Abstract
Purpose
Nonsteroidal anti-inflammatory drugs (NSAIDs) often cause ulcers in the small intestine in humans, but there are few effective agents for treatment of small intestinal ulcers. We found that soluble dietary fibers (SDFs), such as pectin, could prevent the formation of small intestinal lesions induced by indomethacin (IND) in cats. To elucidate the mechanism of protection by SDFs, we examined the viscosities of SDFs and the effects of pectin on gastrointestinal absorption of IND and intestinal hypermotility induced by IND.
Methods
Cats were given regular dry food (RFD-Dry) or RFD-Dry supplemented with pectin, guar gum, polydextrose, or mucin twice daily. IND was administered orally once daily for 3 days. Mucosal lesions in the small intestine were examined 24 h after the final dosing of IND. Plasma concentrations of IND were measured by HPLC. GI motilities were measured using a telemetry system in conscious cats implanted with force transducers. Viscosities of the SDFs were measured using a viscosimeter.
Results
In cats given RFD-Dry, IND (3 mg/kg) increased motility and produced many lesions in the lower half of the small intestine; the total lesion area (TLA) was 7.5 ± 2.6 cm2 (n = 4). Lesions induced by IND were markedly decreased in cats given RFD-Dry supplemented with 3% pectin, guar gum, polydextrose or mucin; TLAs were 0.6 ± 0.3, 0.0 ± 0.0, 1.3 ± 0.8 and 1.6 ± 0.5 cm2 (n = 4) (P < 0.05 vs. RFD-Dry alone), respectively. The viscosity (mPa-S) of pectin, guar gum, polydextrose and mucin (3% concentration) was 414, >1,200, 1 and 4, respectively. Pectin did not affect the absorption of IND nor did it inhibit IND-induced intestinal hypermotility.
Conclusions
SDFs protect the small intestine against NSAID-induced damage, probably by compensating a barrier function of the mucin decreased by IND. Viscosities of the SDFs play a role, at least in part, in the protective effects of the SDFs on the small intestine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent progress in endoscopy, such as the development of capsule endoscopy, has revealed that in humans, non-steroidal anti-inflammatory drugs (NSAIDs) often cause ulcers not only in the upper gastrointestinal (GI) tract, but also in the middle and lower small intestine [1–5]. In contrast with upper GI ulcers, there are few effective agents for the prophylaxis and treatment of small intestinal ulcers. Therefore, the identification of effective therapies for the treatment of NSAID-induced small intestinal ulcers remains an urgent priority. Several different factors related to the pathogenesis of NSAID-induced small intestinal ulcers have been reported [6–8], such as decreased mucosal mucus [9] and blood flow [10, 11]; infiltration of inflammatory cells [12], intestinal bacteria [13, 14], and bile acids [15]; dietary fibers [16]; and increased intestinal motility [17, 18].
Recently, we reported that dietary fibers (DFs) such as cellulose and intestinal hypermotility both play an important role in the formation of small intestinal lesions induced by indomethacin (IND) in cats [19]. In that experiment, supplementation of canned food with cellulose (insoluble DF; IDF) led to an increase in intestinal lesions induced by IND, while the addition of pectin (soluble DF; SDF) decreased lesion formation. These results suggest that IDFs and SDFs play vastly different roles in the pathogenesis of NSAID-induced small intestinal ulcers, i.e., SDFs, unlike IDFs, may protect the small intestine against NSAID-induced mucosal damage. In the present study, we investigated this possibility further examining the effects of various SDFs on the formation of small intestinal lesions induced by NSAIDs (IND and flunixin), and comparing them with the effects of misoprostol and mucin extracted from pig stomach. We found that pectin, guar gum, polydextrose, misoprostol and mucin all prevented lesion formation. To elucidate the mechanism of protection by SDFs, we examined the viscosity of the SDFs as well as the effect of pectin on GI absorption of IND and IND-induced intestinal hypermotility. The results suggest that SDFs might be a novel and safe means for protecting the small intestine against NSAID-induced intestinal lesions.
