Abstract
Current management algorithms propose pH monitoring under proton pump inhibitors (PPIs) in suspected gastroesophageal reflux disease (GERD) with insufficient treatment response, but recent observations challenge this approach because of its low yield. Aim To perform an audit of the outcomes of pH monitoring under PPI therapy in our unit, and to study the yield of additional nonacid reflux monitoring. Methods All pH monitoring studies under antireflux therapy since 1997, with or without simultaneous Bilitec® monitoring, were analyzed. Results From 1997 to 2003, 347 patients (157 men, mean age 49.4 ± 0.8 years) underwent pH studies on PPI therapy (28% half-, 67% full-, and 5% double-dose PPI) for persisting typical (53%) or atypical (75%) symptoms. In 184 patients, simultaneous Bilitec® monitoring was performed. Esophageal pH monitoring on PPI was pathological in 105 (30%) patients. Pathological pH monitoring on PPI was associated with typical reflux symptoms (64 versus 52%, P = 0.03), and a higher prevalence of persisting esophagitis (54 versus 36%, P < 0.005) and of hiatal hernia (58 versus 27%, P < 0.005). Bilitec monitoring on PPI therapy was pathological in 114 (62%) patients, of which 74 (40%) had normal pH monitoring. Adding Bilitec® increased the rate of abnormal results over pH monitoring alone, from 38% to 69% on half-dose, from 27% to 69% on full-dose, and from 0% to 38% on double-dose PPI. Conclusions The rate of abnormal pH monitoring in symptomatic GERD patients while on PPI therapy is relatively low, especially in those on double-dose PPI. Combined pH and Bilitec® monitoring significantly increased the rate of ongoing pathological reflux compared to pH alone in refractory to PPI therapy GERD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroesophageal reflux disease (GERD), defined as the presence of symptoms or lesions that can be attributed to the reflux of gastric contents into the esophagus, is a common disorder affecting up to 35–40% of the adult population [1, 2]. Proton pump inhibitors (PPIs) are the most potent agents for acid suppression, and they have brought relief to many GERD patients [3, 4]. Standard dose (once daily) of various PPIs has been established as providing symptom relief and healing of lesions in the majority of patients [3–8]. However, it has been estimated that about 30% of GERD patients remain symptomatic on standard dose of PPIs [9–13]. Of these patients, the majority will continue to experience GERD symptoms on even higher doses of PPIs [6, 14].
Current management algorithms propose pH monitoring under PPIs in patients with refractory to PPI therapy GERD, in order to assess the degree of acid suppression and determine whether continued symptoms indicate the need for more aggressive therapy [15]. However, two recent studies challenged this approach, showing that ambulatory pH monitoring in refractory to PPI therapy patients is most likely to be normal [16, 17].
Over the past few years, evidence has accumulated that nonacid reflux may be an important contributor to the persistence of symptoms on acid-suppressive therapy. Studies using combined pH and impedance monitoring in patients on PPI therapy that failed to provide symptom relief confirmed that, in up to one-third of patients, symptoms were associated with weakly acidic reflux events [18–20]. The nature of the stimulus that induces heartburn during weakly acidic reflux events has not been identified, but besides acid acting at pH above 4, bile is a potentially important contributor [21]. Esophageal perfusion with bile acids is able to induce a sensation of heartburn [22], and bile reflux has previously been implicated in the pathogenesis of heartburn in patients with pernicious anemia [23]. The Bilitec® 2000, a fiber-optic spectrophotometric probe, was developed to quantify duodeno-gastro-esophageal reflux (DGER) in an ambulatory fashion, and validation studies confirmed a good correlation between Bilitec® measurements and bile acid concentrations [24–26].
A few years ago, we demonstrated that persisting nonacid DGER, as quantified by the Bilitec®, is involved in symptoms that persist during PPI therapy [16]. Since then, we have routinely used combined pH and Bilitec monitoring on acid-suppressive therapy in the evaluation of patients with refractory heartburn symptoms.
