Abstract
Background
Obesity is associated with a proinflammatory state.
Aim
To determine whether obesity at diagnosis is a risk factor for Crohn’s disease vs. ulcerative colitis and also vs. community controls and whether there is a U-shaped relationship between body mass index at diagnosis and risk of Crohn’s disease versus ulcerative colitis.
Methods
A total of 524 consecutive inflammatory bowel disease patients attending gastroenterology clinics were administered a questionnaire inquiring about weight at diagnosis and height as well as other risk factors for inflammatory bowel disease. An opportunistic control group of 480 community controls aged 50–70 were randomly selected from the registers of four local general practices as part of another study.
Results
Obesity at diagnosis was more common in subjects with Crohn’s disease versus ulcerative colitis odds ratio 2.02 (1.18–3.43) p = 0.0096 and also Crohn’s disease versus community controls in the 50–70 year age group (odds ratio 3.22 (1.59–6.52) p = 0.001). There was evidence of a ‘dose response’ with increasing degrees of obesity associated with increased risk. Low BMI at diagnosis was also associated with risk of Crohn’s disease versus ulcerative colitis. A U-shaped relationship between BMI and risk of Crohn’s was supported by the strong inverse association of BMI at diagnosis (p = 0.0001) and positive association of BMI at diagnosis squared (p = 0.0002) when they were fitted together into the model.
Conclusions
Obesity may play a role in the pathogenesis of Crohn’s disease and it may be that obesity-related enteropathy is a distinct entity or a sub-type of Crohn’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Obesity is a rapidly increasing problem with a growing number of associated adverse health consequences being discovered. Abdominal adiposity is associated with a pro-inflammatory state [1]. Many pro-inflammatory cytokines are synthesized by adipose tissue, both by adipocytes themselves and also by the macrophages and lymphocytes that infiltrate mesenteric fat particularly in the obese. In epidemiological studies, obesity has been associated with diarrheal symptoms [2] and increased levels of a marker of inflammation, calprotectin, in the feces [3]. In genetically obese mice, increased intestinal permeability has been reported [4], a defect found in Crohn’s disease (CD) and ulcerative colitis (UC).
CD is typically associated with low body weight and younger age at diagnosis than ulcerative colitis [5, 6]. However, CD may be diagnosed at any age and is by no means associated with low body mass index at diagnosis in all subjects. We postulated that obesity is associated with an inflammatory enteropathy affecting the intestine and because of small bowel involvement, is likely to be classified as CD, rather than UC, which only affects the colon.
We performed a case–control study testing the hypothesis that obesity (BMI > 30) at the time of diagnosis is a risk factor for CD as opposed to ulcerative colitis, and that this would mainly manifest in the over-45 age group, where obesity is more common. Our secondary aim was to explore the possibility that the relation of body mass index (BMI) at diagnosis is U-shaped. We also had an opportunistic group of general population controls aged 50–70 drawn from the catchment population of one of the hospitals from which the cases were drawn and were able to test the hypothesis that obesity is a risk factor for CD compared to the general population in the restricted age range of 50–70.
Subjects and Methods
Between 2001 and 2008, 524 consecutive subjects with confirmed inflammatory bowel disease were recruited from the hospital outpatients at Mayday Hospital (462), a district general hospital in outer London, and during the later period of the study from the Inflammatory Bowel Disease clinic at St George’s Hospital (84), a medical school in London, to add to the generalizabilty of the study. All subjects had had (1) one or more symptoms of diarrhea, rectal bleeding, abdominal pain, or fever; (2) occurrence of symptoms on more than one occasion or continuously for at least 6 weeks;(3) objective evidence of inflammation on radiologic, endoscopic, or histological criteria; (4) or had had surgery for Crohn’s disease or ulcerative colitis in the past with or without ongoing evidence of inflammation.
Cases were assigned to CD or UC on the basis of clinical, endoscopic, histopathological, and radiological criteria. Where the diagnosis of CD or UC was unclear, subjects were assigned to UC or CD by a panel of investigators. Subjects with CD were classified according to the Montreal Classification. The site and disease behavior for subjects with CD were recorded but in some cases where surgery took place in the past or terminal ileal intubation was not achieved, it was not possible to determine the exact site.
The subjects were administered a standardized questionnaire by an investigator inquiring the age at diagnosis, smoking, ethnic group, appendectomy, family history of IBD, and height and weight at diagnosis if these were not obtainable from medical records. Body mass index (BMI) was calculated as weight (kg) divided by height squared in meters.
