Abstract
We analyzed data from 1998–2004 from the National Cancer Data Base to evaluate associations between patient/treatment facility factors and stage at diagnosis for all colon cancers combined and by anatomic location. Compared to patients with private insurance, uninsured patients were significantly more likely to present with advanced-stage disease; Medicaid patients had likelihoods of advanced-stage colon cancer in-between those of privately insured and uninsured patients. Increased odds of advanced-stage colon cancer at diagnosis were also observed among Black (vs. White) patients, women (vs. men), and patients from low socioeconomic status (SES) regions (vs. those from higher SES regions). While the likelihood of advanced-stage disease at diagnosis decreased in later years overall, this decrease was not observed among patients with ascending colon cancers. Screening disparities may lead to more advanced stage at diagnosis among colon cancer patients; programs to improve access to screening among underserved populations may address this disparity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to recent data from the American Cancer Society, cancers of the colon and rectum are the third leading cause of cancer among men and women in the US, and the third leading cause of cancer deaths. Approximately 150,000 individuals are diagnosed with colorectal cancer (CRC) annually, and more than 50,000 die from this cancer [1]. The latter figure is particularly disturbing in that colorectal cancer can be prevented or diagnosed at an early (and highly curable) stage with appropriate screening.
Numerous reports have indicated significant disparities in rates of colorectal cancer screening [2–12]. Disparities in colorectal cancer screening rates are seen by age, gender, household income, race/ethnicity, level of education, having a usual source of healthcare, and insurance type/status. A recent analysis of National Health Interview Survey data indicated that insurance status was responsible for greater differences in the rate of colorectal cancer screening than was race/ethnicity or level of education [13]. Modifications of insurance reimbursement for colorectal cancer screening can have significant effects on early detection of colorectal cancer. As reported by Gross et al. [14], changes in Medicare reimbursement for colorectal cancer screening were associated with an approximately eight-fold increase in colonoscopy claims and a significant increase in the likelihood of early stage diagnosis.
Previous studies using data from a single state or province have reported associations of a variety of patient characteristics with colorectal cancer stage at diagnosis, including age, sex, race/ethnicity, comorbid conditions, insurance status, socioeconomic status, smoking status, and distance to primary care provider [15–29]. Halpern et al. [30] used data from the National Cancer Data Base (NCDB) to evaluate the association between insurance status, race/ethnicity, and stage at diagnosis for 12 sites of cancer, including colorectal cancer, for a large patient population across the US. These investigators found that uninsured patients and patients covered by Medicaid were significantly more likely to present with more advanced colorectal cancer (i.e., stage II or stage III/IV vs. stage I) than were privately insured patients, with odds ratios of approximately 2.0 for uninsured and 1.5 for Medicaid insured patients. Black patients were also slightly more likely to present with advanced (stage III/IV) colorectal cancer compared to White patients, even controlling for insurance status. To more fully evaluate the relationship between insurance status and variations in stage at clinical presentation for colon cancer, this manuscript presents more-detailed analyses of the associations between insurance status, race/ethnicity, age, socioeconomic status, and other factors on the American Joint Commission on Cancer (AJCC) stage at diagnosis for all colon cancers combined and by anatomic location.
Methods
Study Population
Patients in this analysis were drawn from The National Cancer Database (NCDB). The NCDB is a national hospital-based cancer registry jointly sponsored by the American College of Surgeons and the American Cancer Society. Prior to 1997, submissions of cancer patient records to the NCDB were voluntary and open to all cancer facilities in the US. Beginning in 1997, data collection was mandated as a requirement of the Commission on Cancer (CoC)-approved programs. Since 1999, approximately 75% of newly diagnosed cancers in the US have been captured in the database [31].
Cancer cases diagnosed from 1998 to 2004 were extracted from the NCDB utilizing the appropriate ICD-O-3 site and histology codes (n = 607,892). Data were abstracted using coding guidelines documented in the Registry Operations and Data Standards (ROADS) manual for cases diagnosed 1998–2002 [32], and the Facility Oncology Registry Data Standards manual (FORDS) for the diagnosis years 2003–2004 [33], the 6th edition of the AJCC Manual for Staging of Cancer [34] and the 3rd edition of the WHO International Classification of Disease for Oncology [35]. For cases diagnosed prior to 2001, reported ICD-O-2 tumor morphology codes were recoded to ICD-O-3. Only patients with site codes C18.0–C18.9 (colon) were selected for this analysis. While cancers of the colon, rectum, and rectosigmoid junction are often grouped together as colorectal cancer, for greater specificity of this analysis, we did not include patients with cancer of the rectum or rectosigmoid junction. Many patients with rectal cancer may receive neo-adjuvant chemotherapy prior to staging and we did not have full data on use of neo-adjuvant treatments. Further, as rectosigmoid junction cancers may (upon re-analysis) be classified as cancers of the colon or rectum, we also excluded this group.
