayo score of three points or less based on previously determined criteria [15].
The diagnostic criteria for HCV were determined by a combination of positive HCV serology (anti-HCV with or without positive recombinant immunoblot assay) and detection of HCV RNA (either qualitatively or quantitatively) in patients’ sera [17]. The definitions for virological response during or after pegylated inteferon and ribavirin therapy were as follows: sustained virological response (SVR) was defined as negative HCV RNA 24 weeks after completion of therapy; non-responders were defined as failure to clear HCV RNA from serum after 24 weeks of therapy; relapsers were defined as reappearance of HCV RNA in serum after therapy is discontinued.
Patients were included in the study if they were adults (≥18 years old), carried the diagnosis of both HCV and IBD, and received anti-TNF treatment of infliximab, adalimumab or certolizumab. Patients were excluded if they were less than 18 years old, did not bear the diagnoses of IBD and chronic HCV, did not receive anti-TNF treatment or received anti-TNF treatment prior to the diagnosis of HCV, or had insufficient medical records. Permission was obtained from Institutional Review Board at the University of Pennsylvania to review and to analyze the medical records.
Statistical Analysis
Statistical analysis was performed using Prism software version 3.00 (Graph Pad, San Diego, CA, USA). The chi-square test was used to calculate the prevalence of chronic HCV infection among CD and UC. Statistical significance was set as p value <0.05.
Systematic Review of the Literature
We performed a systematic literature review on the treatment of IBD with anti-TNF agents in patients with chronic HCV infection. The examined database included MEDLINE, EMBASE and PUBMED. The key words used were hepatitis C, ulcerative colitis, Crohn’s disease, inflammatory bowel disease, anti-TNF, infliximab, adalimumab and certolizumab. We searched for any original articles between the period of 1950 to May 2010 that were in full-length and English. We also included case reports which described the effects of anti-TNF treatment on the course of IBD and liver functions in patients with concomitant diagnosis.
Results
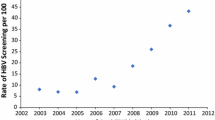
There were 4,274 patients with IBD (n = 2,194 for CD, n = 2,080 for UC) and 3,523 patients with HCV infection identified in our health system. Amongst them, there were 37 (0.87 %) patients who had concurrent IBD and HCV infections (n = 20 for CD, n = 17 for UC). The prevalence of chronic HCV infection among CD and UC was 0.91 and 0.81 % (p = 0.74), respectively.
We excluded 14 patients with IBD and chronic HCV infection from the analysis due to incomplete medical records or loss to follow-up. Of the 23 patients who met the inclusion criteria (14 CD and 9 UC), only 5 patients (22 %) received anti-TNF therapy. Four patients were treated with infliximab and one patient was treated with adalimumab (Table 1). Amongst this cohort, four patients had UC and one patient had CD. Four patients acquired HCV infections via blood transfusion and one patient acquired HCV infection via intravenous drug use. Patients’ demographics and disease characteristics are presented in Table 1. Only one out of five patients was on concurrent IBD specific medications [6-mercaptopurine (6MP)]. The additional medical comorbidities identified in these patients included chronic kidney disease, anxiety and HIV infection. None of the patients in our study cohort had active alcohol intake or illicit drug use. All the patients had active IBD prior to initiation of anti-TNF therapy. Three patients achieved clinical remissions, one patient had a clinical response and one patient had no clinical response to anti-TNF therapy.
The hepatic biochemical tests (HBT) were measured at 2 weeks to 3 months pre-anti-TNF therapy and 1–3 months post-anti-TNF therapy. These patients also had periodic HBT monitoring between 2 and 4 months while on anti-TNF therapy. When compared to baseline HBT, one patient had improvement, three patients remained stable and one patient had worsening HBT. The worsening HBT was likely due to progressive liver disease in view of HIV co-infection. The patient who was on concurrent 6MP had elevated HBT shortly after initiation of concurrent IBD medications. However, this returned to normal once the 6MP dose was reduced from 50 to 25 mg daily. HCV genotypes were identified in two of the five patients, and both were genotype 1. The HCV viral load pre- and post-anti-TNF therapy for every patient is listed in Table 1. Two of the five patients received pegylated interferon and ribavirin. The first patient (patient #2 in Table 1) received pegylated interferon and ribavirin 2 years prior to the initiation of anti-TNF treatment. The second patient (patient #4 in Table 1) had concurrent HIV disease and received pegylated interferon and ribavirin 3 years after termination of anti-TNF therapy. Both patients were non-responders with reappearance of HCV RNA at 2.4 million and 6.8 million copies, respectively. The pre- and post-anti-TNF treatment HBT values [aspartate aminotransferase (AST), alanine transaminase (ALT) and alkaline phosphatase (ALP)], viral load and IBD activity index are listed in Table 2.
