Abstract
Background
Achalasia is characterized by esophageal aperistalsis and impaired relaxation of the lower esophageal sphincter (LES). This contrasts with an insufficient LES, predisposing to gastro-esophageal reflux and Barrett’s esophagus. The co-incidence of achalasia and BE is rare. Pneumatic dilatation (PD) may lead to gastro-esophageal reflux, Barrett’s esophagus development, and esophageal adenocarcinoma.
Aims
To determine the incidence of Barrett’s esophagus and esophageal adenocarcinoma in achalasia patients treated with PD.
Methods
We performed a single-center cohort follow-up study of 331 achalasia patients treated with PD. Mean follow-up was 8.9 years, consisting of regular esophageal manometry, timed barium esophagram, and endoscopy.
Results
Twenty-eight (8.4 %) patients were diagnosed with Barrett’s esophagus, one at baseline endoscopy. This corresponds with an annual incidence of Barrett’s esophagus of 1.00 % (95 % CI 0.62–1.37). Hiatal herniation was present in 74 patients and 21 developed Barrett’s esophagus compared to seven of 257 patients without a hiatal hernia. Statistical analysis revealed a hazard ratio of 8.04 to develop Barrett’s esophagus if a hiatal hernia was present. Post-treatment LES pressures were lower in patients with Barrett’s esophagus than in those without (13.9 vs. 17.4 mmHg; p = 0.03). Two (0.6 %) patients developed esophageal adenocarcinoma during follow-up.
Conclusions
Barrett’s esophagus is incidentally diagnosed in untreated achalasia patients despite high LES pressures, but is more common after successful treatment, especially in the presence of hiatal herniation. Patients treated for achalasia should be considered for GERD treatment and surveillance of development of Barrett’s esophagus, in particular, when they have low LES pressures and a hiatal herniation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Achalasia and Barrett’s esophagus are generally thought to be the opposing ends of the spectrum of esophageal disease, although both relate to malfunctioning of the lower esophageal sphincter (LES). Achalasia is a rare neuro-degenerative disorder with an annual incidence of 1 per 100,000 inhabitants [1]. It is characterized by aperistalsis of the esophageal body and high basal LES pressure without a swallow-induced relaxation of the LES. Predominant symptoms of achalasia are dysphagia and regurgitation, often accompanied by weight loss.
In contrast, Barrett’s esophagus is a more common condition with increasing prevalence up to 1.6 % [2–5]. Barrett’s esophagus is characterized by the replacement of normal squamous cell epithelium by specialized intestinal columnar epithelium. Patients with Barrett’s esophagus have an increased risk of developing esophageal adenocarcinoma [6]. Although the exact etiology of Barrett’s metaplasia is incompletely understood, there is a clear relationship with gastro-esophageal reflux disease (GERD) [7]. In contrast to achalasia, GERD is associated with hiatal hernia, low resting pressure of the LES, and an increased frequency of transient LES relaxations, both facilitating the reflux of acid gastric contents [8].
Treatment of achalasia aims at reducing LES pressure. This is generally achieved by surgical myotomy or pneumatic dilatation (PD) [9]. The effect of PD treatment depends on age, LES pressure 3 months after dilatation, obliteration of the balloon waist during dilatation, and symptoms of classic achalasia [10]. Effective therapy resulting in a low LES pressure may, however, lead to GERD, which in theory may predispose to Barrett’s esophagus. Few data exist on the incidence of GERD after treatment of achalasia, both because of the lack of performance of specific diagnostic procedures such as 24-h pH monitoring after achalasia treatment and limited cohort follow-up data in achalasia patients. However, GERD has been reported in 11–25 % of achalasia patients following myotomy and in 2 % following PD [11]. Even fewer data exist on the development of Barrett’s esophagus in patients who underwent treatment for achalasia.
We hypothesized that adequate PD treatment for achalasia may be complicated by the development of Barrett’s esophagus and possibly esophageal adenocarcinoma. We therefore studied the incidence of and risk factors for Barrett’s esophagus and the development of esophageal adenocarcinoma in a large cohort of achalasia patients treated with PD.
