Abstract
Background
The degree of intratumoral microvascular density is thought to affect tumor metastasis and prognosis in various human cancers, including gastric cancer. Despite recent medical advancements, gastric adenoma or adenocarcinoma remains a considerable therapeutic challenge. Endoscopic submucosal dissection (ESD) is a more recent approach that is now commonly used for radical resection of gastric adenoma and adenocarcinoma.
Aim and Methods
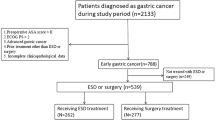
The expression of vascular endothelial growth factor (VEGF), epidermal growth factor receptor (EGFR), and interleukin-6 (IL-6) are related to the prognosis of gastric adenocarcinoma. However, the expression of these factors in gastric adenoma/adenocarcinoma following ESD has not been clearly evaluated. Here, we report on our study of the expression of VEGF, EGFR, and IL-6 by immunohistochemical staining in extracted tissue from adenoma or adenocarcinoma of the stomach by ESD and subsequent evaluation of the correlation of VEGF, EGFR, and IL-6 with other clinicopathological parameters. The patient cohort consisted of 102 patients with adenoma or adenocarcinoma of the stomach.
Results
Immunohistochemical staining for VEGF and IL-6 was significantly higher in both high grade dysplasia and adenocarcinoma than in low grade dysplasia (P < 0.05). There was significant correlation between histological grade and intensity of immunohistochemical staining of VEGF (P = 0.039). Histological differentiation of adenocarcinoma was related to IL-6 expression (P = 0.028). The immunoreactivity of VEGF and IL-6 increased significantly in lesions >2 cm compared to lesions <2 cm (P < 0.05).
Conclusion
The immunohistochemical expression of IL-6 and VEGF can be considered to be useful for clinical diagnosis and follow-up of adenoma or adenocarcinoma of the stomach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is now well known that tumor growth, invasion, and metastasis are dependent on angiogenesis, which is defined as the process of new vessel formation from preexisting vessels [1]. An advanced stage, hematogenous spread, lymph node metastasis, and peritoneal dissemination of gastric carcinoma have been reported to exist more frequently in patients with highly vascularized tumors than in those having tumors with a low vascular density [2]. Vascular endothelial growth factor (VEGF) is one of the most potent angiogenic factors, stimulating endothelial cell proliferation, preventing the regression of newly formed vessels, and increasing microvascular permeability [3, 4]. A number of studies have demonstrated that tumor VEGF expression predicts an increased risk of metastatic diseases and poor survival in patients with gastric cancer [5], esophageal cancer [6], breast cancer [7], ovarian cancer [8], and non-small cell lung cancer [9]. A recent study has revealed a relationship between the increased expression of VEGF and tumor growth, distant metastasis, and a poor prognosis of patients with gastric carcinoma [10]. Experimentally, hypoxia and ischemia are known to induce angiogenesis in various cultured tumor cells by increasing VEGF expression [11]. Epidermal growth factor receptor (EGFR) is a cell-membrane tyrosine kinase receptor belonging to the ErbB family. When activated, EGFR initiates a complex intracellular signal transduction cascade that promotes cancer cell division, migration, apoptosis inhibition, and angiogenesis through the upregulation of VEGF [12]. The expression of EGFR has been extensively studied in patients with gastric cancer with greatly varying results, probably due to the different methods and cut-off values used for defining expression [13, 14]. Interleukin-6 (IL-6) expression is elevated in tissues undergoing active angiogenesis, but it does not directly induce the proliferation of endothelial cells. A significant correlation between IL-6 and VEGF has been reported in a variety of advanced cancers [15]. Recent reports have indicated that the expression of VEGF, EGFR, and serum interleukin-6 (IL-6) are related to the prognosis of gastric adenocarcinoma [5, 15–17]. However, the expression of VEGF, EGFR, and IL-6 in gastric adenomas following removal by endoscopic submucosal dissection (ESD) has not been clearly evaluated. We report here our study of VEGF, EGFR, and IL-6 expression in gastric adenomas and adenocarcinomas by immunohistochemistry after ESD. We also analyzed the relationship between VEGF, EGFR, and IL-6 expression in tissue and the clinicopathological parameters of gastric adenomas and adenocarcinomas.
Materials and Methods
Clinicopathological Materials
The cohort consisted of 102 patients who underwent ESD for gastric adenoma or adenocarcinoma from June 2004 to February 2007 at the Dong-A University Hospital, Busan, Korea.