The analysis included all individuals between ages 50 and 99 with the above-specified cancers diagnosed between 1998 and 2004; at the time of the analysis, 2004 was the most recent year of data available. Patients younger than age 50 were not included in the analysis as most guidelines recommend regular colorectal cancer screening beginning at age 50. Patients with non-invasive (in situ) cancer were excluded based on the reported ICD-O tumor behavior code. In addition, to help ensure more uniform and reproducible populations for the analyses, only patients with histology codes specified by the AJCC as being stageable histologies for colon cancer were included [34]. The sample was further restricted to include only cases categorized as Class 1 or 2, based on standard classifications used by the NCDB. Class 1 cases are those diagnosed at the reporting institution and received all or part of their first course of treatment at that facility. Class 2 cases are diagnosed elsewhere but received part or all of their treatment at the reporting facility. This initial study population consisted of 432,829 colon cancer patients.
We excluded from this analysis patients with unknown stage at diagnosis (26,771), in situ stage at diagnosis (4,125), unknown primary payer/insurance at diagnosis (10,259), age at diagnosis less than 18 years or greater than 99 years (262), sex unknown (192), unknown race (31,112), and other government primary payer/insurance at diagnosis (378). After these exclusions, the final analytical cohort consisted of 359,089 patients with colon cancer, 83% of the total starting population, with a mean age at diagnosis of 72.6 (standard deviation: 10.6) years.
Variables
The dependent variable of interest was cancer stage at diagnosis. Cancer stage was classified according to the AJCC 5th (1998–2002) and 6th edition (2003–2004) based on pathological stage if available. If pathological stage was missing, clinical stage information was used instead. Patient race was categorized as “White, Black, Hispanic, Other, Unknown” and insurance status at the time of diagnosis was categorized as Medicaid, Medicare (which included both Medicare alone and Medicare with supplement), uninsured (which included FORDS codes for not insured—NOS, not insured—charity write-off, and not insured—self-pay), and private insurance plans. The private insurance groups included patients classified with the following primary payers at diagnosis: Health Maintenance Organization (HMO), Preferred Provider Organization (PPO), managed care NOS, private insurance, Tricare/Champus, military, and insured NOS. The plans in the private insurance category were grouped together since these plans represent either privately purchased insurance (purchased by the individual, a family member, and/or employer) or insurance provided by the military that functions in a similar manner as private insurance (Tricare/Champus).
Beyond insurance status and race/ethnicity, associations with stage at diagnosis were evaluated for sex (male, female), age at diagnosis, census region of residence (Atlantic, Great Lakes, Midwest, Mountain, Northeast, Pacific, South, Southeast, and West), education level in patient’s zip-code of resident (proportion in zip-code without a high school degree based on national quartiles of the 2000 US Census as ≥29%, 20–28.9%, 14–19.9%, and <14%), median household income in patient’s zip-code of residence (based on national quartiles of the 2000 US Census as <$30,000, $30,000–34,999, $35,000–45,999, and ≥$46,000), and type of treatment facility (community hospital, community cancer facility, and teaching/research facility). The three types of treatment facilities are described by the CoC. Community hospitals treat at least 300 cancer cases a year and have a full range of services for cancer care but patients need referral for portions of their treatment. Community cancer centers are facilities that offer the same range of services as the community hospitals but have at least 750 annual cancer cases and conduct weekly cancer conferences. Teaching/research facilities differ from community cancer facilities in that the teaching/research facilities have residency programs and ongoing cancer research; 29 of the 39 National Cancer Institute (NCI-designated) Comprehensive Cancer Programs participate in the CoC approvals program and are included among teaching/research facilities in this study.
Statistical Analysis
We used unconditional multivariate logistic regression modeling [36] to calculate odds ratios and corresponding 95% confidence intervals to examine the association between likelihood of presenting with more advanced versus early stage at diagnosis and patient and facility characteristics. Three separate comparisons evaluating associations between study variables and stage at diagnosis were performed: (1) likelihood of diagnosis with stage II versus stage I disease; (2) diagnosis with stage III versus stage I disease; and (3) diagnosis with stage IV versus stage I disease. Subanalyses were also performed by colon cancer anatomic location, separately evaluating associations of stage at diagnosis with ascending/right (ICD-O code C18.2), transverse/middle (C18.4), and descending/left (C18.6) colon tumors.
Analyses were performed with SAS, version 9.1 (SAS Statistical Institute, Cary, North Carolina). Statistical testing was conducted via the SAS procedure for logistic regression (PROC LOGISTIC). All logistic regression analyses controlled for insurance status, race/ethnicity, age at diagnosis, zip-code-based median household income and education level, facility type, year of diagnosis, and census region.
Results
Characteristics of Study Population by Insurance Status
Table 1 presents descriptive information on the overall study population as well as the population by insurance status. Approximately 64% of the overall study population was covered by Medicare insurance for individuals age 65 and older while approximately 30% was covered by private insurance. Uninsured, Medicaid, and Medicare patients younger than age 65 each accounted for approximately 2% of the study population. The overall population was fairly evenly divided among the four stages at diagnosis, with more patients diagnosed with stage II and fewer with stage IV disease. However, the proportion of patients diagnosed with stage I disease was lower and the proportion diagnosed with stage IV disease was greater among uninsured and Medicaid patients compared to older Medicare and privately insured patients.
