Abstract
Background
Limited published data exist on the associated comorbid conditions with functional dyspepsia (FD).
Aims
This study aimed to assess the prevalence, services, and costs related to comorbid conditions associated with FD and the risk of having FD for each comorbid condition.
Methods
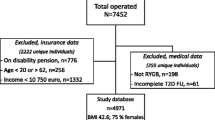
A retrospective database analysis was undertaken using payroll data and adjudicated claims from January 1, 2001, through December 31, 2004 among >300,000 employees. Employees with FD were compared to propensity-score-matched employees without FD (controls). Outcome measures included the prevalence, costs, and utilization of health services for comorbid conditions as defined by the Agency for Healthcare Research and Quality (AHRQ) and the odds ratios of having FD from a multivariate model.
Results
FD employees (N = 1,669) and a 50:1 matched control cohort (N = 83,450) were compared. Compared to matched controls, FD employees were more likely to have all major diagnostic categories. Moreover, 199/261 of the AHRQ’s specific categories were more common in the FD cohort. Annual medical costs for the FD cohort were greater than for controls in 155/261 (59%) specific categories and significantly greater (P ≤ 0.05) in 76 categories (29%). Similarly, services were greater for 179/261 (69%) specific categories and significantly greater (P ≤ 0.05) in 110 categories (42%). In a multivariate model, esophageal disorders, gastritis and duodenitis, and abdominal pain were the most associated with having FD (odds ratios 3.8, 3.7, and 3.6, respectively). Only hypertension complications and disorders of the teeth and jaw were significantly negatively associated with FD.
Conclusion
There is unexplained excess comorbidity associated with FD which may be a major determining factor for excess healthcare services and costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dyspepsia is characterized by pain and/or discomfort centered in the upper abdomen, and further refers to a symptom or set of symptoms that are considered by most physicians to originate from the gastroduodenal region, based on the recommendations of the Rome III committee [1]. Dyspepsia is thought to have a prevalence rate of about 20% in developed countries [2–7]. Functional dyspepsia (FD) is defined by the presence of one or more of four chronic symptoms (epigastric pain, epigastric burning, early satiety, or postprandial fullness) not related to any recognizable organic, systemic, or metabolic disease. Recently, comorbid conditions in functional gastrointestinal disorders (FGIDs) have received great attention, because patients with the irritable bowel syndrome (IBS), the best recognized FGID, often experience a broad set of non-gastrointestinal (GI) complaints [8–10]. Furthermore, patients with IBS and people with IBS in the community have shown a strong association with psychiatric disorders, which some have suggested account for multiple non-GI complaints and, potentially, has therapeutic implications [9, 10].
Very few studies have been published about comorbid conditions in FD [11–13], but have identified other FGIDs including IBS, gastroesophageal reflux disease (GERD), and sleep disorders as being possibly linked. On the other hand, an expanding body of literature has documented multiple comorbid conditions in IBS, which commonly overlaps with dyspepsia [12]. IBS and dyspepsia are both associated with somatization and frequent physician consultations [9, 10, 14, 15]. Thus, it is conceivable that FD is highly associated with multiple comorbid conditions, but this needs to be documented. We aimed here to describe for the first time the comorbidity of FD and determine whether the documented high costs associated with FD [16] are partly explained by these comorbid conditions. Using a large employee sample where we have previously described the costs of FD [16], our objectives in this study were to compare the prevalence, services, and costs related to comorbid conditions among employees with and without FD.
Methods
This retrospective analysis focused on a 4-year study period, from January 1, 2001, through December 31, 2004. Data were extracted from paid health insurance claims within the Human Capital Management Services (HCMS) research reference database containing data on more than 300,000 employees plus their eligible dependents as supplied by multiple, geographically diverse, US-based employers [16–18]. The data classify employees as non-exempt (generally hourly) or exempt (generally salaried and not eligible to receive overtime pay). Confidentiality and anonymity of person-level data were maintained in accordance with the guidelines of the Health Insurance Portability and Accountability Act of 1996.
The two cohorts were derived from the full database based on the presence or absence of primary, secondary, or tertiary ICD-9 (International Classification of Diseases, Ninth Revision) codes for FD diagnoses (ICD-9 code 536.8x) and those with no FD diagnoses.