Written informed consent prior to the procedure was obtained from all patients. Follow-up data on all 102 patient-cases were obtained from the tumor registries and clinical records. Two gastrointestinal pathologists evaluated the ESD specimens, paying special attention to tumor differentiation and depth of invasion.
Immunohistochemistry
The immunostaining was performed using a tissue microarray and automated immunohistochemistry system of Ventana Medical Systems (Tucson, AZ). One 3-mm-diameter core of a formalin-fixed, paraffin-embedded tissue block was removed from each case and put in a new recipient paraffin block for the tissue microarray. All processes of immunohistochemistry were performed automatically using a Ventana autostainer (Benchmark; Ventana Medical Systems). Vascular endothelial growth factor (rabbit polyclonal antibody, 1:200; Santa Cruz Biotechnology), EGFR (mouse monoclonal antibody, 1:1; Zymed Laboratories, San Francisco, CA) and IL-6 (rabbit polyclonal antibody, 1:1000; Abcam, San Francisco, CA) were used as primary antibodies.
Immunostaining for VEGF and IL-6 was considered to be positive if >30% of the tumor cells showed granular cytoplasmic immunostaining. For EGFR, immunostaining was considered to be positive if >10% of the tumor cells showed membranous immunostaining.
Statistical Analysis
Data were analyzed by the chi-square test or the Fisher exact test using SPSS version 14.0 (SPSS, Chicago, IL) to evaluate the relation of VEGF, EGFR, and IL-6 expression to histological grade and other parameters. P values <0.05 were considered to be statistically significant.
Results
Clinicopathological Features
The male-to-female ratio of the 102 patients with gastric adenoma or adenocarcinoma was 2.3 to 1. The mean age of the patients was 62.3 years (range 35–82 years). Histologically, 61 adenomas consisted of 20 tumors with low grade dysplasia (LGD) and 41 with high grade dysplasia (HGD). The 41 adenocarcinomas consisted of 18 well-differentiated, 17 moderately differentiated, and six poorly differentiated adenocarcinomas. The relationship between histological grade and clinical features is summarized in Table 1. Tumor size was measured as the size of the total resected specimen by ESD. Adenocarcinoma was significantly larger than adenoma (P = 0.013).
Relation Between VEGF, EGFR, and IL-6 Immunohistochemistry and Histological Grade
Immunohistochemistry of VEGF
Eighty-seven adenomas and adenocarcinomas (85.3%) showed immunoreactivity for VEGF, with that for VEGF being significantly greater in HGD and adenocarcinoma than in LGD (P = 0.029) (Table 2). We found a correlative relation between the immunoreactivity of VEGF and histological grading (LGD, HGD, adenocarcinoma). However, the histological differentiation (well differentiated, moderately differentiated, poorly differentiated) of adenocarcinoma was not related with VEGF expression. None of the normal or regenerating epithelium as well as stroma were immunoreactive for VEGF.
Correlation Between Histological Grade and Intensity of VEGF Expression
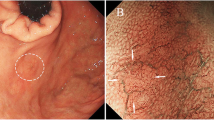
The intensity of immunohistochemistry was classified into three degrees: negative, weakly positive, and strongly positive staining. Histological grade (LGD, HGD, adenocarcinoma) was significantly related to the intensity of immunohistochemistry for VEGF (P = 0.039) (Table 3, Fig. 1d). There was no significant relation between the differentiation of the gastric adenocarcinoma (well-differentiated adenocarcinoma, moderately differentiated adenocarcinoma, and poorly differentiated adenocarcinoma) and the intensity of immunohistochemistry for VEGF (P = 0.666).
Immunohistochemistry of EGFR
None of the adenomas as well as normal or regenerating epithelium were immunoreactive for EGFR (Fig. 2b). Only three adenocarcinomas (2.9%) of all 102 cases showed immunoreactivity for EGFR, and all of these cases were focal (<5%) and weakly positive. One case was well differentiated and two cases were moderately differentiated cancer (Fig. 3d).