The mean age for the study population was 72.6 years of age. Patients in the older Medicare age group were older than those from other insurance status groups, as all of these patients were at least 65 years of age. The population was fairly evenly divided by sex, although there were more women in the Medicaid and older Medicare population and more men in the younger Medicare and privately insured groups. The study population was overwhelmingly White (approximately 83%), but the proportion of Black and Hispanic patients was greater among the uninsured and Medicaid groups. While Black and Hispanic patients accounted for 14% of the overall study population, these two groups represented almost 40% of the uninsured and Medicaid populations. Year of diagnosis was similar among the different insurance groups.
As expected, area-based socioeconomic status (SES) was closely associated with insurance status. Uninsured patients, Medicaid patients, and younger patients with Medicare coverage were more likely to be from areas with lower median household income and lower education rates than were privately insured and older Medicare patients. Uninsured and Medicaid patients were also more likely to be treated at teaching/research hospitals and less likely to be treated at community hospital compared to privately insured and older Medicare patients. Finally, while the study population represented a diverse range of home census regions, privately insured and older Medicare patients showed similar home regions except for the Great Lakes region (which included a greater proportion older Medicare than privately insured patients) and the Pacific region (which included a greater proportion of privately insured than older Medicare patients).
Association of Insurance and Race/Ethnicity with Stage at Diagnosis
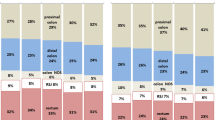
Figures 1 and 2 present the associations between insurance status and race/ethnicity (respectively) with stage at diagnosis for the colon cancer study population, based on the results of the multivariate regression analyses. Compared to privately insured patients, uninsured and Medicaid patients were significantly more likely to be diagnosed with stage II, III, or IV (vs. stage I) colon cancer. The elevated likelihood of more advanced stage diagnosis was significant for all three of these stages at diagnosis comparisons, and was greatest for the likelihood of stage I versus stage IV diagnosis. The odds ratios for uninsured patients were 1.92, 1.81, and 2.47 for stage II, III, and IV (respectively) and were 1.31, 1.33, and 1.68 for Medicaid patients. Younger Medicare and older Medicare patients did not differ significantly from privately insured patients in the likelihood of more advanced stage at diagnosis for the any of the comparisons.
Multivariate analysis of the association of insurance status and colon cancer stage at diagnosis. Multivariate-adjusted odds ratios are presented for the likelihood of stage II, III, or IV versus stage I colon cancer at diagnosis by insurance status. All odds ratios are with respect to privately insured patients. Odds ratios for Medicare patients are separated into younger Medicare (age less than 65) and older Medicare (age 65 and older)
As illustrated in Fig. 2, Black patients with colon cancer had slightly but significantly increased risks of stage III (odds ratio 1.08) or stage IV (odds ratio 1.28) disease at diagnosis compared to White patients, but no significant difference in the likelihood of stage II disease at diagnosis. Both Hispanic patients and patients in the “other race” category has significantly increased likelihood of diagnosis at stage III compared to White patients (odds ratios 1.06 and 1.19, respectively), but did not differ significantly from white patients for the likelihood of diagnosis at stage II or stage IV.
Association of Other Patient Characteristics with Stage at Diagnosis
Table 2 presents results from multivariate regression analyses for other factors associated with stage of colon cancer at diagnosis. Patients in each of the three older age groups were significantly more likely to be diagnosed with stage II versus stage I disease, but less likely to be diagnosed with more advanced (stage III or stage IV) versus stage I disease than were patients in the youngest age group, age 50–59 (results not significantly different for stage II vs. stage I at diagnosis among patients age 60–69). For all three comparisons, men were less likely to be diagnosed with more advanced colon cancer than were women, although the effect for stage IV disease at diagnosis was fairly small (odds ratio 0.97).
Patients from zip-codes with the two lowest median household incomes (<$30,000 and $30,000–$34,999) were significantly more likely to be diagnosed with stage II or stage IV colon cancer than were those from the highest household income zip-codes. Differences between the two high household income zip-codes were not significant. Patients from zip-codes with the lowest education levels (more than 29% of residents not having high school degrees) were significantly more likely to be diagnosed with stage IV colon cancer than were those from the highest education zip-codes (less than 14% of residents not having high school degrees). Compared to patients from the highest education zip-codes, those from the next to the lowest education level zip-codes (20–28.9% of residents not having high school degrees) were significantly more likely to be diagnosed with stage II, III, or IV colon cancer. However, all of these effects were fairly small in magnitude (odds ratios ≤1.10).
No significant differences in the likelihood of more advanced stage at diagnosis were observed by facility type. Patients diagnosed in more recent years were less likely to be diagnosed with stage II, III, or IV cancer than were patients diagnosed in the initial year of the study period, 1998. Finally, in comparing the likelihood of more advanced stage at diagnosis among census regions, patients in the reference group (Southeast region) had the lowest likelihood; odds ratios for all comparisons to the Southeast region were greater than 1.0 (although not all were statistically significant). However, the magnitude of the effect of census region was, in general, fairly small (odds ratio ≤1.10). The main exceptions to this were seen for the Mountain census region (odds ratios 1.21, 1.24, and 1.27 for stage II, III, and IV, respectively) and the Pacific census region (odds ratios 1.15, 1.09, and 1.19, respectively).