The aim of the present study was to perform an audit of the outcome of combined pH and DGER monitoring under various levels of PPI therapy patients with refractory GERD symptoms.
Methods
Study Population
We retrospectively analyzed ambulatory pH and Bilitec® studies in patients with persisting GERD-related symptoms while on PPI therapy. In addition, the daily dose of PPI (half dose, full dose, or double dose) and the presence of typical and atypical symptoms were analyzed in all patients. In a previous short study, we only evaluated patients under full-dose PPI [16]. Heartburn and regurgitation were considered typical symptoms, whereas chest pain, dysphagia, nausea, pulmonary, and ear, nose, and throat (ENT) symptoms were considered atypical symptoms. Although most of these patients experienced partial symptom relief during PPI therapy, they are referred to as PPI-refractory patients below.
Endoscopy
All patients underwent conventional upper gastrointestinal endoscopy while they were on PPI therapy. If necessary, they were sedated for the procedure by intravenous administration of diazepam (up to 10 mg) or midazolam (up to 5 mg). During endoscopy, the presence of esophagitis was noted and graded according to the modified classification of Savary and Miller [27]. In addition, the presence and extent of a hiatal hernia and Barrett’s esophagus were noted.
Ambulatory pH Monitoring
Ambulatory esophageal pH monitoring was performed using an antimony pH electrode with a separate skin reference electrode (Synectics Medical, Stockholm, Sweden). The data were stored on a portable digital recorder (Digitrapper Mk III, Synectics Medical, Stockholm, Sweden). Before each study, the pH probe was calibrated in buffer solutions of pH 7 and 1. The probe was located 5 cm proximal to the lower esophageal sphincter (LES). An episode of acid reflux was defined as a decrease in esophageal pH to less than 4 for more than 10 s [28, 29].
Measurement of Duodeno-Gastro-Esophageal Reflux
The fiber-optic spectrophotometer Bilitec® 2000 (Synectics, Stockholm, Sweden) was used to quantify DGER. The system consists of a miniaturized probe of 1.5 mm diameter that carries light signals into the esophagus and back via a plastic fiber-optic bundle. Before each study, the probe was calibrated in water. The probe was located 5 cm proximal to the LES. An episode of DGER was defined as an increase in esophageal bilirubin absorbance > 0.14 for more than 10 s [28, 29].
Study Protocol
All patients filled out a detailed questionnaire about symptoms and underwent an upper gastrointestinal endoscopy, followed by stationary esophageal manometry. Ambulatory 24-h esophageal pH with or without Bilitec® monitoring was performed on one of the next 4 days. Treatment with PPI daily was continued; all other drugs potentially affecting gastrointestinal motility and gastrointestinal secretion were discontinued at least 1 week prior to the study.
Probes for assessing acid and DGER were introduced via a nasal orifice into the esophagus 5-cm proximal to the LES, defined by previous stationary esophageal manometry. The probes were then attached with adhesive tape to the subject’s nose and cheek. As a final security check, appropriate positioning in the esophagus was confirmed by brief fluoroscopy. Data collection devices were connected to the probes and worn in a belt on the patient’s waist. Registration of acid or DGER lasted for approximately 22 h, after which the probes were removed and the data transferred to a personal computer for analysis. Patients recorded the time of food or fluid consumption and posture changes on a diary card. They were instructed to stay upright during the daytime. During the recording time, only liquid meals (200 mL Nutridrink®; 300 kcal: 13% proteins, 48% carbohydrates, and 39% lipids; Nutricia, Belgium), not interfering with Bilitec® monitoring were used [28, 29]. Patients were asked to preferably drink water and to avoid coffee, tea, and fruit juices during the recording. Patients were instructed to indicate the occurrence of typical and atypical symptoms by pressing a marker button on the data collection device.
