Abstract
Purpose
Celiac disease may be associated with restless legs syndrome (RLS) because of an association with iron deficiency. Often, RLS negatively affects quality of life but may remain undiagnosed. This study evaluated the association between celiac disease and RLS.
Results
The incidence of RLS among 85 patients with celiac disease was 35%, with a prevalence of 25% compared with 10% of spouses (P < 0.02). In 79% of patients with RLS and celiac disease, neuromuscular symptoms began during or after onset of gastrointestinal symptoms. Iron deficiency was present in 40% of celiac patients with active RLS compared with 6% of patients without RLS (P < 0.001). After 6 months of a gluten-free diet, RLS symptoms improved in 50% of 28 patients.
Conclusion
Screening for celiac disease in patients with RLS is important since this commonly overlooked silent disease may be a correctable factor for some patients with idiopathic RLS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Celiac disease is common among white Americans [1], though for many patients, the disease is often undiagnosed for years [2, 3]. Gastrointestinal (GI) symptoms of celiac disease include diarrhea, abdominal pain, weight loss, and constipation [2, 4]. Celiac disease can also occur without GI symptoms, and it should be considered in patients with disorders such as osteoporosis, autoimmune diseases, infertility, and thyroid disease [2], and in children with recurrent urinary tract infections [3].
Celiac disease has been associated with neurological disorders including peripheral neuropathy, cerebellar ataxia, autonomic dysfunction, myopathy, infantile hypotonia, developmental delay, learning disorders, attention deficit hyperactivity disorder, occipital calcifications, seizures, and migraines [5–11]. These disorders may occur in patients with a wide range of GI symptoms.
Restless legs syndrome (RLS) is a central nervous system disorder that is either idiopathic or secondary to a number of conditions and is recognized as the compelling urge to move the legs that worsens at night, often with discomfort [12]. Approximately 7% of the general US population experiences RLS, resulting in sleep disruption and a poor quality of life [13]. The association between RLS and celiac disease has not been previously reported.
Iron deficiency is a common extraintestinal complication of celiac disease and may precede GI symptoms [14, 15]. Important neurology research has shown that patients with RLS usually have central nervous system iron deficiency [16] and may have reduced peripheral iron levels [17]. Also, low amounts of ferritin appear to correlate with increased RLS symptom severity [18]. The commonality of iron deficiency with both celiac disease and RLS prompted an investigation of the epidemiology of RLS in patients with celiac disease.
Methods
Study Design and Definition of Cases
Adults with celiac disease were prospectively interviewed at a community adult gastroenterology clinic over a 6-month period (October 2007 to March 2008) for study inclusion. Additional patients were recruited to the study by a search of a database of patients with celiac disease seen at the same gastroenterology practice during the previous 5 years (October 2002 to October 2007). Evaluation included every patient given the International Classification of Diseases code 579.0 for celiac disease. A chart review documented that standardized criteria for celiac disease were met. The diagnostic criteria to include patients with celiac disease included GI symptoms and/or idiopathic iron deficiency anemia that improved on a gluten-free diet, concomitant with one of the following: (1) duodenal villous blunting or atrophy, increased intraepithelial lymphocytes, elevated tissue transglutaminase immunoglobulin A antibody (tTG; first generation assay abnormal result was tTG >30 U/ml and second generation assay abnormal result was tTG >10 U/ml), and a normal serum immunoglobulin A (IgA) level; (2) duodenal villous blunting or atrophy and increased intraepithelial lymphocytes (included patients who were not tested for tTG or those who had a low tTG level with a low total IgA level); or (3) an elevated tTG.
Patients who met the inclusion criteria were evaluated for RLS. One gastroenterologist (Leonard B. Weinstock) conducted all the standardized interviews. The interviewer asked all patients to confirm that “a survey could be given regarding celiac disease and a condition called restless legs syndrome.” The interviewer described RLS, and patients were asked if they had experienced RLS symptoms at some point in their life. Patients were considered to have RLS if they met all four International Restless Legs Syndrome Study Group diagnostic criteria [19], including the following: the urge to move legs with some discomfort; motor restlessness, symptom worsening with rest that is relieved by movement, worsening of symptoms late in the day or at night. These criteria were reviewed with patients, and a positive response to questions about each was required to establish a positive history of RLS. Incidence of RLS was defined as having had RLS during any period of the patients’ lives. Prevalence of RLS was defined as having active RLS symptoms at the time patients completed the survey. A human studies committee approved the study (Sterling Institutional Review Board; Atlanta, GA). The prevalence of RLS in the spouses of patients and the age of the spouses were determined during the patient interviews. The spouses served as the control population for prevalence data.
