Abstract
Purpose
Gastric atrophy is a premalignant condition. The aim of this study was to evaluate the correlation between histological and endoscopic findings of atrophy, and to analyze the affecting factors.
Methods
Atrophy was graded by endoscopy, and biopsy was performed in the antrum and body for the diagnosis of atrophy according to the Sydney system in the 1,330 subjects.
Results
Both endoscopic and histological atrophy increased in proportion to age (P < 0.001). The prevalence of endoscopic atrophy was significantly lower than that of histological atrophy especially below 50 years of age. The sensitivity and specificity of endoscopy for the diagnosis of atrophy based on histological diagnosis of atrophy were 61.5 and 57.7% in the antrum, and were 46.8 and 76.4% in the body of the stomach. Multivariate analysis showed that an age <50 (OR 0.38, 95% CI 0.25–0.61) and a PG I/II ratio >3 (OR 0.50, 95% CI 0.35–0.71) in the antrum, and an age < 50 (OR 0.43, 95% CI 0.19–1.00) and a CRP > 5 mg/dl (OR 0.53, 95% CI 0.30–0.94) decreased the sensitivity of the endoscopic diagnosis of atrophy in the body.
Conclusions
A high index of suspicion of gastric atrophy is important in the young age group, and confirmation of the diagnosis by histology is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Correa hypothesis postulates that carcinogenesis occurs as a progression from chronic gastritis to gastric atrophy and intestinal metaplasia (IM), then to dysplasia, and finally to cancer [1]. Thus, gastric atrophy has been regarded as a precancerous condition [2, 3]. Most cases of gastric atrophy are associated with Helicobacter pylori (H. pylori) infection, and H. pylori is regarded as an important cause of chronic atrophic gastritis [4–6]. The diagnosis of gastric atrophy is usually performed by histology [7]. However, endoscopists usually encounter the various endoscopic appearances of the gastric mucosa in their common practice [8] and attempts to classify the gastritis are made during a gastroscopy [9]. Such changes are known to be related to the histomorphology and presence of H. pylori in the general population [10]. Research regarding the concordance between the findings of endoscopy and histology in cases with gastritis has been made, but the outcomes showed a kind of disappointing correlation [11–15]. However, in general, the concordance was good in the severe forms of gastritis and normal endoscopy has excluded active gastritis [11–17].
The prevalence of gastric cancer is unacceptably high in Korea; the age-standardized incidence of gastric cancer during 1990–2001 in South Korea, as determined by the Cancer Registry at the Korean National Cancer Center in 2002, was 65.6 per 100,000 person years for men and 25.8 for women [18]. A health check-up program designed to detect gastric cancer was implemented by the Korean government in 2001 for biannual evaluation of Korean citizens above 40 years old. Histological studies of gastroscopy biopsies are regarded as the gold standard for diagnosing gastric atrophy [19]. However, the invasive nature of this method precludes its use for population screening. Moreover, histological biopsy cannot be performed during every gastroscopy. Thus, usually biopsy is performed when atrophy is suspected endoscopically. From this background it is very important to know the correlation between the endoscopic findings and histological gastritis. However, systemic trial has not been performed in Korea, which has a high prevalence of gastric cancer [18] and a high seroprevalence of H. pylori, 59.6% among asymptomatic Korean adults in 2005 [20]. Therefore, the goal of this study was to evaluate the sensitivity and specificity of the endoscopic diagnosis of atrophy, and to analyze the factors associated with the diagnosis.
Subjects and Methods
Study Population
Our study included 1,333 consecutively enrolled subjects who visited Seoul National University Bundang Hospital for gastroscopy from September 2003 to March 2007. Approximately 50% of the subjects had gastrointestinal symptoms such as epigastric pain, epigastric discomfort, epigastric soreness, bloating, or indigestion within 3 months of presentation. They requested gastroscopy with H. pylori testing for gastric cancer screening. The subjects were categorized into five groups (a control group and four different disease groups). The control group consisted of subjects who had only mild gastritis or had a normal gastroscopy without any evidence of significant gastroduodenal disease. The four disease groups included: duodenal ulcer (DU), benign gastric ulcer (BGU), dysplasia, and gastric cancer; these groups were categorized according to the gastroscopy and histological diagnoses. Patients with a history of any stomach surgery, H. pylori eradication therapy or systemic diseases that required medication for a long period of time, or patients who took proton pump inhibitors within 2 weeks were excluded from the study. The Institutional Review Board at Seoul National University Bundang Hospital approved this study, and written informed consent was obtained from all participants.
