Abstract
Background
Alpha-fetoprotein (AFP) levels for the diagnosis of hepatocellular carcinoma (HCC) may vary by geographical region and racial background. No data exists for this test in the Middle Eastern population. In addition, there is limited data on the impact of virological status on AFP levels.
Methods
In a multicenter, case-control study involving 206 cases, 199 cirrhotic and 197 chronic hepatitis controls, we assessed the utility of AFP in the diagnosis of HCC (sensitivity, specificity, positive (PPV) and negative (NPV) predictive values, and positive likelihood ratios (LR). PPV and NPV were evaluated for three additional HCC prevalence rates (5, 10, and 20%).
Results
The best discriminating AFP value was 11.7 ng/ml. The sensitivity ranged from 32 to 79.5% at different AFP levels with the specificity increasing sequentially from 47.7 to 98.5%. Sensitivity of AFP at the best cut-off level for hepatitis C virus (HCV), hepatitis B virus (HBV) and non-viral etiology for HCC was 73.7, 65.6, and 59.5%, respectively. Specificity at this level for HCV, HBV, and non-viral etiology was 36.6, 30.1, and 29.4%, respectively. AFP cut-off levels of 102, 200, and 400 ng/ml showed similar sensitivity (39.8, 35.9, and 32%, respectively) and specificity (96, 98.5, and 98.5% respectively). Positive LR for AFP at >11.7, >20, >102, >200, >400 ng/ml were 2.8, 3.3, 9.9, 23.8, and 21.2, respectively.
Conclusions
In cirrhotic patients, AFP has a poor screening and diagnostic value for HCC. Underlying viral etiology fails to influence the diagnostic accuracy of this test. An AFP level greater than 100 ng/ml has a high degree of specificity and may be used as a confirmatory test.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the fourth most common cancer worldwide, and its incidence is increasing worldwide ranging between 3 and 9% annually [1]. Chronic hepatitis B (HBV) and hepatitis C virus (HCV) infections are the most common underlying causes of HCC [2]. The affected patients are usually cirrhotic upon the diagnosis of HCC except in a small percentage of patients with conditions such as HBV infection, hemochromatosis or aflatoxin exposure. Asymptomatic patients diagnosed with HCC through screening programs are more likely to benefit from curative treatment which in turn would be expected to improve survival [3–5].
Most international guidelines advocate twice-yearly liver ultrasonography (US) for HCC screening and serum alpha-fetoprotein (AFP) features strongly as a diagnostic criterion in patients with cirrhosis of all etiologies [6, 7]. Since the initial report almost five decades ago of an elevated AFP level in HCC patients [8], it has been shown that elevated levels of this oncomarker may also occur in a wide variety of non-hepatic malignancies [9, 10] as well as in non-malignant conditions, such as acute and chronic hepatitis [11–14]. The underlying viral etiology may also modulate the diagnostic accuracy of AFP [15, 16]. This varying efficacy may have implications for the test’s utility as a screening tool in different patient groups, particularly in relation to racial background. We are unaware of any study that has examined the diagnostic utility of serum AFP for HCC in Middle Eastern populations and hence, the usefulness of this test in such patients remains unclear.
We aimed to (1) identify basic test characteristics of AFP in Middle Eastern patients with HCC (sensitivity, specificity, positive predictive value (PPV), and negative predictive value [NPV]), (2) determine the best cut-off value of serum AFP to discriminate cirrhotic patients with and without HCC, and (3) to assess whether HBV and HCV infections can modulate the reliability of AFP as a diagnostic tool.
Patients and Methods
We conducted a case-control study of patients with HCC and cirrhosis whose clinical records were available for retrospective reviews at Riyadh Military Hospital (RMH) and King Khalid University Hospital (KKUH). These hospitals serve as referral centers for population groups residing in different geographical regions of Saudi Arabia. Both centers utilize the recently published guidelines for the diagnosis of HCC [17, 18]. The ethical approval for the study was obtained from the Medical Ethics Committee of both centers.