Data Analysis
The data were analyzed with the aid of commercially available software (Gastrosoft Inc. Synectics Medical, Irvine, TX) and acid and duodenal reflux were quantified separately. Previously, we established normal values for ambulatory pH and Bilitec® monitoring at our center [28, 29]. Upper limits of normal acid and DGER exposure (95th percentile) in healthy volunteers at our center are: percentage total time pH < 4 = 4.7%, and percentage total time bilirubin absorbance > 0.14 = 4.6% Pathological acid reflux is present when intraesophageal pH is below 4 for more than 4% of the time. Pathological DGER is present when intraesophageal bilirubin absorbance is above 0.14 for more than 4.6% of the time [28].
For each symptom episode indicated by the patient, the minimal pH value and the maximal bilirubin absorbance value in a preceding 2-min interval were calculated [30]. Pathological acid reflux was defined as a drop of pH below 4.0 and pathological DGER as bilirubin absorbance > 0.14. The symptom index (SI) was calculated for each patient in relation to both acid and DGER episodes. For acid reflux the SI was calculated as the number of symptoms with pH < 4 divided by the total number of symptoms, multiplied by 100%. The SI for DGER was calculated by the formula: number of symptoms with bilirubin absorbance more than 0.14 divided by the total number of symptoms multiplied by 100%. A positive SI was defined if >50% of the symptoms were associated with pathological reflux.
Statistical Analysis
Values are expressed as mean ± standard error of the mean (SEM). Correlations between pH monitoring and PPI dose, demographics, symptom pattern (typical and atypical symptoms), and endoscopic findings (presence of esophagitis and hiatal hernia) were analyzed using Student’s t-test, or chi-square testing wherever appropriate. P-values < 0.05 were considered to be significant.
Results
Patient Characteristics
Over a 4-year period, 347 patients (157 men, mean age 49.4 ± 0.8 years), referred for poorly responsive reflux symptoms, underwent a pH monitoring under PPI therapy. In 184 patients simultaneous Bilitec® monitoring was also performed.
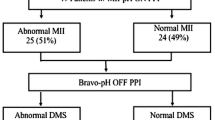
Ninety-six (28%) patients were treated with half PPI dose, 232 (67%) with full PPI dose, and nineteen (5%) with double PPI dose. The low rate of double-dose PPI usage reflects the absence of reimbursement for PPIs above full dose in Belgium. The symptoms of the patients under PPI therapy are summarized in Fig. 1. One hundred and eighty-four patients (53%) had typical symptoms, and 259 patients (75%) had extraesophageal symptoms. In spite of PPI therapy, 42% of the patients continued to experience heartburn, 26% regurgitation, 22% chest pain, 28% ENT symptoms, and 16.5% pulmonary symptoms.
Endoscopy
Upper gastrointestinal endoscopy revealed no esophagitis in 251 (72.3%) patients, and grade 1, 2, 3, and 4 esophagitis, in 61 (17.6%), 27 (7.8%), 3 (0.9%), and 5 (1.4%) patients, respectively. Barrett’s esophagus was found in 17 (0.05%) patients. Eighty-three (24%) patients had an esophageal hernia with a size that ranged in length from 2 to 6 cm (average 1.8 ± 0.14 cm).
Esophageal pH Monitoring
During PPI therapy, ongoing pathological acid exposure was present in 105 (30%) patients. The mean age was 51.6 ± 1.5 years, with 54 men. The age and gender distribution of the patients with pathological or normal pH monitoring were not significantly different (Table 1). The prevalence of persisting erosive esophagitis was significantly higher in patients with pathological pH compared to those without pathological acid reflux (54% versus 36%, P < 0.005). Patients with abnormal pH monitoring had a significantly higher prevalence of hiatal hernia compared to those with normal one (58% versus 27%, P < 0.005) (Table 1).
The prevalence of pathological pH monitoring tended to be lower in patients on double PPI dose compared to those on half and full PPI dose (16% versus 31% versus 32%, respectively), but this difference did not reach statistical significance (Fig. 2). The prevalence of pathological pH monitoring did not differ significantly in patients with or without Barrett’s esophagus (41 versus 34%, NS).