Endoscopic Examinations
The patients in this study were informed to fast for at least 6 h before the endoscopic procedure began. The gastroscopy was performed using GIF-Q260 (Olympus Co., Tokyo, Japan) after local pharyngeal anesthesia was provided using lidocaine spray (Xylocaine). Some patients demanded sedation and received 3–4 mg of intravenous midazolam. All endoscopic investigations were performed by a single highly experienced endoscopist (N. K.), and the findings were described according to the global impression on the presence of gastritis in the antrum and in the body of the stomach. The presence of gastric atrophy was decided by the well visualization of the submucosal vessel due to thinning of mucosa in the antrum and in the body, respectively.
Histological Examination and Helicobacter pylori Tests
To determine the presence of current H. pylori infection, ten biopsy specimens were taken for three types of H. pylori testing (histology, the CLOtest and culture). Two biopsy specimens were taken from the greater curvature of both the antrum and the body of the stomach, respectively, and three from both the lesser curvature of the antrum and body, respectively (Fig. 1). Among the ten specimens, two from the antrum and two from the body were fixed in formalin, and assessed for the presence of H. pylori (by modified Giemsa staining). Moreover, the degree of inflammatory cell infiltration (activity and chronic inflammation), atrophy (loss of appropriate glands), and metaplasia were determined by hematoxylin & eosin (H&E) staining by averaging the score of the biopsy specimens from the greater and lesser curvature of the stomach. The histological features of the gastric mucosa were recorded using the updated Sydney scoring system (i.e., 0 = none, 1 = slight, 2 = moderate, and 3 = marked) [21]. All biopsies were examined independently by two experienced pathologists (H.S.L and H.E.L), who were unaware of the clinical details. In the event of disagreement, the biopsies were re-examined by these two pathologists until agreement was reached. When the specimens were not prepared well enough to correctly evaluate the full-thickness gastric mucosa due to problems such as improper fixation, inaccurate orientation, and inappropriate sections, or whenever inflammation prevented a clear distinction between non atrophic and atrophic phenotypes these samples were classified as indefinite for atrophy [7] and excluded from the enrollment in the present study.
The description of the biopsy sites. Histology and culture were performed on the two specimens from each of A and C each from the antrum, and two specimens B and D each from body, respectively. In addition, rapid urease testing was performed, with one specimen each from C and D. A the greater curvature of mid antrum; B the greater curvature of mid body; C the lesser curvature of mid antrum; D the lesser curvature of mid body
One specimen from each, the lesser curvature of the antrum and the body (Fig. 1), was used for rapid urease testing (CLOtest, Delta West, Bentley, Australia). Two specimens from the antrum and body were used for culture (Fig. 1). The antral and body biopsy specimens were evaluated separately; organisms were identified as H. pylori by Gram staining, colony morphology, and positive oxidase, catalase, and urease reactions [22]. If any one of these three H. pylori tests were positive, the host was regarded as having an on-going H. pylori infection.
Serum Pepsinogen Levels and Biochemistry
Fasting serum was collected from all subjects at the study entry. The samples were centrifuged immediately at 4°C and stored at −70°C until used. Serum concentrations of pepsinogen I and II were measured using a latex-enhanced turbidimetric immunoassay (L-TIA) (HBi Corp, Seoul, Korea, imported from Shima Laboratories, Tokyo, Japan), and PG I to PG II ratios (PG I/II) were calculated. In addition, the plasma C-reactive protein (CRP), hemoglobin, and serum albumin were measured.
Statistical Analysis
All statistical analyses were performed with SPSS software (version 12.0, SPSS Inc., Chicago, IL, USA). The effects of age, gender, H. pylori infection, gastroduodenal diseases, smoking, alcohol, and serum pepsinogen I/II levels on the sensitivity of the endoscopic diagnosis of atrophy in the antrum and in the body of the stomach were expressed as odds ratios (ORs) with 95% confidence intervals (CI). Covariates that showed a significant association by the Chi-square test were subjected to multiple logistic regression analyses. Model fit was assessed using Hosmer-Lemeshow goodness-of-fit tests. Variables found to be significant were included in the final models. A P-value < 0.05 was regarded as statistically significant.