Materials and Methods
Experimental procedures were approved by the Animal Welfare Committee, Faculty of Agriculture, Tottori University, Tottori, Japan. In accordance with our institution’s guidelines, we used as few animals as possible in our studies; four or five cats were included per group, and the same data from the control group were used for all ulcer experiments.
Animals
Male and female mongrel cats bred for the experiments in the animal housing facilities of Tottori University were used after feeding for >6 months.
Diets
The animals were given dry food containing a regular amount of DF (RFD-Dry; CANET®, Petline, Gifu, Japan; DF: 2.8%) or canned food containing a low amount of DF (LFD-Can: PRESCRIPTION DIET®, feline i/d can food, Hill’s-Colgate Japan; DF: 0.4%) twice daily between 9–10 a.m. and 5–6 p.m. The amounts of diet given to the animals were based on the manufacturer’s instructions, i.e., 80 g/3 kg b.w. per day for RFD-Dry and 181 g/3 kg b.w. per day for LFD-Can.
Soluble and Insoluble DFs and Mucin
α-Cellulose (IDF, Sigma, St. Louis, MO), guar gum (SDF, Wako, Osaka, Japan), mucin (from pig stomach, Wako), pectin (SDF from citrus, Wako) and polydextrose (SDF synthesized, Wako) were used. Various amounts (0.1–10%, w/w) of α-cellulose, guar gum, pectin, polydextrose or mucin were added to the RFD-Dry or LFD-Can. In most animals, supplementation with DFs or mucin did not affect total food consumption. When an animal stopped consuming the diet during the 3 study days, the experiment was discontinued, and the data were not used.
Drugs
The following drugs were used: flunixin meglumine (Banamine®, Dainippon, Osaka, Japan), indomethacin (Sigma), misoprostol (Cytotec®, Searle), pentobarbital sodium (Nembutal®, Dainippon) and xylazine (Ceractal®, Bayer, Tokyo, Japan). IND was suspended in 1% carboxymethylcellulose (Wako).
Estimation of Mucosal Damage in the GI Tract
Mucosal damage in the GI tract was estimated according to the methods described in our previous report [20]. IND or flunixin was administered orally or subcutaneously just after the morning meal (10 a.m.) once daily for 3 days, and the animals were killed by bleeding from the carotid artery under deep anesthesia with a combination of xylazine (2 mg/kg, i.m.) and sodium pentobarbital (25–50 mg/kg, i.v.) 24 h after the final dosing of IND or flunixin. Then whole GI tract (from esophagus to distal colon) was removed and cut along the longitudinal axis. The GI tract was spread out on paper, and the whole length of the small intestine from the duodenum to the ileum was divided into ten equal-length parts. The first part was regarded as the duodenum, and regions of the small intestine were numbered sequentially from two to ten. The location (corpus, antrum, duodenum or small intestine), grade (erosion or ulcer) and area of mucosal lesions were measured. The grade of “ulcer” was defined as a severe lesion (deep with mucosal detachment), and “erosion” was defined as a superficial or mild lesion. The lesion area (cm2) was obtained from the product of the length and width of the lesions, and the total lesion area (TLA) was obtained as the sum of the areas of individual lesions in each part of the GI tract. Though the duodenum is a part of the small intestine, the TLA in the small intestine was calculated as the sum of the lesion areas in parts two to ten of the small intestine.
Measurement of Viscosity
Each of the SDFs and mucin were dissolved in distilled water at a concentration of 0.1–10%, and the viscosity was measured twice using a viscosimeter (E-type viscosimeter, Tokyo-Keiki, Tokyo, Japan) at room temperature.