Methods
Patients
Since 1975, all patients with achalasia referred to our hospital have been treated and followed according to a fixed protocol as described before [10]. The diagnosis and treatment protocol did not change over time and was performed by a limited number of physicians. The diagnostic process included the medical history and physical examination, esophageal manometry, a timed barium esophagram, and an upper GI-endoscopy. During manometry, a mean resting LES pressure was recorded as a mean of four (end-expiratory) measurements. LES relaxations and peristalsis of the esophageal body were studied. A timed barium esophagram was performed after swallowing 200 ml barium contrast with standardized records after 0, 1, and 10 min. An upper GI endoscopy was done to rule out other causes of dysphagia. Signs of gastro-esophageal reflux disease were noted. A hiatal hernia was diagnosed during insertion and only when the distance between the gastro-esophageal junction and the aperture of the diaphragm was more then 2 cm.
Therapy
Once a diagnosis of primary achalasia had been established or confirmed, all patients were offered treatment with PD on three consecutive days with an increasing balloon diameter of respectively 30, 35, and 40 mm. The balloons were in the very early days homemade, with a balloon inside a linen cuff with a length of 12 cm and fixed diameters of 30, 35, and 40 mm. In later years, Rigiflex pneumatic dilatation balloons (Boston Scientific, Natick, MA, USA) were used. Dilatation was performed under conscious sedation and fluoroscopic control up to a pressure of 300 mmHg. All pneumatic dilatations were over the years performed by a total of three endoscopists experienced in pneumatic dilatation.
Follow-Up
Every patient was followed according to a fixed protocol. Three months after PD, patients were interviewed for esophageal complaints, the patient’s weight was recorded, and esophageal manometry and barium swallow were repeated. This evaluation, including upper gastrointestinal (GI) endoscopy, was repeated after 1, 2, 4, and 7 years.
Upper GI endoscopy included random biopsy (3–4 biopsies) sampling from the distal esophagus just above the gastro-esophageal junction and targeted biopsy sampling from any specific lesion, such as suspected Barrett’s epithelium, dysplasia, or malignancy. For histological examination, 4 μm hematoxylin and eosin (H&E)-stained routine histological sections were used. In case of suspected Barrett’s esophagus, four biopsies were obtained (one from each quadrant) of every 2 cm of columnar epithelium to assess the presence of intestinal type columnar epithelium. Esophagitis was diagnosed both endoscopically, graded according the Los Angeles classification (grade A–D), and histologically. Barrett’s esophagus was endoscopically classified as short-segment (<3 cm) or long-segment Barrett’s esophagus. Hiatal hernia was assessed during introduction of the endoscope with limited inflation, and diagnosed when the distance between the gastro-esophageal junction (GEJ) and the aperture of the diaphragm was more than 2 cm.
Further follow-up after 7 years consisted of an interview and upper GI endoscopy with biopsy sampling at least every 3 years. Some patients refused these interval endoscopies or other long-term follow-up. These patients were contacted by telephone every year to check on symptoms and weight loss. In case of symptom recurrence or persistence, patients were either retreated with PD or underwent surgical myotomy, depending on the time of relapse, success of initial treatment, and patient’s preferences [10]. If a patient had died, the cause of death was checked with the general practitioner or the civil registration.
