Abstract
Background
In ulcerative colitis (UC), reduction of inflammation may represent a key mechanism in UC therapy, and anti-inflammatory agents would be good candidates for preventing UC. Kaempferol, a natural flavonoid, is believed to have anti-inflammatory activities and has been shown to be potentially immune-modulatory.
Aims
The aim of this study was to determine whether kaempferol alleviates the inflammatory responses of dextran sulfate sodium (DSS)-induced colitis in mice.
Methods
Female C57BL/6J mice were divided into six groups: a negative control group, a DSS control group, and DSS + 0.1% or 0.3% kaempferol pre- or post-fed groups. At the end of the experimental period, clinical and biochemical markers were evaluated.
Results
Plasma levels of NO and PGE2 were significantly decreased in both the 0.3% kaempferol pre- and post-fed groups. The plasma LTB4 level was profoundly decreased in all animals fed kaempferol. Colonic mucosa MPO activity was also suppressed in both the 0.3% kaempferol pre- or post-fed groups. TFF3 mRNA, a marker for goblet cell function, was up-regulated in kaempferol pre-fed animals.
Conclusions
These results indicate that kaempferol is an effective anti-inflammatory agent that protects colonic mucosa from DSS-induced UC. Dietary kaempferol fed prior to colitis induction was more effective to suppress some of the colitis-associated markers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ulcerative colitis, particularly the chronic persistent form, is an intractable disease. Despite our increased understanding of mucosal homeostasis, therapeutic modalities facilitating colonic repair have not been well established. Therapies for UC rely highly on the use of immunosuppressive drugs such as 5-ASA and corticosteroids [1]. However, many patients either do not respond to these agents or demonstrate significant side-effects. New developments in treating IBD can be found in biological treatments with antibodies directed against tumor necrosis factor-α (TNF-α) [2] and with pro- and pre-biotics [3]. However, these do not offer an ideal cure due to the long course of treatment, various adverse reactions, and the tendency of patients to relapse when treatment stops. Therefore, there is a great need to develop effective agents or treatments with fewer adverse reactions.
Dextran sulfate sodium (DSS)-induced colitis is a well-established experimental model in which many of the signs and symptoms of human ulcerative colitis, including diarrhea, bloody feces, weight loss, mucosal ulceration, and shortening of the large intestine also occur. Although the mechanisms by which DSS-induced colitis have remained unknown, recent studies have revealed that DSS increases intestinal permeability and causes injury to the epithelium, suggesting dysfunction of the mucosal defense systems. Moreover, DSS increases the level of colonic myeloperoxidase (MPO) and the production of inflammatory mediators such as nitric oxide (NO) and prostaglandin E2 (PGE2) [4, 5].
Flavonoids have been suggested to exert human health benefits possibly because they are mediated by their anti-oxidant and anti-inflammatory activities. Among the known flavonoids, kaempferol is widely distributed in fruits, vegetables, and plant-based foods.
Kaempferol has been reported to have strong anti-inflammatory properties [6–8]. In our preliminary study, kaempferol had the most effective anti-inflammatory activities among eight polyphenols in the LPS-induced Raw 264.7 model [9]. However, little is known regarding its effects on DSS-induced colitis which is related to dysfunction of intestinal immunity and is characterized the up-regulated inflammation in the colon. Inflammatory conditions are characterized by activation of the transcription factor nuclear factor-κB (NF-κB), resulting in the expression of NF-κB-regulated, inflammation-related genes, such as inducible nitric oxide synthase (iNOS) and cyclooxygenase-2 (COX-2). In fact, many studies have indicated significant over-expression of these markers in DSS-induced colitis model [10–12] and colitis patients [13]. Because kaempferol effectively inhibited the expression of these biomarkers in both our preliminary study and other studies, kaempferol may modulate inflammatory mediators in inflammatory diseases model. The present study was designed to investigate whether kaempferol modulates inflammatory biomarkers, which in turn contributes to amelioration of colitis-related symptoms.