Each subject was assigned an index date. For cohort FD, the index date was the date of the first FD diagnosis between 2001 and 2003. For employees without FD (controls), the index date was the average index date from the group of employees with FD. Because FD is a diagnosis of exclusion [1], in order to ensure that all relevant healthcare claims over a 12-month period for the identified patients were taken into account, the data capture period (or “measurement year”) for all subjects was from 3 months prior to the index date (first FD medical claim) to 9 months after the index date. The employees were required to have medical and prescription drug coverage for the entire measurement year to be included in the study. The 12-month time frame should remove any potential seasonality associated with FD.
Outcome Measures
Outcomes included the prevalence, average annual medical cost paid by the employer, and service utilization (called “reasons for visit or procedures during a visit”) per employee according to comorbid conditions. All billed procedures from an office visit are considered as individual services. In the present study, an examination might be one service and a blood test for an Helicobacter pylori examination would be a second service on the same date. Thus, a healthcare visit may encompass multiple services.
Comorbid conditions were classified according to two categorizations developed by the United States Agency for Healthcare Research and Quality (AHRQ): major diagnostic categories (MDCs) (ICD-9 codes grouped into 17 MDCs that encompass major organ-, disease-, and therapeutic-specific categories) and AHRQ specific categories (ICD-9 codes grouped into 261 more granular categories) [19]. Focusing on categories instead of individual ICD-9 codes avoids a potential double-counting for similar manifestations. Because the Rome committee [1] recommends that an upper endoscopic examination is needed in order to exclude other possible conditions, the costs and frequencies of endoscopies within the FD cohort were analyzed.
Because the data spanned several years, all cost variables were inflated to August 2009 US dollars using non-seasonally adjusted consumer price indices (CPIs) for medical services [20].
Statistical Analysis
Comparisons of the following descriptive statistics were performed between the two cohorts: age, tenure (the number of years which the employee has worked for his or her current employer), gender, marital status, race, exempt/non-exempt status, full-time/part-time status, annual salary, and region (grouped by the first digit of the employee’s ZIP code).
Differences in descriptive characteristics between the FD and control cohorts were compared using Students t-tests for continuous variables and Chi-square (χ2) tests for discrete variables.
To control for demographic differences between cohorts in the comorbidity components, “controls” were matched to “cases” from the FD cohort before average cost and utilization by comorbidity were compared. Using logistic regression, a propensity score was calculated from the following demographic variables: age, tenure, gender, marital status, race, exempt/non-exempt status, full-time/part-time status, and annual salary. Region was also included by dividing the United States into sections defined by the first digit of the ZIP code, resulting in ten general geographic areas. Prior to running the logistic regression, the few missing age and salary values in the data were replaced with cohort average age and salary values, and missing marital status and race values were treated as separate categories of those variables so that no employees would be excluded from the propensity score matching process because of missing data. Then, using this propensity score, 50 controls were matched to each FD case.
To compare cost and utilization by each comorbid category, the means and standard errors were calculated for each of the 17 MDCs and 261 specific categories for each cohort. Average costs and average number of services were calculated across all members of each cohort, not just across cohort members who had a given condition. Students t-tests (assuming unequal variances) were used to assess the significance of cost and utilization differences between cohorts.
Prevalence estimates were generated for each of the AHRQ specific categories and are expressed as a percentage of persons within the cohort with claims (and services) for the diagnostic category. Significant prevalence differences are identified using Woolf’s Chi-square statistic. In addition to quantifying the percentage for each cohort, a prevalence ratio is also provided, which compares the two cohorts. Coexisting condition prevalence is established during the measurement year. Rather than display all 261 specific categories, all GI-related categories and commonly associated non-GI-related categories are shown.
Using the population of matched FD (N = 1,669) and non-FD (N = 83,450) cohorts of employees, a logistic regression model was run in order to estimate the likelihood of being in the FD cohort. Independent variables in the model included indicator variables for 260 of the 261 specific AHRQ condition categories (the category containing FD was not included). Odds ratios for having FD were produced as part of the regression output using two logistic regression methods: one method used stepwise selection of categories, while the other method incorporated all categories. Odds ratios that were significantly different from 1.0 in the stepwise regression were reported. The odds ratios from the full model are available upon request. An odds ratio above 1.0 indicates that employees with the corresponding comorbid condition are more likely to be in the FD cohort, and an odds ratio less than 1.0 indicates that the employee is less likely to be in the FD cohort when compared with employees who do not have the corresponding comorbid condition.