Immunohistochemistry of IL-6
Twenty-two (21.6%) of all 102 patient-cases showed immunoreactivity for IL-6. All of the 20 LGD were negative, five (12.2%) of the 41 HGD, and 17 (41.5%) of the 41 adenocarcinomas were positive. The immunoreactivity of IL-6 was significantly increased in HGD and adenocarcinoma compared to LGD (P = 0.001) (Table 2). Based on cancer subtype, four (22.2%) of 18 cases of well-differentiated cancer and 13 (56.5%) of 23 cases of moderately and poorly differentiated cancer showed immunoreactivity for IL-6 (P = 0.028) (Table 4). The positive rate of immunoreactivity of IL-6 was significantly increased in moderately and poorly differentiated adenocarcinoma relative to well-differentiated adenocarcinoma. The histological differentiation of adenocarcinoma was related to IL-6 expression. Stromal tissue surrounding the epithelium was diffusely immunoreactive for IL-6, with the stroma surrounding the adenocarcinoma being especially more intensely positive than that of stroma surrounding the normal epithelium or adenoma. None of the normal epithelium was positive. All immunohistochemically positive cases for IL-6 showed patterns of granular cytoplasmic immunostaining (Fig. 3c).
Correlation Between Clinicopathological Parameters and VEGF, EGFR, and IL-6 Immunoreactivity
The immunoreactivity of VEGF, EGFR, and IL-6 was compared with other clinicopathological parameters. The correlation between the size of the lesion and positive expression of VEGF was meaningful. The positive expression of VEGF in lesions >2 cm (77.0%) increased significantly compared to that in lesions <2 cm (23.0%) (P = 0.019). In HGD, the positive expression of VEGF in lesions >2 cm (33.3%) increased significantly compared with lesions <2 cm (11.5%) (P = 0.047). In adenocarcinoma, the positive expression of VEGF in lesions >2 cm (34.5%) increased significantly compared with that in lesions <2 cm (4.6%) (P = 0.029) (Table 5).
There was a meaningful correlation between the size of the lesion and the positive expression rate of IL-6. The positive rate of IL-6 in lesions >2 cm was 95.5% compared to 4.5% for lesions <2 cm (P = 0.011). In tumors with HGD, lesions >2 cm had a 22.7% positive expression rate for IL-6 compared to 0.0% in lesions <2 cm (P = 0.024). In adenocarcinoma, lesions >2 cm had a positive IL-6 expression rate of 72.7% compared to 4.5% in lesions <2 cm (P = 0.032) (Table 5).
There was no correlation between immunoreactivity and other parameters, such as sex, age, and lesion site.
Clinical Features and Immunoreactivity in Poorly Differentiated Adenocarcinoma
We analyzed the clinical features and immunoreactivity of poorly differentiated adenocarcinoma following ESD (Table 6). All of the tumors were >2 cm and showed positive immunoreactivity for VEGF. In addition, four of all six poorly differentiated adenocarcinomas were positive for IL-6.
Discussion
Although the incidence is declining, gastric cancer continues to be a major worldwide cause of morbidity and cancer-related deaths [18]. Thus, controversy still exists on the optimal management of gastric cancer. It has recently been suggested that molecular-based approaches may be critical for predicting clinical outcome and guiding treatment strategies in gastric adenoma and adenocarcinoma. As such, determination of VEGF, EGFR, and IL-6 expression could be crucial for two reasons: first, for an assessment of prognosis; secondly, for the identification of patients who could be treated with targeted therapies.
Fibroblast VEGF has recently been identified as a mitogen for endothelial cells in vitro, and it is thought to be a major tumor angiogenesis regulator. The VEGF superfamily of endothelial growth factors seems to play a crucial role in the proliferation and migration of endothelial cells, providing nourishment to growing tumors and enabling the tumor cell to establish continuity with the host vasculature. In many cancers, tumor VEGF expression has been found to be a significant marker for tumor recurrence or reduced survival independent of conventional clinicopathological variables.
Angiogenesis and several proinflammatory cytokines (such as VEGF and IL-6) are also thought to be involved in the development of gastric cancer [19–21].
In our study, histological grade and intensity of immunohistochemistry staining for VEGF had a meaningful correlation. Immunostaining for VEGF was present in a significantly greater percentage of tumors with HGD and adenocarcinoma than in those with LGD. These observations suggest that VEGF may be a final common pathway for other angiogenesis factors.
The role of EGFR in gastric cancer is very controversial. A number of authors have reported that EGFR is highly expressed in gastric cancer, suggesting its suitability as a target for receptor tyrosine kinase inhibitors [22]. Conversely, Takehana et al. [23] reported that overexpression of EGFR is a rare event in gastric carcinoma and occurs predominantly due to EGFR gene amplification.