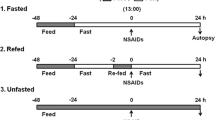
Effect of Pectin on the Gastrointestinal Absorption of IND
A 10% solution of pectin solution (4 ml/kg, corresponding to the 3% pectin in the RFD-Dry) dissolved in water was administered orally to the animals after they had been fasted for 16 h. One hour later, IND (3 mg/kg, p.o.) was administered, and blood samples were collected before and at 0.5, 1, 2 and 4 h after the administration of IND. Concentrations of IND in plasma were measured by HPLC (Type L6200, Hitachi, Japan). The column used for the analysis was an Asahipak ODS-3 (4.6 mm ID × 250 ml, Asahi Kasei Kogyo, Japan). The mobile phase buffer consisted of 45:55 (v/v) 0.1% phosphate/acetonitrile and was delivered at a flow rate of 1.0 ml/min. Plasma sample or standard solution (20 μl) was injected onto the column, which was maintained at 40°C, and absorbance was measured at a detection wave length of 300 nm.
Recording of GI Motility
GI motility was recorded according to the methods described in our previous report [19]. Briefly, under abdominal surgery, a strain-gauge force transducer (size 8 × 5 mm, F-08IS-P, Star Medical, Tokyo, Japan) was sutured onto the serosal surface of the ileum (30 cm proximal to the ileo-cecum junction) to enable measurement of the contractile force of the circular muscle. Changes in ileal contractile activity were then recorded continuously on a personal computer (Dell Inspiron 2200), linked to a receiver (IMT-40RA, Star Medical) using a telemetry system (Model GTS-400, Star Medical).
Statistical Analysis
All data are expressed as mean ± SEM. Differences between groups were analyzed by Student’s t-test for two-group comparisons or analysis of variance (Dunnett’s multiple range test) if more than two variables were considered, with the significance level set at P < 0.05.
Results
Effect of Various SDFs, Mucin and Misoprostol on the Formation of Lesions Induced by IND in the Duodenum and Small Intestine
IND given after feeding of RFD-Dry caused lesions in the duodenum and lower half of the small intestine (Fig. 1a). The TLAs of the duodenum and small intestine were 0.8 ± 0.2 and 7.5 ± 2.6 cm2 (n = 4), respectively (Fig. 2a). The addition of pectin (1, 3 and 10%, w/w) to RFD-Dry markedly inhibited lesion formation in both the duodenum and small intestine in a concentration-dependent manner (Figs. 1b, 2a). The inhibitory effects were stronger in the small intestine than in the duodenum. The TLAs of the small intestine in the groups given 1, 3 and 10% pectin were 1.9 ± 0.9, 0.6 ± 0.3 and 0.0 ± 0.0 cm2 (n = 4), respectively. The effect of pectin on the small intestine was significant (P < 0.05) even at the lowest concentration of 1% (Fig. 2a). Pectin also decreased the TLAs of the duodenum, although the effect was not statistically significant (P > 0.05). However, 10% pectin significantly (P < 0.05) decreased the total area of ulcers, i.e., the areas were 0.6 ± 0.2 cm2 (control) and 0.1 ± 0.0 cm2 (10% pectin) (n = 4), respectively.