Statistics
The development of Barrett’s esophagus and hiatal hernia were expressed as Barrett’s-free and hiatal hernia-free survival curves, calculated by means of the Kaplan–Meier method. The univariate effect of patient characteristics is given as hazard ratios estimated by Cox proportional hazards analyses together with the log-likelihood p values. Statistically significant variables, as well as other clinically relevant variables (age, gender) were included in a multivariate Cox’s proportional hazards analysis. By means of step-wise backward elimination, a final model was constructed comprising variables that were significantly and independently (i.e., controlled for other variables) related to the endpoints Barrett’s esophagus or hiatal hernia, respectively. As a hiatal hernia event during follow-up often was followed by development of Barrett’s epithelium, the effect of hiatal hernia on Barrett-free survival was included in the Cox’s proportional hazard model as a time-dependent covariate. For all Cox models, the assumption of proportional hazards was investigated for each variable by studying the ln(−ln)plot. All analyses were carried out in SPSS for Windows, version 11.0.1 (SPSS, Chicago, IL). The level of statistical significance was set at a two-sided p < 0.05. LES pressures were measured during esophageal manometry before and after treatment, the Wilcoxon signed-rank test was applied to compare these.
Results
Therapy
Over the period of 1975–2003, 394 patients were referred to our hospital with a clinical suspicion of achalasia. Fourteen patients were diagnosed with secondary achalasia caused by malignancy, 16 patients had a non-specific motility disorder, five patients had diffuse esophageal spasms, and in ten patients, no specific diagnosis was made. The remaining 349 patients were diagnosed with primary achalasia. Six (2 %) of these 349 patients refused treatment for various reasons, another six were treated elsewhere, one preferred surgery, and in five patients, severe co-morbidity prohibited any treatment.
The remaining cohort consisted of 331 patients (male/female 160/171, mean age at diagnosis 51 years, range 4–90 years). They were followed for a median period of 8.9 years (range 3 months to 25 years). Sixty (18 %) patients had received previous treatment [pneumatic dilatation or myotomy (n = 19) before referral but they nevertheless presented with persistent symptoms and were offered dilatation again.
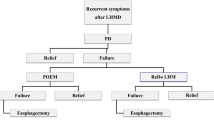
All 331 patients were initially treated with PD. After this initial treatment, 241 (73 %) patients had a persistent remission of symptoms, whereas 88 (27 %) patients were re-dilatated and three (1 %) patients were treated with myotomy because of symptom persistence or recurrence. Eventually during long follow-up, another 13 (4 %) patients underwent surgical myotomy after repeated dilatation. Of these 16 operated patients, six again had symptom recurrence for which treatment with pneumatic dilatation was applied. The majority of patients were treated immediately after the establishment of the diagnosis of achalasia.
Most patients underwent post-treatment endoscopy, 18 (5 %) patients refused routine follow-up endoscopy according to the protocol. During follow-up, 86 (26 %) patients died. In total, 14 (4 %) patients developed esophageal cancer, these included 12 patients with squamous cancers and two patients with adenocarcinoma. One of these patients was treated by esophagectomy and has since then a long disease-free survival. The other patient first was diagnosed with high-grade dysplasia for which she was treated with endoscopic mucosal resection followed by ablative therapy (photodynamic therapy). In the resection specimen, intramucosal carcinoma was present. This patient developed a relapse adenocarcinoma with hepatic metastases 6 years afterwards. Sixty-four (19 %) patients were lost to follow-up after a mean follow-up of 6 years (range 0–19 years) after PD.
Development of Erosive Esophagitis
Data on esophageal histology and endoscopy have been published earlier [12]. In brief, 66 % of patients did not develop any endoscopic signs of esophagitis during follow-up. Grade A esophagitis occurred in 22 % of the patients and 11 % was diagnosed with grade B–D esophagitis according to the Los Angeles Classification system at any time during the follow-up. Histological examination, however, showed a higher prevalence of esophagitis.
