Abstract
Background
The endoscopy unit before remediation may be a high-risk area for slip and fall injuries due to a large number of exposed above-the-floor wires in the endoscopy rooms, dimmed lighting during endoscopic procedures, and staff inattention to obstacles due to preoccupation with the endoscopic patient.
Aim
To describe a novel, previously unappreciated workplace hazard to endoscopic personnel: Exposed wires in the endoscopy unit.
Methods
This study is a retrospective review of 110,000 endoscopic procedures performed during the last 5 years at an academic, teaching hospital with a high-volume endoscopy unit. All significant orthopedic injuries to endoscopic personnel from slips, twists, and falls from tripping over exposed cords in the endoscopy unit were reviewed. The severity of injury was documented based on roentgenographic findings, number of days of missed work, number of days with a modified work schedule, and requirement for orthopedic surgery. The number of potentially exposed cords per endoscopy room was determined.
Results
During the 5-year study period, three endoscopic personnel suffered significant orthopedic injuries from slips, twists, and falls from tripping over cords, wires, or tubing lying exposed over the floor in the endoscopy suite: The resulting injuries consisted of fourth and fifth metacarpal hand fractures due to a fall after tripping on oxygen tubing; a rib fracture due to tripping on electrical wires trailing from an endoscopy cart; and a grade II ankle sprain due to the foot becoming entangled in oxygen tubing. All injuries resulted in lost days of work [mean 9.3 ± 11.0 (SD) days] and in additional days of restricted work (mean 41.7 ± 31.8 days). One injury required orthopedic surgery. Hospital review revealed a mean of 35.3 ± 7.5 cords, wires, or tubing per endoscopy procedure room, the majority of which were exposed above the floor before remediation (n = 10 rooms). Remediation of exposed wires included: bundling related wires together in a cable to reduce the number of independent wires, covering exposed wires on the floor with a nonslip heavy mat, and running wires from ceiling outlets to equipment high above ground (e.g. mounted endoscopy video monitors).
Conclusions
Tripping, slipping, and falling over exposed wires can cause significant injury to endoscopic personnel. This previously undescribed hazard should be preventable by simple remediation, and all endoscopic personnel, hospital architects, hospital administrators, and governmental regulators should be alerted to this potential hazard
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With longer experience with endoscopy, specific injury patterns are being increasingly appreciated among endoscopic personnel due to joint or muscle overuse or other hazards in the endoscopy suite. Previously reported injuries include DeQuervain’s syndrome (colonoscopist’s thumb) from left thumb overuse in turning the control dials during colonoscopy [1], back injuries from wearing a heavy lead apron during endoscopic retrograde cholangiopancreatography (ERCP) [2–5], and epicondylitis (tennis elbow) from repetitive wrist extension and abduction during colonoscopy [2, 6]. Three novel cases of orthopedic injury to endoscopic personnel due to slips, twists, and falls from tripping over exposed cords in the endoscopy suite are reported here. A simple, cost-effective remediation is also reported that should theoretically eliminate this hazard.
Methods
This study is designed as a retrospective review of the endoscopy unit files, the medical files of the hospital, and interviews with endoscopic personnel. Three cases of slip, twist, and fall injuries among personnel in the endoscopy unit during performance of 110,000 endoscopies during the period from March 2004 through February 2009 were identified. This study was approved by the Human Investigation Committee/Institutional Review Board of William Beaumont Hospital.
Case Reports
Metacarpal Fractures
A previously healthy, left-handed, 51-year-old, white, female endoscopy nurse, with no prior orthopedic or neurologic diseases, tripped over the supplemental oxygen tubing lying exposed over the floor in the endoscopy suite and fell on and injured the dorsal aspect of her right hand while accessing endoscopic equipment during an endoscopy. She did not notice the oxygen tubing because the room was darkened during the procedure. She presented to the emergency room several minutes later complaining of constant, severe, right hand pain exacerbated by hand movement. Physical examination revealed tenderness, soft tissue edema, and ecchymosis over the ulnar dorsal aspect of the right hand. There was no sensory or motor deficit and no evident vascular compromise in the hand. Right hand and wrist roentgenograms revealed an oblique fracture of the diaphysis of the third metacarpal and a comminuted fracture of the diaphysis of the fourth metacarpal. She underwent open surgical reduction and internal fixation of these metacarpals using multiple screws for each fracture. The nurse missed 4 weeks of work postoperatively. She then resumed work as an endoscopy charge nurse, rather than a regular endoscopy nurse, to limit right hand stress. She is expected to have mild permanent partial loss of right hand function despite attending physical therapy. She can write normally because she is left-handed.