Effect of pectin on IND-induced GI lesions. IND (3 mg/kg) was administered orally just after feeding of RDF-Dry (a) or RFD-Dry supplemented with 3% pectin (b), once daily for 3 days; GI lesions were examined 24 h after the final dose of IND. C Gastric corpus, A gastric antrum, D duodenum. Small intestine was numbered sequentially from two (upper) to ten (lower). Data show the mean ± SEM lesion areas of each part of the GI mucosa for four animals per group
Effect of SDFs and mucin on the formation of lesions induced by IND in the duodenum and small intestine. Pectin (1–10%) (a), guar gum (0.1–3%), polydextrose (3%) or mucin (3%) (b) was added to RFD-Dry. Data show the mean ± SEM values of four animals per group. a: P < 0.05, b: P < 0.01 (Dunnett’s test) versus control
The effects of other soluble DFs (guar gum and polydextrose) and mucin on lesion formation were also examined. In these experiments, the cats received RFD-Dry supplemented with guar gum, polydextrose or mucin at concentrations of 0.1–3% (w/w). The addition of SDFs or mucin prevented lesion formation in both the duodenum and small intestine (Fig. 2b). The inhibitory effects were stronger in the small intestine than in the duodenum. Guar gum, even at low concentrations (0.1 and 0.3%), significantly inhibited intestinal lesion formation. The TLAs of the small intestine in the group given guar gum (0.1, 0.3 and 3%) were 0.8 ± 0.2, 0.4 ± 0.2 and 0.0 ± 0.0 cm2 (n = 4), respectively. The TLAs of the small intestine in the group given polydextrose (3%) and mucin (3%) were 1.3 ± 0.8 and 1.6 ± 0.5 cm2 (n = 4), respectively. These TLAs were significantly (P < 0.05) smaller than that of the control group (Fig. 2b). The inhibitory effects of SDFs on the duodenum were not significant (P > 0.05), but lesion formation was decreased significantly (P < 0.05) by mucin; i.e., the TLA in the group given mucin was 0.1 ± 0.1 cm2 (n = 4).
The effect of misoprostol on lesion formation was also examined. In this study, misoprostol (3 μg/kg) was administered orally just before feeding of RFD-Dry twice daily for 3 days. Misoprostol significantly (P < 0.05) inhibited the lesion formation in both the duodenum and small intestine. The TLAs were 0.0 ± 0.0 and 0.8 ± 0.6 cm2 (n = 4), respectively.
Effects of Pectin on Lesion Formation Caused by Cellulose and IND in the Small Intestine
In a previous study [19], we reported that IND (3 mg/kg, p.o.) caused mild lesions in the small intestine of cats that consumed a low-fiber diet (LFD-Can, DF: 0.4%) and that the addition of cellulose to LFD-Can increased lesion formation in the small intestine. In this study, we examined the effect of pectin on lesion formation caused by cellulose and IND. As shown in Fig. 3a (data from our previous report [19] were used as a control for the response to cellulose), the addition of cellulose (3 or 6%) to LFD-Can increased lesion formation in a concentration-dependent manner. The TLAs of the small intestine in the groups fed 3 and 6% cellulose were 4.5 ± 2.3 and 12.1 ± 3.6 cm2 (n = 4), respectively. To examine the effects of pectin on lesion formation caused by cellulose and IND, modified diets consisting of LFD-Can supplemented with cellulose (3 or 6%) and pectin (3%) were used. Addition of pectin to the diet markedly decreased lesion formation in the small intestine (Fig. 3b). The TLAs of the small intestine in the group given 3% pectin with 3 or 6% cellulose were 0.0 ± 0.0 and 0.2 ± 0.0 cm2 (P < 0.05; n = 4 per group), respectively.
Effects of cellulose and pectin on the formation of small intestinal lesions induced by IND. The animals were given LDF-can supplemented with cellulose (0–6%) (a), or cellulose (0–6%) and pectin (3%) (b). Data show the mean ± SEM values for four animals per group. Data from our previous report [19] were used as a control for the response to cellulose (a). c: P < 0.05 (Student’s t-test) versus cellulose (6%)
Effects of Pectin on GI Lesion Formation Induced by Flunixin Given S.C.
The effects of pectin on GI lesions induced by flunixin, an NSAID that non-selectively inhibits cyclooxygenase (COX), were examined. Flunixin (1 mg/kg) was given subcutaneously just after feeding of RFD-Dry in the morning once daily for 3 days. As was observed following IND administration, flunixin caused lesions in the duodenum and lower half of the small intestine (Fig 4a). The TLAs of the duodenum and small intestine were 0.4 ± 0.1 and 5.4 ± 1.7 cm2 (n = 4), respectively. Addition of pectin (3%, w/w) to RFD-Dry markedly inhibited lesion formation in the small intestine (Fig 4b). The TLA of the small intestine in the group given 3% pectin was 0.2 ± 0.1 cm2 (n = 4, P < 0.05).