All models and statistics were generated via version 9.1 of the SAS for Windows software package (SAS Institute, Inc., Cary, NC) and were considered to be statistically significant when P ≤ 0.05.
Results
A total of 275,875 employees were eligible for inclusion over the selected time frame: 1,669 employees with FD and 274,206 employees without FD [16]. Among those with FD, 1,363 (82%) of the employees had a primary ICD-9 diagnosis code for FD; 257 (15%) had, at best, a secondary code for FD; and 49 (3%) only had a tertiary code for FD. Using the 50:1 match, a propensity-score-matched control cohort of 83,450 persons without FD was matched to the 1,669 FD employees such that there were no statistically significant differences in any of the demographic fields. The demographic statistics for the FD and matched control cohort are presented in Table 1.
The annual prevalence, costs, and services of comorbid conditions by the 17 AHRQ MDCs are presented in Table 2. Employees in this study who had FD were more likely than employees without FD to have most of the comorbid conditions, including digestive disease, mental disorders, blood-related diseases, and so on, while the pregnancy and childbirth-related diseases were not significantly different between employees with or without FD. In addition, employees with FD also had significantly higher per-employee costs in 13 of the 17 MDCs and significantly higher services in 14 of the 17 MDCs (Table 2). The top MDC prevalence ratios between the two groups were for digestive systems (6.3:1), blood and blood-forming organs (2.6:1), mental disorders (2.1:1), and infectious and parasitic disease (2.0:1). Moreover, the FD cohort had a higher prevalence for 199 of the 261 AHRQ specific categories, with 76 categories being significantly (P < 0.05) higher (data not shown).
Gastrointestinal Comorbid Conditions
The annual prevalence, costs, and services of comorbid conditions by the AHRQ’s more specific GI-related categories are presented in Table 3. The most prevalent specific category, stomach/duodenum disorders, contains ICD-9 code 536.8x, which was part of the inclusion criteria for the FD group, and, as a result, everyone in the FD cohort had this condition category. Abdominal pain and esophageal disorders were the next most prevalent category among the FD cohort after stomach/duodenum disorders. Overall, all GI comorbid conditions were significantly more common in the FD cohort compared to controls, except cancer of the liver/hepatic duct. Moreover, upper and lower GI malignancies, such as those of the esophagus, stomach, colon, and rectum/anus, were more commonly observed in the FD cohort compared to controls. In addition, 25 of the 29 GI-related AHRQ categories had higher annual costs for the FD cohort, with 20 categories being significantly (P < 0.05) higher. Similar to the prevalence data, abdominal pain was the most costly ($489 for those with FD vs. only $57 for the controls) and most service-intensive for the FD cohort category (3.45 services per employee for those with FD vs. only 0.41 for the control cohort). Other items that also had statistically significantly higher (P < 0.05) costs per employee for the FD cohort include: biliary tract disease ($469 for those with FD vs. $49 for the controls), esophageal disorders ($252 vs. $20), cancer of the esophagus ($167 vs. $0), and gastritis and duodenitis ($240 vs. $12).
Twenty-one of these 29 categories had significantly higher annual services (P < 0.05) for the FD cohort. The top categories in the FD cohort included abdominal pain (3.45 services per employee in the FD cohort vs. 0.41 in the control cohort), stomach/duodenum disorders (2.49 vs. 0.01), biliary tract disease (1.01 for those with FD vs. 0.09 for controls), gastritis and duodenitis (0.87 vs. 0.05), and “other” GI disorders (0.99 vs. 0.15).
Endoscopies, including esophagogastroduodenoscopy (EGD; simple primary examination [n = 3, total cost = $734], diagnostic [n = 118, total cost = $66,837], or with biopsy [n = 399, total cost = $199,670]) and esophagoscopy (diagnostic [n = 6, total cost = $1,254] or with biopsy [n = 1, total cost = $660]), were recorded in the claims for one-third of the FD cohort (497/1,669 employees) during the measurement year.