Rib Fracture
A 43-year-old, white, female endoscopy technician with a medical status of a motorcycle injury 8 years earlier, complicated by fourth through eighth left rib fractures treated conservatively, tripped over wires trailing above the floor from an endoscopy cart and fell and hit the left side of her chest against a metal cart while assisting in a darkened endoscopy room. She presented to the emergency room soon thereafter complaining of severe left lower chest wall pain exacerbated by respiration, but without dyspnea. Physical examination revealed an ecchymosis and moderate tenderness on the chest wall overlying the left lateral ninth rib. There was no local crepitus and sensory or motor deficits. Raising the left arm was limited due to the pain. Anteroposterior and oblique roentgenograms of the left ribs and a chest roentgenogram revealed an acute, minimally displaced fracture of the lateral aspect of the ninth left rib, the other, old, healed rib fractures, and no pneumothorax. The patient was treated with ibuprofen 600 mg four times daily, and hydrocortisone bitartrate 10 g and acetaminophen 1000 mg (Vicodin) at bedtime. The patient did not work for 3 days. She then resumed work with restrictions of lifting no more than 15 pounds, minimal abdominal bending, no turning of the chest, and no overhead work. This restricted her to clerical work for 12 weeks, after which she became pain-free without requiring any further analgesics and resumed full-work duties.
Grade II Ankle Sprain
A previously healthy, 54-year-old, white, male gastroenterologist got his left foot entangled on the supplemental oxygen tubing lying above the floor and twisted his left ankle without falling during an endoscopy. He did not notice the tubing because the room was darkened during an endoscopy. He presented to an orthopedist the next morning complaining of increasingly severe left ankle pain exacerbated by foot movement. Physical examination revealed ecchymosis, edema, and tenderness at the left ankle, and exacerbation of ankle pain with forced ankle inversion. Left ankle roentgenograms did not reveal any fracture. The grade II left lateral ankle sprain was treated with daily ice packs for 3 days, with orally administered ibuprofen 600 mg four times daily, and with an elastic bandage for 4 weeks. The physician missed work for 3 days, then resumed work limited to nonclinical hospital administration for 5 work days, and then resumed his full clinical duties, with no functional restrictions or medical consequences.
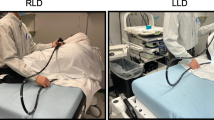
Remediation of Exposed Wires to Prevent Falls
The three injuries occurred during the performance of 110,000 endoscopies during a 5-year period at one hospital. Hospital review revealed a mean of 35.3 ± 7.5 cords, wires, and tubing per endoscopy room during procedures (n = 10 rooms).Footnote 1 Before remediation most of these wires were exposed above the floor. As remediation measures, wires arising from the wall plugged into electrical units <2 m above the floor, such as the endoscopy cart, were switched from being completely exposed above the floor to being completely covered by a heavy metal nonslip mat (Fig. 1a); wires plugged into electrical units high (>2 m) above the floor, such as mounted endoscopy monitors, were switched from coming from wall outlets to dropping from ceiling outlets to reduce the number of wires above the floor (Fig. 1b1); individual wires were combined into cables to reduce the number of independent wires (Fig. 1b2); wires for accessory nonendoscopic equipment (e.g., computers, telephones) were embedded in the wall with the nonendoscopic equipment placed on a counter near the wall (Fig. 1c). Exposed tubing for supplemental oxygenation or endoscopic suction was covered by a heavy metal nonslip mat such as that used for exposed wires on the floor (Fig. 1a). These remediation measures virtually eliminated exposed wires and tubing.