Patients with HCC were identified by screening individual hospitals’ computer-based databases and retrieving the results of all serum AFP performed from January 2006 to March 2008. Subsequently, from this list of patients, we identified all patients who had undergone an abdominal imaging study including US, computed tomography (CT), or magnetic resonance imaging (MRI) within 1 year from the date of the AFP test. We screened these imaging studies for the presence of any focal liver lesion. The medical records of patients found to have a liver lesion were then retrieved and those with HCC identified. We then searched individual hospital-based HCC databases for the period extending from January 2006 to March 2008 and cross-referenced all the HCC cases identified in this manner with those identified through the screening methodology.
In total, 210 treatment-naive, HCC cases were identified in this manner. The diagnosis of HCC was established on the basis of criteria published recently [17] and included the presence of hepatic lesions with typical arterial hypervascularization and washout in the early or delayed venous phase on liver CT and/or MRI. All imaging studies were read by radiologists with extensive expertise in liver radiology. All patients underwent either CT liver and/or MRI. Needle aspiration or histological sampling was obtained only in conditions when non-invasive parameters were not diagnostic. Four patients were labeled as HCC, however they did not fulfill the diagnostic criteria described above, and therefore were excluded from the analysis. We did not utilize serum AFP as one of the diagnostic criteria of HCC for the 206 patients included in the analysis in order to exclude incorporation bias. HCC was therefore diagnosed on the basis of imaging criteria. Thus, a lesion >2 cm, either on CT or MRI, was required to show the typical vascularization pattern that is standard practice in our centers. The median time between AFP and diagnostic imaging study was 50 days (range 1–364 days).
A total of 199 unselected, consecutive, control patients with cirrhosis were identified. Patients with cirrhosis were confirmed either by liver biopsy (n = 118) or by clinical or radiographic factors including four of the following (n = 81): (1) platelet count <100 × 109/l, (2) evidence of esophageal varices on endoscopy, (3) ultrasonographic features consistent with cirrhosis, (4) albumin level less than 30 g/l, (5) international normalized ratio (INR) more than 1.4 and (6) bilirubin level more than 30 μmol/l [19]. HCC was excluded by imaging studies [US, CT, and/or MRI], one of which must have been performed at least 6 months following the measurement of AFP. We included, as a control group, another 197 biopsy-proven, non-cirrhotic chronic hepatitis patients with a serum AFP level available within 6 months of the liver biopsy. All non-cirrhotic controls had a minimum of 6 months of tumor-free follow-up, while cirrhotic controls had a minimum of 12 months of tumor-free follow-up with 6-monthly AFP and US. Additionally, cirrhotic controls with AFP > 20 ng/ml had at least one imaging study with CT and/or MRI. Analyses of various demographic and clinicopathologic characteristics of both HCC cases and cirrhotic controls were performed. The severity of cirrhosis was assessed by Child-Turcotte-Pugh (CTP) scores [20].
Serological and Virological Tests
Laboratory tests including serum AFP, aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma glutamyl transpeptidase (GGT), alkaline phosphatase (ALP), total bilirubin (TB), albumin, platelet count, and INR, HBsAg, and anti-HCV antibody were determined using standard, commercially available assays. AFP was measured by a conventional immunoassay (Elecsys 2010, Roche Diagnostics GmbH, Mannheim, Germany). All AFP measurements in HCC cases were recorded prior to any therapy for HCC, cirrhosis or chronic hepatitis.