Table 2 summarizes the prevalence of typical and atypical symptoms in patients with abnormal or normal pH monitoring. Persisting acid reflux was associated with higher prevalence of typical symptoms in general (62% versus 49%, P = 0.03), and particularly of heartburn (50% versus 39%, P = 0.04). Although the prevalence of atypical symptoms in general did not significantly differ between patients with abnormal and normal pH monitoring (72% versus 76%, NS), patients with an abnormal pH monitoring had a lower probability of having ENT symptoms (20% versus 31%, P = 0.02).
Simultaneous pH and Bilitec® Monitoring
One hundred and eighty-four patients underwent simultaneous pH and Bilitec® monitoring while on PPI therapy (32 on half dose, 139 on full dose, and 13 on double dose). Ongoing pathological acid exposure was present in 49 (27%) patients, and pathological DGER was found in 114 (62%) patients. Seventy-four (40%) patients with pathological Bilitec® monitoring had a normal pH monitoring. The prevalence of pathological acid, DGER, or both, is summarized in Fig. 3. Acid exposure under PPI was positive in only 27%, but adding Bilitec® monitoring increased the diagnoses of persistent reflux to 67%.
Table 3 and Fig. 4 summarize the prevalence of pathological pH and Bilitec® monitoring in patients treated with different PPI doses. Adding Bilitec® monitoring, the diagnoses of persistent reflux increased from 37% to 68% on half dose, from 27% to 69% on full dose, and from 0% to 38% on double dose (Table 3, Fig. 4).
Symptoms and Reflux Episodes
The symptom marker was used by 73 patients, who indicated a total of 415 symptom episodes. Patients pushed the symptom marker button on 41 (10%) occasions in association with acid reflux alone, on 18 (4%) occasions in association with DGER, and on 70 (17%) in association with combined acid and DGER reflux. A positive SI for acid reflux was found in 14 (19%) patients, for DGER in 6 (8%) patients, and for mixed reflux in 4 (5%) patients. Of those with a positive symptom index, nine were referred for surgery, six were managed medically, and for the others no documented follow-up was available in our institution.
Discussion
Acid suppression is considered the most appropriate current therapy for patients with GERD [3, 4, 15, 31]. The available PPIs have been shown to provide high healing rates and symptom relief when used at prescription dosages [3–8, 32]. Although GERD that is refractory to medical treatment is considered relatively uncommon [15], a recent review estimated that the overall prevalence of PPI failure is approximately 30% [13]. In up to half of these patients, persisting acid reflux is considered the origin of symptoms [9–14] and pH testing under PPI treatment to ensure persisting esophageal acid exposure has been suggested [15].
Endoscopy was normal in the majority of patients, consistent with the healing properties of PPI therapy. Nevertheless, a small fraction of patients had persisting erosive esophagitis, and persisting high-grade esophagitis was found in eight patients. The persistence of esophagitis is relatively rare but has been documented previously in the literature [9–14, 16]. In the patients with refractory high-grade esophagitis, it is unclear whether this was due to a more severe spectrum of GERD, decreased sensitivity to PPI therapy or inadequate treatment compliance. Assessing the value of pH monitoring in patients with GERD symptoms refractory to PPI therapy, we found that the overall rate of abnormal results of this technique is relatively low. In keeping with previous reports [16, 17, 30], only 30% of refractory GERD patients had pathological acid exposure of the distal esophagus while the PPI therapy was being continued.
Analyzing the factors that may predictive of pathological pH testing under PPI therapy, we found that there was a significant relationship between the presence of a hiatal hernia and persisting abnormal pH monitoring. Hiatal hernia is considered to play a key role in the pathogenesis of GERD and patients with a hiatal hernia have higher acid exposures than those without hernia [33, 34]. Indeed, our study showed that the likelihood of persisting acid reflux is higher in symptomatic GERD patients on therapy with hiatal hernia compared to those without hernia. The presence of persisting esophagitis was another factor that was significantly associated with pathological pH monitoring in patients with symptoms refractory to PPI therapy. It has previously been shown that the proportion of the 24 h period with esophageal pH < 4 increased progressively from endoscopy-negative GERD patients through those with worsening grades of esophagitis [35]. Thus, we observed that patients with persisting symptoms and persisting erosive esophagitis under PPI therapy had a significantly higher probability of having a pathological pH testing compared to those without esophagitis.