Materials and Methods
Animals and Experimental Design
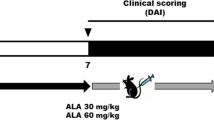
Female C57BL/6J mice were obtained at 6 weeks of age from Jung-Ang Lab Animal Inc. (Seoul, Korea) and were maintained in air-conditioned quarters with 12-h light/dark cycles. They were given a commercial rat food (Jung-Ang Lab Animal Inc., Seoul, Korea) and water ad libitum. The animals were allowed to acclimatize to the laboratory environment for 1 week and were randomly divided into six groups (n = 10 per each group); two groups (noncolitic and control colitic groups) were fed a control diet, two groups were post-fed the kaempferol diets (0.1 and 0.3% kaempferol diets), and the remaining two groups were pre-fed the kaempferol diets (0.1 and 0.3% kaempferol diets) (Fig. 1). Two weeks after the start of the experiment, five groups of mice were allowed to have free access to drinking water containing 2% DSS (wt/v, MW 36,000–50,000) for 4 days, while the control group were given free access to drinking water without DSS. Since kaempferol is a food component, not a synthetic drug, it is expected to exert alleviating effects on mild ulceration. Based on our preliminary study, we found 2% DSS concentration in drinking water caused mild ulceration in the colon. The drinking water with DSS was prepared daily. The compositions of the experimental diet are shown in Table 1. Animals were maintained on the experimental diets for 3 weeks (Fig. 1). Animals were maintained in accordance with university guidelines for the care and use of laboratory animals.
Reagents
DSS and kaempferol were obtained from MP Biomedicals Inc. (Solon, OH, USA) and INDOFINE Chemical Co. (Hillsborough, NJ, USA), respectively. The Trizol reagent was purchased from Invitrogen Inc. (Carlsbad, CA, USA) and mouse enzyme-linked immunosorbent assay (ELISA) kits for the LTB4, NO, and PGE2 measurements were purchased from R&D System Inc. (Minneapolis, MN, USA). Other chemicals were obtained from Sigma-Aldrich (St. Louis, MO, USA).
Disease Activity Index and Histological Observation
The disease activity index (DAI) was determined by scoring changes in weight loss (score: 0, none; 1, 1–5%; 2, 5–10%; 3, 10–20%; 4, >20%), stool consistency (score: 0, normal; 2, loose; 4, diarrhea) and rectal bleeding (score: 0, normal; 2, occult bleeding; 4, dross bleeding) [14]. All parameters were scored from day 14 to day 21 during DSS treatment. At the end of experiment, the mice were killed and the colons and spleens were dissected. The colon length was measured from the ileocecal junction to the proximal rectum and the weights of spleens, a systemic marker for disease progression of ulcerative colitis, were measured. Tissue was obtained from each distal colon 1 cm beyond the anus for histological observation. The specimens were subsequently fixed in a 10% buffered formalin solution. The cut specimen was dehydrated in ethanol, embedded in paraffin wax, sectioned, and stained with hematoxylin and eosin (H&E). Histological analysis was performed by an investigator blinded to the treatment, for severity of inflammation (score: 0, none; 1, weak; 2, moderate; and 3, severe), extent of inflammation (score: 0, none; 1, mucosal; 2, mucosal and submucosal; 3, transmural) and crypt damage (score: 0, none; 1, basal 1/3; 2, basal 2/3; 3, crypt lost but surface epithelium present and 4, crypts and surface epithelium lost).
Preparation of the Blood and Tissue Samples
At the end of the experiment, the mice were sacrificed by exsanguination of the heart under light ether anesthesia and blood was collected by cardiac puncture in 5% EDTA vials. To determine LTB4, NO, and PGE2, the plasma was separated, frozen immediately, and stored at −70°C until the assays. The colon was quickly removed and rinsed with ice-cold PBS. The distal segments were randomly selected from each group and were fixed in 10% formalin solution. Other colon segments of mice were used for biochemical measurements. To do this, the colonic mucosa was scraped with glass slides, frozen immediately in liquid nitrogen, and stored at −70°C until use.
Colonic MPO Activity
The colonic myeloperoxidase activity was measured according to a modification of the method of Krawisz et al. [15]. The colon tissue was rinsed with cold saline, and the mucosa was scraped with glass slides on ice and homogenized in 50 mM phosphate buffer containing 0.5% hexadecyl-trimethyl-ammonium bromide (HTAB; pH 6.0; sigma). The homogenized samples were frozen-thawed three times and centrifuged at 2,000 rpm for 10 min at 4°C. The supernatant (100 μl) was mixed with the reaction mixture (1.9 ml of 10 mM phosphate buffer (pH 6.0) and 1 ml of 1.5 M o-dianisidine hydrochloride containing 0.0005% w/v hydrogen peroxide) and was maintained at 25°C for 6 min. The MPO activity was calculated from the rate of change absorbance during 1 min. The results were expressed as MPO units/g protein; 1 unit of MPO activity was defined as that degrading 1 μmol hydrogen peroxide/min at 25°C.