In our investigation, only three of the 102 patients were positive for EGFR after immunohistochemical staining. These three cases were well or moderately differentiated cancer. The percentage of EGFR expression in gastric cancer patients has been found to be very variable [24–27]. In addition, previous results on the correlation between EGFR expression and other variables, as well as long-term outcome, have been controversial, thereby raising doubts on both the accuracy of the techniques used to evaluate its expression and the prognostic significance of this molecular marker [27, 28].
Cytokines have been proposed to play an important role in Helicobacter pylori-associated gastric inflammation and carcinogenesis, but the exact mechanism of this interaction remains unclear. Several studies have indicated that infection with H. pylori induces the expression and production of various cytokines in gastric mucosa, epithelial cells, or macrophages [29, 30]. Among the cytokines, only IL-6, has been reported to be induced by H. pylori infection in gastric epithelial cells. In addition, IL-6 strongly stimulates the growth of human gastric cancer cell lines. These findings suggest that IL-6 may have a potential role in the pathogenesis of gastric cancer. Interleukin-6, a multifunctional cytokine, is produced by a number of cells and plays a role in the defense mechanism of a host [31]. Higher serum IL-6 levels have been reported in patients with multiple myeloma [32], renal cell carcinoma [33], bladder carcinoma [34], and ovarian cancer [35], compared with normal subjects. Ravoet et al. [36] showed that tumor growth occurred during IL-6 treatment but disappeared immediately upon cessation of the IL-6 treatment. The serum IL-6 level was recently reported to correlate with the disease status of gastric carcinoma, decreasing after tumor resection and increasing when gastric carcinoma recurred [37]. The serum IL-6 level has also been reported to be an autocrine growth factor in lymphoma cell lines [38]. Diffuse IL-6 staining in the stromal area surrounding the epithelial cells was a curious result in our study. There have only been a limited number of published reports on IL-6 expression in gastric adenoma and carcinoma, and none of these used the same antibody that we used. One study of IL-6 expression in prostate tissue [39] reported that no IL-6 staining was noted in the stromal compartment of benign tissue but that there was a positive reaction for IL-6 in an atrophic area of prostate tissue. Another report [40] mentioned that immunoreactiviry to both IL-6 and VEGF was found to mainly be localized in cancer cells rather than in stromal cells. However, in both cases, IL-6 antibodies were obtained from different commercial companies than those supplying the antibodies for our study were used. We were unable to find any other published reports of stromal reaction to IL-6. Interleukin-6 may play a role in tumor-related angiogenesis by inducing tumor cell proliferation and VEGF expression in tumor cells. In our study, immunohistochemical expression of IL-6 in gastric adenoma or adenocarcinoma showed a positive reaction in 21.6% of the patient-cases. The positive immunohistochemical expression of IL-6 was significantly increased in patients with HGD or mucosal carcinoma than in those with LGD (P = 0.001). In addition, the positive immunoreactivity of IL-6 was also significantly increased in moderately and poorly differentiated adenocarcinoma compared to well-differentiated adenocarcinoma. In our study, the immunoreactivity of IL-6 seemed to increase in a histological differentiation-related manner.
Collectively, the results from previous studies on serum IL-6 are consistent with our results and suggest that IL-6 is crucial in tumor development and progression and that it may be a potential target for future research in the treatment of gastric adenoma or adenocarcinoma.
These results suggest that immunohistochemical expression of VEGF and IL-6 may facilitate clinicians to identify tumors at high risk for gastric adenoma or adenocarcinoma.
In summary, we have analyzed the clinical features and immunoreactivity of poorly differentiated adenocarcinoma following ESD. All of the tumors were >2 cm and showed positive immunoreactivity for VEGF. In addition, four of all six poorly differentiated adenocarcinomas were positive for IL-6. In this regard, it may be prudent to reflect on the inclusion criteria for ESD in gastric adenocarcinoma >2 cm and positive for VEGF and IL-6. To the best of our knowledge, this is the first report of immunohistochemical findings in gastric adenoma and early gastric cancer resected by ESD. In conclusion, we found that the immunohistochemical expression of VEGF and IL-6 in gastric adenoma and adenocarcinoma is significantly associated with histological grade. The VEGF was found to be highly expressed in HGD, suggesting a role of angiogenesis in the progression of gastric carcinoma. In addition, the immunoreactivity of IL-6 was increased in a histological differentiation-related manner, suggesting a poor prognosis. The prognostic information based on the immunohistochemical expression of VEGF and IL-6, unlike that of other tumor markers, was independent of classic clinicopathological parameters, such as the size of gastric adenoma or adenocarcinoma.