Association of Patient Characteristics with Stage at Diagnosis by Colon Cancer Anatomic Location
We performed separate evaluations of factors associated with stage IV cancers of the ascending/right, transverse/middle, and descending/left colon. A priori, it was difficult to predict what would be the potential differences by anatomic location in the association between patient characteristics and the likelihood of colon cancer. As cancers of ascending colon are more difficult to detect even when using appropriate screening techniques, it was possible that there would be less impact of patient characteristics on the likelihood of advanced-stage disease in the right colon. However, as uninsured and Medicaid covered individuals as well as individuals from low SES areas are less likely to be screened for colon cancer, and a lower proportion of those who are screened receive colonoscopy (which is a better technique for detecting right colon cancers), it was possible that insurance status and area-based SES would be more strongly associated with advanced stage at diagnosis for right than left colon cancers.
Results are presented in Table 3. As discussed in the Methods section, odds ratios presented in Table 3 were determined using logistic regression while controlling for insurance status; race/ethnicity; age at diagnosis; zip-code-based median household income and education level; facility type; year of diagnosis; and census region.
Overall, few significant differences in the likelihood of stage IV versus stage I diagnosis for ascending versus descending colon cancer were observed by insurance type. Among uninsured and Medicaid covered patients, there was a tendency toward greater likelihood of stage IV versus stage I disease (compared to that for privately insured patients) for ascending colon cancer compared to descending colon cancers. For example, among uninsured patients, the likelihood of stage IV versus stage I descending colon cancer was 2.37, while the likelihood for ascending colon cancer was 2.66. However, the odds ratios for likelihood of stage IV descending, transverse, and ascending colon cancers were not statistically different. Similar patterns were observed for younger and older Medicare patients. Among older Medicare patients, the likelihood of stage IV versus stage I ascending colon cancer was significantly greater than the likelihood of stage IV versus stage I descending colon cancer.
No significant differences in the likelihood of stage IV versus stage I colon cancer by anatomic location were observed for Black, Hispanic, or other race patients (compared to White patients). For the two oldest age groups (70–79 and 80+), a significant difference was observed, with patients in these groups (compared to patients 50–59) having a greater likelihood of stage IV versus stage I cancer of the ascending colon than the descending colon. No significant differences were observed by sex or area-based SES.
While a general increase in the likelihood of advanced-stage disease for ascending versus descending colon cancers was observed among insurance status and age at diagnosis groups, the reverse was seen by facility type. Patients treated at community hospitals and community cancer centers (compared to those treated at teaching/research hospitals) had greater likelihood of stage IV cancers of the descending colon than of the ascending colon. However, in all cases, the likelihood of advanced-stage colon cancer at diagnosis among patients treated at community hospitals and community cancer centers was less than that for teaching/research hospitals.
As presented in Table 2, the odds of being diagnosed with stage IV colon cancer (overall) were significantly decreased among patients diagnosed in 1999 through 2004 compared to patients diagnosed in 1998. A similar decrease in odds of stage IV cancer at diagnosis following 1998 was also observed for patients with cancers of the descending or transverse colon. However, among patients with cancer of the ascending colon, the likelihood of stage IV (vs. stage I) disease at diagnosis decreased slightly in 1999, then showed no significant difference compared to the likelihood in 1998 for the years 2000–2004. The odds of stage IV diagnosis for patients with ascending colon cancer in 2002–2004 (compared to diagnosis in 1998) were significantly greater than the corresponding odds of stage IV diagnosis among patients with descending colon cancer. No significant differences between the likelihood of stage IV descending versus ascending colon cancer were observed by year of diagnosis for patients diagnosed in 1999, 2000, or 2001. The results in Table 3 suggest that the progress in detecting colon cancer at earlier stages (or at least prior to stage IV) observed for 1999–2004 has been limited to cancers of the descending and transverse colon. No significant differences in diagnosis of stage IV descending versus ascending colon cancer were observed by census region of residence.
Association of Medicaid and Medicare Patient Subgroups with Stage of Colon Cancer at Diagnosis
As presented in Table 2, we found that patients with Medicaid coverage were significantly more likely to present with stage II, III, or IV colon cancers than were those with private insurance. We also found no significant difference between patients with Medicare insurance among individuals aged 65 and older compared to private insurance patients in the likelihood of more advanced colorectal cancer stage at diagnosis. Beginning in 2003, coding of insurance status in the NCDB was modified to provide increased specificity. For the two most recent years of data available for this study (2003 and 2004), we were able to separate Medicaid patients in managed-care programs versus Medicaid patients not in managed care. We were also able to separately identify Medicare patients who had supplemental private insurance, Medicare patients with dual Medicare–Medicaid coverage, and Medicare patients with no additional insurance coverage. To further evaluate the role of insurance status on colorectal cancer stage at diagnosis, we performed subgroup analyses among these Medicaid and Medicare populations.
Results of these analyses are presented in Table 4. Among colon cancer patients age 64 or younger with Medicaid coverage, there was a non-significant decrease in the likelihood of stage II or stage III disease at diagnosis for patients with managed care coverage compared to those without Medicaid managed care. The difference between Medicaid managed care and non-managed care patients for the likelihood of stage IV colon cancer at diagnosis was statistically significant, with Medicaid managed care patients experiencing a decrease in the likelihood of stage IV colon cancer at diagnosis by almost 50% compared to their non-managed care counterparts. Among Medicare patients age 65 and older, those who had Medicare plus private supplemental insurance were significantly less likely to present with stage II, III, or IV colon cancer than were patients with Medicare coverage alone. No significant difference was observed between patients with Medicare coverage alone and dual Medicaid–Medicare coverage.