Results
Demographic Data
The 1,330 registered subjects were all from the Korean population. The groups included the controls (n = 321), patients with DU (n = 146), BGU (n = 171), cancer (n = 543) and dysplasia (n = 149). All the subjects were ethnic Koreans. The mean age was 57.7 years (779 male and 551 female). There were 1,107 (83.2%) out of the 1,330 patients that were H. pylori-positive, and 223 (16.8%) were H. pylori-negative. Table 1 shows the baseline characteristics of the enrolled patients. Patients in their 50s (24.4%) or 60s (31.2%) accounted for most of the subjects. H. pylori positivity findings were significantly higher in the male gender (P = 0.003), smokers (P = 0.005), and patients with gastric disease (P < 0.001). Mean levels of serum pepsinogen I (sPG I; P < 0.001) and sPG II (P < 0.001) were higher, and the sPG I/II ratio (P < 0.001) was lower, in the H. pylori-positive compared to the H. pylori-negative group. However, there were no significant differences of alcohol ingestion, serum CRP, albumin, and hemoglobin levels depending on H. pylori positive findings.
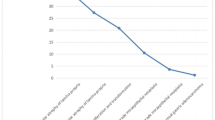
When endoscopic atrophy was analyzed according to age atrophy significantly increased in proportional to age in the antrum as well as in the body (P < 0.001; Fig. 2a). Similar to endoscopic atrophy, the prevalence of histological atrophy, which was found in both of the antrum and the body, significantly increased in proportion to age (P < 0.001; Fig. 2b). However, the prevalence of histological atrophy, which was found only in the body, did not change depending on age.
The histologic findings showed higher activity and chronic inflammation grades in H. pylori-positive subjects compared to the H. pylori-negative subjects in both samples form the antrum and the body of the stomach (Table 2). In addition, the prevalence of atrophy and intestinal metaplasia was higher in H. pylori-positive subjects compared to the H. pylori-negative subjects in both of the antrum and the body of the stomach (Table 2).
Detection Rates of Atrophy by Endoscopic Findings in the Antrum
The sensitivity and specificity of the endoscopic diagnosis of atrophy were calculated based on the histological confirmation of atrophy. The sensitivity and specificity of endoscopic antral atrophy based on histological atrophy regardless of IM were found to be 61.5% (466/758) and 57.7% (328/568), respectively (Table 3). When the sensitivity and specificity of endoscopic antral atrophy were calculated based on atrophy without IM the sensitivity and specificity were found to be 40.0% (78/195) and 66.5% (286/430), respectively (Table 3). When the sensitivity and specificity of endoscopic antral atrophy were calculated based on atrophy with IM the sensitivity and specificity were found to be 68.9% (388/563) and 30.4% (42/138), respectively (Table 3). The sensitivity of the endoscopic diagnosis of atrophy in the antrum was significantly higher in cases of atrophy with IM (68.9%) than in the atrophy without IM (40.0%; P < 0.001).
To identify the factors that affect the sensitivity of the endoscopic diagnosis of atrophy in the antrum, univariate analysis was performed for the age, gender, H. pylori infection, smoking, alcohol, gastroduodenal diseases, hemoglobin, CRP, albumin, and PG I/II ratios. An age younger than 50 years (P < 0.001), female (P = 0.009), non-smokers (P = 0.003), non-alcoholics (P = 0.042), gastric pathology (P < 0.001), and high pepsinogen I/II ratio (P = 0.002) were associated with decreased endoscopic sensitivity. However, there was no association of H. pylori positivity, hemoglobin levels, CRP, or albumin levels with the endoscopic diagnosis of atrophy. The mean level of serum PG I was higher in the group with endoscopically negative results (62.6 ng/ml) compared to the endoscope-positive group (56.2 ng/ml; P < 0.001). However, there was no significant difference in case of PG II with regard to endoscope-negative (17.9 ng/ml) or endoscope-positive (19.2 ng/ml) results. Multivariate analysis showed that two factors, the young age (<50 years; OR 0.38, 95% CI 0.25–0.61) and the pepsinogen I/II ratio >3 (OR 0.50, 95% CI 0.35–0.71), were associated with decreased sensitivity of endoscopic diagnosis of atrophy in the antrum (Table 5).