Remediation measures for exposed cords, wires, and tubing to reduce slip and fall hazards in the endoscopy suite, as illustrated in an endoscopy room equipped with fluoroscopy for endoscopic retrograde cholangiopancreatography. a Covering exposed wires on the floor using a nonslip mat. a1 Before remediation, five cords run above the floor and represent a fall hazard; these include three cables for the transmission of colors to the endoscopic video monitor, one cable to a power strip on the endoscopy cart (to supply electricity to the endoscopic video processor, light source, water pump, coagulation/cautery unit, etc.), and one soft plastic tubing from the wall vacuum to an endoscopic port for endoscopic suction. Soft plastic tubing forms loops above the ground, which present a particular hazard for falls. The soft plastic tubing is used for the wall suction and for the supplemental oxygen. Note the wheels at the bottom of the endoscopy cart on the right of the photographs a1–a3. a2 During remediation, the four cables and the one plastic tubing which ran above the floor in a1 are placed in the grooves of an opened nonslip mat. a3 After remediation: Closing the top door of the nonslip mat conceals the five previously exposed cords or tubing within the mat to eliminate the fall hazard. b1 Outlets from ceiling. Photograph shows outlets placed on the ceiling rather than the walls for wires leading to endoscopic equipment placed >2 m above the floor (e.g., illustrated mounted endoscopic video monitor). This arrangement avoids running these wires directly on the floor and reduces the fall hazard. b2 Bundling of wires. Close-up photograph of the outlet area in b1 shows bundling of ten wires arising individually from outlets in the ceiling to form a single thick cable to reduce the number of independent wires coursing through the room. Note the additional plug arising from the nearby electrical outlet that powers the endoscopic video monitor. c Accessory nonendoscopic equipment placed on countertop near wall. Side-view photograph taken behind the computer in the endoscopy room shows numerous wires embedded within the wall and running just a few inches on the countertop to the computer, computer monitor, internet access, keyboard, and telephone. This arrangement avoids running wires to this equipment on the floor
Discussion
Tripping over cords, wires, and tubing may be a significant, previously unappreciated cause of injury in the endoscopy suite. The currently reported rate extrapolates to approximately 450–600 slip and fall injuries per annum in the USA [calculated as: {3 falls/110,000 endoscopies) × (15–20 million endoscopies per annum in America) [7]}. The obvious pathophysiology is tripping over cords, wires, or tubing exposed above the floor. Contributing factors may include: (1) poor visibility of exposed cords due to dimmed lights during endoscopy; (2) staff inattention to exposed cords due to their preoccupation with the patient during endoscopy; (3) difficulty in negotiating around bulky equipment, such as an endoscopy cart, in cramped passageways in the endoscopy suite. Two of the three reported injuries occurred from tripping or becoming entangled in the oxygen tubing. Soft plastic tubing may pose a particularly strong risk factor for injury because endoscopic personnel may get their feet entangled in loops formed by such tubing (Fig. 1a). An independent risk factor for slipping is the spillage onto the floor of liquids from a leaky endoscopic valve or of surgical lubricants placed on the endoscope tip during endoscopy.
Trailing cords are an established major fall hazard in other work environments or the home [8]. The other contributing risk factors in the endoscopy suite have also been previously described in other environments: poor lighting [9–11], worker inattention to the physical environment [12, 13], cramped passageways [14, 15], and slippery or wet floors [9, 16]. What is novel in this study is the application of these principles to the endoscopy suite, the recognition that the endoscopy suite before remediation is a potential minefield of numerous exposed wires, and the description of simple, inexpensive remediation measures to eliminate this hazard. The remediation measures include bundling individual wires into cables, dropping wires to mounted equipment from ceiling outlets, and covering exposed wires or tubing on the floor with heavy nonslip mats. The effects of the reported remediation have not been clinically analyzed, and thus the remediation has not been proven to be effective. The reported remediations, however, are physiologically and biologically reasonable actions aimed at reducing or preventing injuries. New endoscopy suites should be designed to avoid cords, wires, and tubing exposed above the floor.