References
Folkman J. What is the evidence that tumors are angiogenesis dependent? J Natl Cancer Inst. 1990;82:4–6.
Tomoda M, Maehara Y, Kakeji Y, Ohno S, Ichiyoshi Y, Sugimachi K. Intratumoralneovascularization and growth pattern in early gastric carcinoma. Cancer. 1999;85:2340–2346.
Senger DR, Connolly DT, Van de Water L, Feder J, Dvorak HF. Purification and NH2 terminal amino acid sequence of guinea pig tumor-secreted vascular permeability factors. Cancer Res. 1990;50:1774–1778.
Connolly DT, Heuvelman DM, Nelson R, et al. Tumor vascular permeability factor stimulates endothelial cell growth and angiogenesis. J Clin Invest. 1989;84:1470–1478.
Maeda K, Chung YS, Ogawa Y, et al. Prognostic value of vascular endothelial growth factor expression in gastric carcinoma. Cancer. 1996;77:858–863.
Inoue K, Ozeki Y, Suganuma T, Sugiura Y, Tanaka S. Vascular endothelial growth factor expression in primary esophageal squamous cell carcinoma. Association with angiogenesis and tumor progression. Cancer. 1997;79:206–213.
Toi M, Hoshina S, Takayanagi T, Tominaga T. Association of vascular endothelial growth factor expression with tumor angiogenesis and with early release in primary breast cancer. Jpn J Cancer Res. 1994;85:1045–1049.
Paley PJ, Staskus KA, Gebhard K, et al. Vascular endothelial growth factor expression in early stage ovarian carcinoma. Cancer. 1997;80:98–106.
Fontanini G, Vignati S, Boldrini L, et al. Vascular endothelial growth factor is associated with neovascularization and influences progression of non-small cell lung carcinoma. Clin Cancer Res. 1997;3:861–865.
Yonemura Y, Endo Y, Fujita H, et al. Role of vascular endothelial growth factor C expression in the development of lymph node metastasis in gastric cancer. Clin Cancer Res. 1999;5:1823–1829.
Ferrara N, Davis-Smyth T. The biology of vascular endothelial growth factor. Endocr Rev. 1997;18:4–25.
Lang SA, Klein D, Moser C, et al. Inhibition of heat shock protein 90 impairs epidermal growth factor-mediated signaling in gastric cancer cells and reduces tumor growth and vascularization in vivo. Mol Cancer Ther. 2007;6:1123–1132.
Galizia G, Lieto E, Orditura M, et al. Epidermal growth factor receptor (EGFR) expression is associated with a worse prognosis in gastric cancer patients undergoing curative surgery. World J Surg. 2007;31:1458–1468.
Ito R, Nakayama H, Yoshida K, Matsumura S, Oda N, Yasui W. Expression of Cbl linking with the epidermal growth factor receptor system is associated with tumor progression and poor prognosis of human gastric carcinoma. Virchows Arch. 2004;444:324–331.
Huang SP, Wu MS, Wang HP, Yang CS, Kuo ML, Lin JT. Correlation between serum levels of interleukin-6 and vascular endothelial growth factor in gastric carcinoma. J Gastroenterol Hepatol. 2002;17:1165–1169.
Baselga J, Arteaga CL. Critical update and emerging trends in epidermal growth factor receptor targeting in cancer. J Clin Oncol. 2005;23:2445–2459.
Mendelsohn J, Baselga J. Status of epidermal growth factor receptor antagonists in the biology and treatment of cancer. J Clin Oncol. 2003;21:2787–2799.
Srivastava A, Lauwers GY. Gastric epithelial dysplasia: the Western perspective. Dig Liver Dis. 2008;40:641–649.
Fondevila C, Metges JP, Fuster J, et al. p53 and VEGF expression are independent predictor of tumor recurrence and survival following curative resection of gastric cancer. Br J Cancer. 2004;90:206–215.
Ichikura T, Tomimatsu S, Ohkura E, Mochizuki H. Prognostic significance of the expression of vascular endothelial growth factor(VEGF) and VEGF-C in gastriccarcinoma. J Surg Oncol. 2001;78:132–137.
Tzanakis N, Gazouli M, Rallis G, Giannopoulos G, Papaconstantinou I, Theodoropoulos G. Vascular endothelial growth factor polymorphism in gastric cancer development prognosis, and survival. J Surg Oncol. 2006;94:624–630.