Development of Barrett’s Esophagus
Twenty-eight (8.4 %) of the 331 patients were diagnosed with Barrett’s esophagus (Fig. 1). This group consisted of 12 males and 16 females, all Caucasian. Their mean age when diagnosed with a Barrett’s esophagus was 55.9 years (range 35–84 years). One patient was diagnosed with Barrett’s esophagus at baseline endoscopy, whereas new development of Barrett’s metaplasia was observed in the other 27 Barrett’s patients. The remaining 27 (8.2 %) patients developed a Barrett’s esophagus during follow-up at a mean interval of 67 months (range 6–224 months) after initial treatment with PD. This corresponds with an annual incidence of Barrett’s esophagus in this population of 1.00 % (95 % CI 0.62–1.37) (Fig. 2). Nineteen patients had a Barrett’s esophagus less than 3 cm in length; the other nine had a long segment varying in length from 3 to 7 cm. The characteristics of patients with and without Barrett’s esophagus are listed in Table 1. Both groups did not differ with respect to age or sex. Barrett’s esophagus tended to be more common after myotomy, but this difference was not significant (RR = 2.5 95 % C.I [1.00; 6.19] (p = 0.07).
Development of Esophageal Adenocarcinoma
During follow-up, 2/28 (7 %) of patients with a Barrett’s esophagus developed esophageal adenocarcinoma. This occurred 25 and 27 years after the initial diagnosis of achalasia, at an age of 70 and 84 years, respectively. Both patients had started with endoscopic surveillance from the time of first balloon dilation onwards for a period of 18 and 14 years, respectively. In these patients, the development of esophageal carcinoma was not preceded by the finding of dysplasia in the random surveillance biopsies, the last of which had been obtained 1 and 2 years, respectively, prior to cancer diagnosis.
Hiatal Hernia
A hiatal hernia was present in 74 (22 %) of the 331 patients. Sixteen patients were diagnosed with a hiatal hernia prior to PD treatment and the remaining 58 patients after PD treatment.
Twenty-one (28 %) patients with a hiatal hernia developed a Barrett’s esophagus compared to seven (2 %) of the 257 patients without a hiatal hernia. Three of the 21 patients with hiatal hernia and Barrett’s esophagus had a hiatal hernia at the time of diagnosis of achalasia. The remaining 18 patients developed a hiatal hernia at a mean of 6 years (range 1–15 years) after PD treatment. Statistical analysis using a time-dependent Cox regression analysis revealed a hazard ratio of 8.04 (95 % CI 3.5–18.1), p < 0.001 to develop a Barrett’s esophagus if a hiatal hernia is present (Fig. 3). In a univariate Cox regression analysis, older age appeared as a significant factor in the development of hiatal hernia, in contrast with sex, myotomy, and LES pressure. Statistical analysis of the correlation between Barrett’s esophagus and the later development of hiatal hernia also showed significance (HR 8.8, 95 % CI 4.32–17.9, p < 0.001). The results are listed in Table 2.
LES Pressures
LES pressures were measured before and after treatment. As expected for the total group of achalasia patients, post-treatment LES pressures were lower than pre-treatment LES pressures (median 15.0 vs. 30.0 mmHg; p < 0.001, Wilcoxon signed-rank test) indicating effective dilatation treatment. The LES pressures before or after treatment were not significantly related to development of a hiatal hernia.
Patients with a post-treatment basal LES pressure lower or equal to 15 tended to be at higher risk to develop Barrett’s esophagus: HR = 2.17 95 % CI [0.88; 5.56], p = 0.07 (Table 1).
Finally, a multivariate Cox’s proportional hazards analysis on the development of Barrett’s esophagus and hiatal hernia was performed with all clinically relevant variables as age, gender, therapy, LES pressures, and hiatal hernia included (Table 3). Age was a significant factor involved in the development of hiatal hernia, but not in Barrett’s esophagus. In contrast, myotomy and a post-PD LESP <15 mmHg were significantly related to the development of Barrett’s esophagus, but not related to hiatal hernia.
Use of Acid-Suppressive Medication
Over time, patients in our cohort used a range of different acid-suppressive therapies, usually for short periods of time such as after diagnosing esophagitis at endoscopy. In the total cohort, 27 % used any kind of suppressive therapy at any time during follow-up, and 9.5 % ever used a PPI during follow-up. Of the 28 patients with Barrett’s esophagus, nine (32 %) patients took no acid-lowering medication at any time during the follow-up, six (19 %) patients only used antacids, four (14 %) used H2-receptor antagonists, and nine (32 %) patients were treated with different kinds of acid-lowering therapies among which were proton-pump inhibitors. Of the patients who developed an adenocarcinoma, one was on PPI-treatment and the other on H2 antagonist treatment.