Results of Systematic Review of the Literature
The literature search yielded a total of 1,313 articles, of which 14 were included in our full review. Five articles met the inclusion criteria. Three studies were case reports, describing a total of four patients with concurrent IBD (CD) and chronic HCV infections. They were all treated with anti-TNF agent (infliximab) [18–20]. One study assessed the use of immunomodulators and anti-TNF agents in eight patients with concurrent IBD and HBV or HCV infection. In this study, clinical remission was achieved with anti-TNF agent in one patient who had CD and HCV infection. There was no detrimental effects observed in patient’s underlying liver disease with stable ALT [21]. One study was a single center retrospective analysis consisted of 482 consecutive patients with concurrent IBD and chronic HBV or HCV infection. In this study, only one patient had concurrent IBD (UC) and chronic HCV, who was treated with infliximab. This patient had clinical remission for IBD but had HBT flare of greater than 1.5 of the upper normal limit [22]. Eight of the 14 articles, four review articles [23–26] and four original articles [27–30], were excluded as they did not evaluate the use of anti-TNF agents in patients presenting with both IBD and chronic HCV infection. We also excluded a case report which did not provide any details on the course of CD and HBT in a patient with concurrent diagnosis and was treated with infliximab [31]. The studies that met the inclusion criteria are presented in Table 3. Overall, we were unable to identify any original study which assessed the impact of anti-TNF therapy in patients with a dual diagnosis of IBD and chronic HCV infection.
Discussion
To our best knowledge, this is the first systematic study that assessed the effect of anti-TNF therapy on the course of chronic HCV infection and IBD. In our study, a majority of patients with IBD achieved clinical remissions without any significant changes in the hepatic biochemical profiles or viral loads before and after the anti-TNF treatment. Our data are consistent with the literature [18–22] (Table 3), including multiple rheumatological studies, demonstrating favorable short- and long-term safety profiles of infliximab and adalimumab in patients with IBD and chronic HCV infections [32–34]. All of our patients received long-term treatments with anti-TNF agents with a mean duration of 27 months. The majority of patients had favorable outcomes for IBD without any detrimental effects on their chronic liver diseases. One patient, who received adalimumab for 12 months, did not achieve clinical response for IBD. Her treatment was terminated due to side effects (bronchitis) and lack of response. Her hepatic biochemical profile remained unremarkable throughout the duration of the anti-TNF therapy.
The prevalence of chronic HCV infection in IBD patients of our health system was 0.86 %. This is consistent with the observations from a recent Spanish multicenter study where the prevalence of chronic HCV infection ranged from 0.79 to 1.59 % among 2,076 consecutive IBD patients evaluated in the hospital settings [29]. Albeit, the prevalence of chronic HCV infection has been documented to be as high as 5.98 % in France [35]. Biancone et al. [27] demonstrated in their study that chronic HCV infection was significantly more prevalent in CD than UC (332 patients with CD vs. 162 patients with UC) (7.4 vs. 0.6 %, p = 0.001). The difference was not appreciable in our study, where the prevalence of chronic HCV in our cohort was 0.91 and 0.81 % in patients with CD and UC (p = 0.74), respectively.
A recent multi-center study by Loras et al. [28] noted that patients with IBD and HBV infections had worse liver dysfunction tests compared with patients with IBD and HCV infection when they were treated with immunosuppressive medications. Of the 51 patients with positive HCV RNA, eight patients (15.7 %) developed liver dysfunction while on immunosuppressive medications. Seven patients had mild elevation of the liver function and one patient suffered from a fatal liver failure [28]. Interestingly, none of them were treated with anti-TNF agents. Seven patients received corticosteroids and one patient received azathioprine [28]. The case of fatal liver failure developed during treatment with corticosteroids [28]. Our study exclusively analyzed IBD patients treated with biologic agents and patients who failed immunomodulator (Azathioprine/6-mercaptopurine) therapies previously, either due to lack of response or adverse events. Our observation confirmed the potential safety and benefit of anti-TNF agents in this special patient population.