Discussion
This study has presented detailed results regarding patient characteristics associated with more advanced (stage II, III, or IV vs. stage I) colon cancer diagnoses. As we previously reported [30], uninsured patients and patients with Medicaid coverage as well as Black patients were more likely to present with advanced colorectal cancer (compared to privately insured and White patients, respectively). In this study, we have confirmed these findings and provided greater detail regarding the likelihood of stage II, III, or IV versus stage I at diagnosis. An important finding is that while patients with Medicaid insurance were significantly more likely to present with advanced-stage colon cancer than were privately insured patients, there were significantly less likely to present with an advanced-stage diagnosis than were uninsured patients. This is consistent with higher rates of screening, including colonoscopy, among Medicaid insured compared to uninsured patients [13]. We also confirmed greater likelihoods of advanced-stage colon cancer in all anatomic locations among Black versus White patients. Previous reports indicated that Black patients are more likely to present with proximal colorectal polyps and neoplasms than are non-Hispanic White patients [37, 38]. However, previous studies have reported that after controlling for insurance and other sociodemographic factors, there are minimal or no significant differences in CRC screening rates between Black and White individuals [3, 12].
We also report that women and patients from low SES areas were more likely to present with more advanced colon cancer, while patients from the Southeast census region and patients diagnosed in later years of the study period were less likely to present with more advanced colon cancer. The increased likelihood of more advanced stage among women may reflect women being less likely to receive invasive colon cancer screening procedures than are men [39]. Older patients are more likely than younger patients to present with stage II versus stage I colon cancer, but are less likely to present with advanced (stage III or IV) colon cancer compared to younger patients. Few significant differences by patient characteristics were observed in analyses of the likelihood of stage IV ascending versus descending colon cancer. However, older patients (compared to the youngest patient group) were more likely to present with advanced disease of the ascending than of the descending colon, while patients treated at community hospitals and community cancer centers (compared to those treated at teaching/research hospitals) were more likely to present with stage IV cancer of the descending than of the ascending colon. The association between increased likelihood of advanced-stage cancer of the ascending colon and older age is consistent with previous work indicating a “shift-to-the-right” with advancing age for patients with colonic adenomas [40].
We also found that while the likelihood of stage IV versus stage I cancer at diagnosis decreased in the years 1999–2004 (compared to 1998) for all colon cancer patients overall as well as for patients with cancer of the transverse and descending colon, essentially no change in the likelihood of stage IV cancer at diagnosis was observed among patients with cancer of the ascending colon. This may reflect the greater difficulty in detecting cancers of the ascending colon, even with the use of appropriate screening techniques. For example, flexible sigmoidoscopy will not detect tumors of the ascending colon, and even receipt of a colonoscopy does not ensure that the entire colon was examined.
This finding may also reflect changes in the incidence of colon cancer by anatomic location over time. Thörn et al. [41] reported that the age-standardized rate of cancers of the ascending and transverse colon in Sweden increased between 1959 and 1993, while the rate of cancers of the descending colon remained stable over this period. Cress et al. [42] reported different findings but with a similar impact on differences in colon cancer incidence by anatomic location. Using SEER data, these investigators found decreases in the incidence of colorectal cancers (significant only among men), which were most pronounced for tumors of the sigmoid colon and less pronounced for proximal colon tumors. The results from our study suggest that the progress in detecting colon cancer at earlier stages has been manifest most among patients with cancers of the descending and transverse colon, and less so for patients with cancer of the ascending colon. More research is needed to verify this finding and develop more-sensitive methods for earlier detection of cancers of the ascending colon.
We also performed more detailed evaluations regarding the associations between Medicaid and Medicare insurance status and stage at diagnosis. We observed a trend toward earlier diagnosis among Medicaid managed care patients compared to Medicaid patients without managed care, that was statistically significant for stage IV versus stage I colon cancer. While studies comparing outcomes between Medicaid managed care and non-managed care patients are limited, available literature suggests that Medicaid managed care patients receive more frequent preventive care services [43, 44] and may have better outcomes for conditions associated with on-going care [45], although this has not been found by all investigators [46]. Our results suggest that Medicaid managed care patients may have had better colorectal cancer screening and/or more timely follow-up to abnormal screening results or lower gastrointestinal symptoms than did non-manage care patients.
We also observed statistically significant earlier diagnoses among patients with Medicare plus private insurance (compared to Medicare alone or dual Medicare plus Medicaid) for stage II, III, or IV colon cancer. This is consistent with recent findings that individuals with Medicare plus supplemental insurance coverage were significantly more likely to have interval-appropriate colorectal cancer screening than were Medicare enrollees without supplemental coverage [47]. Other studies have found that even among individuals with private or Medicare insurance coverage, cost-sharing and degree of managed care penetration can influence the likelihood of obtaining CRC screening. Varghese et al. [48] reported that individuals in preferred provider organization (PPO) health plans were significantly more likely to obtain CRC tests than were those in fee-for-service (FFS) plans, which had greater office visit costs. Koroukian et al. [49] reported that among enrollees in Medicare FFS plans, those in areas with a high level of Medicare managed care activity were more likely to receive CRC screening than those from regions with low activity levels. These findings indicate that insurance programs can be structured to facilitate colon screening and thus diagnoses disease earlier or even prevent the development of invasive colon cancer.
