Abstract
The relationship between Helicobacter pylori infection and reflux-induced esophageal diseased is controversial. We examined esophageal disease severity in patients with columnar-lined esophagus and compared results between patients with and without Helicobacter pylori infection. Medical records of 1000 patients diagnosed with columnar-lined esophagus were examined. Endoscopic and histological findings of reflux-induced esophageal disease were compared between H. pylori-positive and H. pylori-negative patients. Four hundred twenty-nine patients (42.9%) showed evidence of H. pylori status, of whom 239 (55.7%) were positive and 190 (44.3%) negative. There were no significant differences in length of columnar-lined segment (P = 0.305), frequency of associated esophagitis (P = 0.583), or presence of gastroduodenal inflammation (P = 0.335, P = 0.131) between the two groups. Histological grade of esophageal disease severity was similar between them, with no statistically significant differences (P = 0.231).
We conclude that in patients with established columnar-lined esophagus, there appears to be no difference in severity of reflux-induced esophageal disease between those with and those without H. pylori infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The association between Helicobacter pylori (HP) and reflux-induced esophageal disease is controversial. Whereas some authors have proposed various mechanisms by which HP may be detrimental to esophageal mucosa [1–4], others have not been able to demonstrate such a relationship and some have suggested that HP may even be protective for this type of disease [5, 6].
There is a well-documented relationship among HP infection, peptic ulcer disease (PUD), and noncardia gastric cancer [7–11], and the vast decrease in prevalence of HP infection over the last 20–30 years has coincided with a rapid decrease in these diseases. Over this same time frame, however, the incidence of gastroesophageal reflux disease (GERD) and esophageal adenocarcinoma has risen dramatically and has led many authors to speculate on the possible association between this and this observed decrease in HP prevalence [12–15].
Some studies have also suggested that patients with previous PUD who have their HP eradicated are much more likely to develop GERD at a later stage [16] and support the theory that HP may be playing some protective role against the development of reflux-induced esophageal pathology.
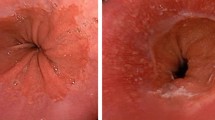
Many studies have looked at the effect of HP on gastric acid output [17–19], which has led to theories of mechanisms of subsequent effect on esophageal mucosa. Authors have suggested that the distribution of HP within the stomach, with resultant varying patterns of gastritis, has different effects on gastric acid output. A predominant antral distribution may cause an increase in acid production via its effect on somatostatin levels, whereas a corpus distribution resulting in chronic gastric atrophy may lead to a subsequent reduction in acid production. There appear to be very few studies, however, comparing this relationship and the resultant effect on esophageal mucosa directly. There is also little known about the direct effect of HP on esophageal mucosa itself, although some studies have observed HP only adhering to areas of gastric metaplasia in esophageal mucosa, and not to intestinal metaplasia, and have therefore concluded that it is unlikely to have any direct malignant potential [20].
The aim of this study was to examine the prevalence of HP infection in a cohort of patients with established columnar-lined esophagus (CLO) and ascertain any differences in severity of their esophageal disease compared to patients who were HP negative (HP−).
Patients and methods
Medical records of 1000 patients diagnosed with CLO and registered with the U.K. National Barrett’s Esophagus Registry were examined. Information was extracted and entered onto the research database situated at the Royal Free Hospital, London.
Specific medical information including patient demographics—age, gender, follow-up—and endoscopic and histological findings were used for this study and patients were divided into two cohorts based on documented HP status as defined below.
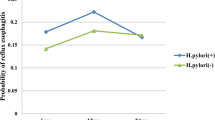
Data collected on smoking habits and alcohol consumption were analyzed as a comparison between cohorts. Scores were calculated based on frequency of consumption of alcohol and usage of tobacco as used in previous studies [21]. Severity of esophageal disease on histology was based on grade reported by the pathologists and assumed a sequence of progression from Campylobacter-like organism (CLO) ± intestinal metaplasia (IM) to indefinite dysplasia (ID) to low-grade dysplasia (LGD) to high-grade dysplasia (HGD) to adenocarcinoma (AC) (see Fig. 1).