The persistence of typical GERD symptoms, especially heartburn, was correlated with a higher prevalence of pathological pH monitoring during PPI therapy. Heartburn is a symptom that has traditionally been considered an acid-mediated event, and the literature suggests that acid exposure is normalized in the majority of patients who respond favorably to medical therapy [36, 37]. Our results are consistent with these observations, showing that patients with persistent heartburn while on PPI treatment were more likely to have an abnormal pH testing than those without heartburn. We also found that the majority of patients with persistent ENT symptoms were more likely to have a normal pH monitoring. Although someone could argue that this lack of association with ENT symptoms is due to the use of only distal pH probe, we recently showed that proximal pH monitoring rarely identified patients with pathological proximal acid exposure who would be considered normal based on distal pH monitoring alone [38].
Our patients used various doses of PPIs and we found that the yield of pH monitoring was higher in patients treated with half and full PPI doses compared to those on double PPI dose. The yield of pH monitoring was considerable low in patients who failed PPI twice daily, being positive in only 16% of patients. Our results are in accordance with observations of a recent study showing that the likelihood of an abnormal pH testing for symptomatic GERD patients on double PPI dose was 7% [17]. These results question the clinical usefulness of ambulatory pH monitoring in patients with persistent symptoms while on PPI therapy, especially in those on double dose.
Among the factors that might play a role in why a patient remains symptomatic while on aggressive acid suppression, persisting DGER has previously been shown to be involved in the PPIs refractoriness [30]. In the subgroup of patients with simultaneous pH and Bilitec® monitoring, we studied the yield of additional nonacid reflux monitoring. Ambulatory pH monitoring under PPI therapy was pathological in only 27% of these patients, whereas combined pH and Bilitec® monitoring allowed documentation of persistent reflux in 67% of the patients. Thus, the addition of a Bilitec® probe resulted in a considerable overall diagnostic gain of 40%. Although the majority of symptom episodes indicated by the symptom marker remained unexplained, addition of DGER monitoring also increased the number of episodes that were attributable to a reflux event.
An increase in the rate of abnormal results of adding Bilitec® probe to pH monitoring was present at each of the used PPI doses. Although acid suppression with PPIs decreased both acid and nonacid reflux in a dose-dependant way, the available literature suggests that PPIs are not as effective at normalizing DGER compared with their effect on acid reflux [30, 39–41]. Our results show that increasing the PPI dose from half to double will normalize the pH parameters in the majority of patients. Although the proportion of patients with DGER decreased while the PPI dose was increased, persisting DGER was still present in 38% of patients treated with double PPI dose.
Recent studies using intraluminal impedance with a pH sensor showed persistent nonacid reflux in patients under PPI therapy [18–20]. The present study confirms evidence for an association between DGER and PPI failure at least in a proportion of symptomatic patients under PPI. The nature and origin of persisting symptoms in the rest of the patients remained unclear, and the involvement of mechanisms other than acid or nonacid reflux have to be considered [9, 21, 42].
In conclusion, we showed that the rate of abnormal results of pH monitoring in symptomatic GERD patients while on PPI therapy is relatively low, especially in those on double PPI dose. Combined pH and Bilitec® monitoring significantly increased the diagnostic yield of ongoing pathological reflux compared to pH alone in refractory to PPI therapy GERD patients.