Detection Rates of Atrophy by Endoscopic Findings in the Body
The sensitivity and specificity for endoscopic atrophy in the body regardless of IM were found to be 46.8% (238/509) and 76.4% (625/818), respectively (Table 3). When the sensitivity and specificity of endoscopic body atrophy were calculated based on atrophy without IM the sensitivity and specificity were found to be 32.8% (38/116) and 79.7% (580/728), respectively (Table 4). When the sensitivity and specificity of endoscopic antral atrophy were calculated based on atrophy with IM the sensitivity and specificity were found to be 50.9% (200/393) and 50.0% (45/90), respectively (Table 4). Similar to antrum, the sensitivity of the endoscopic diagnosis of atrophy in the body was also significantly higher in cases of atrophy with IM (50.9%) than in the atrophy without IM (32.8%; P < 0.001).
The factors associated with the sensitivity of endoscopic atrophy in the body were analyzed, similar to the data from the antrum. In the univariate analysis, an age younger than 50 years (P < 0.001), female (P = 0.002), non-smokers (P = 0.008), non-alcoholics (P = 0.001), gastric pathology (P < 0.001), hemoglobin level ≤12.5 g/dl (P = 0.013), CRP level >5 mg/dl (P = 0.030), and albumin level ≤4.0 g/dl (P = 0.022) were associated with decreased endoscopic sensitivity. However, there was no effect of H. pylori positivity and serum PG I or II levels on the endoscopic diagnosis of atrophy. The multivariate analysis showed that the young age (<50 years; OR 0.43, 95% CI 0.19–1.00) and a CRP level >5 mg/dl (OR 0.53, 95% CI 0.30–0.94) decreased the sensitivity of the endoscopic diagnosis of atrophy in the body of the stomach (Table 5).
Mucosal Inflammation as a Cause of Decreased Sensitivity of Endoscopic Atrophy in the Age Group Below 50 years
An age <50 years was commonly found to be a significant factor associated with decreased sensitivity of the endoscopic diagnosis of atrophy in both the antrum and the body of the stomach. To evaluate whether the gastric mucosal inflammation may be a cause of the decreased sensitivity in the age <50 years group, activity and chronic inflammation were compared between age <50 and ≥50 years cases that were negative for atrophy by endoscopy but positive for atrophy by histology. The mean grades of activity and chronic inflammation for the antrum were higher in the age <50 year group compared to the ≥50 year group (P < 0.001; Fig. 3a, b). By contrast, there was no difference in activity and chronic inflammation between two age groups in cases with atrophy diagnosed by endoscopy that were confirmed by histology.
Differences in the activity (a) and chronic inflammation (b) depending on the age when atrophy was not detected endoscopically in the cases with histological atrophy in the antrum. Similar results were obtained from the body for activity (c) and chronic inflammation according to the Sydney classification (d)
Similar to the antrum, the mean grades of activity for the body were higher in the age <50 year group compared to the ≥50 year group that were negative for atrophy by endoscopy but positive for atrophy by histology (P = 0.038; Fig. 3c). By contrast, there was no difference in activity between two age groups in cases with atrophy diagnosed by endoscopy that were confirmed by histology (Fig. 3c). In case of chronic inflammation there was no difference in the mean grades of between two age groups regardless of endoscopic diagnosis of atrophy (Fig. 3d).