Discussion
To our knowledge, only a limited number of patients have been described with the combination of achalasia and a Barrett’s esophagus [13–15]. This includes a few patients who developed Barrett’s esophagus after PD [14], seven patients who were diagnosed with Barrett’s esophagus without being treated for their achalasia [14, 16], and 31 patients who had undergone surgical myotomy many years prior to the detection of Barrett’s esophagus [14, 15]. Six (16 %) of these 39 patients were simultaneously or later diagnosed with esophageal adenocarcinoma.
The incidence of esophageal adenocarcinoma in patients with Barrett’s esophagus is considered to be approximately 0.5 % per year of follow-up [17, 18] Therefore, the estimated 16 % prevalence of esophageal adenocarcinoma in patients with achalasia and Barrett’s esophagus as deducted from this figures above seems high.
This is the first study that systematically investigated the relationship between achalasia treated with PD, Barrett’s esophagus, and esophageal adenocarcinoma. We observed that 8.4 % of 331 patients with achalasia developed a Barrett’s esophagus, in a single case prior to treatment, but mostly after PD treatment. Risk factors associated with the development of Barrett’s esophagus were the presence of a hiatal hernia, prior myotomy and a lower LES pressure. During follow-up, 2/28 (7 %) patients with Barrett’s esophagus developed an esophageal adenocarcinoma.
Myotomy was performed in 35 patients. In 19 patients this had occurred before referral, yet these 19 patients received renewed pneumatic dilatation for recurrent symptoms after surgery. Another 16 patients were treated with myotomy during FU, six of them received additional dilatation after surgery. Both treatment modalities have the same goal, namely disrupting the LES muscle fibers. A recent study could not show a superiority in success rate of myotomy [19].
The combination of achalasia and Barrett’s esophagus is considered to be rare, as only 39 cases of achalasia with Barrett’s esophagus have been reported in the literature, mostly after myotomy [14, 15]. Although Barrett’s esophagus and achalasia seem to be disorders at the opposing ends of a spectrum, our results show that there is an association between treatment of achalasia, leading to an insufficient LES, and the development of a Barrett’s segment. In our population, the prevalence of Barrett’s esophagus in achalasia patients after treatment was 7.4 %, with an annual incidence of newly development of Barrett’s esophagus of 1.0 % corresponding with a 1,000 new cases per 100,000 subjects/year.
These findings contrast with data on the prevalence and incidence of Barrett’s esophagus in the general population. Endoscopy and autopsy series have suggested a prevalence of 1 % in Western populations [20]. This prevalence may, however, be higher in selected populations. One study for instance reported a 25 % prevalence of Barrett’s esophagus in a population of male veterans [21]. Estimates for the number of new cases per year vary between ten and 48 per 100,000 inhabitants [22, 23]. We recently observed an annual incidence of 24.7 per 100,000/year in a Dutch population of 386,000 subjects followed for 3.4 years [2]. In conclusion, our data suggest that patients treated for achalasia have a higher risk of developing Barrett’s esophagus than the general population. As there is no age- and sex-comparable control population in our study, of course there is surveillance bias. In the absence of such a population, we can only make an indirect comparison with other data. Klinkenberg-Knol et al. [24] observed that 20 (12 %) of 166 patients with severe reflux disease treated with omeprazole developed Barrett’s metaplasia during an average 6.5 years follow-up with annual endoscopy. This incidence is in the same order of magnitude as our observation of Barrett’s metaplasia in 7.3 % of our achalasia patients during an average 8.9 years follow-up.