There are a number of limitations for this study. First, there may be questions regarding the generalizability of data from the NCDB. The NCDB includes data only from CoC hospitals, excluding cancer patients who are diagnosed and treated only at non-CoC hospitals. CoC hospitals are required to meet or exceed standards for the diagnosis and treatment of cancer, and undergo regular performance evaluations. However, facilities with CoC-approved programs constitute a diverse mix of hospitals. Non-CoC facilities are also diverse, including a number of NCI-designated Comprehensive Cancer Centers, so the patient population treated at non-CoC facilities is not necessarily skewed towards underserved individuals. Further, a previous analysis of breast cancer patient referral patterns indicated no significant differences between CoC and non-CoC programs [50]. Finally, the age and cancer stage distributions of the study population are similar to those observed in data from SEER, and the insurance status distribution is similar to that determined using US insurance status rates for a population with the same age, gender, and race/ethnicity distribution as the study population. Based on these factors, it appears unlikely that our results are systematically biased by treatment referral patterns to CoC-approved cancer programs.
Our study also lacked individual-level data on measures of SES, including education and income. We used categories of education and income based on the patients’ zip-codes of residence to help control for associations with SES. While these area-level indices are likely correlated with individual SES and may independently influence access to care, they do not fully reflect individual-level variation in SES.
In addition, the observed association between Medicaid insurance and more advanced stage of cancer at diagnosis does not distinguish between patients who became eligible for Medicaid coverage because of their cancer diagnosis from those who were covered by Medicaid prior to diagnosis. Bradley et al. [51] reported that patients with CRC who enrolled in Medicaid after their cancer diagnosis were more likely to have late stage disease than were those enrolled prior to diagnosis. In the population studied by Bradley et al., 54% of Medicaid patients with CRC enrolled in Medicaid prior to diagnosis, while 46% enrolled after diagnosis. Ramsey et al. [52] found that in Washington state, 57% of Medicaid patients diagnosed with five major types of cancer (including CRC) had enrolled in Medicaid within three months of their diagnosis. Data specific to CRC patients were not presented. In our study, the odds ratios associated with Medicaid insurance may be modified by retroactive enrollment of patients who were initially uninsured. However, information on date of Medicaid enrollment for patients with Medicaid as the primary payer is generally not available from cancer registries, including the NCDB.
The study may underestimate the benefits of private and Medicare insurance in facilitating appropriate CRC screening due to the use of Stage I patients as the referent group. CRC screening, and colonoscopy in particular, reduces the incidence rate for colon cancer through removal of precancerous polyps; individuals whose cancers are prevented in this way will not be included in the study population of patients with invasive cancers.
Finally, multiple barriers that affect receipt of optimal medical care, including both internal factors (e.g., low interest in screening, denial of risks, fear) and external factors (e.g., availability of information in formats/languages that can be understood by patients, distance/ease of transportation to medical care facilities, receptivity of providers), were not included in our study. Lack of adequate insurance is a crucial factor regarding access to timely and appropriate medical care, and may be more feasible to address than many other personal and societal barriers. However, addressing this factor alone is unlikely to resolve all disparities in cancer screening and treatment.
Despite these limitations, our study provides important results on patient factors associated with colon cancer stage at diagnosis. These results also have important implications for colon cancer screening programs. Over the past several years, with heightened education (for both patients and providers), CRC screening rates have increased [53–55]. In addition, increasingly more screening colonoscopies are being performed as compared to fecal occult blood tests (FOBT) and flexible sigmoidoscopy [55], which are likely to miss more cancer (and pre-cancer lesions) than is colonoscopy [56–58]. However, as noted in the Introduction, many previous studies have identified disparities associated with receipt of CRC screening based on insurance status, race/ethnicity, SES, age, and other factors.
Our results suggest that screening disparities could lead to more advanced stage at diagnosis among colon cancer patients, and that programs to improve access to CRC screening among underserved populations are likely to result in earlier diagnosis. Investments in improved CRC and better access to care for at-risk populations (particularly uninsured and Medicaid patients) may have substantial benefits in terms of morbidity, mortality, quality of life, and even costs. However, improved access or incentives (such as decreased co-payments) even among private insurance and Medicare patients may also lead to improved screening and earlier stage at diagnosis. Further research is needed to quantify potential outcomes resulting from improved screening and/or changes in insurance coverage for these populations.
References
American Cancer Society. Cancer Facts and Figs 2008. Atlanta: American Cancer Society; 2008.
Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–2069.
Chen JY, Diamant A, Pourat N, Kagawa-Singer M. Racial/ethnic disparities in the use of preventive services among the elderly. Am J Prev Med. 2005;29:388–395.
Gordon NP, Rundall TG, Parker L. Type of health care coverage and the likelihood of being screened for cancer. Med Care. 1998;36:636–645.
Hsia J, Kemper E, Kiefe C, et al. The importance of health insurance as a determinant of cancer screening: evidence from the Women’s Health Initiative. Prev Med. 2000;31:261–270.