Data were examined and classified as the most pathological findings for that patient. On endoscopy this meant the greatest length of CLO recorded and the presence of esophagitis, gastritis, or duodenitis if documented at any stage for those patients; and on histology the most severe pathology attained as per Fig. 1. This was considered a more useful indication of disease severity than follow-up endpoint to negate the process of any possible disease regression that may have resulted over the follow-up period due to pharmacological intervention.
All endoscopic and histological findings used in the analysis were documented after HP status for the patient was noted.
Definition of the cohorts
Two cohorts were defined from information extracted from the database.
Helicobacter pylori positive (HP+)
Patients with documented evidence of HP infection on CLO test, breath test, or serology or observed at histology (stomach or esophagus), and with no subsequent documentation of HP− status were taken as being HP+ for the purpose of the study. Patients who had undergone eradication therapy but who on repeat testing remained HP+ (i.e., unsuccessful eradication) were also included in this cohort.
Helicobacter pylori negative (HP−)
All patients with documented evidence of HP− status on CLO, breath test, or serology were included in the HP− cohort, except for patients who had received successful eradication therapy having been previously noted to be HP+. Patients who had received eradication therapy but had no posttreatment status documented were also excluded from the study.
Demographic, endoscopic, and histological data were compared between the HP+ and the HP− groups, with statistical analyses undertaken using SPSS version 11.0. The chi-square test of association was used to compare categorical data between the groups, and the independent t-test and Mann-Whitney U to examine differences between continuous variables.
Results
Prevalence of HP infection
Of the 1000 patients examined, 429 (42.9%) had documented evidence of HP status. Of these, 239 (55.7%) had evidence of being HP+ or had documentation of having had eradication therapy at some time over their follow-up. Sixty-six (27.6%) had eradication therapy, with 20 having a documented HP− status posttreatment; 6 remained HP+ and 40 had no HP status documented in the notes posttreatment.
HP+ cohort
One hundred seventy-nine patients were included in the HP+ cohort. Seventy-two (40%) were diagnosed as being HP+ on their first endoscopy that was diagnostic for CLO; 99 (55%) were diagnosed after their initial diagnosis of CLO (an average of 5.36 years postdiagnosis) and 8 (5%) before their diagnosis.
HP− cohort
One hundred ninety patients had documented evidence of being HP− (not including the 20 successfully eradicated patients). One hundred four (55%) were diagnosed on the same endoscopy as their initial diagnostic for CLO endoscopy; 68 (36%) were diagnosed after their initial diagnosis of CLO (an average of 4.71 years postdiagnosis) and 18 (9%) before their diagnosis (an average of 2.17 years before).
Comparison between HP+ and HP− Cohorts
Demographics/patient characteristics
The ratio of males to females in the HP+ group was 2.1:1 (121:57) and 1.6:1 (117:73) in the HP− group, with no significant differences between them (P = 0.199, χ2 test).
The mean age at diagnosis of CLO was also similar between the two cohorts, being 60.45 years in the HP+ group and 58.42 years in the HP− group (P = 0.148, t-test).
The mean endoscopic follow-up period was longer for the HP+ group (5.39 years) compared to the HP− group (3.35 years) (P < 0.001).
Of the patients who were diagnosed as being HP+, 48 (19.6%) were detected on CLO test alone, 49 (20.0%) on histology, 53 (21.6%) on serology, 3 (1.2%) on breath test, and the rest on a combination of these tests. Of the patients included in the HP− cohort, 124 (65.3%) were detected by CLO test alone, 52 (27.4%) on serology, 5 (2.6%) on breath test, and the rest on a combination of these tests.
There were no significant differences in smoking habits (P = 0.796, χ2) or in overall alcohol consumption (P = 0.067) between the two cohorts.
Endoscopic findings
The mean length of CLO segment at worst pathology was 6.13 cm for the HP+ group and 5.91 cm for the HP− group, with no significant differences on statistical analysis (P = 0.269, Mann-Whitney U).
There was no significant difference in the frequency of associated esophagitis (P = 0.583, χ2 test) or in associated gastroduodenal inflammation or ulceration (P = 0.335, inflammation; P = 0.131, ulceration, χ2) between the two cohorts.
Histological findings
Distribution of grades of histology at worst pathology were very similar between the two groups, with no significant differences overall (P = 0.231) or when proportions of nondysplastic and dysplastic disease were analyzed more closely (P = 0.386).