Different Distribution of Histological Atrophic Grade and Serum Pepsinogen I/II Ratio in 758 Subjects Depending on Endoscopic Diagnosis of Atrophy in the Antrum
To evaluate why the serum PG I/II ratio >3 was significantly associated with decreased sensitivity of the endoscopic diagnosis of atrophy in the antrum subjects with histological atrophy in the antrum or in the body were classified according to their PG I/II ratio 3. In the group of subjects with histological atrophy in the antrum (n = 675), the prevalence of a PG I/II ratio >3 was significantly lower in the group with atrophy present by endoscopy (42.6%) than in the group with atrophy absent by endoscopy in the antrum (63.9%; P < 0.001; Table 6). In the group of subjects with histological atrophy in the body (n = 363) the prevalence of a PG I/II ratio >3 was significantly lower in the group with atrophy present by endoscopy (28.4%) than in the group with atrophy absent by endoscopy in the antrum (38.3%) (P = 0.047; Table 6). In the next, atrophic grade was compared between the group with atrophy absent by endoscopy and the group with atrophy present by endoscopy in the antrum based on histological atrophy. The mean grade of histological atrophy in the antrum was significantly higher (1.50) in the group with atrophy present by endoscopy than in the group with atrophy absent by endoscopy (1.38; P = 0.012; Table 6). In addition, the mean grade of histological atrophy in the body was significantly higher (0.99) in the group with atrophy present by endoscopy than in the group with atrophy absent by endoscopy (0.70; P < 0.001; Table 6). This finding also suggests that atrophy was more severe in the group with atrophy present by endoscopy than in the group with atrophy absent by endoscopy.
Discussion
Gastric atrophy and intestinal metaplasia (IM) are regarded as precancerous conditions [3, 6, 23], and thus a precise knowledge of the presence of atrophy and IM is of considerable importance, especially at a young age. Previously, we showed that the mean prevalence of atrophy in the antrum and body of the stomach was found to be 42.5 and 20.1%, respectively, and that the association of H. pylori infection was the most important risk factor of atrophy in Korea [24]. Thus, gastric atrophy is an important condition in Korea, which has a high prevalence of gastric cancer [18] and a high seroprevalence of H. pylori [20]. Previously, a Chinese study reported that H. pylori eradication significantly diminished the development of gastric cancer in a subgroup of H. pylori carriers without precancerous lesions (e.g., gastric atrophy and intestinal metaplasia, or dysplasia) [25]. In addition, a Korean study found that the eradication of H. pylori could not interrupt gastric cancer development in a patient with IM [26]. These findings encapsulate the idea of ‘point of no return’ and suggests that the diagnosis of atrophy or IM is very important, especially in the younger age group.
Theoretically, gastritis detected during endoscopy should be confirmed by histology because the definitions are based on histological findings. However, it is also true that the decision to perform a biopsy at specific sites is determined by the endoscopic findings. A Japanese group found that gastritis extended from the antrum to the body more rapidly one ages, especially in cases with H. pylori infection [27, 28], which are different from the results in Western patients. In Western countries, atrophic gastritis is usually classified as type A or type B (antrum predominant). Type A is autoimmune gastritis and predominantly involved the fundic gland mucosa, and was most predominant along the greater curvature of the fundus and body. In the present study, the prevalence of histologic atrophic gastritis, which was found only in the body but not in the antrum, was constant at 4.0–7.9% regardless of age, confirming that the incidence of pernicious anemia is very low in Korea as well as Japan [27]. In contrast, the prevalence of histologic atrophy, which was found in the antrum as well as in the body, increased from 3.8% (below 30 years) to 44.1% (over 70 years). Korean and Japanese patients have similar ethnic backgrounds and a high prevalence of H. pylori infection as well as gastric cancer. Thus, we attempted to correlate the macroscopic and microscopic findings of atrophy in the antrum and in the body, respectively. The sensitivity and specificity of endoscopic atrophy, based on the histologic diagnosis, were found to be 61.5 and 57.7% in the antrum, and 46.8 and 76.4% in the body of the stomach, respectively. These results suggest that a high index of suspicion for a gastric diagnosis of atrophy is important, and if gastric atrophy is suspected by endoscopy, then histological confirmation is necessary. There is a possibility that the sensitivity of endoscopic diagnosis of atrophy might be increased by using advanced endoscopic techniques such as chromoscopy/magnification/narrow band imaging, which were not used in the present study. However, it takes a long time to perform endoscopy with these techniques and it is not practical for the endoscopists in Korea where routine endoscopy is frequently undertaken just because of gastric cancer screening.