Ioannou GN, Chapko MK, Dominitz JA. Predictors of colorectal cancer screening participation in the United States. Am J Gastroenterol. 2003;98:2082–2091.
Kandula NR, Wen M, Jacobs EA, Lauderdal DS. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic Whites: cultural influences or access to care? Cancer. 2006;107:184–192.
Ko CW, Kreuter W, Baldwin LM. Effect of Medicare coverage on use of invasive colorectal cancer screening tests. Arch Intern Med. 2002;162:2581–2586.
Pollack LA, Blackman DK, Wilson KM, Seeff LC, Nadel MR. Colorectal cancer test use among Hispanic and non-Hispanic US populations. Prev Chronic Dis. 2006;3:A50.
Potosky AL, Breen N, Graubard BI, Parsons PE. The association between health care coverage, the use of cancer screening tests. Results from the National Health Interview Survey. Med Care. 1998;36:257–270.
Ross JS, Bradley EH, Busch SH. Use of health care services by lower-income and higher-income uninsured adults. JAMA. 2006;295:2027–2036.
Seeff LC, Nadel MR, Klabunde CN, et al. Patterns and predictors of colorectal cancer test use in the adult US population. Cancer. 2004;100:2093–2103.
Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31.
Gross CP, Andersen MS, Krumholz HM, McAvay GJ, Proctor D, Tinetti ME. Relation between Medicare screening reimbursement and stage at diagnosis for older patients with colon cancer. JAMA. 2006;296:2815–2822.
Bradley CJ, Given CW, Roberts C. Disparities in cancer diagnosis and survival. Cancer. 2001;91:178–188.
Campbell RJ, Ferrante JM, Gonzalez EC, Roetzheim RG, Pal N, Herold A. Predictors of advanced-stage colorectal cancer diagnosis: results of a population-based study. Cancer Detect Prev. 2001;25:430–438.
Fazio L, Cotterchio M, Manno M, McLaughlin J, Gallinger S. Association between colonic screening, subject characteristics, and stage of colorectal cancer. Am J Gastroenterol. 2005;100:2531–2539.
Frederiksen BL, Osler M, Harling H, Danish Colorectal Cancer Group, Jørgensen T. Social inequalities in stage at diagnosis of rectal but not in colonic cancer: a nationwide study. Br J Cancer. 2008;98:668–673.
Gonzalez EC, Ferrante JM, Van Durme DJ, Pal N, Roetzheim RG. Comorbid illness and the early detection of cancer. South Med J. 2001;94:913–920.
Lee-Feldstein A, Feldstein PJ, Buchmueller T. Health care factors related to stage at diagnosis and survival among Medicare patients with colorectal cancer. Med Care. 2002;40:362–374.
Longnecker MP, Clapp RW, Sheahan K. Associations between smoking status and stage of colorectal cancer at diagnosis in Massachusetts between 1982 and 1987. Cancer. 1989;64:1372–1374.
Mandelblatt J, Andrews H, Kao R, Wallace R, Kerner J. The late-stage diagnosis of colorectal cancer: demographic and socioeconomic factors. Am J Public Health. 1996;86:1794–1797.
Parikh-Patel A, Bates JH, Campleman S. Colorectal cancer stage at diagnosis by socioeconomic and urban/rural status in California, 1988–2000. Cancer. 2006;107:1189–1195.
Parsons MA, Askland KD. Cancer of the colorectum in Maine, 1995–1998: determinants of stage at diagnosis in a rural state. J Rural Health. 2007;23:25–32.
Pollack LA, Gotway CA, Bates JH, et al. Use of the spatial scan statistic to identify geographic variations in late stage colorectal cancer in California (United States). Cancer Causes Control. 2006;17:449–457.
Roetzheim RG, Pal N, Tennant C, et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999;91:1409–1415.
Rogers SO, Ray WA, Smalley WE. A population-based study of survival among elderly persons diagnosed with colorectal cancer: does race matter if all are insured? (United States). Cancer Causes Control. 2004;15:193–199.
Schwartz KL, Crossley-May H, Vigneau FD, Brown K, Banerjee M. Race, socioeconomic status and stage at diagnosis for five common malignancies. Cancer Causes Control. 2003;14:761–766.
Woods SE, Basho S, Engel A. The influence of gender on colorectal cancer stage: the state of Ohio, 1996–2001. J Womens Health (Larchmt). 2006;15:877–881.
Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and race/ethnicity with cancer stage at diagnosis: a retrospective analysis. Lancet Oncol. 2008;9:222–231.
Commission on Cancer. Site by stage distribution of cases reported to the NCDB: diagnosis year 2003. Available at: http://www.facs.org/cancer/ncdb/ver7_site_stage_2003.htm. Accessed 22 Dec 2008.
Commission on Cancer. Registry operations and data standards (ROADS). Available at: http://www.facs.org/cancer/coc/roads/roads1998.pdf. Accessed 22 Dec 2008.
Commission on Cancer. Facility oncology registry data standards manual (FORDS). Available at: http://www.facs.org/cancer/coc/fords/fordsoriginal2003.pdf. Accessed 22 Dec 2008.
Greene F, Page D, Fleming I, et al. AJCC cancer staging manual. 6th ed. Chicago, IL: Springer; 2002.