A random sample of 480 subjects aged 50–70 from the registers of four general practices local to Mayday Hospital were recruited for another study on the epidemiology of fecal calprotectin. These subjects aged 50–70 were all Caucasian and were recruited between 2000 and 2005. The methods obtained in their recruitment have been described elsewhere. Briefly, they were selected at random from the registers of four local general practices [7]. A further 160 subjects were recruited to this study after the reported study. There was a 60% response rate. BMI at diagnosis in these subjects equates to BMI at the time they were interviewed. Data was not available in the controls about history of appendectomy, or family history of inflammatory bowel disease.
Statistical Considerations
We performed an initial pilot study of 214 subjects with CD and UC [7]. At that point, we hypothesized that the risk was found only in subjects over the age of 45. We calculated that to detect a 2.25-fold increase in risk associated with obesity in those over 45 would require 500 subjects of all ages with ulcerative colitis and Crohn’s disease with 80% power at a significance level of 0.01. We estimated based on our pilot studies that approximately 35–40% of subjects with inflammatory bowel disease presented after this age.
Univariate comparisons for binary explanatory variables between UC and CD was by Chi-square test, and continuous explanatory variables by t test. The main analysis of obesity as a risk factor for CD versus ulcerative colitis as the main outcome was by logistic regression. Also, CD and UC were analyzed separately versus community controls as the secondary analysis and was performed using logistic regression including only the cases of inflammatory bowel disease with an age at diagnosis between 50 and 70 years.
Sub-normal weight was analyzed additionally as an explanatory factor for risk of CD versus UC to explore a possible U-shaped relationship between BMI at diagnosis and risk of CD. In the final logistic model, both were included as explanatory variables, with BMI 18+ to <30 being the reference category. Evidence for increasing degrees of obesity being associated with increasing risk of CD (dose response) was explored by analyzing by logistic regression BMI split into categories (BMI 18 to <30, 30 to <35, 35 to <40, 40+, excluding BMI < 18) modeled as a continuous rather than a categorical variable. Exploring the U-shaped relationships by breaking continuous variables into categories leads to a loss of statistical power and hence in a separate model BMI at diagnosis as a continuous variable was also modeled including a quadratic term of BMI squared, which is a standard method for exploring U-shaped relationships with continuous variables [8].
Analyses were performed using SPSS version 10. Adjustment was made for age at diagnosis (years), sex, current smoking at time of diagnosis (yes/no), manual occupation (coded as yes/no/missing), ethnic group (coded as Caucasian, south Asian, Afro-Caribbean, and other) and family history of IBD in a first or second-degree relative (yes/no). Data on history of appendectomy was only collected after the start of the study and was missing in 134/524 subjects. It was coded as yes/no/missing. Finally, because the prevalence of obesity has been increasing rapidly over the past two decades, adjustment was made for the year of diagnosis as the number of years prior to 2008 the diagnosis was made.
The association of obesity with disease distribution and behavior was assessed using logistic regression with present/absent/missing as the disease characteristic variables and obesity as the dependent variable.
Ethical approval was granted by London and Surrey Borders ethics committee in 2004 and subjects gave consent to participate.
Results
Table 1 shows the demographic details of the UC and CD subjects in the study. The findings demonstrate the known associations of smoking, younger age at diagnosis, and appendectomy with CD. There was no difference in the height and weight at diagnosis and neither the BMI at diagnosis. There was no difference in the distribution of missing data for appendectomy and manual social class between UC and CD. Conventional risk factors for CD versus UC were all in the expected direction with smoking and appendectomy being more common in CD as was younger age of diagnosis. Obesity at diagnosis was more common in subjects with CD throughout the range of ages at diagnosis but the finding was not statistically significant. According to our original hypothesis that the association of obesity at diagnosis mainly pertained to older subjects aged 45+, we also analyzed this group separately from the data on all subjects presented in the tables. There were 163 subjects diagnosed age 45+, of which 19/63(38%) of subjects with CD and 14/100(14%) of subjects with UC were obese at the time of diagnosis (p = 0.014, Chi-square).
Table 2 shows the characteristics of the subjects in the 50–70 year age group are shown for the two disease groups and the control group. Within this age group, obesity at diagnosis was shown to have a stronger association with CD than the established risk factor of smoking at diagnosis. Manual occupation was more common in subjects with CD than both UC and controls. Only three CD subjects and two UC subjects were non-Caucasian compared to none of the controls.