Several hypotheses may explain the association between achalasia and Barrett’s esophagus. The most obvious hypothesis is that efficient treatment leads to insufficiency of the LES predisposing to GERD and possibly to its complications [25]. This is supported by the association between a lower LES pressure and the development of Barrett’s esophagus in our cohort and also by our findings that esophagitis is very common during follow-up after PD [12].
Although all achalasia patients were at each visit asked for esophageal complaints, it can be difficult to discriminate symptoms related to the primary motility disorder and those related to the secondary reflux after treatment. Since most achalasia patients have persistent esophageal complaints, we were unable to find a clear correlation between classical reflux symptoms and the development of Barrett’s esophagus after achalasia treatment.
Twenty-seven percent of all patients in our cohort used acid-suppressive medication at any time during long-term follow-up, predominantly for short-term periods. This proportion was higher among the patients diagnosed with Barrett’s esophagus. Our cohort study does not allow any conclusions whether this use of acid-suppressive medication in any way interfered with the rate of progression to Barrett’s metaplasia and further [26].
Surprisingly, in the literature and also in our study, a few achalasia patients appeared to have BE already prior to baseline treatment. One hypothesis is that the development of Barrett’s esophagus had already occurred before achalasia started. Secondly, it has recently been shown that transient LES relaxations (TLESRs) accompanied by acid reflux may also occur in achalasia patients [27]. The combination of TLESR-induced acid reflux with impaired esophageal clearance may therefore be an explanation for the observed development of Barrett’s esophagus in both treated and untreated achalasia patients. A last explanation could be that in (untreated) achalasia patients, chronic food stasis and fermentation of retained food may cause chronic esophageal inflammation, predisposing to Barrett’s esophagus [16, 20, 28–31].
Apart from TLESRs as a predisposing mechanism to reflux, the presence of a hiatal hernia is also an important etiologic factor in the development of GERD and Barrett’s esophagus. Various studies have reported a prevalence of hiatal hernia in 95 % of patients with severe reflux and Barrett’s esophagus with a length of 3 cm or more and 74 % in shorter Barrett’s esophagus [3, 32, 33]. We found that 28 % of patients with a hiatal hernia developed BE in contrast to only 3 % of achalasia patients without a hiatal hernia and the presence of a hiatal hernia after treatment of achalasia revealed a hazard ratio of 8.04 to develop Barrett’s esophagus. We were surprised to find that 74 out of 331 (23 %) achalasia patients had a hiatal hernia. Previous cross-sectional studies in achalasia have reported a prevalence varying between 1.4 and 2.3 % [34–36]. Goldenberg et al. [37] described a higher prevalence, i.e., 14.1 % hiatal hernias in achalasia probably because radiographic examinations were reviewed. They found that eight of ten radiographically demonstrated hiatal hernias had not been recorded in the clinical records proving underreporting probably because of the seemingly triviality of the diagnosis. The assessment of hiatal hernias poses some difficulties. Both barium swallow and upper GI endoscopy in particular have limited sensitivity in diagnosing small herniation [38, 39]. High-resolution manometry may be the most accurate instrument to diagnose these small herniations. We assessed the presence of a hernia during insertion of the scope and also used the retroflection view to grade the severity of the hernia and only diagnosed a hiatal hernia if the length was more than 2 cm.
Our results confirm that a hiatal hernia is not uncommon in achalasia patients and show that it is a significant risk factor for the development of Barrett’s esophagus after esophageal dilation (Fig. 3). Barrett’s esophagus is a pre-malignant condition predisposing to esophageal adenocarcinoma. The esophageal cancer risk in patients with a Barrett’s esophagus differed between 1/52 and 1/297 years of follow-up in different reports [17]. The incidence of adenocarcinoma in our achalasia patients with Barrett’s esophagus was 7.1 % (2/28) during an average 13.4 years follow-up, which corresponds to previously mentioned annual risk of 0.5 % [14]. Reviewing all the cases of achalasia combined with Barrett’s esophagus, Guo et al. [14] found that adenocarcinoma had occurred in 19 % of achalasia cases with Barrett’s esophagus, which developed a mean of 18 years after treatment for achalasia. The mean follow-up of the Barrett’s patients in our study was 13.4 years in total after achalasia diagnosis and 7.5 years after Barrett’s development. With longer follow-up, the incidence of Barrett’s esophagus and adenocarcinoma in our cohort may further increase. The presence of Barrett’s esophagus could have alerted both patients and physicians, but we found no significant difference (p = 0.4) in drop-out percentage between Barrett and non-Barrett patients.