Viscosity of SDFs and Mucin
The viscosity of the SDFs and mucin (0.03–30%) increased in a concentration-dependent manner and was highest for guar gum, followed by pectin, mucin, and polydextrose (Fig 5). The viscosity (mPa-S) of guar gum, pectin, polydextrose, and mucin (all at a concentration of 3%) was >1,200, 414, 1, and 4, respectively.
Effect of Pectin on GI Absorption of IND
When IND (3 mg/kg) was administered orally after a 16-h fast, the plasma concentration of IND increased rapidly and reached a maximum at 30 min after administration; the concentration gradually decreased over the following 4-h period (Fig. 6). To investigate the effect of pectin on GI absorption of IND, 10% pectin solution (4 ml/kg, p.o.) was administered 1 h before IND administration. As shown in Fig. 6, the administration of pectin did not affect the time-dependent changes in plasma concentrations of IND. In the respective groups given vehicle and pectin, the T max (h) was reached at 0.5 h in both groups; C max (μg/ml) was 4.6 ± 1.2 and 3.6 ± 0.1 μg/ml; T 1/2 (h) was 1.3 h and 1.9 h; AUC(0–4 h) was 6.4 ± 0.8 (n = 5) and 7.1 ± 1.3 (n = 5) μg × h/ml.
Effect of pectin on the gastrointestinal absorption of IND. IND (3 mg/kg) was administered orally 1 h after the administration of vehicle (○: water) or pectin (●: 4 ml/kg of 10% pectin solution). Plasma concentrations of IND were measured using HPLC. Data show the mean ± SEM values of five animals per group
Effect of Pectin and Misoprostol on IND-Induced Hypermotility in the Ileum
Consistent with the results of our previous report [19], IND (3 mg/kg) administered orally after consumption of RFD-Dry markedly increased ileal motility (Fig. 7b). The inclusion of pectin (3%) in the RFD-Dry did not affect the increase in IND-induced ileal motility (Fig. 7c). Misoprostol (3 μg/kg, p.o.) given just before feeding of RFD-Dry markedly prevented the increase of motility induced by IND (Fig. 7d).
Discussion
Dietary fibers are classified according to their physicochemical properties as soluble or insoluble. It is well known that IDFs such as cellulose will increase in volume by absorbing water and will stimulate intestinal motility by distending the intestinal wall, whereas SDFs such as pectin are highly water soluble and make viscous solutions (gel) that facilitate the smooth transit of food from the upper to the lower intestine [20, 21]. Recently, we reported that IDFs play an important role in the formation of lesions in the small intestine induced by IND in cats. In the present study, we examined the role of SDFs in NSAID-induced small intestinal ulcers in cats and found that the addition of 3% SDFs (i.e., pectin, guar gum, or polydextrose) to regular-fiber diets (RFD-Dry, DF: 2.8%) significantly decreased IND-induced intestinal lesion formation. The inhibitory effects were observed at very low concentrations of guar gum (0.1%) and pectin (1%), and they increased in a concentration-dependent manner. Pectin (3%) also markedly decreased the formation of small intestinal lesions in response to the administration of flunixin, a non-selective COX inhibitor that is used therapeutically in animals. These results suggest that SDFs, in contrast with IDFs, protect the small intestine against NSAID-induced mucosal damage.