Plasma LTB4 Concentration
The plasma leukotriene (LT) B4 concentration in the plasma was measured by ELISA according to the manufacturer’s protocol.
Plasma NO and PGE2 Concentrations
The circulating NO and PGE2 concentrations were measured by using ELISA kit according to the manufacturer’s instructions.
Real-Time Quantitative PCR
Total RNA was isolated from cells using the Trizol reagent according to the manufacturer’s instructions. Real-time quantitative PCR was performed in triplicate in 384-well plates. A 384-well high-throughput analysis was performed using the ABI Prism 7900 Sequence Detection System (PE Applied Biosystems, www.appliedbiosciences.com) and white-colored 384-well plates (AB gene, Hamburg, Germany) were used for the intensification of the fluorescent signals by a factor of three. The fluorescence emission from each sample was collected using a charge-coupled-device camera and the quantitative data were analyzed using the Sequence Detection System software (SDS version 2.0, PE Applied Biosystems). The reaction mixtures contained 10 pmol/μl of each primer and 2× SYBR Green PCR Master Mix (PE Applied Biosystems, www.appliedbiosciences.com), which includes HotStarTaqt DNA-Polymerase in an optimized buffer, a dNTP mix (with dUTP additive), SYBRs Green I fluorescent dye, and ROX dye as a passive reference. The primer sequences were as follows: for TFF3, sense 5′-GTG GAC TGC GGC TAC CCC CAT-3′ and antisense 5′-AAG GTG CAT TCT GCT TCC TGC-3′ [16]; for iNOS, sense 5′-TCC TGT GGC ATC CAT GAA ACT-3′ and antisense 5′-GGA GGA GCT GAT GGA GTA GTA G-3′ [17]; for COX-2, sense 5′-CTC GCG ATG CTC TTC CGA G-3′ and antisense 5′-AAG GAT TTG CTG CAT GGC TG-3′ [18]; for TNF-α, sense 5′-AGC ACA GAA AGC ATG ATC CG-3′ and antisense 5′-CTG ATG AGA GGG AGG CCA TT-3′ [18]; for IL-1β, sense 5′-ACC TGC TGG TGT GTG ACG TT-3′ and antisense 5′-TCG TTG CTT GGT TCT CCT TG-3′ [18]; for IL-6, sense 5′-GAG GAT ACC ACT CCC AAC AGA CC-3′ and antisense 5′-AAG TGC ATC ATC GTT GTT CAT ACA-3′ [18]; for β-actin, sense 5′-TCC TGT GGC ATC CAT GAA ACT-3′ and antisense 5′-GAA GCA TTT GCG GTG CAC GAT-3′ [17]. The thermal cycling conditions were 50°C for 2 min and 95°C for 10 min followed by 40 cycles of 95°C for 30 s, 60°C for 30 s, and 72°C for 30 s. The real-time PCR mRNA levels were normalized to rat β-actin mRNA level ± SD.
Statistics
All data from the experiment are expressed as means ± SD. Data were compared using a one-way analysis of variance (ANOVA) followed by Duncan’s multiple range test. In all statistical analyses, a p value of <0.05 was considered to be statistically significant.
Results
Disease Activity Index, Colon Length, and Spleen Enlargement
At day 21, mice fed experimental diets supplemented with kaempferol showed significantly lower DAI scores compared to mice in the control group (p < 0.05) (Table 2). DSS treatment significantly reduced the colon length (p < 0.05), while the 0.3% kaempferol diet effectively reversed the DSS-induced shortening of the colon (p < 0.05) (Table 2). DSS control mice exhibited significantly higher spleen weight compared to vehicle control group, and kaempferol pre-diet decreased spleen weights in these mice (p < 0.05) (Table 2).
Histological Observation
The histology of colon sections of DSS-treated mice revealed multiple erosive lesions, inflammatory cell infiltration and crypt shortening (Fig. 2). The mice fed 0.3% kaempferol pre-diet showed profoundly less deformity of the tissue compared to the DSS control mice (p < 0.05) (Table 2), indicating kaempferol pre-diet has preventive effect on DSS-induced UC model.