The role of TNF in chronic HCV infection is not well understood. Several studies have suggested that the HCV core protein has the potential to inhibit the TNF-mediated apoptotic signaling pathway, providing a selective advantage for HCV replications and avoidance of the host antiviral defense mechanism [36–38]. Thus, further suppression of TNF alpha by the biologic agents have been thought to pose a potential threat for florid viral replication and worsening of chronic HCV infection. This has placed a great limit on physicians from utilizing anti-TNF agents in patients with IBD and chronic HCV infections. On the contrary, there are studies postulating liver injury associated with an increased production of TNF-α observed in patients with chronic HCV infections [6–8, 39, 40]. Zein et al. [12] conducted a double-blinded randomized placebo controlled trial assessing the effect of etanercept as an adjunctive treatment in patients with chronic HCV. Etanercept is a recombinant DNA-derived protein composed of tumor necrosis factor receptor (TNFR) linked to the Fc portion of human IgG1. It is structurally different, though shares a similar mechanism of action, to the conventional anti-TNFs used in IBD (e.g. infliximab or adalimumab). Both of them act by inhibiting the interaction between TNF and cell surface receptors leading to reduction of cellular inflammation. In this trial, patients with chronic HCV infections were randomly assigned to receive standard HCV therapy (interferon alfa-2b and ribavirin) with or without etanercept 25 mg subcutaneously twice per week for 24 weeks. At the end of their study, they found a higher SVR in the etanercept group compared to the placebo group (63 vs. 32 %). They also observed lower frequency of adverse events in the etanercept group. This study supported the notion that etanercept inhibit TNF-mediated HCV replication, restore TNF-induced CD4+ cell impairment and enhance antiviral effects of interferon and ribavirin combination therapy [12]. However, studies on etanercept as a potential therapy for IBD have not been promising [41]. Although we did not demonstrate a positive effect on the HCV clearance, our study suggested that the use of anti-TNF agents did not have any deleterious effect on the hepatic biochemical profile, including one of the five patients who received concomitant interferon therapy. HIV and HCV co-infection depicts a worse outcome for patient with IBD [28], and this was demonstrated in our study.
Our study has several limitations. The retrospective nature of the study design did not allow us to be more precise in our timing or comprehensive collections of the viral loads and liver biopsies with the administration of anti-TNFs. Our patient population was older, with a mean age of 65 years, compared with other studies of <50 years [27, 29, 35], raising the question of generalization. We relied on the values reflected from viral loads and hepatic biochemical profiles as indices of clinical activity of patients’ chronic HCV infections; however, these values may not directly correspond to the severity of liver injury on histology. Given the low prevalence of patients who have concurrent IBD and chronic HCV infections, and being a single-center study, our study cohort consisted of a small number of patients. Thus, our statistical analysis on the difference in HCV RNA pre- and post-anti-TNF therapy, as well as the clinical response of IBD was limited.
In our systematic review of the literature, data were scarce on the use of anti-TNF agents in patients with concomitant IBD and chronic HCV infections. The results of our systematic literature review indicated that therapy with anti-TNF agents improves the clinical course of IBD without worsening chronic HCV infection. They also demonstrated safety in the use of interferon-based therapy in patients with IBD. Large scale, multi-center studies are needed to fully evaluate the effects of anti-TNF treatments on the course of chronic HCV infection in patients with a background of IBD. The course of IBD while on interferon-based therapy also needs to be assessed in larger studies.
In summary, concurrent chronic HCV infections in IBD patients are uncommon. Treatment of IBD with infliximab and adalimumab in patients with chronic HCV infections did not result in hepatic biochemical test flares while there were improvements in IBD activity scores with the infliximab therapy. However, our results should be interpreted with caution due to the small number of patients studied. Future prospective studies on a large number of patients are warranted to further evaluate the impact of anti-TNF treatment on the hepatic biochemical tests in patients with IBD and concomitant chronic HCV infection.
References
Peyrin-Biroulet L, Deltenre P, de Suray N, et al. Efficacy and safety of tumor necrosis factor antagonists in Crohn’s disease: meta-analysis of placebo-controlled trials. Clin Gastroenterol Hepatol. 2008;6:644–653.