In addition, the aggravation of IND-induced small intestinal lesions due to the inclusion of cellulose (3 and 6%) in low-fiber diets (LFD-Can, DF: 0.4%) was markedly inhibited by dietary supplementation with 3% pectin. These results suggest that the protective action of pectin on the mucosa may be related to the same mechanism by which cellulose promotes lesion formation. There are several possible mechanisms that could account for the ability of SDFs to protect the mucosa and prevent the formation of NSAID-induced small intestinal lesions. The first possibility is that soluble DFs protect the mucosa as a result of their physicochemical properties; i.e., their viscosity. Like the SDFs, 3% mucin (extracted from pig stomach) also decreased IND-induced intestinal lesions. SDFs and mucin have similar polysaccharide structures, are viscous, and form gels when dissolved in water. We found that the viscosity of all the SDFs and mucin increased in a concentration-dependent manner. There was also a good correlation between viscosity and the protective action of SDFs on the mucosa, i.e., guar gum was the most viscous, followed by pectin, mucin, and polydextrose, and the same relationship order was observed with respect to their protective effects on the mucosa (i.e., guar gum > pectin > mucin ≥ polydextrose). Kunikata et al. [9] reported that IND decreased mucus production in the small intestine of rats, whereas PGE2 increased mucus production and prevented IND-induced small intestinal lesion formation. In the present study in cats, misoprostol (PGE1 derivative) markedly inhibited the lesion formation in the small intestine caused by IND. These results suggest that mucin plays an important role in the protection of the small intestine against NSAID-induced mucosal damage. SDFs may cover the surface of the mucosa and compensate for the loss of mucin’s barrier function caused by IND, thereby protecting the mucosa from aggravating factors such as intestinal bacteria [13, 14] and bile acids [15]. It remains unclear whether SDFs distribute equally on the surface of the intestinal mucosa. In this study, limpid and viscous liquid layers were often observed on wide areas of the mucosal surface of the small intestine in cats fed pectin or guar gum. However, further studies on the distribution of SDFs on the surface of the small intestinal mucosa will be needed to confirm this finding. The results of the present study suggest that soluble DFs and mucin are effective for protection of the intestinal mucosa against NSAID-induced damage. It is unlikely that SDFs protect the intestinal mucosa by increasing the secretion/production of mucin stimulated by prostaglandins, because IND, a strong COX inhibitor, was administered during the experiments for 3 consecutive days.
It is well known that SDFs prevent the absorption of various substances such as bile acids, cholesterol, and glucose [22, 23]. Therefore, as another possible mechanism, SDFs may prevent lesion formation by decreasing the rate of NSAID absorption from the GI tract. To investigate this possibility, we examined the effects of pectin on GI absorption of IND by measuring the plasma concentration of IND after oral administration. The results showed that pectin did not affect the absorption of IND from the GI tract. This was supported by our finding that the formation of small intestinal lesions caused by parenteral (s.c.) administration of a non-selective COX inhibitor (flunixin) was also markedly inhibited by the addition of pectin to the diet. We also found that in rats with adjuvant-induced arthritis, the addition of 10% pectin or guar gum to the rat chow diet markedly decreased the induction of intestinal lesions by IND (10 mg/kg/day, p.o., for 3 days) without affecting the anti-inflammatory (anti-edema) effect of IND (H. Satoh, unpublished observation). These data suggest that it is unlikely that SDFs inhibit intestinal lesion formation by preventing the absorption of NSAIDs from the GI tract; i.e., SDFs can prevent the intestinal side effects of NSAIDs without affecting their anti-inflammatory effects.
Intestinal bacteria and bile acids have been postulated to play a role in the pathogenesis of small intestinal ulcers induced by IND [13–15, 24]. We previously reported that antibiotics (neomycin and erythromycin) and a bile acid-absorbing resin (cholestyramine) prevented the induction of intestinal lesions by IND in cats [19]. Since SDFs can inhibit the diffusion of many substances [22, 23], it is possible that SDFs decrease NSAID-induced small intestinal lesions by preventing the infiltration of intestinal bacteria and bile acids into the mucosa—a possibility that warrants further investigation in future studies.