Endoscopic and histological findings are summarized in Table 1.
Discussion
Reports of the prevalence of HP infection in esophageal disease vary from 14% to 40% in GERD/esophagitis and 25% to 62% in CLO [22–27], although the prevalence of HP in esophageal adenocarcinoma seems to be much lower and reports have suggested anything from 0% to 20% [23, 25, 28]. From our study of a cohort of patients with CLO, the prevalence of HP infection in patients that had been tested was fairly high, at 55.7%. Even if the remaining 571 patients who were not tested for HP were found to be negative, this would give an overall prevalence of HP infection of 24.5%. As we would reasonably predict this to be higher, it may be that the prevalence of HP in the entire cohort would have been greater than the reported prevalence of HP infection in normal/control populations, which ranges from 17% to 36% [24, 28]. Whether it would have reached reported prevalence rates seen in patients with PUD, 48–94% [24, 28], however, seems unlikely.
Demographics and patient characteristics were similar between the two groups. Follow-up in the HP− group, however, was significantly shorter, and whether more dysplastic disease may have developed over a longer period of time is debatable. Overall, patterns of disease distribution and endoscopic findings relating to esophageal disease severity were remarkably similar between the two groups, with no significant differences in any of the parameters examined. This seems to support the theory that HP may play little or no role in the progression of reflux-induced esophageal disease. However, that the predicted high prevalence of HP infection in the entire cohort could suggest a role in the initial pathogenesis of the disease is a possibility.
An unexpected finding of this study was that the frequency of associated gastroduodenal inflammation and ulceration did not seem to be higher in the HP+ group. This may reflect the fact that the vast majority of these patients would have been on long-term acid suppression treatment and therefore would be expected to have limited clinical evidence of gastroduodenal disease. There is also evidence that HP+ patients on proton pump inhibitors or H2 receptor antagonists show a greater level of acid suppression [29, 30], an observation that has added weight to the argument that HP need not be eradicated in patients with esophageal disease.
On the other hand, long-term proton pump inhibitor therapy has also been shown consistently to alter the distribution of HP from an antral- to a corpus- or fundus-predominant pattern, an alteration that enhances the progress of atrophic gastritis and thus the risk of gastric cancer [31].
Whether or not to treat HP infection in these patients, therefore, is still controversial and there remains to be any current consensus over this. Interestingly, in our study, 571 of 1000 (57.1%) patients with CLO were not tested for HP at any time over their follow-up, and of those who were, only 27.6% of patients who were HP+ underwent eradication therapy.
Conclusion
In this study of patients with established CLO, there were no significant differences in esophageal disease severity between those who were HP+ and those who were HP−.
References
Lee JM, O’Morain CA (1998) Different management for Helicobacter pylori positive and negative patients with gastro-oesophageal reflux disease? Gut 43(Suppl 1):S14–S20
Fink SM et al. (1984) The association of histologic gastritis with gastroesophageal reflux and delayed gastric emptying. J Clin Gastroenterol 6:301–309
Vicari J, Falk GW, Richter JE (1997) Helicobacter pylori and acid peptic disorders of the esophagus: is it conceivable? Am J Gastroenterol 92:1097–1102
Boyd EJ (1996) The prevalence of esophagitis in patients with duodenal ulcer or ulcer-like dyspepsia. Am J Gastroenterol 91:1539–1543
Labenz J, Malfertheiner P (1997) Helicobacter pylori in gastro-oesophageal reflux disease: Causal agent, independent or protective factor? Gut 41:277–280
Hirschl AM, Schulze K, Hentsche E (1989) Serological, microbiological and clinical results of a 43 months follow-up after successful eradication of H. pylori in duodenal ulcer disease. Am J Gastroenterol 89:1374