Histological observation of the colon. Histological sections of the colonic mucosa from each group stained with hematoxylin and eosin showing the anti-inflammatory effects of the kaempferol-supplemented diets. a Group 1 (DSS-); b Group 2 (DSS +); c Group 3 (D + K 0.1%); d Group 4 (D + K 0.3%); e Group 5 (K 0.1% + D); f Group 6 (K 0.3% + D) (× 100)
Colonic MPO Activity and Plasma LTB4 Concentration
DSS administration increased colonic MPO activity and 0.3% kaempferol diets (groups 4 and 6) were found to decrease MPO activity significantly compared to the levels observed in the DSS control mice (group 2) (Fig. 3a, p < 0.05). The level of plasma LTB4, a neutrophil chemotactic factor, was significantly increased in the DSS control group (group 2) when compared with its basal level in the normal group (group 1) (Fig. 3b). The plasma level of LTB4 profoundly decreased in all animals fed kaempferol diets compared with the DSS control mice (group 2) (Fig. 3b), p < 0.05).
Effects of kaempferol diets on colonic MPO activity and on the plasma LTB4 level in C57BL/6 J mice. The mice were pre- or post-fed kaempferol-supplemented diets for 3 weeks, with 2% DSS added to tap water. After 3 weeks, MPO activities in the colonic mucosa (a) and the concentration of LTB4 in plasma (b) were measured. The black or white bar represents non-supplemented diets in the presence or absence of DSS treatment, respectively. DSS (−), non-colitic group; DSS (+), DSS control group; D + K (0.1%), post-fed 0.1% kaempferol diet group; D + K (0.3%), post-fed 0.3% kaempferol diet group; K (0.1%) + D, pre-fed 0.1% kaempferol diet group; K (0.3%) + D, pre-fed 0.3% kaempferol diet group. Each bar represents the mean ± SD. The bars with different letters differ significantly (p < 0.05) from each other
Plasma NO and PGE2 Concentrations
Increased NO has been demonstrated in inflammatory disease (IBD). Prostaglandins, especially PGE2, are known to as potent activators of inflammation, and many studies have reported that increased levels of PGE2 are correlated with disease activity. The plasma level of the levels of PGE2 and NO were significantly decreased in both 0.3% kaempferol pre- and post-fed animals (Figs. 4B, 5B, p < 0.05).
Effects of kaempferol diets on colonic mucosa COX-2 and iNOS mRNA expressions and on the plasma PGE2 and NO levels in C57BL/6 J mice. The mice were pre- or post-fed kaempferol-supplemented diets for 3 weeks, with 2% DSS added to tap water. After 3 weeks, colonic COX-2 (a) and iNOS (c) mRNA expressions and the concentrations of PGE2 (b) and NO (d) in plasma were measured. The black or white bar represents non-supplemented diets in the presence or absence of DSS treatment, respectively. DSS (−), non-colitic group; DSS (+), DSS control group; D + K (0.1%), post-fed 0.1% kaempferol diet group; D + K (0.3%), post-fed 0.3% kaempferol diet group; K (0.1%) + D, pre-fed 0.1% kaempferol diet group; K (0.3%) + D, pre-fed 0.3% kaempferol diet group. Each bar represents the mean ± SD. The bars with different letters differ significantly (p < 0.05) from each other
Effects of kaempferol diets on colonic TNF-α, IL-1β, and IL-6 mRNA expressions in C57BL/6 J mice. The mice were pre- or post-fed kaempferol-supplemented diets for 3 weeks, with 2% DSS added to tap water. After 3 weeks, colonic iNOS mRNA expression (a) and the concentration of NO (b) in plasma were measured. The black or white bar represents non-supplemented diets in the presence or absence of DSS treatment, respectively. DSS (−), non-colitic group; DSS (+), DSS control group; D + K (0.1%), post-fed 0.1% kaempferol diet group; D + K (0.3%), post-fed 0.3% kaempferol diet group; K (0.1%) + D, pre-fed 0.1% kaempferol diet group; K (0.3%) + D, pre-fed 0.3% kaempferol diet group. Each bar represents the mean ± SD. The bars with different letters differ significantly (p < 0.05) from each other
Colonic COX-2 and iNOS mRNA Expression Level
To investigate whether the inhibitions of PGE2 and NO production are related to the modulation of the COX-2 and iNOS gene level, RT-PCR analyses for COX-2 and iNOS mRNA expression were performed. The COX-2 and iNOS mRNA levels were significantly increased in the DSS control group (Group 2) compared to the normal group (Group 1). The expressions were significantly down-regulated by both 0.3% kaempferol pre- and post-fed animals (Figs. 4A, 5A, p < 0.05).