It is now clear that a biopsy specimen from one site in the stomach may not reveal the true extent of gastritis. Furthermore, considerable difficulties persist amongst pathologists in agreement on the assessment of the presence and severity of gastric atrophy [7]. However, in the present study, two biopsies were taken from the greater and lesser curvature of the mid-antrum and mid-body, and all biopsies were examined independently by two experienced pathologists, following the new criteria for classification and grading of gastric mucosal atrophy; the findings have shown a high level of agreement among gastrointestinal pathologists trained in different cultural contexts [7]. Thus, the low concordance rate of atrophy, between macroscopic and microscopic findings might be in a similar line with the disappointing correlation regarding the concordance between endoscopy and histology findings for the diagnosis of gastritis [11–15].
When we comprehensively analyzed the factors associated with this low concordance rate, including age, gender, H. pylori infection, smoking, alcohol, gastroduodenal disease, hemoglobin, CRP, albumin, and PG I/II levels, the age below 50 years was found to be a significant factor associated with the decreased sensitivity of the endoscopic diagnosis of atrophy in both the antrum and the body of the stomach. It might be related to the result that severity of atrophy becomes severe as one gets older, which has also been suggested by the increase of the prevalence of histological atrophy in the present study. Furthermore, when the activity and chronic inflammation grade according to the Sydney classification were compared between the age group <50 and age ≥50 years, both the activity and chronic inflammation in the antrum and body were significantly higher in the age group <50 years than in the age group ≥50 years when endoscopic atrophy was not diagnosed, but was positive for atrophy by histology. However, these differences disappeared in cases with atrophy diagnosed by endoscopy, which were confirmed by histology. These results suggest that the marked inflammatory cell infiltration could be one of the possible reasons for the decrease in sensitivity of the endoscopic diagnosis of atrophy. This might be similar to the cases with inflammatory bowel diseases such as ulcerative colitis or Crohn’s disease, in which the initial colonoscopic feature is a loss of submucosal vascularity due to marked inflammatory cell infiltration.
Another significant factor that was associated with decreased sensitivity of the endoscopic diagnosis of atrophy in the body was a CRP > 5 mg/dl. Recently, a study has shown that CRP, a marker for a rapid acute-phase protein response increased after acetylsalicylic acid-induced gastric mucosal injury in dogs [29], which suggests that CRP might be useful together with gastroscopy for the diagnosis and monitoring of gastric injury [29]. It might be quite a jump if we interpret that the increased CRP could reflect the gastric inflammation in the body of the stomach. However, it could be possible to interpret that increased CRP may have a relation to gastric mucosal inflammation, which prevents clear visualization of submucosal vessels in the body of the stomach.
Two biochemically distinct pepsinogens are produced by the gastric mucosa. Pepsinogen I is produced primarily by the fundic mucosa, whereas pepsinogen II is secreted by the fundic, antral, and duodenal mucosa. Serum PG levels have been shown to reflect the morphological and functional status of the gastric mucosa including mucosal atrophy [30–33]. Internationally, a value of 3.0 is widely reported to be the optimal PGI /II cut-off value for atrophic gastritis or intestinal metaplasia [32–35]. In the present study, a PG I/II ratio >3 was associated with a decreased sensitivity of the endoscopic diagnosis of atrophy in the antrum. The decreased sensitivity of the endoscopic diagnosis of atrophy with a PG I/II ratio >3 may be related to less severe histological atrophy and thus decreased findings of atrophy by endoscopy. To support this speculation, the distribution of atrophy by endoscopy was evaluated in 758 subjects with confirmed histological atrophy according to PG I/II ratio 3. We found that in the group of subjects with histological atrophy in the antrum, the prevalence of the PG I/II ratio >3 was significantly lower in the group with atrophy present by endoscopy (42.6%) compared to the group with atrophy absent by endoscopy (63.9%; P < 0.001). In addition, in the group of subjects with confirmed histological atrophy in the body, the prevalence of a PG I/II ratio >3 was lower in the group with atrophy present by endoscopy (28.4%) compared to the group with atrophy absent by endoscopy (38.3%; P = 0.047). These results suggest that the diagnosis of atrophy by endoscopy could be difficult when the histological atrophy is mild. Furthermore, when the histological atrophic grade was compared between the group with atrophy absent by endoscopy and the group with atrophy present the histological atrophic grade was significantly higher in the group with atrophy present by endoscopy than in the group with atrophy absent. These results are consistent with the findings that the concordance was good in the severe forms of gastritis [11–17].