Statistical Analysis
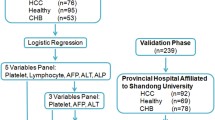
The data was entered into MS Excel and analyzed using SPSS PC+ version 16.0 statistical software and MedCalc software. Descriptive statistics (median, range, and proportions) were used to describe the skewed and qualitative variables. Comparison of non-parametric and categorical data was performed by the Mann–Whitney U test, Kruskal–Wallis test, and Chi-square test, as appropriate. Characteristics of test procedure (sensitivity, specificity, PPV, NPV, likelihood ratios, receiver operating characteristic (ROC) curve, and area under the curve) were used to evaluate the optimal cut-off value for AFP. Since positive and negative predictive values depend on the prevalence of the disease [21], these variables were evaluated considering four HCC prevalences (5, 10, 20, and 50%) [22–26]. Univariate and multivariate (logistic regression) analyses were used in cirrhotic patients and HCC cases to identify independent variables associated with an elevated AFP level. A p value of < 0.05 was considered as statistically significant.
Results
The median age of HCC patients was 66 years (range 24–93 years) and those of cirrhotic controls 58 years (range 13–93 years; p < 0.0001), and non-cirrhotic controls 44 years (range 17–67 years; p < 0.0001). HCC patients were predominantly males (n = 147; 71.3%) compared to the cirrhotic controls (51.3%) and chronic hepatitis (56.3%) (p < 0.0001) (Table 1). HCV was an etiological factor for HCC in 100 (48.5%) while HBV was etiological in 64 (31.1%) and five patients (2.4%) had combined HBV and HCV infections. The remaining 37 (18%) were all diagnosed with cryptogenic cirrhosis except for one patient who was confirmed to have primary hemochromatosis. None of the patients had any significant history of alcohol consumption. Of the 206 HCC patients, 202 were diagnosed based on the noninvasive imaging diagnostic criteria while in four the diagnosis was established by liver biopsy. All HCC cases had features of underlying liver cirrhosis. Eight patients with cirrhosis had serum AFP > 100 ng/ml. All underwent imaging examination; three had both US and CT scans, and five had US, CT, and MRI scans. None of these patients demonstrated any focal hepatic lesions. All eight patients had follow-up imaging studies with CT/MRI (including one with hepatic angiography) over a minimum period of 12 months after the initial diagnostic imaging study, and again, none of these patients showed evidence of hepatic lesions. One patient showed a complete normalization of AFP level, one died (lung malignancy), three were lost to follow-up, and another three continued to have elevated AFP levels in the same range.
Fifty-five HCC patients (26.7%) had unifocal disease at the time of diagnosis and 39 (18.9%) had evidence of vascular invasion. The majority were Child-Pugh class B (106 HCC; 51.5%), followed by Child-Pugh class A (58 HCC; 28.1%), and least Child-Pugh C (42 HCC; 20.4%).
Sensitivity and Specificity of AFP for Diagnosis of HCC at Various Cut-Off Values
Serum AFP was significantly higher in HCC (median 35.4 ng/ml [range 0.5–805,795]) than cirrhotic (median 6.4 ng/ml [range 1–1,105]; p < 0.0001) and non-cirrhotic chronic hepatitis controls (median 3.3 ng/ml [0.6–62.6]; p < 0.0001) (Table 1). Across all patient groups, 312 (51.8%) had serum AFP > 5.8 ng/ml (laboratory upper limit of normal) including 79.5% of HCC cases, 52.3% of cirrhotics and 22.8% of chronic hepatitis controls (p < 0.0001). The distribution of patients for (1) AFP > 10 ng/ml was seen in 69.4, 29.1, and 10.6% across HCC cases, cirrhotic controls and chronic hepatitis controls, respectively (p < 0.0001) (2) AFP > 20 ng/ml was seen in 57.7, 17.3, and 3.5% of HCC cases, cirrhotic controls and chronic hepatitis controls, respectively (p < 0.0001) and (3) for AFP > 200 ng/ml in; and 36.4, 1.7, and 0% of HCC cases, cirrhotic controls and chronic hepatitis controls, respectively (p < 0.0001) (Fig. 1). Sensitivity and specificity for varied AFP cut-off values, when HCC cases were compared with cirrhotic controls, are presented in Table 2.