Table 3 shows the relation of obesity and low body mass index at diagnosis with risk of CD versus UC analyzed by logistic regression. Unadjusted, the association of obesity is not significant, but adjustment for age at diagnosis greatly strengthens the association, with further strengthening of the association after adjustment for low BMI at diagnosis. Low BMI at diagnosis, however, demonstrated attenuation of the association with CD after controlling for age at diagnosis and became non-significant. Adjusting for other risk factors had little effect on the association of obesity with risk of CD. Table 3b demonstrates that there is a dose response of increasing degrees of obesity versus the reference category of subjects with BMI18 to <30. In subjects aged 45 or over, unadjusted the odds ratio for obesity and risk of CD was 2.65(1.22–5.79) p = 0.014. After adjustment for age at diagnosis, sex, and smoking at the time of diagnosis, the odds ratio for increased to 3.18(1.39–7.27), p = 0.0054.
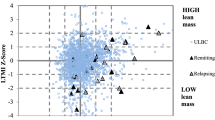
Table 4 shows the effect of modeling BMI at diagnosis as a linear term and as BMI squared to reflect the U-shaped relationship of BMI with risk CD disease versus UC. Neither unadjusted BMI at diagnosis nor BMI squared is significantly associated with risk of CD, but after mutual adjustment there is a strong inverse association of BMI at diagnosis and positive association with BMI squared. This is indicative of a U-shaped relationship between BMI at diagnosis and risk of CD versus UC. These associations are little affected by adjusting for possible confounders.
In the 50–70 age group, similar odds ratios were seen for obesity at diagnosis when the CD group was compared to the control group (Table 5). This was little affected by adjustment for risk factors of social class and year of diagnosis whereas there was no association of obesity at diagnosis and UC compared to the control group.
Further analysis was performed among patients with CD according to disease location: colonic, ileocolonic, or ileal and according to disease behavior: inflammatory, structuring, fistulating, perianal, and history of surgery according to the presence of obesity at diagnosis (Table 6). Only two subjects had primary disease above the ileum with no ileal involvement and they were considered to have ileal disease. No significant differences were found between the association of obesity and disease site, although obese subjects demonstrated a trend towards being less likely to undergo surgery and there was a trend towards obesity being associated with pure ileal disease. No association was found with perianal disease, fistulating disease, or stricturing disease behavior.
Discussion
To the best of our knowledge, this is the first study to establish a positive association between obesity and risk of Crohn’s disease versus ulcerative colitis. Unadjusted, the association was not significant in the whole population, but was so in the 45 year olds and older. After controlling for age at diagnosis, which is lower in CD and associated with lower BMI, the association with CD versus UC was significant. The risk was increased approximately twofold after adjustment when applied throughout the age range. Furthermore, there was a suggestion of a U-shaped relationship between body mass index at diagnosis and risk of CD versus UC, with low BMI at diagnosis also being associated with risk. However, the effect of low body mass index was greatly attenuated and became non-significant after controlling for other risk factors, principally age at diagnosis. Modeling BMI diagnosis together with BMI at diagnosis squared showed the strongest association to support a U-shaped relation of BMI at diagnosis with risk of CD versus UC.
These relations were independent of age of diagnosis, smoking, sex, ethnic group, social class, appendectomy, and family history of IBD. Furthermore, they were also independent of period effects, with adjustment for year of diagnosis having little effect on the association in both the comparison of CD versus UC and versus the community controls. In the case-control comparison of CD subjects aged 50–70 versus community controls, the association of obesity was significant unadjusted, and was little affected by adjustment.
A possible limitation is the potential for selection bias. By recruiting consecutive subjects attending outpatients, we believe that this has been minimized. Subjects with milder disease with a more remote diagnosis may have been under-represented, but as obese subjects were less likely to have undergone surgery (a proxy for more severe disease) we believe that this is unlikely. Additionally, subjects were recruited from two centers and similar results were obtained. Further adding validity to our findings is the observation that recognized risk factors for CD versus UC such as smoking and appendectomy were associated in the expected way, as was younger age at diagnosis.
Another potential source of bias is recall bias. The data on BMI at diagnosis was dependent on recall of body weight at the time of diagnosis in about 25% of the subjects, mainly those diagnosed a longer time ago. There is no obvious reason why subjects with UC should be biased to recalling lower weights than CD subjects. Obesity has been increasing rapidly over the past few decades and hence another potential source of bias would be if the CD patients were diagnosed more recently than the UC patients. This was not the case, and controlling for year at diagnosis had no effect on either the CD vs. UC or CD vs. community control comparisons. To further allay these fears, we compared self-recalled weight at diagnosis with actual weight in a subset of our case population. Among 81 subjects, self-reported weight correlated well with documented weight. Of 39 subjects with UC, recall weight minus actual weight was 1.19 kg (SEM 0.82) heavier versus 0.23 kg (SEM 0.56) heavier for CD indicating, if anything, UC patients recalled a greater weight than CD patients. Furthermore, there was no significant association of time from interviewed to diagnosis for the difference between recalled and actual weight, nor did controlling for length of time since diagnosis weaken our findings.