In conclusion, the results of this study showed that the endoscopic diagnosis of atrophy was not accurate, especially at an age below 50 years old, and when the atrophy was mild by histological criteria. Thus, a high index of suspicion for gastric atrophy is especially important in the younger age group, and confirmation by histology is necessary.
References
Correa P. Human gastric carcinogenesis: a multistep and multifactorial process—First American Cancer Society Award lecture on cancer epidemiology and prevention. Cancer Res. 1992;52:6735–6740.
Correa P. A human model of gastric carcinogenesis. Cancer Res. 1988;48:3554–3560.
Sipponen P, Kekki M, Haapakoski J, et al. Gastric cancer risk in chronic atrophic gastritis: statistical calculations of cross-sectional data. Int J Cancer. 1985;35:173–177. doi:10.1002/ijc.2910350206.
Kuipers EJ, Uyterlinde AM, Peña AS, et al. Long-term sequelae of Helicobacter pylori gastritis. Lancet. 1995;345:1525–1528. doi:10.1016/S0140-6736(95)91084-0.
Hopkins RJ, Girardi LS, Turney EA. Relationship between Helicobacter pylori eradication and reduced duodenal and gastric ulcer recurrence: a review. Gastroenterology. 1996;110:1244–1252. doi:10.1053/gast.1996.v110.pm8613015.
Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345:784–789. doi:10.1056/NEJMoa001999.
Rugge M, Correa P, Dixon MF, et al. Gastric mucosal atrophy: interobserver consistency using new criteria for classification and grading. Aliment Pharmacol Ther. 2002;16:1249–1259. doi:10.1046/j.1365-2036.2002.01301.x.
Kaur G, Raj SM. A study of the concordance between endoscopic gastritis and histological gastritis in an area with a low background prevalence of Helicobacter pylori infection. Singapore Med J. 2002;43:090–092.
Bah A, Saraga E, Armstrong D, et al. Endoscopic features of Helicobacter pylori-related gastritis. Endoscopy. 1995;27:593–596. doi:10.1055/s-2007-1005764.
Redéen S, Petersson F, Jönsson KA, Borch K. Relationship of gastroscopic features to histological findings in gastritis and Helicobacter pylori infection in a general population sample, Sweden. Endoscopy. 2003;35:946–950. doi:10.1055/s-2003-43479.
Atkins L, Benedict EB. Correlation of gross gastroscopic findings with gastroscopic biopsy in gastritis. N Engl J Med. 1956;254:641–644.
Kreuning J, Bosman FT, Kuiper G, Wal AM, Lindeman J. Gastric and duodenal mucosa in “healthy” individuals. J Clin Pathol. 1978;31:69–77. doi:10.1136/jcp.31.1.69.
Jönsson KA, Gotthard R, Bodemar G, Brodin U. The clinical relevance of endoscopic and histologic inflammation of a gastroduodenal mucosa in dyspepsia of unknown origin. Scand J Gastroenterol. 1989;24:385–395. doi:10.3109/00365528909093064.
Myren J, Serck-Hanssen A. The gastroscopic diagnosis of gastritis, with particular reference to mucosal reddening and mucus covering. Scand J Gastroenterol. 1974;9:457–462.
Fung WP, Papadimitriou JM, Matz LR. Endoscopic, histological and ultrastructural correlations in chronic gastritis. Am J Gastroenterol. 1979;71:269–279.
Tytgat GNJ. The Sydney system: endoscopic division. Endoscopic appearances in gastritis/duodenitis. J Gastroenterol Hepatol. 1991;6:223–234. doi:10.1111/j.1440-1746.1991.tb01469.x.
Toukan AU, Kamal MF, Amr SS, Arnaout MA, Abu-Romiyeh AS. Gastroduodenal inflammation in patients with nonulcer dyspepsia. A controlled endoscopic and morphometric study. Dig Dis Sci. 1985;30:313–320. doi:10.1007/BF01403839.
Shin HR, Won YJ, Jung KW, et al. Nationwide cancer incidence in Korea, 1999 2001; first result using the national cancer incidence database. Cancer Res Treat. 2005;37:325–331.
