Abstract
Background
Non-adherence to medical therapy after liver transplantation is confounded by different methods of measurement.
Aims
(1) To compare the performance of three different methods of measuring non-adherence: (a) biochemical (standard deviation [SD] tacrolimus levels), (b) clinician report, (c) self-report. (2) To identify pre-transplant predictors of post-transplant non-adherence. (3) To evaluate whether SD tacrolimus is an accurate predictor of graft outcomes.
Methods
In this retrospective cohort study, charts of adult recipients of a liver transplant 2003–2009 (sample A, n = 444) were reviewed to determine pre-transplant predictors of non-adherence and clinician report of non-adherence. SD tacrolimus levels were measured between 6 and 18 months post-transplant. A subset of sample A (n = 122) completed a survey on non-adherence. The three methods were compared using linear and logistic regression. Multivariable analysis was used to investigate pre-transplant predictors of non-adherence. In sample B (transplant recipients 1995–2003, n = 544) Cox regression was used to determine the relationship between SD immunosuppressant level and graft failure.
Results
Non-adherence was found in 22–62 % of subjects, with the highest rates indicated by self-report. Clinician report of non-adherence was associated with both self-report and SD tacrolimus. On multivariable analysis, unemployment at time of listing and chart evidence of pre-transplant non-adherence were significant predictors of higher SD of tacrolimus. History of substance abuse and pre-transplant chart evidence of non-adherence were also significant independent predictors of post-transplant chart evidence of non-adherence. Drug variability in the immediate post-transplant setting was independently associated with graft failure over time (hazard ratio 1.005 per unit increase in standard deviation, p = 0.04).
Conclusions
Non-adherence among liver transplant recipients is a common problem associated with increased risk of graft failure. SD tacrolimus can be used to measure non-adherent behavior and perhaps target patients for behavioral interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The continued shortage of donor livers requires that transplant professionals allocate organs in an ethical manner. This challenging task is aided by tools such as the model for end-stage liver disease (MELD) score, which accurately and objectively assesses pre-transplant severity of illness [1]. However, determining candidacy for transplantation also requires assessment of psychosocial factors such as level of social support, history of substance abuse, financial status, and non-adherence to medical recommendations, in determining transplant candidacy [2, 3]. Our ability to objectively measure these factors and their predictive value in determining post-transplant outcomes in the adult liver transplant population remain incompletely understood (Fig. 1).
Non-adherence in adult liver transplantation: a problem that cuts across all domains of patient care. Understanding the implications of non-adherent behavior on future outcomes could redefine the selection process for transplant listing. Which factors in the pre-transplant setting predict non-adherent behavior? Are non-adherent behaviors associated with poor outcomes including graft failure? These questions are the focus of this study
Among the psychosocial factors affecting post-transplant outcomes, non-adherence to immunosuppressant (IS) therapy is considered to be the leading cause of preventable graft failure [4], contributing to 20 % of late acute rejection episodes and 16 % of graft losses within the overall transplant population [5]. A meta-analysis of 147 studies of kidney, heart, liver, and other transplant recipients found non-adherence to IS therapy to be prevalent, with an overall rate of 19–25 cases per 100 patients per year [6].
In liver transplantation, the effect of non-adherence on graft outcomes has been well studied in pediatric and adolescent transplant recipients [7–11]. Among adults, various international studies have attempted to measure non-adherence to IS therapy using self-reported non-adherence [12] and electronic medication monitoring [13], with the majority of patients found to be adherent to IS therapy. This is in contrast to a US study that found half of liver transplant recipients reporting non-adherence to IS therapy [14]. Adult liver transplant recipients in the US remain an understudied population for whom we have minimal data regarding the causes and effects of non-adherence.
In the clinical setting, the ability to detect and intervene upon non-adherence is limited due to the paucity of accurate objective methods for measuring non-adherence in transplant recipients. There is no gold standard method for measuring non-adherence [15]. Methods used to assess the extent to which patients take medications and attend clinic visits include both direct (observed therapy, measurement of drug/metabolite levels) and indirect measures (patient surveys, clinical response, rate of prescription refill, electronic medication monitoring, and medical chart notes) [16]. Each method has its limitations, and many techniques remain to be validated.