Non-gastrointestinal Comorbid Conditions
The annual prevalence, costs, and services of comorbid conditions by the AHRQ’s specific non-GI-related categories are presented in Table 4 and were chosen to represent various diagnostic areas. Of these, other upper respiratory infections was the most prevalent category among the FD cohort. Respiratory, cardiovascular, genitourinary, and musculoskeletal diseases were more commonly prevalent in the FD cohort than among controls. Moreover, neurologic/psychiatric disease including migraine, personality disorders, and affective disorders were more commonly reported in the FD cohort. More interestingly, non-specific diseases, including screening for suspected conditions, medical examination, or unknown diagnosis, were commonly observed in the FD cohort. In addition, the FD cohort had higher annual costs for 26 of these 27 non-GI-related AHRQ categories, with 20 categories being significantly (P < 0.05) higher. For the FD cohort, intervertebral disc disorders was the most costly ($331 for those with FD vs. only $187 for the controls). Other items that also had statistically significantly higher (P < 0.05) costs per employee for the FD cohort include: non-specific chest pain ($270 for those with FD vs. $75 for the controls), other benign neoplasms ($157 vs. $54), and other connective tissue disease ($141 vs. $71).
Twenty-four of these 27 categories had significantly more annual services (P < 0.05) for the FD cohort. The top categories in the FD cohort included intervertebral disc disorders (3.22 services per employee in the FD cohort vs. 1.83 in the control cohort), non-specific chest pain (1.67 vs. 0.42), and sprains and strains (1.46 vs. 0.67).
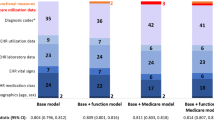
The stepwise logistic regression identified 21 AHRQ specific categories as being associated with significantly high or low odds of being in the FD cohort (Table 5). After controlling for all other AHRQ categories, 19 specific categories were more likely within the FD cohort, and two were less likely within the FD cohort. Esophageal disorders, gastritis and duodenitis, and abdominal pain were most associated with having FD (odds ratios of 3.8, 3.7, and 3.6, respectively). Only hypertension complications/secondary and disorders of the teeth and jaw were significantly negatively associated with FD.
Discussion
This is the first study we know of to present US data on the comorbid conditions of FD, and we found that employees with FD have a higher prevalence of comorbid conditions compared to matched controls: about 6 times higher in digestive diseases, about 2.5 times higher in blood and blood from organ-related diseases, and about 2 times higher in mental disorders or infectious diseases. Moreover, employees with FD had more healthcare services and medical costs than matched controls, due to other comorbid conditions (except pregnancy-related conditions). The team’s prior research on subjects with FD using the same database found that FD employees incurred $5,138 more in annual medical and drug costs and absence payments compared with controls, and FD employees also had greater medical costs for each place of service (all P ≤ 0.0001). Within the FD cohort, healthcare represented 72% and prescription drugs represented 10% of the overall costs. The employees with FD had an additional 0.83 absence days per year and produced 12% fewer units of work per hour than controls (both P ≤ 0.05) [16].
FD is one of the most commonly studied FGIDs, but is heterogeneous and is often under-recognized or misdiagnosed in clinical practice [21]. As stated by the Rome committee, FD is a “diagnosis by exclusion”; thus, to arrive at this diagnosis, at least an upper endoscopic examination is needed in order to exclude other possible conditions. Only one-third of the FD cohort had an endoscopy during the analysis period. While it is possible that subjects may have had a procedure more than 3 months prior to their index date, these data were not available for review.
The MDCs with the highest comorbidities (Table 2) include infections and parasitic diseases. To better understand the infections, we explored the impact of H. pylori within the population. Based on claims, 31 of the 1,669 (1.86%) patients with FD and 64 of 83,450 (0.077%) patients without FD had a diagnosis of H. pylori during the measurement year (P < 0.05).
Moreover, FD has reported overlap with other FGIDs, including IBS, GERD, and other abdominal pain disorders [8, 22, 23]. In a recent systematic review describing the prevalence of IBS in subjects with dyspepsia, Ford et al. [23] identified 19 studies which met their eligibility criteria, comprising 18,173 subjects, and they showed that the prevalence of IBS in subjects with dyspepsia was 37% (95% confidence interval [CI], 30–45%). All included studies in this systemic review were based on questionnaire criteria for IBS and dyspepsia, and they concluded that subjects with dyspepsia have an eightfold increase in prevalence of IBS compared with the population.