References
Isolauri J, Laippala P (1995) Prevalence of symptoms suggestive of gastroesophageal reflux disease in an adult population. Ann Med 27:67–70
Spechler SJ (1992) Epidemiology and natural history of gastroesophageal reflux disease. Digestion 51(suppl 1):24–29
Dehn TCB, Sheperd HA, Colin-Jones D et al (1990) Double blind comparison of omeprazole versus cimetidine in the treatment of symptomatic erosive reflux oesophagitis, assessed endoscopically, histologically and by 24 h pH monitoring. Gut 31:509–513
Hetzel DJ, Dent J, Reed WD et al (1988) Healing and relapse of severe peptic esophagitis after treatment with omeprazole. Gastroenterology 95:903–912
Sontag SJ, Hirwhowitz BI, Holt S et al (1992) Two doses of omeprazole versus placebo in symptomatic erosive esophagitis: the U.S. multicenter study. Gastroenterology 102:108–118
Klinkenberg-Knol EC, Festen HP, Jansen JB et al (1994) Long-term treatment with omeprazole for refractory reflux esophagitis: efficacy and safety. Ann Intern Med 121:161–167
Earnest D, Dorsch E, Jones J et al (1998) A placebo-controlled dose-ranging study of lansoprazole in the management of reflux esophagitis. Am J Gastroenterol 93:238–243
Chiba N, De Gara CJ, Wilkonson JM et al (1997) Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology 112:1798–1810
Holloway RH, Dent J, Narielvala F et al (1996) Relation between oesophageal acid exposure and healing of oesophagitis with omeprazole. Gut 38:649–654
Klinkenberg-Knol EC, Meuwissen SGM (1990) Combined gastric and esophageal 24-h pH monitoring and esophageal manometry in patients with reflux disease resistant to treatment with omeprazole. Aliment Pharmacol Ther 4:485–495
Katzka DA, Paoletti V, Leite L et al (1996) Prolonged ambulatory pH monitoring in patients with persistent gastroesophageal reflux disease symptoms: testing while on therapy identifies the need for more aggressive anti-reflux therapy. Am J Gastroenterol 91:2110–2113
Fass R, Mackel C, Sampliner RE (1994) 24-h pH monitoring in symptomatic patients without erosive esophagitis who did not respond to antireflux treatment. J Clin Gastroenterol 19:97–99
Fass R, Shapiro M, Dekel R, Sewell J (2005) Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease-where next? Aliment Pharmacol Ther 22:79–94
Leite LP, Johnston BT, Just RJ et al (1996) Persistent acid secretion during omeprazole therapy: a study of gastric acid profiles in patients demonstrating failure of omeprazole therapy. Am J Gastroenterol 9:1527–1531
DeVault KR, Castell DO (2005) Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol 100:190–200
Bautista JM, Wong WM, Pulliam G, Esquivel RF, Fass R (2005) The value of ambulatory 24 hr esophageal pH monitoring in clinical practice in patients who were referred with persistent gastroesophageal reflux disease (GERD)-related symptoms while on standard dose anti-reflux medications. Dig Dis Sci 50(10):1909–1915
Charbel S, Khandwala F, Vaezi M (2005) The role of esophageal pH monitoring in symptomatic patients on PPI therapy. Am J Gastroenterol 100:283–289
Vela M, Camacho-Lobato L, Srinivasan R, et al (2001) Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology 120:1599–1606
Zerbib F, Roman S, Ropert A, des Varannes SB, Pouderoux P, Chaput U, Mion F, Vérin E, Galmiche JP, Sifrim D (2006) Esophageal pH-impedance monitoring and symptom analysis in GERD: a study in patients off and on therapy. Am J Gastroenterol 101(9):1956–1963
Mainie I, Tutuian R, Shay S, Vela M, Zhang X, Sifrim D, Castell DO (2006) Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut 55(10):1398–1402
Tack J (2006) Review article: the role of bile and pepsin in the pathophysiology and treatment of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 24 Suppl 2:10–6