Accurately measuring non-adherence and understanding its effects on graft outcomes would be critical to improving the transplantation selection process. This topic has been understudied in the American adult liver transplant population. While various methods of measuring non-adherence have been used in the literature, no single study has attempted to compare the validity of these methods within one population of adult liver transplant recipients. We aimed to assess the post-transplant level of non-adherence in liver transplant recipients by using three methods of quantifying non-adherence: biochemical, clinician-report, and self-report [11]. We compared these methods of quantifying non-adherence and investigated various patient-specific characteristics in the pre-transplant setting that may predict post-transplant non-adherence [20]. Lastly, we investigated the relationship between post-transplant non-adherence and graft survival, using our most objective measure of non-adherence in this study—immunosuppressant variability—which we hypothesize is a good predictor of the negative outcomes of non-adherence.
Definition of Terms
In the transplant literature, the term non-adherence is used to describe general behaviors that deviate from a prescribed post-transplant health regimen, with emphasis on a collaboration between the patient and healthcare professional [18]. In the literature, the definition of non-adherence has been widely interpreted, leading to confusion as to how to measure non-adherence. In 2009, the Non-Adherence Consensus Conference convened to define non-adherence as follows: “Deviation from the prescribed medication regimen sufficient to influence adversely the regimen’s intended effect” [15]. This definition focuses on non-adherence to IS therapy with emphasis on the negative outcomes of non-adherence. In the clinical setting, non-adherence encompasses numerous behaviors that jeopardize health outcomes including: (1) improper medication adherence (e.g., not having a prescription filled, forgetting or intentionally not taking a medication), (2) failure to adhere to the recommended laboratory testing schedule, and (3) failure to attend clinic visits or cooperate with other testing or treatment. In accordance with the Non-Adherence Consensus Committee’s recommendations, we focus on non-adherence to immunosuppressant (IS) therapy given its association with worse outcomes for transplant recipients. We also include other non-adherent behaviors that may negatively affect health outcomes including: missed clinic appointments, missed blood draws, and substance use [22].
Methods
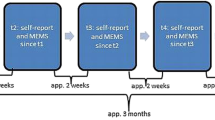
We conducted a retrospective cohort study of adult liver transplant recipients at the University of Michigan Health System (UMHS). Our two sub-populations consisted of a group of 444 patients who underwent liver transplantation from 2003 to 2009 (sample A), as well as a second group of 544 liver transplant recipients from 1995 to 2003 (sample B). Sample A was used to determine correlations between the three different measures of non-adherence described below, as well as to investigate associations between pre-transplant factors and post-transplant non-adherence. This population included a subgroup of transplant recipients who participated in a survey evaluating self-reported non-adherent behaviors. Sample B was used to determine the impact of post-transplant non-adherence on graft survival. Inclusion criteria are illustrated in Fig. 2. Both samples included transplant recipients who underwent standardized pre-transplantation psychosocial evaluation and survived at least 18 months post-transplantation. Recipients of multi-organ transplants were excluded, as well as patients with less than three tacrolimus levels. The study was approved by the University of Michigan Institutional Review Board (IRB) with written informed consent obtained by survey participants.