Fritz A, Percy C, Jack A, et al. International Classification of Diseases for Oncology, ICD-O. 3rd ed. Geneva: World Health Organization; 2000.
Breslow NE, Day NE. Statistical Methods in Cancer Research. Vol 1. The Analysis of Case-Control Studies. Lyons: International Agency for Research on Cancer; 1980.
Shavers VL. Racial/ethnic variation in the anatomic subsite location of in situ and invasive cancers of the colon. J Natl Med Assoc. 2007;99:733–748.
Thornton JG, Morris AM, Thornton JD, Flowers CR, McCashland TM. Racial variation in colorectal polyp and tumor location. J Natl Med Assoc. 2007;99:723–728.
Ko CW, Kreuter W, Baldwin LM. Persistent demographic differences in colorectal cancer screening utilization despite Medicare reimbursement. BMC Gastroenterol. 2005;5:10.
Gerharz CD, Gabbert H, Krummel F. Age-dependent shift-to-the-right in the localization of colorectal adenomas. Virchows Arch A Pathol Anat Histopathol. 1987;411:591–598.
Thörn M, Bergström R, Kressner U, Sparén P, Zack M, Ekbom A. Trends in colorectal cancer incidence in Sweden 1959–1993 by gender, localization, time period, and birth cohort. Cancer Causes Control. 1998;9:145–152.
Cress RD, Morris C, Ellison GL, Goodman MT. Secular changes in colorectal cancer incidence by subsite, stage at diagnosis, and race/ethnicity, 1992–2001. Cancer. 2006;107:1142–1152.
Bailey JE, Womeodu RJ, Wan JY, Van Brunt DL, Somes GW. Improvements in diabetes management and outcomes in a Medicaid managed care system. Tenn Med. 2001;94:425–430.
Fairbrother G, Hanson KL, Butts GC, Friedman S. Comparison of preventive care in Medicaid managed care and Medicaid fee for service in institutions and private practices. Ambul Pediatr. 2001;1:294–301.
Kenney G, Sommers AS, Dubay L. Moving to mandatory Medicaid managed care in Ohio: impacts on pregnant women and infants. Med Care. 2005;43:683–690.
Reisinger AL, Sisk JE. Preventive service use and Medicaid managed care in New York City. Am J Manag Care. 2000;6:45–51.
Schneider EC, Rosenthal M, Gatsonis CG, Zheng J, Epstein AM. Is the type of Medicare insurance associated with colorectal cancer screening prevalence and selection of screening strategy? Med Care. 2008;46:S84–S90.
Varghese RK, Friedman C, Ahmed FAL, Manning M, Seeff LC. Does health insurance coverage of office visits influence colorectal cancer testing? Cancer Epidemiol Biomarkers Prev. 2005;14:744–747.
Koroukian SM, Litaker D, Dor A, Cooper GS. Use of preventive services by Medicare fee-for-service beneficiaries: does spillover from managed care matter? Med Care. 2005;43:445–452.
Katz SJ, Hofer TP, Hawley S, et al. Patterns and correlates of patient referral to surgeons for treatment of breast cancer. J Clin Oncol. 2007;25:271–276.
Bradley CJ, Given CW, Roberts C. Late stage cancers in a Medicaid-insured population. Med Care. 2003;41:722–728.
Ramsey SD, Zeliadt SB, Richardson LC, et al. Disenrollment from Medicaid after recent cancer diagnosis. Med Care. 2008;46:49–57.
Breen N, Wagener DK, Brown ML, Davis WW, Ballard-Barbash R. Progress in cancer screening over a decade: results of cancer screening from the 1987, 1992, and 1998 National Health Interview Surveys. J Natl Cancer Inst. 2001;93:1704–1713.
Liang SY, Phillips KA, Nagamine M, Ladabaum U, Haas JS. Rates and predictors of colorectal cancer screening. Prev Chronic Dis. 2006;3:A117.
Phillips KA, Liang SY, Ladabaum U, et al. Trends in colonoscopy for colorectal cancer screening. Med Care. 2007;45:160–167.
Collins JF, Lieberman DA, Durbin TE, Weiss DG, Veterans Affairs Cooperative Study #380 Group. Accuracy of screening for fecal occult blood on a single stool sample obtained by digital rectal examination: a comparison with recommended sampling practice. Ann Intern Med. 2005;142:81–85.
Morikawa T, Kato J, Yamaji Y, Wada R, Mitsushima T, Shiratori Y. A comparison of the immunochemical fecal occult blood test and total colonoscopy in the asymptomatic population. Gastroenterology. 2005;129:422–428.
Segnan N, Senore C, Andreoni B, et al. Comparing attendance and detection rate of colonoscopy with sigmoidoscopy and FIT for colorectal cancer screening. Gastroenterology. 2007;132:2304–2312.
Author information
Authors and Affiliations
Corresponding author
Additional information
A portion of this work was completed while Dr. Halpern was Strategic Director of Health Services Research at the American Cancer Society, Atlanta, GA.
Rights and permissions
About this article
Cite this article
Halpern, M.T., Pavluck, A.L., Ko, C.Y. et al. Factors Associated with Colon Cancer Stage at Diagnosis. Dig Dis Sci 54, 2680–2693 (2009). https://doi.org/10.1007/s10620-008-0669-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-008-0669-0