Abstract
Esophageal mucin secretion in patients with reflux esophagitis (RE) is significantly impaired. Rabeprazole augments gastric mucin secretion. We have studied, therefore, the effect of rabeprazole on esophageal mucin secretion in patients with RE. The study was conducted in 15 patients with RE treated with rabeprazole (20 mg QD) for 8 weeks. Esophageal secretions were collected during consecutive infusions of initial NaCl, HCl/Pepsin (HCl/P), and a final NaCl, using a specially designed esophageal catheter, before and after therapy. Mucin was measured using standard methodology. After rabeprazole administration esophageal mucin concentration as well as secretion increased during perfusion with initial saline (P < 0.01), HCl/P (P < 0.02), and concluding saline (P < 0.001). Stimulation of esophageal mucin secretion by rabeprazole may indicate that the mechanisms governing its secretion are similar to those implicated in gastric mucin output. Enhancement of esophageal mucin secretion by rabeprazole may translate into esophagoprotective potential in patients with reflux esophagitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In patients with gastroesophageal reflux disease (GERD), especially accompanied by endoscopic erosions, so-called reflux esophagitis (RE), esophageal epithelium is injured by acid and pepsin within the gastroesophageal reflux (GER) [1–5].
Experimental data from animal models point to potential pathogenetic role of bile acids in the esophageal mucosal injury around the luminal pH of 7.0, however their impact is limited at best as a great majority of GER episodes exhibit pH 4.0 or lower [6–10].
Thus acid and pepsin duet remains as the leading injurious force in the development of pathogenetically significant and clinically detrimental sequelae.
Since injurious components of the GER always act on the luminal aspect of the squamous epithelium, the mucus/buffer layer (0.095 μm thick) covering the mucosa represents a vanguard of mucosal defense, the so-called pre-epithelial barrier [11]. This mucus/buffer layer is continuously eroded by the luminal mechanical and chemical forces and restored by continuous secretion from esophageal submucosal mucous glands as well as freshly swallowed salivary secretions [3, 12–15]. Of note, as we have recently demonstrated for the first time in humans, protective factors elaborated by salivary and esophageal submucosal mucous glands, especially bicarbonate and nonbicarbonate buffers, epidermal growth factor (EGF), and transforming growth factor alpha (TGFα) are significantly augmented by stimulation of serotonin receptor 5HT4 [16].
We have recently demonstrated that mucin content, the predominant and most protective component of mucus, in patients with RE is significantly impaired [17]. Furthermore, this esophageal mucin secretion impairment persists even after endoscopic healing of RE, strongly implying that the diminished esophageal mucin content represents a pre-existing condition, predisposing patients to erosive mucosal injury during GER episodes [17].
Administration of rabeprazole results in a significant increase in gastric mucin secretion, even during coadministration of naproxen [22, 23]. If administration of rabeprazole may result also in increased esophageal mucin secretion accompanied by healing of RE remains to be explored.
We have therefore studied the mucin content of esophageal secretion, collected during esophageal mucosal exposure to NaCl followed by HCl/pepsin and again NaCl, a sequence intended to mimic the natural GER scenario, before and after 8 weeks of rabeprazole administration resulting in healing of RE confirmed endoscopically.
Materials and Methods
Study Design
The institutional review board approved this study, conducted at the University of Kansas Medical Center. Each GERD patient with endoscopically confirmed RE received rabeprazole 20 mg QD for 8 weeks. Patients were instructed to take the study medication 30 min prior to breakfast. Salivary and esophageal secretion studies were conducted before and at the end of 8 weeks of therapy and within 2 h from the last dose of study medication when healing of RE was endoscopically confirmed. All secretory studies were conducted between 9:00 am and 11:00 am in order to eliminate the potential impact of circadian rhythm on investigated parameters.
For assessment of esophageal mucin content the laboratory personnel remained blinded to coding of esophageal secretion samples (sample numbers were consecutively assigned for the entire group of patients regardless of whether they were undergoing esophageal perfusion procedure the first or second time) collected before or after healing of RE with rabeprazole.