Rutgeerts P, Sandborn WJ, Feagan BG, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462–2476.
Velayos FS, Sandborn WJ. Pneumocystis carinii pneumonia during maintenance anti-tumor necrosis factor-alpha therapy with infliximab for Crohn’s disease. Inflamm Bowel Dis. 2004;10:657–660.
Toruner M, Loftus EV Jr, Harmsen WS, et al. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology. 2008;134:929–936.
Strader DB, Wright T, Thomas DL, et al. Diagnosis, management, and treatment of hepatitis C. Hepatology. 2004;39:1147–1171.
Kallinowski B, Haseroth K, Marinos G, et al. Induction of tumour necrosis factor (TNF) receptor type p55 and p75 in patients with chronic hepatitis C virus (HCV) infection. Clin Exp Immunol. 1998;111:269–277.
Kishihara Y, Hayashi J, Yoshimura E, et al. IL-1 beta and TNF-alpha produced by peripheral blood mononuclear cells before and during interferon therapy in patients with chronic hepatitis C. Dig Dis Sci. 1996;41:315–321.
Nelson DR, Lim HL, Marousis CG, et al. Activation of tumor necrosis factor-alpha system in chronic hepatitis C virus infection. Dig Dis Sci. 1997;42:2487–2494.
Fukuda R, Ishimura N, Ishihara S, et al. Intrahepatic expression of pro-inflammatory cytokine mRNAs and interferon efficacy in chronic hepatitis C. Liver. 1996;16:390–399.
Larrea E, Garcia N, Qian C, et al. Tumor necrosis factor alpha gene expression and the response to interferon in chronic hepatitis C. Hepatology. 1996;23:210–217.
Calabrese LH, Zein N, Vassilopoulos D. Safety of antitumour necrosis factor (anti-TNF) therapy in patients with chronic viral infections: hepatitis C, hepatitis B, and HIV infection. Ann Rheum Dis. 2004;63:ii18–ii24.
Zein NN. Etanercept as an adjuvant to interferon and ribavirin in treatment-naive patients with chronic hepatitis C virus infection: a phase 2 randomized, double-blind, placebo-controlled study. J Hepatol. 2005;42:315–322.
Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1:514.
Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987;317:1625–1629.
Lewis JD, Chuai S, Nessel L, et al. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008;14:1660–1666.
Vermeire S, Schreiber S, Sandborn WJ, et al. Correlation between the Crohn’s disease activity and Harvey–Bradshaw indices in assessing Crohn’s disease severity. Clin Gastroenterol Hepatol. 2010;8:357–363.
Ghany MG, Strader DB, Thomas DL, et al. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335–1374.
Abdelmalek MF, Liu C, Valentine JF. Successful treatment of chronic hepatitis C with pegylated interferon, ribavirin, and infliximab in a patient with Crohn’s disease. Am J Gastroenterol. 2007;102:1333–1334.
Campbell S, Ghosh S. Infliximab therapy for Crohn’s disease in the presence of chronic hepatitis C infection. Eur J Gastroenterol Hepatol. 2001;13:191–192.
Holtmann MH, Galle PR, Neurath MF. Treatment of patients with Crohn’s disease and concomitant chronic hepatitis C with a chimeric monoclonal antibody to TNF. Am J Gastroenterol. 2003;98:504–505.
Biancone L, Del Vecchio Blanco G, Pallone F, et al. Immunomodulatory drugs in Crohn’s disease patients with hepatitis B or C virus infection. Gastroenterology. 2002;122:593–594.
Katsanos KH, Tsianos VE, Zois CD, et al. Inflammatory bowel disease and hepatitis B and C in Western Balkans: a referral centre study and review of the literature. J Crohns Colitis. 2010;4:450–465.
Chevaux JB, Bigard MA, Bensenane M, et al. Inflammatory bowel disease and hepatitis B and C. Gastroenterol Clin Biol. 2009;33:1082–1093.
Shale MJ. The implications of anti-tumour necrosis factor therapy for viral infection in patients with inflammatory bowel disease. Br Med Bull. 2009;92:61–77.
Shale MJ, Seow CH, Coffin CS, et al. Review article: chronic viral infection in the anti-tumour necrosis factor therapy era in inflammatory bowel disease. Aliment Pharmacol Ther. 2010;31:20–34.