Subject inclusion diagram. Sample A was designed to evaluate post-transplant non-adherence in the 6 to 18-month period, once tacrolimus levels had stabilized and did not reflect early graft failure or post-operative drug variability. This cohort was used to investigate three different parameters of measuring non-adherence including: (1) standard deviation (SD) tacrolimus level, (2) clinician reports of non-adherence in the medical chart, and (3) self-reported non-adherence via survey. Sample A was also designed to investigate pre-transplant predictors of post-transplant non-adherence quantified in the three ways listed above. Sample B included a larger cohort designed to investigate the relationship between post-transplant non-adherence (quantified by SD tacrolimus levels) and graft failure. Both samples included transplant recipients who underwent standardized pre-transplantation psychosocial evaluation, survived at least 18 months post-transplantation, and had at least three tacrolimus levels available for analysis
Sample A
Methods of Measuring Non-Adherence
Post-transplant non-adherence was quantified in three ways: (1) Biochemical: the standard deviation (SD) of tacrolimus blood levels measured during the period from 6 to 18 months post-transplant. Tacrolimus levels from the first 6 months were excluded given that during this interim, medication doses are altered due to side-effects, there is the potential for early graft failure, and levels are subject to post-operative variability. The 6 to 18-month period reflects a crucial time during which non-adherent behaviors can be measured more objectively once drug levels have stabilized and the potential for early graft failure has been eliminated. The analysis was limited to tacrolimus because fewer than 20 % of patients were on cyclosporine, and the different baseline levels of these medications would otherwise confound analysis of standard deviation. (2) Clinician-Report: medical chart documentation of non-adherence determined by >1 documented missed follow-up visit in a year, missed blood-draws, or staff notes indicating failure of the patient to follow medical recommendations. This measure was treated in a dichotomous fashion: the presence or absence of evidence of non-adherence. (3) Self-Reported: survey responses indicating non-adherence as measured by the validated Medication Adherence Report Scale (MARS) [23, 24]. Subjects who were still alive and followed in our center at the time of the study received a mailed survey inquiring about their level of social support [25], ability to take immunosuppressant medications, likelihood of missing doctor’s visits, and barriers to adherence. Survey responses were tabulated and coded by a research assistant, with the investigators remaining blinded to the results until statistical analysis was complete. An adaptation of the MARS [23] and Multidimensional Adherence Questionnaire (MAQ) [28] was used to assess self-reported non-adherence. This survey can be seen in the Appendix. For the purposes of statistical analysis, responses of “sometimes” or greater, on the four-point scale were categorized as non-adherence.
In order to assess the validity of these three measures of non-adherence, we analyzed the correlation between the biochemical method, the other two methods using linear regression, and between the clinician-report and self-report using logistic regression. Strength of association is reported using R 2 for linear regression and likelihood ratio Chi-square value for logistic regression.
Pre-Transplant Predictors of Post-Transplant Non-Adherence
The electronic medical charts of Sample A were reviewed to identify pre-transplant predictors of post-transplant non-adherence. This data abstraction was performed by the investigators blinded to the results of outcomes described above. Potential risk factors that were considered included age, gender, race, marital status, employment status, health insurance (as a measure of socio-economic status), history of substance abuse, etiology of disease, and level of social support as assessed during evaluation for transplant listing. Each transplant recipient had undergone a psychosocial evaluation conducted by one of two transplant social workers. These evaluations were conducted using standardized forms, which were documented in electronic medical charts that comprised the chart review. The psychosocial evaluation consisted of a thorough investigation of substance abuse history, mental health history, social support, financial status, and health insurance coverage.
Pre-transplant predictors of non-adherence were correlated with two types of post-transplant dependent variables: (1) continuous (SD of tacrolimus levels) and (2) dichotomous (reporting non-adherence at least “sometimes” in response to any one of the five questions on the mailed survey, or presence of chart evidence of non-adherence). Statistical analyses were performed using linear regression for continuous data and logistic regression for categorical data. In order to avoid model selection bias, all variables were entered into the multivariable models. Residual-versus-fitted plots were assessed to confirm the appropriateness of parametric methods. Calculations were performed using Stata v11 (Statacorp, College Station, TX, USA).
Sample B
Non-Adherence as Measured by Immunosuppressant Variability and Graft Outcomes
Sample B was chosen to allow at least 5 years follow-up time, and was used to determine the relationship between post-transplant non-adherence (as measured by SD immunosuppressant medication during months 6–18 post-transplant) and graft failure, defined as death or the need for re-transplantation. Unlike sample A, this larger cohort was used to evaluate the potential relationship between long-term non-adherence and graft failure. These patients did not undergo a survey investigating self-reported non-adherence. In this sample, the statistical method used permitted analysis of subjects on cyclosporine in addition to tacrolimus. Cox regression (stratified by immunosuppressant type) was used to determine the relationship between SD immunosuppressant level and graft failure, adjusting for potential confounders including age at transplant, gender, race, date of transplant, and pre-transplant MELD score.