Data Collection
Clinical characteristics, concomitant secondary RLS diseases, family history of RLS, history of anemia and iron deficiency, and timing of RLS onset with respect to GI symptoms were queried. Data were collected to determine the use of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, dopamine receptor blockers, antipsychotics, and dopamine agonists because these medications can affect RLS symptom severity [20]. A review of patients’ laboratory data was performed to validate a history of iron deficiency. Restless legs syndrome severity was determined by a prospective assessment using the international restless legs scale (IRLS) [19] in those currently affected. The IRLS system comprises ten questions with responses ranging from 0 to 4 (range of score, 0–40); the score reflects the frequency and severity of sensory and motor aspects of RLS on sleep, mood, and activities of daily living. Patients were asked if RLS symptoms improved on a gluten-free diet, and, if so, to estimate the percent of symptom improvement and the length of time to achieve improvement. Patients were also asked whether they took iron supplements during this time. Patients with inactive RLS were asked retrospectively to describe an average week when they experienced RLS symptoms using the IRLS questionnaire.
Statistical Analysis
The chi-square test was used to compare patient and control groups. A P value of <0.05 was considered significant. Odds ratios (ORs) and 95% confidence intervals (CIs) estimated by unconditional logistic regression were used to evaluate the prevalence of RLS in patients compared with spouse controls.
Results
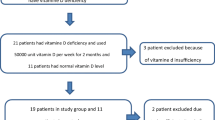
Participants
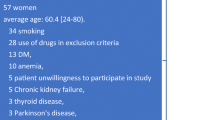
Ninety-five patients met RLS criteria; ten patients from the database search were lost to follow-up (three died and seven moved without an available telephone number or address). All remaining 85 patients completed the survey: 34 patients during prospective clinic visits and 51 patients (identified through the database search) during telephone interviews. The study included 85 patients with celiac disease and 63 spouses without celiac disease. A similar percentage of patients with celiac disease and RLS was married (73%) compared with patients with celiac disease without RLS (75%; Table 1). More males were in the spouse control group than in the celiac group, but the mean age of the spouse group was not significantly different than that of the celiac group. Most study participants had their celiac disease diagnosed with a positive biopsy and had an elevated tTG or a positive biopsy alone (Table 1).
Secondary Risk Factors for RLS
Secondary RLS conditions other than iron deficiency were uncommon in the patients with and without RLS. A review of family histories revealed prevalence of RLS in a first-degree relative of approximately 20% in both patient groups (Table 1). One patient with RLS had a first-degree relative with both celiac disease and RLS. A similar proportion of patients with RLS took SSRIs (7%) compared with patients without RLS (9%), and use of SSRIs did not appear to have an effect on RLS symptoms. No patients with RLS used tricyclic antidepressants compared with 4% of patients without RLS. No RLS study participants used dopamine antagonists or dopamine agonists. One patient without RLS who also had Parkinson’s disease took dopaminergic medication. Medication data were not available for the spouse controls.
Restless Legs Syndrome in Patients with Celiac Disease and Risk of Iron Deficiency
None of the celiac patients with RLS had been previously diagnosed with RLS by a physician or knew that they could seek treatment for this condition. The incidence of RLS in patients with celiac disease was 35%; the incidence of RLS was not evaluated in spouse controls. The prevalence of RLS in patients with celiac disease was 25% (95% CI, 15–34%) compared with a prevalence of 10% (95% CI, 2–17%) in spouse controls (P < 0.02; OR = 3.1; Fig. 1). The percentage of female patients with celiac disease and RLS (93%) was higher than the percentage of female patients with celiac disease but without RLS (75%; P < 0.05). Concomitant iron deficiency was significantly more common in celiac patients with active RLS (40%) than celiac patients without RLS (6%; P < 0.001; Table 2; Fig. 2). A larger proportion of celiac patients with active RLS also had a prior history of iron deficiency (57%) than celiac patients without RLS (44%), but the difference was not significant (P = 0.441; Table 2). Interestingly, a lower percentage of celiac patients with RLS were currently anemic (15%) compared with celiac patients without RLS (39%), but the difference was not significant (P < 0.057; Table 2). Comparing celiac patients with active RLS versus prior RLS, a higher percentage of patients with active RLS symptoms had current iron deficiency than patients with a prior history of RLS (Table 2), although no formal statistical comparisons were conducted.