In conclusion, patients with achalasia treated with pneumatic dilatation are at considerable risk for development of Barrett’s esophagus. We observed the development of Barrett’s esophagus in 28 (8.4 %) of 331 achalasia patients before treatment and during long-term follow-up. This implicates that achalasia and Barrett’s are not mutually exclusive disorders. In contrast, achalasia and LES lowering therapy should be considered a risk factor for the development of Barrett’s mucosa. Hiatal hernia and lower esophageal sphincter pressures increase the risk of developing Barrett’s esophagus. During endoscopic and radiographic follow-up of achalasia patients, careful attention should be paid to the presence of hiatal hernia, especially in combination with low LES pressures, since this combination strongly increases the risk for BE and eventually adenocarcinoma of the esophagus.
References
Mayberry JF. Epidemiology and demographics of achalasia. Gastrointest Endosc Clin North Am. 2001;11:235–248, v.
van Soest EM, Dieleman JP, Siersema PD, Sturkenboom MC, Kuipers EJ. Increasing incidence of Barrett’s oesophagus in the general population. Gut. 2005;54:1062–1066.
Cameron AJ, Lomboy CT. Barrett’s esophagus: age, prevalence, and extent of columnar epithelium. Gastroenterology. 1992;103:1241–1245.
Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825–1831.
van Blankenstein M, Looman CW, Johnston BJ, Caygill CP. Age and sex distribution of the prevalence of Barrett’s esophagus found in a primary referral endoscopy center. Am J Gastroenterol. 2005;100:568–576.
de Jonge PJ, van Blankenstein M, Looman CW, Casparie MK, Meijer GA, Kuipers EJ. Risk of malignant progression in patients with Barrett’s oesophagus: a Dutch nationwide cohort study. Gut. 2010;59:1030–1036.
Kauer WK, Stein HJ. Role of acid and bile in the genesis of Barrett’s esophagus. Chest Surg Clin N Am. 2002;12:39–45.
Schoeman MN, Tippett MD, Akkermans LM, Dent J, Holloway RH. Mechanisms of gastroesophageal reflux in ambulant healthy human subjects. Gastroenterology. 1995;108:83–91.
Walzer N, Hirano I. Achalasia. Gastroenterol Clin North Am. 2008;37:807–825, viii.
Alderliesten J, Conchillo JM, Leeuwenburgh I, Steyerberg EW, Kuipers EJ. Predictors for outcome of failure of balloon dilatation in patients with achalasia. Gut. 2011;60:10–16.
Reynolds JC, Parkman HP. Achalasia. Gastroenterol Clin North Am. 1989;18:223–255.
Leeuwenburgh I, Van Dekken H, Scholten P, et al. Oesophagitis is common in patients with achalasia after pneumatic dilatation. Aliment Pharmacol Ther. 2006;23:1197–1203.
Ellis FH Jr, Gibb SP, Balogh K, Schwaber JR. Esophageal achalasia and adenocarcinoma in Barrett’s esophagus: a report of two cases and a review of the literature. Dis Esophagus. 1997;10:55–60.
Guo JP, Gilman PB, Thomas RM, Fisher RS, Parkman HP. Barrett’s esophagus and achalasia. J Clin Gastroenterol. 2002;34:439–443.
Csendes A, Braghetto I, Burdiles P, Korn O, Csendes P, Henriquez A. Very late results of esophagomyotomy for patients with achalasia: clinical, endoscopic, histologic, manometric, and acid reflux studies in 67 patients for a mean follow-up of 190 months. Ann Surg. 2006;243:196–203.