Results
Sample A
Among the 444 liver transplant recipients from 2003 to 2009 who met inclusion criteria, 318 had at least three tacrolimus levels available during the period between 6 and 18 months post-transplant. Seventy-six out of 398 (19 %) were on cyclosporine and 299 were still alive and followed in our center at the time of the study, of which 165 (55 %) responded to the survey (Fig. 2) (see Table 1 for demographics and characteristics of the study population).
Biochemical Measure of Non-Adherence
Among the patients with immunosuppressant levels available between 6 and 18 months post-transplant, 322/398 (81 %) were on tacrolimus. Of the 322 patients on tacrolimus, 318 had at least three levels available and thus met inclusion criteria for analysis. The median standard deviation of tacrolimus levels in this sample was 2.1 (range 0.3–11.2). As shown in Table 2, on multivariable analysis, unemployment at the time of listing and chart evidence of pre-transplant non-adherence were significant predictors of higher standard deviation of tacrolimus (increased drug variability) (p = 0.02 and 0.01, respectively). In other words, being employed at listing was associated with a 0.59 lower standard deviation of tacrolimus levels, and pre-transplant chart evidence of non-adherence was associated with a 0.56 higher standard deviation of tacrolimus levels after transplantation.
Clinician Report of Non-Adherence
Among the medical charts reviewed in sample A, 97/444 (22 %) had chart evidence of non-adherence during the post-transplant period. The most common reasons were missed appointments (n = 57) and missed labs (n = 13). As shown in Table 3, on multivariable analysis, history of substance abuse and pre-transplant chart evidence of non-adherence are significant independent predictors of post-transplant chart evidence of non-adherence (p = 0.03 and <0.001, respectively).
Self-Reported Non-Adherence
Among the 165 survey respondents, 122 had complete data for analysis. Seventy-six out of 122 (62 %) reported being non-adherent with their medications at least once in the past 3 months. The most common infraction was missing a dose accidentally. Only 2 % of respondents admitted to being non-adherent “frequently” or “always.” Sixteen percent reported missing a doctor’s visit at least “sometimes,” with illness at the time of the appointment being the most common reason provided. On average, social support scores were relatively high (mean 4.1, with the maximum score being 5), with lower scores being associated with higher rates of reported non-adherence (p = 0.015). None of the pre-transplant variables listed above were associated with self-reported medication non-adherence (data not shown), though this could have been due to the small sample size.
Correlation Between Methods
Chart evidence of post-transplant non-adherence was associated with self-reported non-adherence (odds ratio 2.5, p = 0.03, likelihood ratio Chi-square 4.8), as well as the standard deviation of tacrolimus (coefficient 0.43, p = 0.03, R 2 0.015). Self-report of non-adherence was associated with a 2.7 higher standard deviation of tacrolimus levels, but this association was not statistically significant (p = 0.03) possibly due to a smaller sample size of 122. These associations provide construct validity for the various measurement methods, and suggest that the standard deviation of tacrolimus is not purely caused by biologic variability, but also reflects medication non-adherence.
Sample B
Analysis of the 359 transplant recipients in sample B demonstrated that a higher SD level (increased drug variability) during the 6–18 month post-transplant period was associated with a higher risk of graft failure (hazard ratio 1.005 per unit increase in SD, p = 0.04). This relationship was independent of patient age, race, gender, date of transplant, or severity of illness as measured by the MELD score. In order to demonstrate this graphically, the patients on tacrolimus (n = 228) were divided into two groups of equal size based upon their standard deviation (high or low), and the survival curve is shown in Fig. 3.
Kaplan-Meier survival estimates. Survival curves for patients with standard deviation (SD) of tacrolimus that was lower than the median (n = 180) versus higher than the median (n = 179). The association between standard deviation of immunosuppressant level and survival was statistically significant in the adjusted analysis (see text). Sample B: Analysis of 228 liver transplant recipients on tacrolimus from 1995 to 2003 who were followed for at least 5 years post-transplant. Higher SD level (increased drug variability) during the first 6–18 months post-transplant was associated with a higher risk of graft failure (hazard ratio 1.005 per unit increase in standard deviation, p = 0.04)
Discussion
This study aimed to compare three different methods for measuring non-adherence in liver transplant recipients, and to determine the impact of non-adherence on graft survival. We found evidence of non-adherence in 22–62 % of subjects, with the highest rates indicated by self-report. All three measures were correlated with one another, thus demonstrating construct validity. The standard deviation of tacrolimus stands out as being the only objective measure, and was independently associated with graft failure over time. If this finding is confirmed in prospective studies, patients with widely fluctuating tacrolimus levels should be targeted for behavioral interventions to improve graft survival.