Colonic TFF3 mRNA Expression Level
The expression of trefoil factor family 3 (TFF3) was used as parameters for the goblet cell function. TFF3 mRNA expression was significantly decreased in the distal colon mucosa of mice after acute colitis (group 2) when compared with its basal level in a normal group (group 1) (Fig. 6, p < 0.05). The gene expression was significantly up-regulated by 0.1 and 0.3% kaempferol pre-fed animals (Fig. 6, p < 0.05), implying that pre-fed kaempferol promotes epithelial cell repair.
Effects of kaempferol diets on colonic mucosa TFF3 mRNA expression level in C57BL/6 J mice. The mice were pre- or post-fed kaempferol-supplemented diets for 3 weeks, with 2% DSS added to tap water. After 3 weeks, colonic TFF3 mRNA expression was measured. The black or white bar represents non-supplemented diets in the presence or absence of DSS treatment, respectively. DSS (−), non-colitic group; DSS (+), DSS control group; D + K (0.1%), post-fed 0.1% kaempferol diet group; D + K (0.3%), post-fed 0.3% kaempferol diet group; K (0.1%) + D, pre-fed 0.1% kaempferol diet group; K (0.3%) + D, pre-fed 0.3% kaempferol diet group. Each bar represents the mean ± SD. The bars with different letters differ significantly (p < 0.05) from each other
Colonic Pro-inflammatory Cytokines mRNA Expression Level
TNF-α, IL-1β, and IL-6 contribute to tissue damage in DSS-induced colitis. The colon mucosa TNF-α, IL-1β, and IL-6 mRNA expressions were increased to 7.2-, 4.5-, and 2.2-fold over basal level, respectively, in animal fed 2% DSS drinking water (p < 0.05). The colonic mRNA expressions of TNF-α, IL-1β, and IL-6 were significantly suppressed in both 0.3% kaempferol pre-fed animals (Fig. 5, p < 0.05).
Discussion
Ulcerative colitis (UC) is a mucosal inflammatory disease that causes ulcerations of the colon. It exhibits increased risk for the development of colon cancer. The prevalence of UC in Asian populations is lower than in Western populations [19]; however, an epidemiological study from Korea showed that both UC and Crohn’s disease (CD) are becoming increasingly prevalent in Korean population [20]. Therapies for IBD rely highly on the use of glucocorticoids, sulfasalazine, and immunosuppressive drugs such as 5-ASA and corticosteroids. However, these pharmacological treatments as yet do not offer an ideal cure due to different side-effects or toxicity, which remains a major clinical problem [21]. Therefore, there is a great need to develop an effective agent or treatment with fewer adverse reactions.
Polyphenols are a group of phytochemicals that are found in plant foods. They are believed to have many biologically activities and have been shown to be potentially immune-modulatory [22]. Given that inflammatory stress contributes to UC, reduction of inflammation may represent a key mechanism in UC therapy, and anti-inflammatory agents would be good candidates for UC prevention. The aim of this study was to investigate the preventive and therapeutic effect of kaempferol on DSS-induced colitis. The results of this study showed that DSS induces a considerable amount of inflammation with increased blood levels of inflammatory mediators and increased expression of colon COX-2 and iNOS mRNA. Histological examination of the colonic tissue sections was also conducted; the samples from the DSS-induced colitic mice showed profound changes in their colonic architecture, such as mucosal ulcerations, crypt destruction, erosion and goblet cell depletion (Fig. 2). Conversely, histological analyses of the colons from the kaempferol-treated mice showed a decreased degree of tissue (Fig. 2).
The exact etiology of DSS-induced ulcerative colitis is not fully understood, however, DSS induced colitis by direct cytotoxicity and this barrier dysfunction is likely to result in both increased uptake of luminal antigens and activation of inflammatory response [23]. Recent studies have demonstrated that the imbalance of pro-inflammatory cytokines and anti-inflammatory cytokines are related to the pathogenic mechanisms of UC [24]. Activation of the PI3K/Akt and NF-κB signal transduction pathway facilitate the expression and secretion of pro-inflammatory cytokines which create imbalanced cytokine profiles [25]. In this study, kaempferol diets effectively down-regulated the colonic mRNA expression level of the major pro-inflammatory cytokines, e.g., TNF-α, IL-1β, and IL-6, which indicate that kaempferol plays a role in the cytokines production. TNF-α can activate multiple inflammatory cells as well as increase epithelial and vascular endothelial cell permeability. In UC model, the levels of cytokines are influenced by several inflammation-related cells such as macrophages, neutrophils, leukocytes, and others. MPO is an index of neutrophil recruitment in UC model. Therefore, MPO activity may reflect more specific inflammatory events compared to cytokine concentration. In this study, both the colonic MPO activity and blood LTB4 level were significantly increased in the DSS group compared to the non-colitic mice, and all groups supplemented with kaempferol showed significantly decreased concentrations of these markers. Animals pre-treated with kaempferol showed a higher degree of reduction than those treated by post-feeding. This observation is supported by data from literature. Regasini et al. [26] reported that kaempferol derivative markedly decreased MPO activity when compared with other flavonols. Another comparative study by Kanashiro et al. [27] showed that kaempferol significantly inhibit human neutrophil degranulation.