The current study confirmed a higher proportion of GI comorbid conditions in FD, including abdominal pain, esophageal disorders, and nausea/vomiting, among employees with FD compared to controls. Most interestingly, we found that employees with FD also had a higher prevalence of upper GI malignancy, notably, esophageal cancer, stomach cancer, and pancreatic cancer, compared to matched controls. However, we cannot conclude that FD leads to upper GI malignancy; rather, dyspepsia could result from malignancy or its treatment [24].
In terms of non-GI comorbid conditions in subjects with FD, existing studies are very limited. Hillilä et al. [25] showed that dyspepsia was more common in subjects with depression. There have been a number of studies of comorbid conditions in IBS summarized in systematic reviews [9, 10]. Specifically, IBS has been shown to have more prevalent psychiatric comorbidities compared to controls. In our study, employees with FD had more prevalent mental comorbid conditions compared to matched controls, including conditions such as dissociative/personality disorder, affective disorders, and other mental conditions. Overall, the present study showed a significantly higher prevalence of almost all of the MDC categories among employees with FD compared to matched controls, while GI diseases were 6 to 14 times higher among employees with FD compared to controls. In the only other investigation comparable to this study evaluating the comorbidity of dyspepsia (but not FD), Wallander et al. [8] reported that sleep disorder, angina, and osteoarthritis/rheumatoid arthritis were associated with dyspepsia (based on the UK General Practice Research Database).
This study observed that respiratory, cardiovascular , and mental disease, as well as GI disease were more common among employees with FD. Moreover, our study showed higher proportions of other comorbid conditions, such as infectious disease, endocrine disease, and even injury and poisoning, compared to matched controls. The logistic regression of all categories identified two significant somatization categories, “Dissociative/personality disorders” (odds ratio = 1.423, with 95% Wald CI from 1.154 to 1.754) and “Affective disorders” (odds ratio = 1.327, CI from 1.056 to 1.668), that were associated with FD.
More interestingly, 18 of the top 30 most prevalent AHRQ “specific” categories were non-specific, with terms like “other” or “undefined” in the title. A number of these categories might support an “exclusionary diagnosis” of FD in that they may reflect excessive testing being done to exclude other diagnoses. As a result, many of these categories might have only been from the pre-index period; however, it is uncertain how long these non-specific issues persisted. Overall, the FD cohort had higher costs in 155 of the AHRQ categories than the control cohort (76 significantly higher) and more medical services in 179 categories than the control cohort (110 significantly increased). The fact that no categories were more costly and only one category had more services among the non-FD cohort than among the FD cohort, while so many differences were significantly greater for the FD cohort, suggests that most of the significant P-values are not spurious results of having performed multiple comparisons. If that had been the case, the number of significant differences would likely be more evenly divided between the two cohorts.
It is likely that prevalent comorbid conditions among employees with FD drive frequent use of healthcare services. The present study’s definition of services counts each procedure code recorded in the medical claims data as a unique service, thus, an office examination and a blood test for an H. pylori examination on the same date would count as two services. The present study showed that employees with FD had about 7 times higher healthcare service use compared to matched controls. Moreover, healthcare services among employees with FD were more frequent in most of the comorbid conditions, including the circulatory system and respiratory disease, mental disease, endocrinological and musculoskeletal disease, and genitourinary disease, versus the matched controls.
While the prevalence analysis focused on the proportion of subjects with each condition, a sub-analysis examined the number of comorbidities within the cohort of patient with FD. While one subject had claims in 60 of the AHRQ specific categories, 20.8% of the cohort had four or fewer specific categories, and 94.7% of the cohort had claims in 20 or fewer categories.
Limitations
The comprehensive analysis of all specific categories may have identified chance associations instead of true relationships. The logistic regression results focused on were from a stepwise selection model, which limits the number of comparisons in the final model. Lastly, while the differences identified in Tables 2, 3, and 4 may be the result of chance findings, they are almost entirely all higher for the FD cohort, which gives more support for the conclusions.