Cantu P, Savojardo D, Baldoli D, Bonavina L, Penagini R. Barrett’s esophagus in untreated achalasia: ‘guess who’s coming to dinner’ first. Dis Esophagus. 2008;21:473.
Sikkema M, de Jonge PJ, Steyerberg EW, Kuipers EJ. Risk of esophageal adenocarcinoma and mortality in patients with Barrett’s esophagus: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2010;8:235–244; quiz e232.
Shaheen NJ, Crosby MA, Bozymski EM, Sandler RS. Is there publication bias in the reporting of cancer risk in Barrett’s esophagus? Gastroenterology. 2000;119:333–338.
Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–1816.
Burke CA, Achkar E, Falk GW. Effect of pneumatic dilation on gastroesophageal reflux in achalasia. Dig Dis Sci. 1997;42:998–1002.
Gerson LB, Shetler K, Triadafilopoulos G. Prevalence of Barrett’s esophagus in asymptomatic individuals. Gastroenterology. 2002;123:461–467.
Prach AT, MacDonald TA, Hopwood DA, Johnston DA. Increasing incidence of Barrett’s oesophagus: education, enthusiasm, or epidemiology? Lancet. 1997;350:933.
Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456.
Klinkenberg-Knol EC, Nelis F, Dent J, et al. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety, and influence on gastric mucosa. Gastroenterology. 2000;118:661–669.
Spiess AE, Kahrilas PJ. Treating achalasia: from whalebone to laparoscope. JAMA. 1998;280:638–642.
Kuipers EJ. Barrett’s oesophagus, proton pump inhibitors and gastrin: the fog is clearing. Gut. 2010;59:148–149.
van Herwaarden MA, Samsom M, Smout AJ. Prolonged manometric recordings of oesophagus and lower oesophageal sphincter in achalasia patients. Gut. 2001;49:813–821.
Benini L, Sembenini C, Castellani G, et al. Pathological esophageal acidification and pneumatic dilitation in achalasic patients. Too much or not enough? Dig Dis Sci. 1996;41:365–371.
Crookes PF, Corkill S, DeMeester TR. Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci. 1997;42:1354–1361.
Stamp DH. Three hypotheses linking bile to carcinogenesis in the gastrointestinal tract: certain bile salts have properties that may be used to complement chemotherapy. Med Hypotheses. 2002;59:398–405.
Orlando RC. Overview of the mechanisms of gastroesophageal reflux. Am J Med. 2001;111:174S–177S.
Ott DJ, Gelfand DW, Chen YM, Wu WC, Munitz HA. Predictive relationship of hiatal hernia to reflux esophagitis. Gastrointest Radiol. 1985;10:317–320.
Ott DJ, Hodge RG, Chen MY, Wu WC, Gelfand DW. Achalasia associated with hiatal hernia: prevalence and potential implications. Abdom Imaging. 1993;18:7–9.
Binder HJ, Clemett AR, Thayer WR, Spiro HM. Rarity of hiatus hernia in achalasia. N Engl J Med. 1965;272:680–682.
Olsen AM, Holman CB, Andersen HA. The diagnosis of cardiospasm. Dis Chest. 1953;23:477–498.
Taub W, Achkar E. Hiatal hernia in patients with achalasia. Am J Gastroenterol. 1987;82:1256–1258.
Goldenberg SP, Vos C, Burrell M, Traube M. Achalasia and hiatal hernia. Dig Dis Sci. 1992;37:528–531.
Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601–616.
Hyun JJ, Bak YT. Clinical significance of hiatal hernia. Gut Liver. 2011;5:267–277.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leeuwenburgh, I., Scholten, P., Caljé, T.J. et al. Barrett’s Esophagus and Esophageal Adenocarcinoma Are Common After Treatment for Achalasia. Dig Dis Sci 58, 244–252 (2013). https://doi.org/10.1007/s10620-012-2157-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2157-9