Figure 2 depicts the ROC curve analysis of AFP in the population including HCC cases and cirrhotic controls. The AFP threshold for the best compromise sensitivity specificity was 11.7 ng/ml, (AUROC, 0.748; p = 0.0001; 95% CI: 0.703–0.790) and this was used for the analyses in patient subgroups. At this point, the sensitivity was 68.4% and specificity 75.4%.
Predictive Values for HCC at Various AFP Intervals
We calculated the PPV and NPV of various AFP levels obtained at estimated HCC prevalences of 5, 10, 20, and 50% (Table 3). For a cut-off value of 11.7 ng/ml, the decline in HCC frequency caused the PPV to decrease to 12.7% at the lowest prevalence of 5%. Similarly, at a level of 20 ng/ml, the level at which more intensive investigations are undertaken, AFP showed a PPV of 77.6% and NPV of 65.2% at study highest prevalence of 50%. The PPV at this level reduced progressively to reach 14.3% with an increase in the NPV to 97.3% at the lowest prevalence of 5%. The best PPV at the lowest HCC prevalence was observed upon using a 200-ng/ml cut-off level, which provided a correct allocation to over half the cases. Increasing the AFP cut-off level to 400 ng/ml did not improve the diagnostic accuracy of the test (Table 2). The positive likelihood ratios (LR) of various AFP cut-off levels are presented in Table 2, showing the highest LR of 23.8 at an AFP level > 200 ng/ml.
Correlation Between Serum AFP and Other Parameters
Serum AFP > 11.7 ng/ml was observed in 142 (68.9%) HCC cases, 49 (24.6%) cirrhotics, and 15 (7.6%) of chronic hepatitis controls (p < 0.0001). No significant correlation was found between serum AFP levels (above or below 11.7 ng/ml) and age, sex, and tumor number; or various laboratory parameters (platelet count, bilirubin, albumin, INR, ALT, and ALP), except for serum AST (p = 0.001), and GGT (p = 0.02). The Child-Pugh class did not affect the probability of having an elevated AFP (class A: 25.5%; class B: 51.1%; class C: 23.4%; p = 0.14).
There was a trend towards higher AFP levels in HCC patients with HCV etiology, and to a lesser extent HBV infection, when compared with non-viral etiology. Of the 100 patients with HCV-related HCC, 74% exhibited a higher AFP level compared to 26% with AFP < 11.7 ng/ml. In this group, the sensitivity was 73.7% (95% CI: 67.2–79.9) and the specificity was 36.6% (95% CI: 30.3–42.7) for HCC for AFP > 11.7 ng/ml (Table 4). Similarly, of the 64 patients with HBV-related HCC, 42 showed a high AFP with the sensitivity for HCC being 65.6% and specificity of 30.1%. There was no significant difference in the sensitivity of higher AFP (>11.7 ng/ml) for the diagnosis of HCC in HCV and HBV-related HCC (p = 0.492). Lastly, 22 HCC patients of non-viral etiology showed an AFP > 11.7 ng/ml, exhibiting a sensitivity of 59.5% and specificity of 29.4%. There was no significant difference between HCV and non-viral etiology-related HCC patients with an AFP level > 11.7 ng/ml (p = 0.219), or for HBV versus non-viral etiology-related HCC (p = 0.586). Similarly, there was no significant difference in the specificity of higher AFP cut-offs in the diagnosis of HCC for HCV versus HBV, HCV versus non-viral etiology, and HBV versus non-viral etiology (p = NS, for all comparisons). However, HCV patients with AFP level > 11.7 ng/ml demonstrated a higher PPV (53.3%) at the cost of a marginally lower NPV (58.7%) compared to those with HBV and non-viral etiology (30.7, 65.1, and 16.1, 76.2%, respectively).