Study Population
Eligible patients were men and women, 18–69 years of age, Hp negative, with a history of daily heartburn symptoms for 12 months prior to screening. Patients with evidence of structural abnormality of the gastrointestinal tract or disease/conditions other than RE were excluded. Exclusions included (but not limited to): Barrett’s esophagus, medication-induced erosive esophagitis, inflammatory bowel disease (IBD), active diverticulitis, peptic ulcer, esophageal stricture or ulcer, primary motor disorders of the esophagus or stomach, gastroparesis, gastrointestinal malignancies, gastrointestinal obstruction, chronic diarrhea, chronic constipation, surgery of the alimentary tract, pancreatitis, cholelithiasis, neurological or psychiatric disorders or other diseases or conditions that in the opinion of the investigator significantly affect salivary secretion (including smoking), pregnancy, current or history of drug or alcohol abuse. All medications potentially affecting salivary or esophageal secretions were prohibited during the study.
The study population, with endoscopically confirmed RE during enrollment, included ten males and five females, mean age 48 years (range 30–68 years) with RE (three grade A, six grade B, and six grade C, according to LA classification).
Secretion Collection Procedure
Patients were instructed to fast after midnight and to take their medication with a glass of water 1 h before their scheduled appointment on the day of secretion collection procedure.
The esophageal secretion collection procedure was conducted using the specially designed esophageal perfusion catheter (Wilson-Cook Medical, Winston Salem, NC) equipped with two inflatable intraesophageal balloons as we have described previously [5, 16].
The esophageal catheter was designed to seal a 3.75-cm segment of the esophagus between two small soft inflatable 20-mm balloons. The distal balloon was placed 5 cm above the lower esophageal sphincter, whereas the proximal balloon was located 3.75 cm orad. The distal balloon was inflated with ≥6 cc of air and the proximal balloon with 5 cc of air to provide acceptable recovery rates (>95%) of the initially infused testing 10 cc volume.
During esophageal perfusion, subjects remained in an upright position (under 90° angle) and were asked to expectorate saliva to different container to prevent its interference with esophageal secretions. Additionally, accidentally swallowed saliva was retained above the upper balloon and subsequently aspirated through the separate channel to different container.
Periods I through IV were designed to mimic the gastroesophageal reflux scenario. Three perfusion intervals (1.5 min each) constituted period I (baseline/initial saline), the next three perfusion intervals (initial HCl/Pepsin) represented period II, the next three perfusion intervals (final HCl/Pepsin) represented period III, and the last three perfusion intervals (final saline) constituted period IV (Table 1).
Esophageal Perfusion Model
Following inflation of the esophageal balloons, 10.0 ml solution was infused at 1.5-min intervals and then aspirated and reinfused three times. The final aspiration was transferred to a collecting container and the infusion was continued with a new 10.0 ml of corresponding solution. Esophageal perfusion in each subject was performed using a fresh solution for each 1.5-min interval: (1) NaCl (0.15 M), which corresponds to 0.9% saline or (2) HCl (0.01 M; pH 2.1) with pepsin 0.5 mg/ml (Sigma Chem. Co. MO). The molarity of HCl is based on an average concentration of hydrogen ions within the gastroesophageal refluxate [18]. The concentration of pepsin was chosen based on the data on proteolytic activity of the gastric juice in patients with reflux esophagitis [19, 20].
Esophageal Mucin Analysis
The content of mucin in the esophageal perfusate was measured by the periodic acid/Schiff (PAS) method developed by Mantle et al. [21] as described in our previous publications [5, 16].
All samples of the esophageal perfusate (for each esophageal perfusion period: period I-initial NaCl, period II-initial HCl/pepsin, period III-final HCl/pepsin, and period IV-final NaCl separately) were diluted 10× with saline, giving an approximate concentration of mucin between 10 and 100 μg/2 ml.
Reagents
-
A.
Schiff reagent containing 1.7% sodium metabisulphite (Sigma Chem. Co).
-
B.
Freshly made periodic acid solution (10 μl 50% periodic acid dissolved in 10 ml 7% acetic acid).
Procedure
-
0.2 ml of vigorously vortexed sample.
-
1.8 ml of NaCl added and mixed.
-
0.2 ml of freshly made periodic acid solution in 7% acetic acid added and vortexed.
-
The samples were incubated at 37°C for 2 h.
-
0.2 ml of a Schiff reagent (containing 1.7% sodium metabisulphite) was subsequently added and again vortexed.
-
In order to develop a color, samples were kept at room temperature for 30 min.
-
The developed color was measured at A555 against a blank.
Solutions of human esophageal mucin (10–100 μg/ml), purified from dialyzed and lyophilized esophageal mucus by density gradient ultracentrifugation in CsCl as described previously [5, 22–24], were used for the standard curve.