Obst B, Wagner S, Sewing KF, Beil W. Helicobacter pylori causes DNA damage in gastric epithelial cells. Carcinogenesis. 2000;21:1111–1115.
Takehana T, Kunitomo K, Suzuki S, et al. Expression of epidermal growth factor receptor in gastric carcinomas. Clin Gastroenterol Hepatol. 2003;1:438–445.
Garcia I, Vizoso F, Martin A, et al. Clinical significance of the epidermal growth factor receptor and HER2 receptor in resectable gastric cancer. Ann Surg Oncol. 2003;10:234–241.
Mammano E, Belluco C, Sciro M, et al. Epidermal growth factor receptor(EGFR): mutational and protein expression analysis in gastric cancer. Anticancer Res. 2006;26:3547–3550.
Gamboa-Dominguez A, Dominguez-Fonseca C, Quintanilla-Martinez L, et al. Epidermal growth factor receptor expression correlates with poor survival in gastric adenocarcinoma from Mexican patients: a multivariate analysis using a standardized immunohistochemical detection system. Mod Pathol. 2004;17:579–587.
Hirono Y, Tsugawa K, Fushida S, et al. Amplification of epidermal growth factor receptor gene and its relationship to survival in human gastric cancer. Oncology. 1995;52:182–188.
Sanz-Ortega J, Steingerg SM, Moro E. et al. Comparative study of tumor angiogenesis and immunohistochemistry for p53. c-ErbB2, c-myc and EGFR as prognostic factors in gastric cancer. Histopathology 2000;15:455–462.
McNamara D, El-Omar E. Helicobacter pylori infection and the pathogenesis of gastric cancer: a paradigm for host-bacterial interactions. Dig Liver Dis. 2008;40:504–509.
Rappolee DA, Mark D, Banda MJ, Werb Z. Wound macrophages express TGF-alpha and other growth factors in vivo: analysis by mRNA phenotyping. Science. 1998;241:708–712.
Hirano T, Akira S, Taga T, Kishimoto T. Biological and clinical aspects of interleukin 6. Immunol Today. 1990;11:443–449.
Bataille R, Jourdan M, Zhang XG, Klein B. Serum levels of interleukin 6, a potent myeloma cell growth factor, as a reflect of disease severity in plasma cell dyscrasias. J Clin Invest. 1989;84:2008–2011.
Tsukamoto T, Kumamoto Y, Miyao N, Masumori N, Takahashi A, Yanase M. Interleukin-6 in renal cell carcinoma. J Urol. 1992;148:1778–1781.
Seguchi T, Yokokawa K, Sugao H, Nakano E, Sonoda T, Okuyama A. Interleukin-6 activity in urine and serum in patients with bladder carcinoma. J Urol. 1992;148:791–794.
Berek JS, Chung C, Kaldi K, Watson JM, Knox RM, Martinez-Maza O. Serum interleukin-6 levels correlate with disease status in patients with epithelial ovarian cancer. Am J Obstet Gynecol. 1991;164:1038–1042.
Ravoet C, DeGreve J, Vandewoude K, et al. Tumor stimulating effects of recombinant human interleukin-6. Lancet. 1994;344:1576–1577.
Wu CW, Wang SR, Chao MF, et al. Serum interleukin-6 levels reflect disease status of gastric cancer. Am J Gastroenterol. 1996;91:1417–1422.
Yoshizaki K, Matsuda T, Nishimoto N, et al. Pathogenic significance of interleukin-6 (IL-6/BSF-2) in Castleman’s disease. Blood. 1989;74:1360–1367.
Hobisch A, Rogatisch H, Hittmair A, et al. Immunohistochemical localization of interleukin-6 and its receptor in benign, premalignant and malignant prostate tissue. J Pathol. 2000;191:239–244.
Huang SP, Wu MS, Shum CT, et al. Interleukin-6 increases vascular endothelial growth factor and angiogenesis in gastric carcinoma. J Biomed Sci. 2004;11:517–527.
Acknowledgments
This study was supported by research funds from Dong-A University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, SA., Choi, SR., Jang, JS. et al. Expression of VEGF, EGFR, and IL-6 in Gastric Adenomas and Adenocarcinomas by Endoscopic Submucosal Dissection. Dig Dis Sci 55, 1955–1963 (2010). https://doi.org/10.1007/s10620-009-0967-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0967-1