It is striking that more than two-thirds of transplant recipients surveyed reported being non-adherent with their medications at least once in the prior month, and this behavior was significant enough to be documented in the medical record in one-quarter of subjects. This finding is consistent with high rates of self-reported non-adherence in transplant recipients [6, 21]. In a single-center US study, 56 % of transplant recipients reported non-adherence within the 2–5 year post-transplant period [14]. Various international studies have reported rather low rates of non-adherence among liver transplant recipients [12], which may be attributed to differences in methodology and social factors (i.e., differences in access to medical care and medications in US vs. non-US health care systems).
The only consistent predictor that could be identified from the pre-transplant setting was the reliability that patients displayed in obtaining labs and/or showing up for clinic visits. These behaviors are commonly used in the clinical setting to predict adherence, and our study substantiates this practice. Missed office appointments has been shown to be correlated with IS therapy non-adherence, which was confirmed in this study [14]. Pre-transplant substance abuse and non-adherence were found to be significantly associated with post-transplant non-adherence as measured by chart evidence. This finding has been substantiated by other studies using self-reported measures of non-adherence [14, 17]. When using high SD tacrolimus levels as a measure of post-transplant non-adherence, pre-transplant unemployment was significantly associated with non-adherence; however, this was not substantiated using other measurements of non-adherence.
Importantly, only 33 % of patients with pre-transplant chart evidence of non-adherence had evidence of non-adherence in the post-transplant setting, and 14 % of patients without such indicators pre-transplant did become non-adherent. Thus, more accurate and objective metrics are needed for determining transplant candidacy with respect to adherence.
Tacrolimus variability in the immediate post-transplant setting was found to be independently associated with graft failure over time. The association between drug variability and graft failure was strongest in the early post-transplant period (days 1,000–2,000). This finding suggests that consistent immunosuppressive therapy is especially critical in the early post-transplant period, when there is increased risk for graft rejection.
Deviations in tacrolimus levels may be a cost-effective and clinically useful tool for predicting transplant outcomes. This is one of various methods to assess non-adherence to IS therapy. One problem with using drug variability as a measure of non-adherence is that it does not take into account the dynamic process of medication consumption, which may vary due to fluctuating renal function, medication metabolism, drug–drug interactions and side-effects [15, 27]. Electronic medication monitoring has been suggested as the most sensitive measure of non-adherence [13, 19]. However, it is an expensive and labor-intensive method of measuring non-adherence with the potential for Hawthorne bias. In a cross-sectional study of kidney transplant recipients, a comparison was made between the diagnostic accuracy of various methods of measuring non-adherence including: electronic monitoring, immunosuppressant drug assay, patient self-report, and physician collateral report [27]. Individual measures of non-adherence were found to have poor sensitivity, whereas a composite adherence score compiled of non-adherence information from patient self-report, medical team collateral report, and drug assay had the highest sensitivity [6, 14, 27]. This can be a difficult task in the clinical setting, and using drug variability as a measure of non-adherence may be a cost-effective and easy-to-use clinical tool that should be further evaluated for its diagnostic accuracy of non-adherence.
Our study was limited by its single-center nature, and the fact that we were unable to capture all transplant recipients in our various sub-samples. In particular, although we achieved a reasonable 55 % response rate to our mailed survey, this sample reflects only 37 % of transplant recipients during the study period due to the length of follow-up. Moreover, our responders were not ethnically diverse with a low percentage being among African American and Hispanic minorities. Patients among ethnic minorities may be at increased risk for non-adherence; however, this has not been substantiated in the literature [14]. Additionally, those who are non-adherent may be less likely to complete the surveys or alternatively died before being surveyed due to non-adherent behaviors. The most important limitation, however, is the fact that transplant recipients themselves are already a selected group, with the least adherent patients usually deemed not to be candidates. For this reason, prospective studies are needed.