Pro-inflammatory eicosanoids, LTB4 and PGE2, are metabolites of arachidonic acid and are implicated in inflammation. We found that kaempferol diet resulted in significantly decreased levels of LTB4 and PGE2 in the plasma of the DSS-induced UC mice (Figs. 3, 4b). LTB4 plays a permissive role in the action of neutrophils during the amplification of intestinal inflammatory reaction [28]. The increased levels of COX-2-derived PGE2 are found at sites of intestinal inflammation and correlate with disease activity [29]. The effects of PGE2 are mediated through the EP2/EP4 receptors on dendritic cells [30] and an EP4 agonist ameliorates typical colitis symptoms by suppressing the production of several cytokines in the DSS-induced colitis model [31]. In the present study, all kaempferol-supplemented diets were shown to decrease colonic COX-2 mRNA expression significantly, and the pre- or post-fed 0.3% kaempferol diet group showed a markedly decreased plasma PGE2 level. Although the exact mechanism of kaempferol is not fully understood, kaempferol effectively inhibited the transport of MRP1-mediated LTC4, a leukotriene family, and inhibited phospholipase A2 group IIA (PLA2-IIA) which leads to a decrease in eicosanoids levels and to reduced inflammation [32, 33]. Together, these data suggest that a diet supplemented with kaempferol influences the inflammatory cell release and activation by the down-regulation of TNF-α and the modulation of arachidonic acid metabolism.
TNF-α also activates immune cells and release of inflammatory mediators, e.g., NO, which facilitates inflammatory reaction. Excessive amounts of reactive nitrogen species produced via iNOS during chronic inflammation may play a key role in the pathogenesis of colitis-associated neoplasia [34]. In our experiments, the pre- or post-fed 0.3% kaempferol diet group showed a significant decrease in both colonic iNOS mRNA expression and in their blood NO level. Hämäläinen et al. [8] reported that kaempferol inhibits NF-κB, a significant transcription factor for iNOS. They also found that it inhibited the activation of the signal transducer and activator of transcription 1 (STAT-1), another important transcription factor for iNOS, in activated macrophages [8]. The inflamed IBD luminal epithelium, but not the inflammatory cells, also contained increased amounts of NOS, and its immunoreactivity was significantly higher in UC than in CD [35].
Trefoil factor families (TFFs) were subsequently measured to determine whether kaempferol exerts an effect on mucosal protection and repair. TFFs have been used as parameters for goblet cell function, which plays a critical role in mucosal protection and repair [36]. TFF3, the major TFF, is able to enhance epithelial cell migration and reconstitute the gastrointestinal tract [37]. Although many aspects of TFF3 biology are unknown, there is evidence indicating that TFF3 plays a role in IBD. The TFF3 promoter is known to control TGFβ type II receptors, and deficiency of TGFβ signaling, specifically in the intestine, contributes to the development of IBD [38]. Podolsky et al. [39] demonstrated that the UC-associated TLR2-R753Q variant is functionally deficient in the ability to induce TFF3 synthesis. Feng et al. [37] reported that TFF3 was significantly decreased in the distal colon mucosa in the DSS-induced colitis model and partially recovered at the regenerative phase. These findings indicate that goblet cell-derived TFF3 was possibly related to the pathogenesis of ulcerative colitis. The results indicated that TFF3 mRNA expression was significantly decreased in the distal colon mucosa of mice treated with DSS and was up-regulated in the kaempferol pre-fed animals. These findings imply that pre-fed kaempferol diets maintain and repair the goblet cell function and help the related epithelial repair capacity during acute inflammation induced by DSS. The experimental 0.1–0.3% kaempferol levels are 1–3 g/day and that are about 15 times higher level than the daily dietary intake in humans [40].