Rauws EA, Tytgat GN (1990) Cure of duodenal ulcer associated with eradication of Helicobacter pylori. Lancet 335:1233–1235
Parsonnet J, et al. (1991) Helicobacter pylori infection and the risk of gastric carcinoma. N Engl J Med 325:1127–1131
Axon A, Forman D (1997) Helicobacter gastroduodenitis: a serious infectious disease. BMJ 314:1430–431
Nomura A, Stemmermann GN, Chyou PH, Perez-Perez GI, Blaser MJ (1994) Helicobacter pylori infection and the risk for duodenal and gastric ulceration. Ann Intern Med 120:977–981
Uemura N, et al. (2001) Helicobacter pylori infection and the development of gastric cancer. N Engl J Med 345:784–789
Richter JE (2001) H pylori: the bug is not all bad. Gut 49:319–320
Blaser MJ (1999) Hypothesis: the changing relationships of Helicobacter pylori and humans: implications for health and disease. J Infect Dis 179:1523–1530
Sehiguchi T, Shirota T, Horikoshi T (1996) Helicobacter pylori infection and severity of reflux oesophagitis. Gastroenterology 110:A755
Grebenev AL (1994) Helicobacter pylori (Hp) and reflux oesophagitis. Gastroenterology 89:A1372
Labenz J, et al. (1997) Curing Helicobacter pylori infection in patients with duodenal ulcer may provoke reflux esophagitis. Gastroenterology 112:1442–1447
Levi S, et al. (1989) Campylobacter pylori and duodenal ulcers: the gastrin link. Lancet 1:1167–1168
Smith JT, et al. (1990) Inappropriate hypergastrinaemia in asymptomatic healthy subjects infected with Helicobacter pylori. Gut 31:522–525
el Omar EM, et al. (1995) Helicobacter pylori infection and abnormalities of acid secretion in patients with duodenal ulcer disease. Gastroenterology 109:681–691
Sharma VK, Demian SE, Taillon D, Vasudeva R, Howden CW (1999) Examination of tissue distribution of Helicobacter pylori within columnar-lined esophagus. Dig Dis Sci 44:1165–1168
Caygill CP, et al. (2002) Lifestyle factors and Barrett’s esophagus. Am J Gastroenterol 97:1328–1331
Rugge M, et al. (2001) The phenotype of gastric mucosa coexisting with Barrett’s oesophagus. J Clin Pathol 54:456–460
Oberg S, et al. (1999) Helicobacter pylori is not associated with the manifestations of gastroesophageal reflux disease. Arch Surg 134:722–726
Newton M, Bryan R, Burnham WR, Kamm MA (1997) Evaluation of Helicobacter pylori in reflux oesophagitis and Barrett’s oesophagus. Gut 40:9–13
Henihan RD, et al. (1998) Barrett’s esophagus and the presence of Helicobacter pylori. Am J Gastroenterol 93:542–546
Loffeld RJ, Ten Tije BJ, Arends JW (1992) Prevalence and significance of Helicobacter pylori in patients with Barrett’s esophagus. Am J Gastroenterol 87:1598–1600
Hackelsberger A, et al. (1998) The prevalence of Helicobacter pylori gastritis in patients with reflux oesophagitis: a case-control study. Eur J Gastroenterol Hepatol 10:465–468
Grimley CE, Holder RL, Loft DE, et al. (1999) Helicobacter pylori-associated antibodies in patients with duodenal ulcer, gastric and oesophageal adenocarcinoma. Eur J Gastro Hepatol 11:503–509
Verdu EF, et al. (1995) Effect of Helicobacter pylori status on intragastric pH during treatment with omeprazole. Gut 36:539–543
Labenz J, et al. (1996) Helicobacter pylori augments the pH-increasing effect of omeprazole in patients with duodenal ulcer. Gastroenterology 110:725–732
Kuipers EJ, et al. (1996) Atrophic gastritis and Helicobacter pylori infection in patients with reflux esophagitis treated with omeprazole or fundoplication. N Engl J Med 334:1018–1022
Acknowledgments
We are very grateful to the registrants and registering centers who made this study possible and to the following, who provide financial support for the registry: The Barrett’s Oesophagus Foundation, The Wexham Gastrointestinal Trust, The Childwick trust, The R. L. St. J. Harmsworth Memorial Research Fund, and The David and Frederick Barclay Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramus, J.R., Gatenby, P.A.C., Caygill, C.P.J. et al. Helicobacter pylori Infection and Severity of Reflux-Induced Esophageal Disease in a Cohort of Patients with Columnar-Lined Esophagus. Dig Dis Sci 52, 2821–2825 (2007). https://doi.org/10.1007/s10620-006-9706-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9706-z