Furthermore, our study did not delve into the important question of why patients are non-adherent. We investigated the association between levels of social support and adherent behaviors; however, given a majority of our sample reported having good social support, we were unable to tease out the effects of support on post-transplant behaviors. A study from Spain among renal and liver transplant recipients suggested that increased number of tablets, frequency of dosing, and side-effects pose potential barriers to adherence [12]. Taking into account these potential barriers to adherence and the importance of stable therapeutic immunosuppressant levels for graft outcomes suggested by this study, one might consider advocating newer once-daily extended-release formulations of immunosuppressants such as tacrolimus, which may ensure sustained drug blood levels and improved adherence [28–30]. Adherence may also be related to personality styles such as impulsivity and poor coping skills [31], as well as levels of “conscientiousness” [17]. Additional questions to consider in future studies include whether healthcare providers give adequate support to transplant recipients. Are patients equipped with the proper tools—including education and access to health care resources—that would enable them to achieve their therapeutic goals? Our findings suggest that patients at risk for non-adherence, including those with a history of substance abuse, should be carefully followed after liver transplantation with additional supports provided by social workers, psychologists, and physicians. Currently, there is scarce data on the most effective interventions for increasing medication adherence post-transplantation; however, the literature suggest a multi-disciplinary approach to chronic disease management [32].
In summary, non-adherence to recommended medical care is a common problem in liver transplant recipients, and is independently associated with worse outcomes. Our findings lend support for the use of standard deviation of immunosuppressant levels as a screening tool for non-adherence. Further studies are needed to determine whether interventions targeted towards non-adherent patients could improve outcomes. Predicting which liver transplant candidates are most likely to be adherent remains a difficult and subjective clinical problem.
References
Martin AP, Bartels M, Hauss J, Fangmann J. Overview of the MELD score and the UNOS adult liver allocation system. Trans Proc. 2007;39:3169–3174.
Volk M. Personal communication. In: Lieber S, ed. City; 2010.
Aranda-Michel J, Dickson RC, Bonatti H, Crossfield JR, Keaveny AP, Vasquez AR. Patient selection for liver transplant: 1-year experience with 555 patients at a single center. Mayo Clinic Proc. 2008;83:165–168.
Chisholm MA, Lance CE, Williamson GM, Mulloy LL. Development and validation of the immunosuppressant therapy adherence instrument (ITAS). Patient Educ Couns. 2005;59:13–20.
Denhaerynck K, Dobbels F, Cleemput I, et al. Prevalence, consequences, and determinants of nonadherence in adult renal transplant patients: a literature review. Trans Int. 2005;18:1121–1133.
Dew MA, DiMartini AF, De Vito Dabbs A, et al. Rates and risk factors for nonadherence to the medical regimen after adult solid organ transplantation. Transplantation. 2007;83:858–873.
Lisson GL, Rodrigue JR, Reed AI, Nelson DR. A brief psychological intervention to improve adherence following transplantation. Ann Trans. 2005;10:52–57.
Falkenstein K, Flynn L, Kirkpatrick B, Casa-Melley A, Dunn S. Non-compliance in children post-liver transplant. Who are the culprits? Pediatr Trans. 2004;8:233–236.
Stuber ML, Shemesh E, Seacord D, Washington J III, Hellemann G, McDiarmid S. Evaluating non-adherence to immunosuppressant medications in pediatric liver transplant recipients. Pediatr Trans. 2008;12:284–288.
Venkat VL, Nick TG, Bucuvalas JC, Wang Y. An objective measure to identify pediatric liver transplant recipients at risk for late allograft rejection related to non-adherence. Pediatr Trans. 2008;12:67–72.
Shemesh E, Shneider BL, Savitzky JK, et al. Medication adherence in pediatric and adolescent liver transplant recipients. Pediatrics. 2004;113:825–832.
Morales JM, Varo E, Lazaro P. Immunosuppressant treatment adherence, barriers to adherence and quality of life in renal and liver transplant recipients in Spain. Clin Transpl. 2012;26:369–376.
Drent G, Haagsma EB, Geest SD, et al. Prevalence of prednisolone (non)compliance in adult liver transplant recipients. Transpl Int. 2005;18:960–966.