The case–control comparison was based on a relatively small number of cases owing to the age range of the controls. Nevertheless, we felt it useful to include this comparison to add further validity to the main finding of the association of obesity at diagnosis with CD versus UC. Other concerns about the case–control comparison relate to the comparability of the cases and controls. The cases were drawn from all the general practices in Croydon of some 40 practices together with some patients from a different hospital, whereas the controls were drawn from only four general practices. Subjects with CD had a higher proportion of manual workers, but subjects with UC were similar to the controls, suggesting that the populations were comparable. Adjustment for social class did not attenuate the strength of association of obesity with CD. We were unable to control for family history of inflammatory bowel disease or appendectomy but these had little effect in the main comparison with ulcerative colitis disease controls.
Misclassification between UC and CD is another potential problem, particularly in subjects with colonic CD. When the analysis was restricted to CD subjects without colonic involvement alone compared to subjects with UC, the relationship of obesity at diagnosis was if anything stronger after adjustment for age at diagnosis, sex, and smoking at time of diagnosis (odds ratio 2.43 (1.23–4.80) p = 0.01). Misclassification is therefore unlikely to explain our findings.
Our original hypothesis was that the association would mainly apply at older ages where environmental effects would be expected to be more pronounced. It remained true that this was the case, but also that obesity was a risk factor in younger subjects. Also, originally we hypothesized that the association would relate to maximum ever pre-morbid BMI more strongly than BMI at diagnosis, but reverted to BMI at diagnosis to allow easier replication and to reduce possible bias [7].
Interpretation of the Findings
We believe that despite these possible sources of bias, the association of obesity and risk of CD versus UC is a true one as is the U-shaped relationship of body mass index at diagnosis. Each of the potential sources of bias has been addressed above and the association appears robust despite controlling for multiple confounders. Furthermore, there was evidence of a ‘dose response’ with increasing degrees of obesity being associated with increased risk.
Using disease controls as we did has certain drawbacks in trying to determine etiological significance, in that risk factors common to both CD and UC will not be observed, and the assessment as to whether revealed risk factors are a negative attribute of one condition or positive of the other can be difficult to interpret. In this instance, both forms of inflammatory bowel disease are associated with weight loss at time of diagnosis, so that, if anything, the strength of the true association with obesity was underestimated. The limited comparison we were able to perform against community controls also supports the notion that these findings are of potential etiological significance. The possibility that subjects with UC had an abnormally low BMI at diagnosis and that subjects with CD had a normal BMI seems unlikely in view of the finding that CD was over-represented at both extremes of the distribution of BMI and the limited comparison in the 50–70 year old age group where subjects with CD were more likely to being obese than controls.
These findings appear contrary to the common experience of CD being associated with low body mass index. In our population, subjects with CD were over-represented in both the sub-normal BMI category and the obese category. This could reflect two different types of pathogenic mechanism behind being underweight and overweight at presentation. Being underweight at presentation could be the effect of a more severe form of disease principally but not solely presenting in adolescence and early adulthood with a strong genetic component, whereas obesity could predispose to a less severe from of disease commonly but not exclusively presenting at an older age.
The association of obesity with some cases of CD has biological plausibility. We have previously demonstrated that obesity is associated with elevated levels of fecal calprotectin (a marker of gut inflammation) in a population of healthy 50–70 year olds [3], the first demonstration in humans that obesity could be associated with inflammation at a remote tissue rather than just with circulating levels of inflammatory mediators.
Waist:hip ratio is a better marker of intra-abdominal fat, which is the type of fat associated with the inflammatory phenomena observed in obese subjects [9]. It is possible that had we measured waist:hip ratio the association observed would have been even stronger.
A number of mechanisms could underlie the association of obesity with CD. Mesenteric fat is intimately related to the lesions of CD with fat hypertrophy and fat wrapping observed [9, 15]. Adipose tissue is immunologically and metabolically active. As well as being infiltrated with macrophages and lymphocytes (more so in the obese), preadipocytes can respond to a number of stimuli to produce pro-inflammatory cytokines [10] thus perpetuating inflammation. They can additionally differentiate into macrophages [11]. Adipocytes themselves can also produce a number of pro-inflammatory cytokines and have been demonstrated to express receptors for and synthesise substance p [12], a neuropeptide involved in gut inflammation. Obese subjects have insulin resistance and higher circulating levels of free fatty acids. Circulating free fatty acids are associated with enhanced pro-inflammatory cytokine production by a number of cells including macrophages providing another mechanism for the association [13, 14]. The gut inflammation induced by obesity is more likely to be diagnosed as CD rather than ulcerative colitis because of the propensity of CD to affect the whole gut rather just the colon and the distal colon in particular as in ulcerative colitis.