Briefly, the esophageal mucus in aspirated esophageal secretions was isolated after exhausting dialysis (with Spectra/Por CE DispoDialyzer of 1000 D cut off) using Spectra/Por EZ-1 Multidialyzer (Spectrum Laboratories, Rancho Dominguez, CA). The dialyzed samples of esophageal secretions were subsequently lyophilized using a freeze-drying (Labconco, CA) system.
Lyophilized mucus was assessed gravimetrically and pure mucin was isolated after dissolving lyophilized gastric mucus in cesium chloride solution (42% w/v) and ultracentrifugation at 260,000 g for 48 h (Beckman Ultracentrifuge model L5-50, SW-41 swinging rotor). After ultracentrifugation each tube was fractionated into 12 separate fractions, the fraction containing mucin (fractions 2–5) was collected, exhaustively dialyzed, lyophilized, and the final content of mucin assessed gravimetrically. Purified human esophageal mucin was used as standard for the standard curve established using PAS methodology, in a similar fashion as all samples of esophageal secretions used for the final measurements of esophageal mucin concentration and output.
Data Processing and Statistical Analysis
Data, presented as mean ± standard error of the mean (SEM) were analyzed statistically using paired Student’s t-test using SigmaStat software (SYSTAT, Inc. CA).
Sample size was not based on statistical considerations.
Results
Among our patients with RE grades (three patients with grade A, six patients with grade B, and six patients with grade C according to LA classification) we achieved 93% healing rate after 8 weeks of rabeprazole (20 mg QD) administration; only one patient with grade C LA experienced incomplete healing after 8 weeks, but grade C improved to grade A.
Eight weeks of rabeprazole administration resulted also in significant increase of secretion elaborated from the esophageal submucosal mucous glands in patients with completely healed endoscopic erosions (Table 2).
The end volume of esophageal perfusate and collected de novo elaborated esophageal secretion during infusion of initial NaCl was 6.79 ± 0.06 ml/min (period I) and increased significantly, by 5.9%, to 7.19 ± 0.11 ml/min (P = 0.004) after healing of RE with 8 weeks of rabeprazole administration.
The corresponding volume of esophageal perfusate/secretion significantly increased, by 10%, during the mucosal exposure to initial HCl/pepsin (7.27 ± 0.16 versus 6.60 ± 0.11 ml/min; P = 0.002; period II) after healing of RE with rabeprazole administration.
The corresponding volume of esophageal perfusate/secretion significantly increased, by 7.2%, during the mucosal exposure to final HCl/pepsin (7.11 ± 0.15 versus 6.63 ± 0.12 ml/min; P = 0.016; period III) after healing of RE with 8 weeks of rabeprazole administration.
Finally, the corresponding volume of esophageal perfusate/secretion also significantly increased, by 9.8%, during the mucosal exposure to the final saline perfusion (7.28 ± 0.17 versus 6.63 ± 0.11 ml/min; P = 0.004; period IV).
Additionally, healing of RE was associated with a significant increase in mucin concentration within the perfusate/secretion elaborated by the esophageal submucosal mucous glands.
The concentration of esophageal mucin within the esophageal perfusate during the mucosal exposure to initial saline in patients with RE was 0.22 ± 0.04 mg/ml (period I) and increased significantly, by 118%, to 0.48 ± 0.09 mg/ml (P = 0.013) after healing of RE with 8 weeks of rabeprazole administration.
The concentration of esophageal mucin within the esophageal perfusate during mucosal exposure to initial HCl/pepsin in patients with RE was 0.17 ± 0.04 mg/ml (period II) and increased significantly, by 140%, to 0.41 ± 0.08 mg/ml (P = 0.011) after healing of RE with rabeprazole.
The concentration of esophageal mucin within the esophageal perfusate during the mucosal exposure to final HCl/pepsin in patients with RE was 0.16 ± 0.04 mg/ml (period III) and increased by 123%, to 0.36 ± 0.10 mg/ml (P = 0.072) after 8 weeks of rabeprazole administration.
The concentration of esophageal mucin within the esophageal perfusate during the mucosal exposure to final saline in patients with RE was 0.10 ± 0.03 mg/ml (period IV) and increased significantly and profoundly, by 455%, to 0.54 ± 0.11 mg/ml (P < 0.001) after healing of RE with 8 weeks of rabeprazole administration.