Lamba S, Nagurka R, Desai KK, Chun SJ, Holland B, Koneru B. Self-reported non-adherence to immune-suppressant therapy in liver transplant recipients: demographic, interpersonal, and intrapersonal factors. Clin Transpl. 2012;26:328–335.
Fine RN, Becker Y, De Geest S, et al. Nonadherence consensus conference summary report. Am J Transpl. 2009;9:35–41.
Osterberg L, Blaschke T. Drug therapy—adherence to medication. N Engl J Med. 2005;353:487–497.
Dobbels F, Vanhaecke J, Dupont L, et al. Pretransplant predictors of posttransplant adherence and clinical outcome: an evidence base for pretransplant psychosocial screening. Transplantation. 2009;87:1497–1504.
Chisholm MA. Enhancing transplant patients’ adherence to medication therapy. Clin Transpl. 2002;16:30–38.
Drent G, De Geest S, Haagsma EB. Prednisolone noncompliance and outcome in liver transplant recipients. Transpl Int. 2006;19:342–343.
Telles-Correia D, Barbosa A, Mega I, Monteiro E. Psychosocial predictors of adherence after liver transplant in a single transplant center in Portugal. Prog Transpl. 2012;22:91–94.
Kung M, Koschwanez HE, Painter L, Honeyman V, Broadbent E. Immunosuppressant nonadherence in heart, liver, and lung transplant patients: associations with medication beliefs and illness perceptions. Transplantation. 2012;93:958–963.
Dew MA, DiMartini AF, Steel J, et al. Meta-analysis of risk for relapse to substance use after transplantation of the liver or other solid organs. Liver Transpl. 2008;14:159–172.
Ediger JP, Walker JR, Graff L, et al. Predictors of medication adherence in inflammatory bowel disease. Am J Gastroenterol. 2007;102:1417–1426.
O’Carroll RE, McGregor LM, Swanson V, Masterton G, Hayes PC. Adherence to medication after liver transplantation in Scotland: a pilot study. Liver Transpl. 2006;12:1862–1868.
Medical Outcomes Study Social Support Survey (MOSSS). Available at: http://www.rand.org/health/surveys_tools/mos/mos_socialsupport.html. Accessed 7/2010; Sherbourne CD SA. The MOS social support survey. Soc Sci Med. 1991;32:705–714.
Telles-Correia D, Barbosa A, Mega I, Monteiro E. Adherence correlates in liver transplant candidates. Transpl Proc. 2009;41:1731–1734.
Schafer-Keller P, Steiger J, Bock A, Denhaerynck K, De Geest S. Diagnostic accuracy of measurement methods to assess non-adherence to immunosuppressive drugs in kidney transplant recipients. Am J Transpl. 2008;8:616–626.
Beckebaum S, Iacob S, Sweid D, et al. Efficacy, safety, and immunosuppressant adherence in stable liver transplant patients converted from a twice-daily tacrolimus-based regimen to once-daily tacrolimus extended-release formulation. Transpl Int. 2011;24:666–675.
Dharancy S, Giral M, Tetaz R, Fatras M, Dubel L, Pageaux GP. Adherence with immunosuppressive treatment after transplantation: results from the French trial PREDICT. Clin Transpl. 2012;26:E293–E299.
Merli M, Di Menna S, Giusto M, et al. Conversion from twice-daily to once-daily tacrolimus administration in liver transplant patient. Transpl Proc. 2010;42:1322–1324.
Stilley CS, DiMartini AF, de Vera ME, et al. Individual and environmental correlates and predictors of early adherence and outcomes after liver transplantation. Prog Transpl. 2010;20:58–66; quiz 67.
De Bleser L, Matteson M, Dobbels F, Russell C, De Geest S. Interventions to improve medication-adherence after transplantation: a systematic review. Transpl Int. 2009;22:780–797.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix: Survey Materials
Appendix: Survey Materials



Rights and permissions
About this article
Cite this article
Lieber, S.R., Volk, M.L. Non-Adherence and Graft Failure in Adult Liver Transplant Recipients. Dig Dis Sci 58, 824–834 (2013). https://doi.org/10.1007/s10620-012-2412-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2412-0