Siddiqui A, Rodriguez-Stanley S, Zubaidi S, Miner PB Jr (2005) Esophageal visceral sensitivity to bile salts in patients with functional heartburn and in healthy control subjects. Dig Dis Sci 50(1):81–85
Orlando RC, Bozymski EM (1973) Heartburn in pernicious anemia. Aconsequence of bile reflux. N Engl J Med 289:522–523
Bechi P, Paucciani F, Baldini F, et al (1993) Long-term ambulatory enterogastric reflux monitoring. Validation of a new fiberoptic technique. Dig Dis Sci 38:1297–1306
Vaezi MF, LaCamera RG, Richter JE (1994) Bilitec 2000 ambulatory duodenogastric reflux monitoring system. Studies on its validation and limitations. Am J Phys 267:G1050–1057
Stipa F, Stein HJ, Feussner H et al (1997) Assessment of non-acidic esophageal reflux: comparison between long-term reflux aspiration test and fiberoptic bilirubin monitoring. Dis Esophagus 10:24–28
Tack J, Koek G, Demedts I, Sifrim D, Janssens J (2004) Gastroesophageal reflux disease poorly responsive to single-dose proton pump inhibitors in patients without Barrett’s esophagus: acidreflux, bile reflux, or both? Am J Gastroenterol 99:981–988
Savary M, Miller G (1977) L’oesophage. Manuel et Atlas d’Edoscopie. Verlag Gassmann, Solothurn, Switzerland
Cuomo R, Koek G, Sifrim D et al (2001) Analysis of ambulatory duodeno-gastro-esophageal reflux monitoring. Dig Dis Sci 45:246–239
Tack J, Koek GH, Bisschops R et al (2003) Dietary restrictions during ambulatory monitoring of duodeno-gastro-esophageal reflux. Dig Dis Sci 48:1213–1220
Klinkenberg-Knol E, Nelis F, Dent J et al (2000) Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety and influence on gastric mucosa. Gastroenterology 118:661–669
Castell DO, Kahrilas PJ, Richter JE et al (2002) Esomeprazole (40 mg) compared with lansoprazole (30 mg) in the treatment of erosive esophagitis. Am J Gastroenterol 97:575–583
Karhilas PJ, Lin S, Chen J et al (1999) The effect of hiatus hernia on gastro-oesophageal junction pressure. Gut 94:476–482
Cameron AJ (1999) Barrett’s esophagus: prevalence and size of hiatal hernia. Am J Gastroenterol 94:2054–2059
Fiorucci S, Santucci L, Chiuchiu S et al (1992) Gastric acidity and gastroesophageal reflux patterns in patients with esophagitis. Gastroenterology 103:855–861
Carlsson R, Dent J, Bolling-Sternevald E et al (1998) The usefulness of a structural questionnaire in the assessment of symptomatic gastroesophageal reflux disease. Scand J Gastroenterol 33:1023–1029
Bytzer P (2003) Goal of therapy and guidelines for treatment success in symptomatic gastroesophageal reflux disease patients. Am J Gastroenterol 98(suppl):S31–S39
Cool M, Poelmans J, Feenstra L, Tack J (2004) Characteristics and clinical relevance of proximal esophageal pH monitoring. Am J Gastroenterol 99:2317–2323
Champion G, Richter JE, Vaezi MF et al (1994) Duodeno-gastro-oesophageal reflux: relationship to pH and importance in Barrett’s oesophagus. Gastroenterology 107:747–754
Marshall RE, Anggiansah A, Manifold DK et al (1998) Effect of omeprazole 20 mg twice daily on duodenogastric and gastro-oesophageal bile reflux in Barrett’s oesophagus. Gut 43:603–606
Menges M, Muller M, Zeitz M (2001) Increased acid and bile reflux in Barrett’s esophagus compared to reflux esophagitis, and effect of proton pump inhibitor therapy. Am J Gastroenterol 96:331–337
Fass R, Naliboff B, Higa L et al (1998) Differential effect of long-term esophageal acid exposure on mechanosensitivity and chemosensitivity in humans. Gastroenterology 115:1363–1373
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karamanolis, G., Vanuytsel, T., Sifrim, D. et al. Yield of 24-Hour Esophageal pH and Bilitec Monitoring in Patients with Persisting Symptoms on PPI Therapy. Dig Dis Sci 53, 2387–2393 (2008). https://doi.org/10.1007/s10620-007-0186-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-007-0186-6