Horn TL, Reynolds J, de Villiers W, et al. Hepatitis C virus and inflammatory bowel disease. Dig Dis Sci. 2009;54:1171–1177.
Biancone L, Pavia M, Del Vecchio Blanco G, et al. Hepatitis B and C virus infection in Crohn’s disease. Inflamm Bowel Dis. 2001;7:287–294.
Loras C, Gisbert JP, Minguez M, et al. Liver dysfunction related to hepatitis B and C in patients with inflammatory bowel disease treated with immunosuppressive therapy. Gut. 2010;59:1340–1346.
Loras C, Saro C, Gonzalez-Huix F, et al. Prevalence and factors related to hepatitis B and C in inflammatory bowel disease patients in Spain: a nationwide, multicenter study. Am J Gastroenterol. 2009;104:57–63.
Chevaux JB, Nani A, Oussalah A, et al. Prevalence of hepatitis B and C and risk factors for nonvaccination in inflammatory bowel disease patients in Northeast France. Inflamm Bowel Dis. 2010;16:916–924.
Alderson JW, Van Dinter TG Jr, Opatowsky MJ, et al. Disseminated aspergillosis following infliximab therapy in an immunosuppressed patient with Crohn’s disease and chronic hepatitis C: a case study and review of the literature. MedGenMed. 2005;7:7.
Ferri C, Ferraccioli G, Ferrari D, et al. Safety of anti-tumor necrosis factor-alpha therapy in patients with rheumatoid arthritis and chronic hepatitis C virus infection. J Rheumatol. 2008;35:1944–1949.
Marotte H, Fontanges E, Bailly F, et al. Etanercept treatment for three months is safe in patients with rheumatological manifestations associated with hepatitis C virus. Rheumatology (Oxford). 2007;46:97–99.
Peterson JR, Hsu FC, Simkin PA, et al. Effect of tumour necrosis factor alpha antagonists on serum transaminases and viraemia in patients with rheumatoid arthritis and chronic hepatitis C infection. Ann Rheum Dis. 2003;62:1078–1082.
Longo F, Hebuterne X, Tran A, et al. Prevalence of hepatitis C in patients with chronic inflammatory bowel disease in the region of Nice and evaluation of risk factors. Gastroenterol Clin Biol. 2000;24:77–81.
Ray RB, Meyer K, Ray R. Suppression of apoptotic cell death by hepatitis C virus core protein. Virology. 1996;226:176–182.
Ray RB, Meyer K, Steele R, et al. Inhibition of tumor necrosis factor (TNF-alpha)-mediated apoptosis by hepatitis C virus core protein. J Biol Chem. 1998;273:2256–2259.
Tilg H, Kaser A, Moschen AR. How to modulate inflammatory cytokines in liver diseases. Liver Int. 2006;26:1029–1039.
Tilg H, Wilmer A, Vogel W, et al. Serum levels of cytokines in chronic liver diseases. Gastroenterology. 1992;103:264–274.
Gonzalez-Amaro R, Garcia-Monzon C, Garcia-Buey L, et al. Induction of tumor necrosis factor alpha production by human hepatocytes in chronic viral hepatitis. J Exp Med. 1994;179:841–848.
Sandborn WJ, Hanauer SB, Katz S, et al. Etanercept for active Crohn’s disease: a randomized, double-blind, placebo-controlled trial. Gastroenterology. 2001;121:1088–1094.
Conflict of interest
Dr. Gary R. Lichtenstein has served as a consultant and performed research with Alaven, Jansen Orthobiotech, Proctor and Gamble, Warner Chilcotte, UCB, Prometheus Laboratories, Inc, Salix Pharmaceuticals, Shire Pharmaceuticals, Santarus, Ferring. He has served as a consultant to Abbott Corporation, Elan, Meda, Millenium, Ono Pharmaceuticals. Pfizer, Schering Plough, Wyeth. He has done research with Bristol-Myers Squibb.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, M.V., Blonski, W., Buchner, A.M. et al. The Influence of Anti-TNF Therapy on the Course of Chronic Hepatitis C Virus Infection in Patients with Inflammatory Bowel Disease. Dig Dis Sci 58, 1149–1156 (2013). https://doi.org/10.1007/s10620-012-2457-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2457-0