Notes
Cords, wires, and tubing: (1) in all ten rooms included those for the main endoscopic television monitor, endoscopy cart, endoscope water pump, supplemental oxygen, wall vacuum, intravenous line, blood pressure cuff, electrocardiographic leads, and pulse oximetry; (2) in eight rooms for the auxiliary endoscopic television monitor; (3) in one (ERCP) room for the portable X-ray machine, fluoroscopy display monitor, electrically powered ERCP stretcher, and anesthesia gas machine. In all ten rooms, an additional 11.3 + 1.1 wires were easily embedded in the wall and are not included in the above total. These wires were for telephone jacks, computer, computer monitor, keyboard, mouse, and X-ray view box (Fig. 1c).
References
Cappell MS. Colonoscopist’s thumb: DeQuervain’s syndrome (tenosynovitis of the left thumb) associated with overuse during endoscopy. Gastrointest Endosc. 2006;64(5):841–843.
Buschbacher R. Overuse syndromes among endoscopists. Endoscopy. 1994;26(6):539–544.
Hansel SL, Crowell MD, Pardi DS, Bouras EP, Dibaise JK. Prevalence and impact of musculoskeletal injury among endoscopists: a controlled pilot study. J Clin Gastroenterol. 2009;43(5):399–404.
Keate RF, Drden GW, Wang K, Chen YK, et al. Occupational injuries to endoscopists: report from the ASGE web survey. Abstract S1450. Gastrointest Endosc. 2006;63(5):111.
Liberman AS, Shrier I, Gordon PH. Injuries sustained by colorectal surgeons performing colonoscopy. Surg Endosc. 2005;19(12):1606–1609.
Shergill AK, Asundi KR, Barr A, et al. Pinch force and forearm-muscle load during routine colonoscopy: a pilot study. Gastrointest Endosc. 2009;69(1):142–146.
Seeff LC, Richards TB, Shapiro JA, et al. How many endoscopies are performed for colorectal cancer screening? results from CDC’s survey of endoscopic capacity. Gastroenterology. 2004;127(6):1670–1677.
Stevens M, Holman CD, Bennett N. Preventing falls in older people: impact of an intervention to reduce environmental hazards in the home. Am Geriatr Soc. 2001;49(11):1442–1447.
Bentley TA, Haslam RA. Identification of risk factors and countermeasures for slip, trip and fall accidents during the delivery of mail. Appl Ergon. 2001;32(2):127–134.
McMurdo ME, Millar AM, Daly F. A randomized controlled trial of fall prevention strategies in old peoples’ homes. Gerontology. 2000;46(2):83–87.
Morley JE. Falls: where do we stand? Mo Med. 2007;104(1):63–67.
Bellemere P. A national campaign for the prevention of hand accidents. Chir Main. 2003;22(5):233–239.
Pickett W, Brison RJ, Niezgoda H, Chipman ML. Nonfatal farm injuries in Ontario: a population-based survey. Accid Anal Prev. 1995;27(4):425–433.
Kallin K, Jensen J, Olsson LL, Nyberg L, Gustafson Y. Why the elderly fall in residential care facilities, and suggested remedies. Fam Pract. 2004;53(1):41–52.
Schillings AM, Mulder T, Duysens J. Stumbling over obstacles in older adults compared to young adults. Neurophysiol. 2005;94(2):1158–1168.
Tammelleo AD. Legal case briefs for nurses, AL: nurse spills water—patient falls: liability issue. NY Regan Rep Nurs Law. 1991;31(9):3.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cappell, M.S. Injury to Endoscopic Personnel from Tripping over Exposed Cords, Wires, and Tubing in the Endoscopy Suite: A Preventable Cause of Potentially Severe Workplace Injury. Dig Dis Sci 55, 947–951 (2010). https://doi.org/10.1007/s10620-009-0923-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0923-0