Takeuchi et al. [17, 18] reported that intestinal hypermotility plays an important role in the formation of NSAID-induced small intestinal lesions in rats. In a previous report [19], we suggested that indigestible solid components of food, such as IDFs, together with NSAID-induced intestinal hypermotility may cause damage to the surface of the intestinal mucosa when mucus is decreased. The effects of SDFs on GI motility have been studied in relation to glucose absorption, since it is well known that SDFs often cause glucose flattering [21, 23]. There have been conflicting reports on the effect of SDFs on GI motility; i.e., SDFs have been shown in some studies to stimulate GI motility in humans [25], dogs [20], and pigs [26], whereas other studies have shown no effect on motility in humans [27] and dogs [21]. We examined the effect of pectin and misoprostol on ileal hypermotility caused by IND. IND administered after feeding markedly increased the motility of the ileum in the areas where mucosal lesions were observed. The increase in motility was markedly prevented by misoprostol, but not affected by the addition of pectin (3%) to the diet. These results indicate that soluble DFs do not prevent NSAID-induced intestinal lesions by inhibiting intestinal motility.
There are currently no effective approved agents for the prevention of the ulcerogenic effects of NSAIDs on the small intestine in humans. The results of the present study revealed that the addition of small amounts of SDFs to the diet prevented the induction of small intestinal lesions by NSAIDs. Therefore, we conclude that SDFs seem to be useful agents for preventing the side effects of NSAIDs on the small intestine without affecting their anti-inflammatory effects. The viscosity of SDFs may play a role, at least in part, in their protective effects on the small intestine.
References
Chutkan R, Toubia N. Effect of nonsteroidal anti-inflammatory drugs on the gastrointestinal tract: diagnosis by wireless capsule endoscopy. Gastrointest Endosc Clin N Am. 2004;14:67–85.
Fortun PJ, Hawkey CJ. Nonsteroidal anti-inflammatory drugs and the small intestine. Curr Opin Gastroenterol. 2007;23:134–141.
Goldstein JL, Eisen GM, Lewis B, Gralnek IM, Zlotnick S, Fort JG. Video capsule endoscopy to prospectively assess small bowel injury with celecoxib, naproxen plus omeprazole, and placebo. Clin Gastroenterol Hepatol. 2005;3:133–141.
Laine L, Connors LG, Reicin A, et al. Serious lower gastrointestinal clinical events with nonselective NSAID or coxib use. Gastroenterology. 2003;124:288–292.
Maiden L, Thjodleifsson B, Theodors A, Gonzalez J, Bjarnason I. A quantitative analysis of NSAID-induced small bowel pathology by capsule enteroscopy. Gastroenterology. 2005;128:1172–1178.
Lanas Á, Scarpignato C. Microbial flora in NSAID-induced intestinal damage: a role for antibiotics? Digestion. 2006;73(suppl 1):136–150.
Wallace JL. Nonsteroidal anti-inflammatory drugs and gastroenteropathy: the second hundred years. Gastroenterology. 1997;112:1000–1016.
Whittle BRJ. Mechanisms underlying intestinal injury induced by anti- inflammatory COX inhibitors. Eur J Pharmacol. 2004;500:427–439.
Kunikata T, Tanaka A, Miyazawa T, Kato S, Takeuchi K. 16, 16-Dimethyl prostaglandin E2 inhibits indomethacin-induced small intestinal lesions through EP3 and EP4 receptors. Dig Dis Sci. 2002;47:894–904.
Anthony A, Pounder RE, Dhillon AP, Wakefield AJ. Vascular anatomy defines site of indomethacin induced jejunal ulceration along the mesenteric margin. Gut. 1997;41:763–770.
Miura S, Suematsu M, Tanaka S, et al. Microcirculatory disturbance in indomethacin-induced intestinal ulcer. Am J Physiol. 1991;261:G213–G219.
Asako H, Kubes P, Wallace J, Gaginella T, Wolf RE. Indomethacin-induced leukocyte adhesion in mesenteric venules: role of lipoxygenase products. Am J Physiol. 1992;262:G903–G908.