Characteristics and Outcome of Restless Legs Syndrome
Restless legs syndrome started during or after the onset of GI symptoms in 79% of patients and before GI symptoms in 21% (Fig. 3). Restless legs syndrome went undiagnosed and untreated in patients for an average of 6 years (range, 0.5–40 years; standard deviation, 10 years; Table 1). Patients with RLS had their celiac disease diagnosed for a mean of 6 years but recalled having GI symptoms for an average of 14 years before a formal diagnosis. However, patients without RLS experienced a mean of 10 years (standard deviation, 13 years) of GI symptoms before their celiac disease was diagnosed. The difference in the duration of celiac disease in patients who had the disease diagnosed and those who did not was not clinically significant.
Percentage of patients with celiac disease and restless legs syndrome (RLS) (n = 30) who described having onset of RLS symptoms before or during/after initiation of gastrointestinal (GI) symptoms. A substantially greater percentage of patients with celiac disease reported initiation of RLS symptoms during or after experiencing GI symptoms rather than before experiencing GI symptoms. Noteworthy is the fact that RLS may precede GI disturbance and diagnosis of celiac disease
Twenty-eight of the patients with RLS were interviewed to see if they thought that initiating the gluten-free diet correlated with overall improvement of RLS symptoms. Of this group, 14 (50%) stated that their RLS symptoms improved on a gluten-free diet, and the mean percent improvement of RLS symptoms was 78%, which occurred after a mean of 5.7 months on a gluten-free diet. Restless legs syndrome resolved completely in nine of these patients. Two patients had their RLS diagnosed close to the time of study initiation, so they were not asked to describe the effects of a gluten-free diet on their RLS symptoms.
Discussion
This study is the first to investigate the epidemiology of RLS in celiac disease. Restless legs syndrome was found to be a frequently associated condition in 85 patients with celiac disease: the incidence was 35%, and the prevalence was 25%. The findings of this study have clinical importance for several reasons. Celiac disease is emerging as the “great modern-day imposter,” often presenting with extraintestinal manifestations [21]. Celiac disease is often clinically silent or has mild GI symptoms and, therefore, may be undiagnosed for many years. Most cases of RLS are idiopathic [20], and determining adequate treatment can be challenging [13]. In this study, 50% of 28 patients had substantial improvement in their RLS symptoms after gluten withdrawal. This might be due to improved iron absorption, although other factors such as reductions in inflammation or bacterial overgrowth may have played a role in some patients. Recognition that RLS occurs in patients with celiac disease could yield potential diagnostic and therapeutic benefits for both groups of patients.
This study presents the epidemiology of RLS in patients with celiac disease, and because an association between the two conditions has been newly recognized, further studies are warranted. The small sample size and the retrospective nature of the study, including the potential for patients’ self-selection for inclusion and recall bias of RLS and celiac disease symptoms, could limit the accuracy of the results. Ferritin levels were not measured in or available from all patients. This made the assessment of RLS severity and comparison of iron deficiency problematic, although low-normal ferritin levels (<50 ng/ml) are clinically significant in RLS [18, 22, 23]. The use of spouses for controls may have been less ideal than age- and sex-matched controls, since prevalence of RLS tends to vary by sex in large epidemiologic studies. In 10,263 French adults, the incidence of RLS over a 12-month period in females was 10.8% compared with 5.8% in males [24]. In 2,019 Canadians, 17% of females and 13% of males had RLS [25]. In 1,803 adults in the United States, the prevalence of RLS was 10% and did not differ by sex [26]. In another study that we performed in 272 patients with Crohn’s disease and 177 spouse controls, both groups were well matched for age and sex distribution, and the prevalence of RLS in spouses was 8% [27]. In comparison, the prevalence of RLS in spouse controls in the current work was 10%, indicating that the presence of RLS in this group was similar to that found in larger studies within the general adult population [25, 26]. The overall higher prevalence of RLS in patients with celiac disease in this study compared with spouse and historical controls is an interesting finding. Furthermore, this observation may not be limited to adults, as others in the community setting have observed RLS to be frequently diagnosed in pediatric patients with celiac disease (Alessio Fasano, MD, personal communication, January 2008).
The original rationale for this study was that both conditions often have concomitant iron deficiency, and central nervous system iron deficiency is a pathogenic factor in RLS. Peripheral iron deficiency can be subtle and variable in patients with celiac disease [14, 15], as often is the case in patients with RLS [17]. Central nervous system iron deficiency does not always correlate with peripheral iron deficiency, although to varying degrees, iron repletion can be helpful in the management of patients with RLS [16, 28]. After patients with celiac disease initiate a gluten-free diet, anemia may improve without iron administration, but there is a lag time to total correction of iron deficiency [14]. In one study, after 6 months of a gluten-free diet, 14 of 18 patients (78%) recovered from anemia, but only 5 of 18 (28%) recovered from iron deficiency, and at 12 months only 9 of 18 patients (50%) experienced normalization of their iron deficiency [14]. These observations help support the finding of the present study in which 50% of 28 patients had RLS improvement, and patients felt most relieved of RLS symptoms after a mean of 6 months after starting the gluten-free diet. Iron deficiency was found to be more common but not universal in patients with celiac disease and active RLS than in those with celiac disease and prior RLS or those with celiac disease but without RLS.