Carpenter HA, Talley NJ. Gastroscopy is incomplete without biopsy: clinical relevance of distinguishing gastropathy from gastritis. Gastroenterology. 1995;108:917–924. doi:10.1016/0016-5085(95)90468-9.
Yim JY, Kim N, Choi SH, et al. Seroprevalence of Helicobacter pylori in South Korea. Helicobacter. 2007;12:333–340. doi:10.1111/j.1523-5378.2007.00504.x.
Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney system. International workshop on the histopathology of gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161–1181.
Kim N, Kim JM, Kim CH, et al. Institutional difference of antibiotic resistance of Helicobacter pylori strains in Korea. J Clin Gastroenterol. 2006;40:683–687. doi:10.1097/00004836-200609000-00004.
Morson BC, Sobin LH, Grundmann E, Johansen A, Nagayo T, Serck-Hanssen A. Precancerous conditions and epithelial dysplasia in the stomach. J Clin Pathol. 1980;33:711–721. doi:10.1136/jcp.33.8.711.
Kim N, Park YS, Cho SI, et al. Prevalence and risk factors of atrophic gastritis and intestinal metaplasia in a Korean population without significant gastroduodenal disease. Helicobacter. 2008;13:245–255. doi:10.1111/j.1523-5378.2008.00604.x.
Wong BC, Lam SK, Wong WM, et al. China gastric cancer study group. Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA. 2004;291:187–194. doi:10.1001/jama.291.2.187.
Kim N, Park RY, Cho SI, et al. Helicobacter pylori infection and development of gastric cancer in Korea: long-term follow-up. J Clin Gastroenterol. 2008;42:448–454. doi:10.1097/MCG.0b013e318046eac3.
Kimura K, Satoh K, Ido K, Taniguchi Y, Takimoto T, Takemoto T. Gastritis in the Japanese stomach. Scand J Gastroenterol. 1996;31(Suppl 214):17–20. doi:10.3109/00365529609094509.
Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969;1:87–97. doi:10.1055/s-0028-1098086.
Bayramli G, Ulutas B. Acute phase protein response in dogs with experimentally induced gastric mucosal injury. Vet Clin Pathol. 2008;37:312–316. doi:10.1111/j.1939-165X.2008.00060.x.
Samloff IM, Varis K, Ihamaki T, Siurala M, Rotter JI. Relationships among serum pepsinogen I, serum pepsinogen II and gastric mucosal histology: a study in relatives of patient with pernicious anemia. Gastroenterology. 1982;83:204–209.
Sitas F, Smallwood R, Jewell D, et al. Serum anti-Helicobacter pylori IgG antibodies and pepsinogens A and C as serological markers of chronic atrophic gastritis. Cancer Epidemiol Biomarkers Prev. 1993;2:119–123.
Miki K, Ichinose M, Kawamura N, et al. The significance of low serum pepsinogen levels to detect stomach cancer associated with extensive chronic gastritis in Japanese subjects. Jpn J Cancer Res. 1989;80:111–114.
Kang JM, Kim N, Yoo JY, et al. The role of serum pepsinogen and gastrin test for the detection of gastric cancer in Korea. Helicobacter. 2008;13:146–156. doi:10.1111/j.1523-5378.2008.00592.x.
Kodoi A, Yoshihara M, Sumii K, Haruma K, Kajiyama G. Serum pepsinogen in screening for gastric caner. J Gastroenterol. 1995;30:452–460. doi:10.1007/BF02347560.
Miki K, Morita M, Sasajima M, Hoshina R, Kanda E, Urita Y. Usefulness of gastric cancer screening using the serum pepsinogen test method. Am J Gastroenterol. 2003;98:735–739. doi:10.1111/j.1572-0241.2003.07410.x.
Conflict of Interest or Financial Arrangement
No author has conflicts of interest or financial arrangements that could potentially influence the described research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Alisher Eshmuratov and Jong Chun Nah contributed equally to this work.
Rights and permissions
About this article
Cite this article
Eshmuratov, A., Nah, J.C., Kim, N. et al. The Correlation of Endoscopic and Histological Diagnosis of Gastric Atrophy. Dig Dis Sci 55, 1364–1375 (2010). https://doi.org/10.1007/s10620-009-0891-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0891-4