Predictors of Elevated AFP Level
Univariate and multivariate logistic regression analyses were performed for the HCC cases and cirrhotic controls to examine age ≥50 years, sex, Child-Pugh class, portal vein thrombosis, virologic status, serum albumin, bilirubin, ALT, GGT, AST, INR, ALP, and platelet count as potential independent predictors of elevated AFP level (>11.7 ng/ml) (Table 5). Univariate analysis revealed that age ≥ 50 years (p = 0.02), male gender (p = 0.04), presence of portal vein thrombosis (p = 0.003), presence of either HCV or HBV (p = 0.005), elevated ALT (p = 0.0004), AST (p < 0.0001), GGT (p = 0.01), ALP (p = 0.02), and a lower albumin (p = 0.002), were significant predictors of an elevated AFP level. On multivariate analysis, the presence of portal vein thrombosis (p = 0.006), presence of either HCV or HBV (p = 0.005), AST (p = 0.001), GGT (p = 0.01), and albumin (p = 0.025) were independent predictors of AFP elevation (Table 5).
Discussion
The utility of AFP as a screening and diagnostic test for HCC has been seriously questioned recently. Many studies have shown that the diagnostic characteristics of this test do not support its routine use. In our study, the diagnostic accuracy of AFP was 75%, and the best cut-off value to identify HCC superimposed on cirrhotics was 11.7 ng/ml. Earlier studies from North America and Europe have identified 20–30 ng/ml as the best cut-off limit above which investigations for HCC are needed [26–28], which differs from our lower cut-off value, perhaps as a reflection of the difference in patient population. A study on a Southeast Asian population showed that an AFP level of 200 ng/ml served as the best cut-off value for diagnosing HCC [29]. This study, however, included a very small number of patients (20 HCC cases), which may limit the significance of its findings.
The relationship of ethnicity to the level of AFP elevation in HCC patients has been previously studied. In a Caucasian population, 38% of HCC cases did not exhibit elevated AFP levels [26], while 43% of African-Americans, and 18% of a mixed group of Asians, Hispanics, and Caucasians showed normal AFP levels in HCV-related HCC patients [27]. Another study on Asian patients revealed that 16% of HCV-related HCC patients had normal AFP levels [30]. In our cohort of Middle Eastern patients, 20% of HCC patients had a normal serum AFP level, with the number increasing to 32% at the ROC identified cut-off level. It becomes apparent therefore that different ethnic groups have a diversely different secretory profile for AFP, possibly influenced by a combination of environmental and biological factors.
In this case-control study, the sensitivity, specificity, and PPV of the identified cut-off level were of modest value, but at a realistic HCC prevalence rate of 5%, the NPV for elevated AFP levels (laboratory cut-off level [>5.8 ng/ml] or ROC determined cut-off level [>11.7 ng/ml]) reached 98%. While a previous study by Trevisani et al. [26] reported a similar NPV, an elevated AFP level had a sensitivity of 60% in correctly identifying HCC cases. In our population, an elevated AFP > 5.8 ng/ml correctly identified 80% of the HCC cases albeit, at a dismally poor PPV of 7.4% with a marginally better performance at 12.8% for ROC determined cut-off levels. Therefore, our findings suggest that in a clinical setting of at-risk population of cirrhotics being screened for HCC, the best PPV (53.8%) would be achieved in those with AFP levels > 200 ng/ml.
Similar to findings in Caucasian populations [26–28], the specificity of an AFP level > 200 ng/ml in our study was greater than 98% for HCC cases, although the sensitivity at this cut-off level in our population was higher (36 vs. 22%) [26]. In a North American study including a mixed ethnic group of Caucasians, African-Americans, Asians, and Hispanics, the sensitivity of AFP > 200 ng/ml for identifying HCC approached 32%, with a lower sensitivity in the African-American group compared to the non-African-American group [27].