In summary, kaempferol is concluded to be a protective and therapeutic compound in acute DSS-induced colitis. The beneficial effects of kaempferol appear to be related to the decreased production of inflammatory mediators, and some proportion of the mechanisms may be involved in arachidonic acid metabolism. Kaempferol also displayed epithelial cell repair capacity, which suggests other possible applications in gastrointestinal health.
References
Caprilli R, Angelucci E, Cocco A, et al. Efficacy of conventional immunosuppressive drugs in IBD. Dig Liver Dis. 2004;36:766–780.
Sandborn WJ. Strategies for targeting tumour necrosis factor in IBD. Best Pract Res Clin Gastroenterol. 2003;17:105–117.
Geier MS, Butler RN, Howarth GS. Inflammatory bowel disease: current insights into pathogenesis and new therapeutic options; probiotics, prebiotics and synbiotics. Int J Food Microbiol. 2007;115:1–11.
Holma R, Salmenperä P, Virtanen I, et al. Prophylactic potential of montelukast against mild colitis induced by dextran sulphate sodium in rats. J Physiol Pharmacol. 2007;58:455–467.
Kwon HS, Oh SM, Kim JK. Glabridin, a functional compound of liquorice, attenuates colonic inflammation in mice with dextran sulphate sodium-induced colitis. Clin Exp Immunol. 2008;151:165–173.
Havsteen BH. The biochemistry and medical significance of the flavonoids. Pharmacol Ther. 2002;96:67–202.
Middleton E, Kandaswami C, Theoharides TC. The effects of plant flavonoids on mammalian cells: implications for inflammation, heart disease, and cancer. Pharmacol Rev. 2000;52:673–751.
Hämäläinen M, Nieminen R, Vuorela P, et al. Antiinflammatory effects of flavonoids: genistein, kaempferol, quercetin, and daidzein inhibit STAT-1 and NF-κB activations, whereas flavone, isorhamnetin, naringenin, and pelargonidin inhibit only NF-κB activation along with their inhibitory effect on iNOS expression and nitric oxide production in activated macrophages. Mediat Inflamm. 2007;2007:45673.
Park MY, Kwon HJ, Sung MK. Evaluation of aloin and aloe-emodin as anti-inflammatory agents in aloe by using murine macrophages. Biosci Biotechnol Biochem. 2009;73:828–832.
Cho EY, Choi SC, Lee SH, et al. Nafamostat mesilate attenuates colonic inflammation and mast cell infiltration in the experimental colitis. Int Immunopharmacol. 2011;11:412–427.
Crespo I, García-Mediavilla MV, Gutiérrez B, et al. A comparison of the effects of kaempferol and quercetin on cytokine-induced pro-inflammatory status of cultured human endothelial cells. Br J Nutr. 2008;100:968–976.
Sánchez-Fidalgo S, Cárdeno A, Villegas I, et al. Dietary supplementation of resveratrol attenuates chronic colonic inflammation in mice. Eur J Pharmacol. 2010;633:78–84.
Hanai H, Sugimoto K. Curcumin has bright prospects for the treatment of inflammatory bowel disease. Curr Pharm Des. 2009;15:2087–2094.
Cooper HS, Murthy SN, Shah RS, et al. Clinicopathologic study of dextran sulfate sodium experimental murine colitis. Lab Invest. 1993;69:238–249.
Krawisz JE, Sharon P, Stenson WF. Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Assessment of inflammation in rat and hamster models. Gastroenterology. 1984;87:1344–1350.
Babyatsky M, Lin J, Yio X, et al. Trefoil factor-3 expression in human colon cancer liver metastasis. Clin Exp Metastasis. 2009;26:143–151.
Naito Y, Uchiyama K, Kuroda M, et al. Role of pancreatic trypsin in chronic esophagitis induced by gastroduodenal reflux in rats. J Gastroenterol. 2006;41:198–208.
Nakao A, Moore BA, Murase N, et al. Immunomodulatory effects of inhaled carbon monoxide on rat syngeneic small bowel graft motility. Gut. 2003;52:1278–1285.
Yang SK, Loftus EV, Sandborn WJ. Epidemiology of inflammatory bowel disease in Asia. Inflamm Bowel Dis. 2001;7:260–270.
Yang SK, Song IS, Kim YH. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986–2001: a KASID study. Gastroenterology. 2003;124:A210.
Louis E, Belaiche J, Reenaers C. Are we giving biologics too much time? When should we stop treatment? World J Gastroenterol. 2008;14:5528–5531.
Shapiro H, Singer P, Halpern Z, et al. Polyphenols in the treatment of inflammatory bowel disease and acute pancreatitis. Gut. 2007;56:426–435.