Robert A, Asano T. Resistance of germfree rats to indomethacin-induced intestinal lesions. Prostaglandins. 1977;14:333–341.
Satoh H, Guth PH, Grossman MI. Role of food in gastrointestinal ulceration produced by indomethacin in the rat. Gastroenterology. 1982;83:210–215.
Ishihara Y, Okabe S. Effects of cholestyramine and synthetic hydrotalcite on acute gastric or intestinal lesion formation in rats and dogs. Dig Dis Sci. 1981;26:553–560.
Satoh H, Guth PH, Grossman MI. Role of bacteria in gastric ulceration produced by indomethacin in the rat: cytoprotective action of antibiotics. Gastroenterology. 1983;84:483–489.
Takeuchi K, Miyazawa T, Tanaka A, Kato S, Kunikata T. Pathogenic importance of intestinal hypermotility in NSAID-induced small intestinal damage in rats. Digestion. 2002;66:30–41.
Tanaka A, Matsumoto M, Hayashi Y, Takeuchi K. Functional mechanism underlying cycloxygenase-2 expression in rat small intestine following administration of indomethacin: relation to intestinal hypermotility. J Gastroenterol Hepatol. 2005;20:38–45.
Satoh H, Shiotani S, Otsuka N, Hato K, Nishimura S. Role of dietary fibers, intestinal hypermotility and leukotrienes in the pathogenesis of NSAID-induced small intestinal ulcers in cats. Gut (in press).
Bueno L, Praddaude F, Fioramonti J, Ruckebusch Y. Effect of dietary fiber on gastrointestinal motility and jejunal transit time in dogs. Gastroenterology. 1981;80:701–707.
Xu X, Brining D, Rafiq A, Hayes J, Chen J. Effects of enhanced viscosity on canine gastric and intestinal motility. J Gastroenterol Hepatol. 2005;20:387–394.
Ebihara K, Maduhara R, Kiriyama S. Major determinants of plasma glucose-flattening activity of a water-soluble dietary fiber: effects of Konjak mannan on gastric emptying and intraluminal glucose-diffusion. Nutr Rep Int. 1981;23:1145–1156.
Jenkins DJA, Wolever TMS, Leeds AR, et al. Dietary fibres, fibre analogues, and glucose tolerance: importance of viscosity. Br Med J. 1978;1:1392–1394.
Reuter BK, Davies NM, Wallace JL. Nonsteroidal anti-inflammatory drug enteropathy in rats: role of permeability, bacteria, and enterohepatic circulation. Gastroenterology. 1997;112:109–117.
Shimoyama Y, Kusano M, Kawamura O, et al. High-viscosity liquid meal accelerates gastric emptying. Neurogastroenterol Motil. 2007;19:879–886.
Cherbut C, Albina E, Champ M, Doublier JL, Lecannu G. Action of guar gum on the viscosity of digestive contents and on the gastrointestinal motor function in pigs. Digestion. 1990;46:205–213.
Schönfeld JV, Evans DF, Wingate DL. Effect of viscous fiber (guar) on postprandial motor activity in human small bowel. Dig Dis Sci. 1997;42:1613–1617.
Acknowledgments
The authors wish to thank Dr. M. Morimoto of Research Center for Bioscience and Technology, Tottori University, and Dr. S. Nakamura of Research Division, Ophtecs, Japan, for their useful advices on the viscosity studies and pharmacokinetic studies. We are greatly indebted to Dr. Y. Akiba (CURE/UCLA & BBRI, Los Angeles, California) for providing valuable discussion and suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Satoh, H., Hara, T., Murakawa, D. et al. Soluble Dietary Fiber Protects Against Nonsteroidal Anti-inflammatory Drug-Induced Damage to the Small Intestine in Cats. Dig Dis Sci 55, 1264–1271 (2010). https://doi.org/10.1007/s10620-009-0893-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0893-2