The utility of serum AFP in HCV-related HCC has been studied previously in a systematic review of five studies [31]. Sensitivity of AFP levels >20 ng/ml ranged from 41 to 73%, while specificity ranged from 60 to 94%. Additionally, HCV-related HCC demonstrated a higher sensitivity and specificity over non-HCV related HCC. In our study, HCV-infected patients demonstrated a higher sensitivity and specificity, and a lower NPV over HBV and non-viral etiology-related HCC, although this did not reach statistical significance. However, HCV-infected patients exhibited a higher PPV compared to HBV and non-viral etiology-related HCC (p < 0.05) thereby suggesting that AFP perhaps may have its best utility in HCV-infected individuals compared to others. These findings should be further evaluated in larger studies designed specifically to address this issue. Finally, HCC attributed to non-viral etiology showed the lowest sensitivity (60%), specificity (29%), and PPV (16%) compared to those with HCV- and HBV-infected groups. This is in contrast to the findings of two Italian studies that showed a specificity of 100% and a PPV of 94% for elevated AFP levels in HCC related to non-viral etiology [26, 28]. These findings could be explained in part by the possible differing backgrounds of non-virus related HCC in the two population groups. In Western populations, the majority of non-viral HCC were related to alcoholic liver disease which, however, did not serve as an etiological factor in our patients.
The findings in our population confirm previous reports that in the presence of a normal AFP at prevalence rates encountered in clinical settings, almost all patients (98%) will not have HCC. However, the advantage of such a high NPV is offset by findings that, at this prevalence rate, AFP levels are extremely poor in predicting the true presence of HCC (<13%). This means that almost 87% of cirrhotic patients with an abnormal AFP will undergo unnecessary intensive investigations contributing to huge overall expense on the healthcare system. These findings must also be taken in the context of our findings that up to 32% of our HCC cases have normal AFP levels; and when considering the AFP trigger level of 20 ng/ml for more incursive testing as recommended in international guidelines, then this false-negative rate increased to 43%. This means that when AFP is used alone as a screening test, HCC would not be detected in 43% of the cases. Similarly, previous studies have shown that when using this trigger level of 20 ng/ml, 37–46% of HCC would escape detection [26, 27, 32].
Such high false-negative rates are unacceptable for a screening or diagnostic test. Previous studies performed in Western populations have reported similar findings [26–28] and our findings add to the growing body of evidence against the utilization of AFP in such settings. As previously suggested [33], the best utilization of this test remains in the clinical setting where a lesion has been detected on imaging modalities and elevated levels of AFP can be used as a confirmatory test. Trevisani et al. [26] found that an AFP level of 100 ng/ml had a specificity of 99% in the diagnosis of HCC. In our population, this rate of specificity was achieved with a level of 200 ng/ml, although the specificity reached with 102 ng/ml was not much different at 97%. This suggests that a level of about 100 ng/ml may be used as a confirmatory test for HCC in the appropriate setting.
International [7] and regional guidelines [18] continue to use AFP levels of > 400 ng/ml cut-off level as a criterion for the diagnosis of HCC, while others have reduced this cut-off level to 200 ng/ml [17]. In our study, we have shown that an AFP level of 200 ng/ml is a more suitable cut-off level with an equivalent sensitivity, specificity, PPV, NPV and positive LR when compared to 400 ng/ml. In addition, an AFP level of 102 ng/ml also demonstrated a comparable sensitivity, specificity and NPV although, at the expense of the PPV. This cut-off level of AFP should be further evaluated in larger prospective screening trials in order to validate these observations.
As previously reported, HCC patients are generally older and predominantly male [27, 30]. Similarly, in our study, there were significant differences in the demographic characteristics between the HCC cases and cirrhotic controls. A greater age and male predominance was evident in HCC patients. While we realize the limitation imposed by the lack of age- and gender-matched controls, we believe this was unavoidable as doing it differently would have introduced a selection bias. Likewise, HCC is a complication of cirrhosis and it would be expected that these patients would have more advanced biochemical disturbances compared to cirrhotic and chronic hepatitis patients as reflected in our study. Moreover, when we performed logistic regression analysis in HCC cases and cirrhotic controls to identify independent predictors of elevated AFP, age and male gender did not feature as independent predictors of elevated AFP levels, thereby suggesting that the lack of age- and gender-matched controls did not confound the diagnostic value of serum AFP levels.