Furthermore, small intestinal bacterial overgrowth (SIBO) is associated with both celiac disease [29] and irritable bowel syndrome (IBS) [30, 31], suggesting that increases in inflammation due to a high concentration of intestinal bacteria may be involved in both conditions. This is particularly interesting given that refractory symptoms of celiac disease [29] and IBS [32] can be relieved by antibiotic therapy. In healthy volunteers, administration of bacterial lipopolysaccharides induced the expression of inflammatory cytokines (i.e, interleukin-6), which was temporally associated with hypoferremia [33]. Interleukin-6 upregulates the levels of hepcidin, a liver-produced hormone that controls plasma iron levels by regulating absorption of dietary iron from the intestine [34, 35]. Hepcidin in turn induces the internalization and degradation of ferroportin, reducing cellular iron efflux [35]. Although alternative explanations are possible, we hypothesize that celiac disease–associated SIBO can lead to chronic inflammation and poor iron uptake, which can both increase the likelihood of developing RLS and exacerbate RLS symptoms [16].
This study suggests that celiac disease is frequently associated with RLS and that treatment with a gluten-free diet, aggressive replacement of iron, or antibiotic treatment of bacterial overgrowth may improve the quality of life in patients with celiac disease who have RLS. Screening for celiac disease in patients with idiopathic RLS may have importance because celiac disease is a commonly overlooked silent disease. Thus, celiac disease may be an underlying correctable factor for some patients diagnosed with idiopathic RLS.
References
Green PH. The many faces of celiac disease: clinical presentation of celiac disease in the adult population. Gastroenterology. 2005;128:S74–S78.
Cranney A, Zarkadas M, Graham ID, et al. The Canadian celiac health survey. Dig Dis Sci. 2007;52:1087–1095.
Saalman R, Fallstrom SP. High incidence of urinary tract infection in patients with coeliac disease. Arch Dis Child. 1996;74:170–171.
Rampertab SD, Pooran N, Brar P, Singh P, Green PH. Trends in the presentation of celiac disease. Am J Med. 2006;119(355):e9–e14.
Briani C, Zara G, Toffanin E, et al. Neurological complications of celiac disease and autoimmune mechanisms: preliminary data of a prospective study in adult patients. Ann N Y Acad Sci. 2005;1051:148–155.
Gabrielli M, Cremonini F, Fiore G, et al. Association between migraine and celiac disease: results from a preliminary case-control and therapeutic study. Am J Gastroenterol. 2003;98:625–629.
Gobbi G, Bouquet F, Greco L, et al. Coeliac disease, epilepsy, and cerebral calcifications. The Italian working group on coeliac Disease and epilepsy. Lancet. 1992;340:439–443.
Green PH, Alaedini A, Sander HW, Brannagan TH 3rd, Latov N, Chin RL. Mechanisms underlying celiac disease and its neurologic manifestations. Cell Mol Life Sci. 2005;62:791–799.
Hadjivassiliou M, Chattopadhyay AK, Grunewald RA, et al. Myopathy associated with gluten sensitivity. Muscle Nerve. 2007;35:443–450.
Tursi A, Giorgetti GM, Iani C, et al. Peripheral neurological disturbances, autonomic dysfunction, and antineuronal antibodies in adult celiac disease before and after a gluten-free diet. Dig Dis Sci. 2006;51:1869–1874.
Zelnik N, Pacht A, Obeid R, Lerner A. Range of neurologic disorders in patients with celiac disease. Pediatrics. 2004;113:1672–1676.
Walters AS. Toward a better definition of the restless legs syndrome. The international restless legs syndrome study group. Mov Disord. 1995;10:634–642.
Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165:1286–1292.
Annibale B, Severi C, Chistolini A, et al. Efficacy of gluten-free diet alone on recovery from iron deficiency anemia in adult celiac patients. Am J Gastroenterol. 2001;96:132–137.
Harper JW, Holleran SF, Ramakrishnan R, Bhagat G, Green PH. Anemia in celiac disease is multifactorial in etiology. Am J Hematol. 2007;82:996–1000.