Since the comorbidity cost and utilization data were generally not normally distributed, some bias may exist. Because the annual time period began 3 months prior to the initial diagnosis, it may be unclear if the events are in the pre- or post-diagnosis period. As FD is a diagnosis of exclusion, some of the identified comorbidities (such as esophagitis, peptic ulcer disease, malignancy, etc.) may indicate a serious underlying disease that causes stomach pain/discomfort and should not be labeled as FD. Because the study time frame covers the 3 months before to the 9 months after the diagnosis of FD, it would suggest that these diagnoses occurred in the post-period time frame and the FD diagnosis may be suspect or represent a misdiagnosis. The possibility of a misdiagnosis is prevalent in all claims-based analyses: while the study used the ICD-9 code for FD (536.8x), it was not possible to verify its accuracy. Because the employers did not provide coverage for over-the-counter (OTC) agents, the costs of these products are not included in the study. Finally, the possibility that there is a biological basis for the comorbidity of FD with some disorders (especially GI disorders, including GERD and gastritis) cannot be excluded.
Conclusions
This study showed excess comorbidity among employees with functional dyspepsia (FD) compared to employees without FD. The additional comorbidity is likely to be a major determining factor driving excess healthcare services as well as high healthcare costs associated with FD. Like irritable bowel syndrome (IBS), FD is a heterogeneous disorder, but the condition significantly impacts on quality of life and is associated with very substantial costs [16]. Limited objective data exist on FD comorbidities. Because FD is a diagnosis of exclusion, a better understanding of associated comorbidities may provide insight into the processes resulting in dyspepsia and, ultimately, provide the basis for a more refined diagnosis of FD—as opposed to a diagnosis based on exclusions. These novel data indicate that FD is associated with many comorbidities, similar to IBS. We do not know whether the successful treatment of FD will impact on these comorbidities, but the knowledge that these exist should help promote the development of new, comprehensive, and potentially cost-saving management strategies in the future.
Abbreviations
- FD:
-
Functional dyspepsia
- AHRQ:
-
Agency for Healthcare Research and Quality
- FGIDs:
-
Functional gastrointestinal disorders
- IBS:
-
Irritable bowel syndrome
- HCMS:
-
Human Capital Management Services
- ICD-9:
-
International Classification of Diseases, Ninth Revision
- MDCs:
-
Major diagnostic categories
- CPIs:
-
Consumer price indices
References
Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–1479.
Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–1580.
Jones R, Lydeard S. Prevalence of symptoms of dyspepsia in the community. BMJ. 1989;298:30–32.
Penston JG, Pounder RE. A survey of dyspepsia in Great Britain. Aliment Pharmacol Ther. 1996;10:83–89.
Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ III. Dyspepsia and dyspepsia subgroups: a population-based study. Gastroenterology. 1992;102:1259–1268.
Camilleri M, Dubois D, Coulie B, et al. Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States: results of the US Upper Gastrointestinal Study. Clin Gastroenterol Hepatol. 2005;3:543–552.
Hsu PI, Lai KH, Tseng HH, et al. Eradication of Helicobacter pylori prevents ulcer development in patients with ulcer-like functional dyspepsia. Aliment Pharmacol Ther. 2001;15:195–201.
Wallander MA, Johansson S, Ruigomez A, Garcia Rodriguez LA, Jones R. Dyspepsia in general practice: incidence, risk factors, comorbidity and mortality. Fam Pract. 2007;24:403–411.
Whitehead WE, Palsson OS, Levy RR, Feld AD, Turner M, Von Korff M. Comorbidity in irritable bowel syndrome. Am J Gastroenterol. 2007;102:2767–2776.
Riedl A, Schmidtmann M, Stengel A, et al. Somatic comorbidities of irritable bowel syndrome: a systematic analysis. J Psychosom Res. 2008;64:573–582.
Frankhuisen R, Van Herwaarden MA, Heijkoop R, et al. Functional dyspepsia and irritable bowel syndrome in patients with achalasia and its association with non-cardiac chest pain and a decreased health-related quality of life. Scand J Gastroenterol. 2009;44:687–691.
Choung RS, Locke GR, Schleck CD, Zinsmeister AR, Talley NJ. Do distinct dyspepsia subgroups exist in the community? A population-based study. Am J Gastroenterol. 2007;102:1983–1989.