Healing of RE with rabeprazole had also profound and significant impact on the rate of esophageal mucin secretion.
The rate of esophageal mucin secretion during the mucosal exposure to initial saline in patients with RE was 1.48 ± 0.29 mg/min (period I) and increased significantly, by 129%, to 3.39 ± 0.62 mg/min (P = 0.008) after 8 weeks of rabeprazole administration.
The rate of esophageal mucin secretion, during the mucosal exposure to initial HCl/pepsin in patients with RE was 1.14 ± 0.26 mg/min (period II) and increased significantly, by 164%, to 3.01 ± 0.62 mg/min (P = 0.007) after healing of RE with 8 weeks of rabeprazole administration.
The rate of esophageal mucin secretion during the mucosal exposure to final HCl/pepsin in patients with RE was 1.10 ± 0.28 mg/min (period III) and increased by 137%, to 2.61 ± 0.78 mg/min (P = 0.065) after 8 weeks of rabeprazole administration.
The rate of esophageal mucin secretion during the mucosal exposure to final saline in patients with RE was 0.64 ± 0.18 mg/min (period IV) and increased significantly and profoundly, by 404%, to 3.87 ± 0.79 mg/min (P < 0.001) after healing of RE with 8 weeks of rabeprazole administration.
Discussion
We have recently demonstrated for the first time in humans, in a double-blind placebo-controlled study protocol, that administration of rabeprazole (20 mg QD) for 7 days results in significant increase in gastric mucin secretion (by 167%; P < 0.0001) [23].
In another novel, double-blind placebo-controlled crossover-designed study protocol we have demonstrated that administration of naproxen (500 mg BID) for 7 days results in significant decline of gastrin mucin production (by 49%, P < 0.01). Coadministration, however, of naproxen (500 mg BID) with rabeprazole (20 mg QD) resulted in significant restoration of an impairment in mucin production (by 67%, P = 0.003) [22].
In presented study, we demonstrate for the first time in humans that healing of RE with rabeprazole (8 weeks of 20 mg QD) is associated with significant increases in the rate of secretion of esophageal mucin both in basal conditions (during mucosal exposure to initial saline) and following mucosal challenge with HCl/pepsin, mimicking the natural gastroesophageal reflux scenario.
Although in presented study, we enrolled three patients with grade A, six patients with grade B, and six patients with grade C reflux esophagitis according to LA classification, these numbers are too small to make meaningful statistical analysis of subgroups regarding their rate of mucin secretion before and after healing. Such a study, however, should be conducted in the future with simultaneous assessment of esophageal acid exposure time during 24-h pH monitoring. This insight could be of great pathogenetic value, as the integrity of the esophageal mucosa depends upon equilibrium between aggressive factors and protective mechanisms [1, 5, 11, 12].
It appears that augmentation of mucin production by esophageal submucosal mucous glands represents a similar phenomenon to that demonstrated within the gastric mucosa where this mucin secretion stimulatory impact prevailed even during coadministration of naproxen [22].
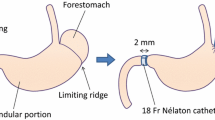
It has been recently demonstrated that secretion of esophageal mucin, the major protective component of mucus, in patients with RE is significantly impaired even after endoscopic healing of RE [17], strongly implying that this impairment may be a pre-existing condition that predisposes patients to erosive mucosal injury during GER episodes as depicted in our illustration (Fig. 1a).
Schematic outline of the cross-sectional view of the esophageal mucosa covered with the mucus buffer layer generated by secretion from salivary and esophageal submucosal mucus glands. a In patients with RE the thickness of the mucus buffer layer is significantly impaired and overwhelmed by erosive power of acid and pepsin within the gastroesophageal refluxate, resulting in injury penetrating through the multilayered squamous epithelium. b Administration of rabeprazole results in augmented mucus buffer layer thickness as well as diminished erosive power of acid and pepsin within the gastroesophageal refluxate, resulting in healing of erosive mucosal changes
The esophageal mucin-secretion-enhancing property of rabeprazole in addition to inhibition of gastric acid secretion could be of great value in healing of erosive esophagitis (Fig. 1b).
Whether the mucin-enhancing property of rabeprazole is unique to its chemical structure or shared by other proton pump inhibitors (PPIs) in humans remains to be explored [22]. Of note, in an animal study, rabeprazole, but not omeprazole or lansoprazole, augmented gastric mucin production in an experimental setting [25].