Allen RP, Earley CJ. The role of iron in restless legs syndrome. Mov Disord. 2007;22(Suppl 18):S440–S448.
Aul EA, Davis BJ, Rodnitzky RL. The importance of formal serum iron studies in the assessment of restless legs syndrome. Neurology. 1998;51:912.
Sun ER, Chen CA, Ho G, Earley CJ, Allen RP. Iron and the restless legs syndrome. Sleep. 1998;21:371–377.
Walters AS, LeBrocq C, Dhar A, et al. For the international restless legs syndrome study group. Validation of the international restless legs syndrome study group rating scale for restless legs syndrome. Sleep Med. 2003;4:121–132.
Satija P, Ondo WG. Restless legs syndrome: pathophysiology, diagnosis and treatment. CNS Drugs. 2008;22:497–518.
Lee SK, Green PH. Celiac sprue (the great modern-day imposter). Curr Opin Rheumatol. 2006;18:101–107.
Berger K, von Eckardstein A, Trenkwalder C, Rothdach A, Junker R, Weiland SK. Iron metabolism and the risk of restless legs syndrome in an elderly general population–the MEMO-Study. J Neurol. 2002;249:1195–1199.
Oertel WH, Trenkwalder C, Zucconi M, et al. State of the art in restless legs syndrome therapy: practice recommendations for treating restless legs syndrome. Mov Disord. 2007;22(Suppl 18):S466–S475.
Tison F, Crochard A, Leger D, Bouee S, Lainey E, El Hasnaoui A. Epidemiology of restless legs syndrome in French adults: a nationwide survey: the INSTANT Study. Neurology. 2005;65:239–246.
Lavigne GJ, Montplaisir JY. Restless legs syndrome and sleep bruxism: prevalence and association among Canadians. Sleep. 1994;17:739–743.
Phillips B, Young T, Finn L, Asher K, Hening WA, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000;160:2137–2141.
Weinstock L, Bosworth B, Scherl E, et al. Crohn’s disease is associated with restless legs syndrome: a new extraintestinal manifestation [ACG abstract 1115]. Am J Gastroenterol. 2008;103:S435–S436.
Earley CJ, Heckler D, Allen RP. Repeated iv doses of iron provides effective supplemental treatment of restless legs syndrome. Sleep Med. 2005;6:301–305.
Tursi A, Brandimarte G, Giorgetti G. High prevalence of small intestinal bacterial overgrowth in celiac patients with persistence of gastrointestinal symptoms after gluten withdrawal. Am J Gastroenterol. 2003;98:839–843.
Pimentel M, Chow EJ, Lin HC. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol. 2000;95:3503–3506.
Pimentel M, Chow EJ, Lin HC. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome: a double-blind, randomized, placebo-controlled study. Am J Gastroenterol. 2003;98:412–419.
Sharara AI, Aoun E, Abdul-Baki H, Mounzer R, Sidani S, ElHajj I. A randomized double-blind placebo-controlled trial of rifaximin in patients with abdominal bloating and flatulence. Am J Gastroenterol. 2006;101:326–333.
Kemna E, Pickkers P, Nemeth E, van der Hoeven H, Swinkels D. Time-course analysis of hepcidin, serum iron, and plasma cytokine levels in humans injected with LPS. Blood. 2005;106:1864–1866.
Nemeth E, Rivera S, Gabayan V, et al. Il-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Invest. 2004;113:1271–1276.
Nemeth E, Tuttle MS, Powelson J, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004;306:2090–2093.
Acknowledgments
The authors would like to thank Barry H. Cohen, PhD (Director, MA Program in Psychology; New York University; 6 Washington Place, New York, New York 10003), for assisting with statistical analysis. Editorial assistance was provided under the direction of the authors by MedThink Communications with support from Salix Pharmaceuticals, Inc. Presented at the American College of Gastroenterology annual scientific meeting, 3–8 October 2008.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosures
Dr. Weinstock is on the speaker’s bureau for Salix Pharmaceuticals, Inc. Dr. Walters has received research funding from the National Institutes of Health; Xenoport Inc., Schwarz Pharma, and Kyowa Pharmaceuticals, Inc. Dr. Walters has received research funding and is on the speaker’s bureau of GlaxoSmithKline and Boehringer-Ingelheim. Dr. Mullen: none. Dr. Duntley: none.
Rights and permissions
About this article
Cite this article
Weinstock, L.B., Walters, A.S., Mullin, G.E. et al. Celiac Disease Is Associated with Restless Legs Syndrome. Dig Dis Sci 55, 1667–1673 (2010). https://doi.org/10.1007/s10620-009-0943-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0943-9