Talley NJ, Piper DW. The association between non-ulcer dyspepsia and other gastrointestinal disorders. Scand J Gastroenterol. 1985;20:896–900.
Choung RS, Locke GR 3rd, Zinsmeister AR, Schleck CD, Talley NJ. Psychosocial distress and somatic symptoms in community subjects with irritable bowel syndrome: a psychological component is the rule. Am J Gastroenterol. 2009;104:1772–1779.
Ford AC, Forman D, Bailey AG, Cook MB, Axon AT, Moayyedi P. Who consults with dyspepsia? Results from a longitudinal 10-yr follow-up study. Am J Gastroenterol. 2007;102:957–965.
Brook RA, Kleinman NL, Choung RS, Melkonian AK, Smeeding JE, Talley NJ. Functional dyspepsia impacts absenteeism and direct and indirect costs. Clin Gastroenterol Hepatol. 2008;8:498–503.
Rajagopalan K, Kleinman NL, Brook RA, Gardner HH, Brizee TJ, Smeeding JE. Costs of physical and mental comorbidities among employees: a comparison of those with and without bipolar disorder. Curr Med Res Opin. 2006;22:443–452.
Kleinman NL, Brook RA, Rajagopalan K, Gardner HH, Brizee TJ, Smeeding JE. Lost time, absence costs, and reduced productivity output for employees with bipolar disorder. J Occup Environ Med. 2005;47:1117–1124.
Elixhauser A, Steiner C, Palmer L. Clinical classifications software, 2004. February 6, 2004. US Agency for Healthcare Research and Quality. Available at http://www.ahrq.gov/data/hcup/css.htm#download. Accessed November 4, 2004. Also available through HCUP Methods Series: Report #2004-02 Comorbidity Software Documentation, available at http://www.hcup-us.ahrq.gov/reports/methods.jsp. Accessed: November 4, 2004.
Consumer Price Index: All Urban Consumers (Current Series). Bureau of labor statistics, United States Department of Labor, August 2009. Available at http://data.bls.gov/PDQ/outside.jsp?survey=cu, accessed 9/9/09.
Stanghellini V, Frisoni C. Editorial: reflux, dyspepsia, and Rome III (or Rome IV?). Am J Gastroenterol. 2010;105:2632–2634.
Neumann H, Monkemuller K, Kandulski A, Malfertheiner P. Dyspepsia and IBS symptoms in patients with NERD, ERD and Barrett’s esophagus. Dig Dis. 2008;26:243–247.
Ford AC, Marwaha A, Lim A, Moayyedi P. Systematic review and meta-analysis of the prevalence of irritable bowel syndrome in individuals with dyspepsia. Clin Gastroenterol Hepatol 2010;8:401–409. 2009/7/23.
Vakil N, Talley N, van Zanten SV, et al. Cost of detecting malignant lesions by endoscopy in 2741 primary care dyspeptic patients without alarm symptoms. Clin Gastroenterol Hepatol. 2009;7:756–761.
Hillilä MT, Hämäläinen J, Heikkinen ME, Färkkilä MA. Gastrointestinal complaints among subjects with depressive symptoms in the general population. Aliment Pharmacol Ther. 2008;28:648–654.
Acknowledgments
The authors would also like to acknowledge Stephen George, MS, RPh, formerly Vice President, Conexus Health, and Arthur K. Melkonian, MD, formerly of the HCMS Group, now of Promtest LLC, Yerevan, Armenia, for their assistance in the design and conduct of the original research. Dr. Melknonian also assisted in reviewing this manuscript. The original research support for this study was provided by Conexus Health, Tampa, FL. All subsequent analyses were not funded. The study sponsor provided funding and guidance on protocol development and interpretation of the data.
Conflict of interest
The corresponding author had full access to all of the data and takes full responsibility for the veracity of the data and statistical analysis.
The authors disclose the following: Richard Brook, Nathan Kleinman, and James Smeeding received consulting fees from Conexus Health associated with this research in 2004 and 2005. The remaining authors disclose no conflicts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brook, R.A., Kleinman, N.L., Choung, R.S. et al. Excess Comorbidity Prevalence and Cost Associated with Functional Dyspepsia in an Employed Population. Dig Dis Sci 57, 109–118 (2012). https://doi.org/10.1007/s10620-011-1822-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1822-8