In conclusion, our study shows that in Middle Eastern patients with cirrhosis, an AFP cut-off level of 11.7 ng/ml yields the best sensitivity and specificity for the diagnosis of HCC, but even at this best cut-off value, AFP is a poor diagnostic and screening test for HCC. These findings are not modulated by the etiology of underlying liver cirrhosis. Finally, our study also demonstrated that an AFP level of 102 ng/ml achieves a high degree of specificity and may be considered as an appropriate cut-off for HCC confirmation.
References
Velazquez RE, Rodriguez M, Navascues CA, et al. Prospective analysis of risk factors for hepatocellular carcinoma in patients with liver cirrhosis. Hepatology. 2003;37:520–527.
Szilagyi A, Alpert L. Clinical and histopathological variation in hepatocellular carcinoma. Am J Gastroenterol. 1995;90:15–23.
Yuen MF, Cheng CC, Lauder IJ, Lam SK, Ooi CG, Lai CL. Early detection of hepatocellular carcinoma increases the chance of treatment: Hong Kong experience. Hepatology. 2000;31:330–335.
McMahon BJ, Bulkow L, Harpster A, et al. Screening for hepatocellular carcinoma in Alaska natives infected with chronic hepatitis B: a 16-year population-based study. Hepatology. 2000;32:842–846.
Wong LL, Whitney ML, Severino P, Wong LM. Improved survival with screening for hepatocellular carcinoma. Liver Transpl. 2000;6:320–325.
Colombo M. Early diagnosis of hepatocellular carcinoma in Italy. A summary of a Consensus Development Conference held in Milan, 16 November 1990, by the Italian Association for the Study of the Liver (AISF). J Hepatol. 1992;14:401–403.
Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL Conference. J Hepatol. 2001;35:421–430.
Bergstrand CG, Czar B. Demonstration of a new protein fraction in serum from the human fetus. Scand J Clin Lab Invest. 1956;8:174.
Masopust J, Kithier K, Radl J, Koutecky J, Kotal L. Occurrence of fetoprotein in patients with neoplasms and nonneoplastic diseases. Int J Cancer. 1968;3:364–373.
Javadpour N. The role of biologic tumour markers in testicular cancer. Cancer. 1980;45:1755–1761.
Liaw YF, Tai DI, Chen TJ, Chu CM, Huang MJ. Alpha-fetoprotein changes in the course of chronic hepatitis: relation to bridging hepatic necrosis and hepatocellular carcinoma. Liver. 1986;6:133–137.
Bloomer JR, Waldmann TA, McIntire KR, Klatskin G. Alpha-fetoprotein in non-neoplastic hepatic disorders. JAMA. 1975;233:38–41.
Silver HKB, Deneault J, Gold P, Thompson WG, Shuster J, Freedman SO. The detection of α-fetoprotein in patients with viral hepatitis. Cancer Res. 1974;34:244–247.
Bayati N, Silverman AL, Gordon S. Serum alpha-fetoprotein levels and liver histology in patients with chronic hepatitis C. Am J Gastroenterol. 1998;93:2452–2456.
Tsai JF, Chang WY, Jeng JE, Ho MS, Lin ZY, Tsai JH. Frequency of raised a-fetoprotein level among Chinese patients with hepatocellular carcinoma related to hepatitis B and C. Br J Cancer. 1994;69:1157–1159.
Stroffolini T, Andreone P, Andriulli A, et al. Characteristics of hepatocellular carcinoma in Italy. J Hepatol. 1998;29:944–952.
Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208–1236.