Joo YE, Karrasch T, Mühlbauer M, et al. Tomato lycopene extract prevents lipopolysaccharide-induced NF-kappaB signaling but worsens dextran sulfate sodium-induced colitis in NF-kappaBEGFP mice. PLoS One. 2009;4:e4562.
Hicks A, Monkarsh SP, Hoffman AF, et al. Leukotriene B4 receptor antagonists as therapeutics for inflammatory disease: preclinical and clinical developments. Expert Opin Investig Drugs. 2007;16:1909–1920.
Huang XL, Xu J, Zhang XH et al. PI3K/Akt signaling pathway is involved in the pathogenesis of ulcerative colitis. Inflamm Res. 2011.
Regasini LO, Vellosa JC, Silva DH, et al. Flavonols from Pterogyne nitens and their evaluation as myeloperoxidase inhibitors. Phytochemistry. 2008;69:1739–1744.
Kanashiro A, Souza JG, Kabeya LM, et al. Elastase release by stimulated neutrophils inhibited by flavonoids: importance of the catechol group. Z Naturforsch C. 2007;62:357–361.
Sharma JN, Mohammed LA. The role of leukotrienes in the pathophysiology of inflammatory disorders: is there a case for revisiting leukotrienes as therapeutic targets? Inflammopharmacology. 2006;14:10–16.
Singh VP, Patil CS, Jain NK, et al. Effect of nimesulide on acetic acid- and leukotriene-induced inflammatory bowel disease in rats. Prostaglandins Other Lipid Mediat. 2003;71:163–175.
Sheibanie AF, Yen JH, Khayrullina T, et al. The proinflammatory effect of prostaglandin E2 in experimental inflammatory bowel disease is mediated through the IL-23– > IL-17 axis. J Immunol. 2007;178:8138–8147.
Jiang GL, Nieves A, Im WB, et al. The prevention of colitis by E Prostanoid receptor 4 agonist through enhancement of epithelium survival and regeneration. J Pharmacol Exp Ther. 2007;320:22–28.
Leslie EM, Mao Q, Oleschuk CJ, et al. Modulation of multidrug resistance protein 1 (MRP1/ABCC1) transport and ATPase activities by interaction with dietary flavonoids. Mol Pharmacol. 2001;59:1171–1180.
Lättig J, Böhl M, Fischer P, et al. Mechanism of inhibition of human secretory phospholipase A2 by flavonoids: rationale for lead design. J Comput Aided Mol Des. 2007;21:473–483.
Kawanishi S, Hiraku Y, Pinlaor S, et al. Oxidative and nitrative DNA damage in animals and patients with inflammatory diseases in relation to inflammation-related carcinogenesis. Biol Chem. 2006;387:365–372.
Kruidenier L, Kuiper I, Lamers CB, et al. Intestinal oxidative damage in inflammatory bowel disease: semi-quantification, localization, and association with mucosal antioxidants. J Pathol. 2003;201:28–36.
Hoffmann W. TFF (trefoil factor family) peptides and their potential roles for differentiation processes during airway remodeling. Curr Med Chem. 2007;14:2716–2719.
Feng ZM, Fang DC, Chen WS, et al. Rodent IRR-219 (IgGFcgammaBP) and rTFF3, expressed mainly in the intestinal mucosa, depleted during dextran sulfate sodium-induced colitis. Dig Dis Sci. 2007;52:2104–2112.
Hahm KB, Im YH, Parks TW, et al. Loss of transforming growth factor beta signalling in the intestine contributes to tissue injury in inflammatory bowel disease. Gut. 2001;49:190–198.
Podolsky DK, Gerken G, Eyking A, Cario E. Colitis-associated variant of TLR2 causes impaired mucosal repair because of TFF3 deficiency. Gastroenterology. 2009;137:209–220.
Fink BN, Steck SE, Wolff MS, et al. Dietary flavonoid intake and breast cancer risk among women on Long Island. Am J Epidemiol. 2007;165:514–523.
Acknowledgments
This work was supported by the Korean Ministry of Health and Welfare Grant number A06-0546-AD-1101-06-N1-00020B and by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2010-0001886).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, MY., Ji, G.E. & Sung, MK. Dietary Kaempferol Suppresses Inflammation of Dextran Sulfate Sodium-Induced Colitis in Mice. Dig Dis Sci 57, 355–363 (2012). https://doi.org/10.1007/s10620-011-1883-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1883-8