There was a suggestion of different clinical features in obese subjects with Crohn’s compared to other subjects. Although there was a trend for obese subjects with Crohn’s disease to be less likely to undergo surgery indicating a more benign course, after adjustment for age at diagnosis this lost statistical significance. Likewise, there was a trend for the ileal location to be favored but numbers did not allow any firm conclusions to be drawn. This will need to be the subject of future studies.
Conclusions
Obesity has powerful physiological effects on the body. The effect of obesity on the gut and indeed the gut on obesity have been neglected areas of research. These observations require independent corroboration in other populations and ethnic groups and in prospective studies, but provide a framework for further study with many of the methodological issues having been addressed by this report. The association, if confirmed, merits further study into the role of obesity in disease progression in Crohn’s. It also raises the possibility that obesity-related enteropathy exists, which is a distinct entity from other forms of Crohn’s disease.
References
Mendall MA, Patel P, Asante M, et al. Relation of serum cytokine concentrations to cardiovascular risk factors and coronary heart disease. Heart. 1997;78:273–277.
Delgado-Aros S, Locke GR 3rd, Camilleri M, et al. Obesity is associated with increased risk of gastrointestinal symptoms: A population-based study. Am J Gastroenterol. 2004;99:1801–1806.
Poullis A, Foster R, Shetty A, Fagerhol MK, Mendall MA. Bowel inflammation as measured by fecal calprotectin: A link between lifestyle factors and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev. 2004;13:279–284.
Brun P, Castagliuolo I, Di Leo V, et al. Increased intestinal permeability in obese mice: New evidence in the pathogenesis of nonalcoholic steatohepatitis. Am J Physiol Gastrointest Liver Physiol. 2007;292:G518–G525.
Timmer A. Environmental influences on inflammatory bowel disease manifestations. Lessons from epidemiology. Dig Dis 2003;21:91–104.
Karmiris K, Koutroubakis IE, Kouroumalis EA. The emerging role of adipocytokines as inflammatory mediators in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11:847–855.
John BJPS, Mendall MA, et al.: Relation of obesity to late onset Crohn’s. Gut 2006;55:A74.
May S, Bigelow C. Modeling nonlinear dose-response relationships in epidemiologic studies: Statistical approaches and practical challenges. Dose Response. 2005;3:474–490.
John BJ, Irukulla S, Abulafi AM, Kumar D, Mendall MA. Systematic review: Adipose tissue, obesity and gastrointestinal diseases. Aliment Pharmacol Ther. 2006;23:1511–1523.
Xu H, Barnes GT, Yang Q, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112:1821–1830.
Charriere G, Cousin B, Arnaud E, et al. Preadipocyte conversion to macrophage. Evidence of plasticity. J Biol Chem. 2003;278:9850–9855.
Karagiannides I, Kokkotou E, Tansky M, et al. Induction of colitis causes inflammatory responses in fat depots: Evidence for substance p pathways in human mesenteric preadipocytes. Proc Natl Acad Sci USA. 2006;103:5207–5212.
Suganami T, Nishida J, Ogawa Y. A paracrine loop between adipocytes and macrophages aggravates inflammatory changes: Role of free fatty acids and tumor necrosis factor alpha. Arterioscler Thromb Vasc Biol. 2005;25:2062–2068.
Suganami T, Tanimoto-Koyama K, Nishida J, et al. Role of the toll-like receptor 4/nf-kappab pathway in saturated fatty acid-induced inflammatory changes in the interaction between adipocytes and macrophages. Arterioscler Thromb Vasc Biol. 2007;27:84–91.
Peyrin-Biroulet L, Chamaillard M, Gonzalez F, Beclin E, Decourcelle C, Antunes L, Gay J, Neut C, Colombel JF, Desreumaux P. Mesenteric fat in Crohn’s disease: A pathogenetic hallmark or an innocent bystander? Gut. 2007 Apr;56(4):577–583 (Epub 2006 Sep 6, Review).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mendall, M.A., Viran Gunasekera, A., Joseph John, B. et al. Is Obesity a Risk Factor for Crohn’s Disease?. Dig Dis Sci 56, 837–844 (2011). https://doi.org/10.1007/s10620-010-1541-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1541-6