Abdo AA, Karim HA, Al Fuhaid T, et al. Saudi Gastroenterology Association guidelines for the diagnosis and management of hepatocellular carcinoma: summary of recommendations. Ann Saudi Med. 2006;26(4):261–265.
Abdo AA, Al-Jarallah BM, Sanai FM, et al. Hepatitis B genotypes: relation to clinical outcome in patients with chronic hepatitis B in Saudi Arabia. World J Gastroenterol. 2006;12(43):7019–7024.
Child CG III, Turcotte JG. Surgery in portal hypertension. In: Child CG III, ed. The liver and portal hypertension. Philadelphia: W.B. Saunders; 1964:50.
Komaroff AL, Berwick DM. Decision theory and medical practice. In: Isselbacher KJ, Adams RD, Braunwald E, Pedersdorf RG, Wilson JD, eds. Principles of internal medicine. Update IV. New York: McGraw-Hill; 1983:243–254.
Colombo M, De Franchis R, Del Ninno E, et al. Hepatocellular carcinoma in Italian patients with cirrhosis. N Engl J Med. 1991;325:675–680.
Zoli M, Malagotti D, Bianchi G, Gueli C, Marchesini G, Pisi E. Efficacy of surveillance program for early detection of hepatocellular carcinoma. Cancer. 1996;78:977–985.
Imberti D, Fornari F, Sbolli G, Buscarini E, Squassante L, Buscarini L. Hepatocellular carcinoma in liver cirrhosis. A prospective study. Scand J Gastroenterol. 1993;28:540–544.
Curley SA, Izzo F, Gallipoli A, de Bellis M, Cremona F, Parisi V. Identification and screening of 416 patients with chronic hepatitis at high risk to develop hepatocellular carcinoma. Ann Surg. 1995;222:375–383.
Trevisani F, D’Intino PE, Morselli-Labate AM, et al. Serum α-fetoprotein for diagnosis of hepatocellular in patients with chronic liver disease: Influence of HBsAg and anti-HCV status. J Hepatol. 2001;34:570–575.
Nguyen MH, Garcia RT, Simpson PW, Wright TL, Keeffe EB. Racial differences in effectiveness of α-fetoprotein for diagnosis of hepatocellular carcinoma in hepatitis C virus cirrhosis. Hepatology. 2002;36:410–417.
Soresi M, Magliarisi C, Campagna P, et al. Usefulness of alpha-fetoprotein in the diagnosis of hepatocellular carcinoma. Anticancer Res. 2003;23:1747–1753.
Taketa K, Okada S, Win N, Hlaing NK, Wind KM. Evaluation of tumor markers for the detection of hepatocellular carcinoma in Yangon General Hospital, Myanmar. Acta Med Okayama. 2002;56:317–320.
Kim KA, Lee JS, Jung ES, et al. Usefulness of serum alpha-fetoprotein (AFP) as a marker for hepatocellular carcinoma (HCC) in hepatitis C virus related cirrhosis: analysis of the factors influencing AFP elevation without HCC development. Korean J Gastroenterol. 2006;48(5):321–326.
Gupta S, Bent S, Kohlwes J. Test characteristics of alphafetoprotein for detecting hepatocellular carcinoma in patients with hepatitis C. A systematic review and critical analysis. Ann Intern Med. 2003;139:46–50.
Farinati F, Marino D, De Giorgio M, et al. Diagnostic and prognostic role of alpha-fetoprotein in hepatocellular carcinoma: both or neither? Am J Gastroenterol. 2006;101(3):524–532.
Sherman M. Alphafetoprotein: an obituary. J Hepatol. 2001;34:603–605.
Conflict of interest
No conflicts of interest exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanai, F.M., Sobki, S., Bzeizi, K.I. et al. Assessment of Alpha-Fetoprotein in the Diagnosis of Hepatocellular Carcinoma in Middle Eastern Patients. Dig Dis Sci 55, 3568–3575 (2010). https://doi.org/10.1007/s10620-010-1201-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1201-x