Since rabeprazole was administered for 8 weeks, some effect on mucin production could have been related to increasing serum gastrin, although QD dosing in the morning usually results in negligible to mild increases in serum gastrin levels.
The importance of mucin in mucosal protection within the alimentary tract has been recently demonstrated in Muc2-deficient mice which, after losing the gene responsible for synthesis MUC2 mucin, instrumental for maintaining goblet cell integrity, spontaneously developed colitis [26].
Conclusion
Stimulation of esophageal mucin secretion, elaborated by submucosal mucous glands, after administration of rabeprazole may indicate that the mechanisms governing esophageal mucin secretion are similar to those implicated in gastric mucin output.
Enhancement of esophageal mucin secretion, the major defensive component of the esophageal pre-epithelial barrier, during rabeprazole administration, may translate into esophagoprotective potential in patients with reflux esophagitis.
Reference List
Sarosiek J, McCallum RW. Mechanisms of oesophageal mucosal defense. Best Pract Res Clin Gastroenterol. 2000;14:701–717. doi:10.1053/bega.2000.0119. PMID: 11003804.
Sarosiek J, Jensen RT, Maton PN, et al. Salivary and gastric epidermal growth factor in patients with Zollinger-Ellison syndrome: its protective potential. Am J Gastroenterol. 2000;95:1158–1165. doi:10.1111/j.1572-0241.2000.02003.x. PMID: 10811321.
Marcinkiewicz M, Namiot Z, Edmunds MC, McCallum RW, Sarosiek J. Detrimental impact of acid and pepsin on the rate of luminal release of transforming growth factor alpha. Its potential pathogenetic role in the development of reflux esophagitis. J Clin Gastroenterol. 1996;23:261–268. doi:10.1097/00004836-199612000-00005. PMID: 8957727.
Sarosiek J, Scheurich CJ, Marcinkiewicz M, McCallum RW. Enhancement of salivary esophagoprotection: rationale for a physiological approach to gastroesophageal reflux disease. Gastroenterol. 1996;110:675–681. doi:10.1053/gast.1996.v110.pm8608875. see comment. PMID: 8608875.
Namiot Z, Sarosiek J, Rourk RM, Hetzel DP, McCallum RW. Human esophageal secretion: mucosal response to luminal acid and pepsin. Gastroenterol. 1994;106:973–981. PMID: 8144002.
Vaezi MF, Singh S, Richter JE. Role of acid and duodenogastric reflux in esophageal mucosal injury: a review of animal and human studies. Gastroenterol. 1995;108:1897–1907. doi:10.1016/0016-5085(95)90156-6. PMID: 7768397.
Gerson LB, Boparai V, Ullah N, Triadafilopoulos G. Oesophageal and gastric pH profiles in patients with gastro-oesophageal reflux disease and Barrett’s oesophagus treated with proton pump inhibitors. Aliment Pharmacol Ther. 2004;20:637–643. doi:10.1111/j.1365-2036.2004.02127.x. PMID: 15352912.
Marshall RE, Anggiansah A, Manifold DK, Owen WA, Owen WJ. Effect of omeprazole 20 mg twice daily on duodenogastric and gastro-oesophageal bile reflux in Barrett’s oesophagus. Gut. 1998;43:603–606. PMID: 9824338.
Sarela AI, Hick DG, Verbeke CS, Casey JF, Guillou PJ, Clark GW. Persistent acid and bile reflux in asymptomatic patients with Barrett esophagus receiving proton pump inhibitor therapy. Arch Surg. 2004;139:547–551. doi:10.1001/archsurg.139.5.547. PMID: 15136356.
Fass R, Shapiro M, Dekel R, Sewell J. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease–where next? Aliment Pharmacol Ther. 2005;22:79–94. doi:10.1111/j.1365-2036.2005.02531.x. PMID: 16011666.
Sarosiek J, McCallum RW. What is the secretory potential of submucosal mucous glands within the human gullet in health and disease? Digestion. 1995;56(1):15–23. PMID: 7556966.
Namiot Z, Yu ZJ, Piascik R, Hetzel DP, McCallum RW, Sarosiek J. Modulatory effect of esophageal intraluminal mechanical and chemical stressors on salivary prostaglandin E2 in humans. Am J Med Sci. 1997;313:90–98. doi:10.1097/00000441-199702000-00004. PMID: 9030674.
Marcinkiewicz M, Sarosiek J, Edmunds M, Scheurich J, Weiss P, McCallum RW. Monophasic luminal release of prostaglandin E2 in patients with reflux esophagitis under the impact of acid and acid/pepsin solutions. Its potential pathogenetic significance. J Clin Gastroenterol. 1995;21:268–274. doi:10.1097/00004836-199512000-00003. PMID: 8583097.
Sarosiek J, McCallum RW. Do salivary organic components play a protective role in health and disease of the esophageal mucosa? Digestion. 1995;56(1):32–37. PMID: 7556968.
Sarosiek J, McCallum RW. What role do salivary inorganic components play in health and disease of the esophageal mucosa? Digestion. 1995;56(1):24–31. PMID: 7556967.
Majewski M, Jaworski T, Sarosiek I, et al. Significant enhancement of esophageal pre-epithelial defense by tegaserod: implications for an esophagoprotective effect. Clin Gastroenterol Hepatol. 2007;5:430–438. doi:10.1016/j.cgh.2007.01.002. PMID: 17445751.
Namiot Z, Sarosiek J, Marcinkiewicz M, Edmunds MC, McCallum RW. Declined human esophageal mucin secretion in patients with severe reflux esophagitis. Dig Dis Sci. 1994;39:2523–2529. doi:10.1007/BF02087685. PMID: 7995174.
Demeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB. Patterns of gastroesophageal reflux in health and disease. Ann Surg. 1976;184:459–470. doi:10.1097/00000658-197610000-00009. PMID: 13747.
Hirschowitz BI. A critical analysis, with appropriate controls, of gastric acid and pepsin secretion in clinical esophagitis. Gastroenterol. 1991;101:1149–1158. PMID: 1936784.
Walker V, Taylor WH. Pepsin 1 secretion in chronic peptic ulceration. Gut. 1980;21:766–771. doi:10.1136/gut.21.9.766. PMID: 6776016.
Mantle M, Allen A. A colorimetric assay for glycoproteins based on the periodic acid/Schiff stain. Biochem Soc Trans. 1978;6:607–609. PMID: 208893.
Jaworski T, Sarosiek I, Sostarich S, et al. Restorative impact of rabeprazole on gastric mucus and mucin production impairment during naproxen administration: its potential clinical significance. Dig Dis Sci. 2005;50:357–365. doi:10.1007/s10620-005-1611-3. PMID: 15745101.
Skoczylas T, Sarosiek I, Sostarich S, McElhinney C, Durham S, Sarosiek J. Significant enhancement of gastric mucin content after rabeprazole administration: its potential clinical significance in acid-related disorders. Dig Dis Sci. 2003;48:322–328. doi:10.1023/A:1021983611768. PMID: 12643610.
Sarosiek J, Rourk RM, Piascik R, Namiot Z, Hetzel DP, McCallum RW. The effect of esophageal mechanical and chemical stimuli on salivary mucin secretion in healthy individuals. Am J Med Sci. 1994;308:23–31. doi:10.1097/00000441-199407000-00006. PMID: 8010333.
Takiuchi H, Asada S, Umegaki E, Tahashi Y, Ohshiba S. Effects of proton pump inhibitors: omeprazole, lansoprazole and E-3810 on the gastric mucin. In: Proc. 10th World Congress of Gastroenterol, Los Angeles, CA; 1994;1404P. [PMID: 1629582].
Van der Sluis M, De Koning BA, De Bruijn AC, et al. Muc2-deficient mice spontaneously develop colitis, indicating that MUC2 is critical for colonic protection. Gastroenterol. 2006;131:117–129. doi:10.1053/j.gastro.2006.04.020. PMID: 16831596.
Acknowledgment
Supported by a grant from Eisai Inc. and Ortho-McNeil Janssen Scientific Affairs, LLC. The authors are indebted to Dr. Malcolm Robinson for his valuable and unbiased input during preparation and re-editing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarosiek, I., Olyaee, M., Majewski, M. et al. Significant Increase of Esophageal Mucin Secretion in Patients with Reflux Esophagitis After Healing with Rabeprazole: Its Esophagoprotective Potential. Dig Dis Sci 54, 2137–2142 (2009). https://doi.org/10.1007/s10620-008-0589-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-008-0589-z