Abstract
Oxidative stress leads to chronic liver damage. Silybin has been conjugated with vitamin E and phospholipids to improve its antioxidant activity. Eighty-five patients were divided into 2 groups: those affected by nonalcoholic fatty liver disease (group A) and those with HCV-related chronic hepatitis associated with nonalcoholic fatty liver disease (group B), nonresponders to treatment. The treatment consisted of silybin/vitamin E/phospholipids. After treatment, group A showed a significant reduction in ultrasonographic scores for liver steatosis. Liver enzyme levels, hyperinsulinemia, and indexes of liver fibrosis showed an improvement in treated individuals. A significant correlation among indexes of fibrosis, body mass index, insulinemia, plasma levels of transforming growth factor-β, tumor necrosis factor-α, degree of steatosis, and γ-glutamyl transpeptidase was observed. Our data suggest that silybin conjugated with vitamin E and phospholipids could be used as a complementary approach to the treatment of patients with chronic liver damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of complementary drugs or alternative medicine for the treatment of chronic liver damage is emerging in many countries. It has recently been suggested that in the future a therapeutic approach to chronic liver disease will consist of a number of “complementary” therapeutic approaches considering the multitude of the pathogenic mechanisms [1, 2]. The spectrum of liver damage ranges from simple steatosis to cirrhosis or hepatocellular carcinoma (HCC). Fatty liver is a condition that is generally a consequence of ethanol abuse. However, nonalcoholic fatty liver disease (NAFLD) in recent years has become a pathological condition of increasing importance, affecting about 20% of the adult population in industrialized countries [3, 4]. This type of chronic liver damage may occur as a “primary” condition that is generally associated with obesity and metabolic disorders, such as insulin resistance or diabetes mellitus, dyslipidemia, arterial hypertension, or visceral obesity. However, it may also be a complication of other causes, such as chronic hepatitis C virus (HCV) infection [5, 6]. The contemporaneous presence of NAFLD in this later group of patients may negatively affect the progression of fibrosis and the response to antiviral treatment [7]. NAFLD may eventually evolve into cirrhosis or HCC. The pathogenic mechanisms of liver damage progression are extremely complicated and involve a series of consecutive “hits” from fatty infiltration, oxidative stress, lipid peroxidation, apoptosis, necroinflammation, and activation of stellate cells that leads to cirrhosis. Treatment of NAFLD is based on the management of associated conditions such as obesity, diabetes, and hyperlipemia. However, many drugs have also been suggested for intervention of the disease at various points along the progression. Weight reducing (phentermine, sibutramine, orlistat), antidiabetic (metformin, rosiglitazone, pioglitazone), cytoprotective, antioxidant (ursodeoxycholic acid, vitamin E, n-acetylcysteine), and other drugs have been tested for the treatment of NAFLD, but no generally accepted conclusions have been reached [8–11].
There have been a substantial number of reports published that describe the in vitro antioxidant and protective effect from liver damage of silymarin in animals and humans [12]. Silymarin protects against alcohol-induced liver diseases in humans [13–15]. Silymarin has been largely used in patients with HCV-related liver damage, even though a recent review identified only 14 properly conducted trials [16]. Investigators from the Mayo Clinic Foundation designed an open-label pilot study using silymarin in patients with nonlcoholic steatohepatitis (NASH) [17]. Silybin is the component in silymarin that acts as a free radical scavenger, suppresses the proliferation of hepatic stellate cells, and suppresses collagen deposition in vitro in humans [18–20]. Silybin is rapidly absorbed in humans when conjugated with a phytosome and vitamin E. It has a hematic peak of 2 hr and is widely distributed in plasma and tissues, which include liver, lung, stomach, skin, and prostate [21]. In this new complex silybin reduces collagen accumulation and lipid peroxidation in rats with induced fibrosis and ameliorates liver damage in patients with chronic hepatitis [22, 23]. In this open pilot preliminary study we evaluate the effects of this new pharmaceutical complex of silybin-vitamin E-phospholipids in patients with NAFLD who had or did not have contemporaneous HCV-related chronic hepatitis.
Methods
The study protocol followed the ethical guidelines of the 1975 Declaration of Helsinki and was approved by our departmental Ethics Committee. Eighty-five patients were consecutively enrolled in the study on the basis of bright liver being present on ultrasonography (US) and divided into two groups. The first group was represented by 59 patients (males/females = 39/20; median age and range, 44 and 22–76 years) affected by NAFLD and negative for other known causes of chronic liver damage (group A). Twenty-six patients (males/females = 19/7; median age and range, 51 and 20–75 years) represented the second group and were diagnosed with HCV-related chronic hepatitis associated with NAFLD (group B). Patients in group B were all HCV genotype 1b and nonresponders to previous treatments with interferon and ribavirin; this treatment had been terminated almost 1 year prior to the initiation of the study. The presence of bright liver in the enrolled patients suggested the presence of liver steatosis, graded from 0 to 3 according to Joseph et al. [24]. However, we were unable to conclusively determine the extent of liver involvement or the possible occurrence of NASH. Confirmation of HCV infection on the basis of viral genotype excluded the possibility of a fatty liver disease caused by HCV genotype 3 [25]. None of these patients were drug users or exposed to environmental toxins, such as pesticides or other xenobiotics. All enrolled patients reported a daily alcohol intake of less than 20 g throughout their lifetimes, although this was not considered an exclusion criterion as previously proposed [26]. Other associated diseases, including autoimmune, genetic, or other possible causes of chronic liver damage, were used for exclusion and based on global screening results of all patients prior to enrolment in the study.
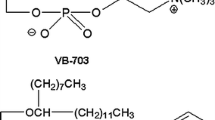
Outpatients referred to our department for their liver disease were selected over 6 consecutive months and divided into two groups using a systematic random sampling procedure. We treated 53 (39 with only NAFLD and 14 HCV-positive) patients after evaluating them based on the inclusion/exclusion criteria and obtaining written informed consent. Thirty-two patients were included in the untreated control. The main findings from the treated and untreated groups are summarized in Table 1. Cirrhosis was excluded on the basis of clinical, biochemical, and instrumental (US and upper gastrointestinal endoscopy) parameters. Diabetes was diagnosed using oral glucose load according to WHO criteria [27]. An increase in plasma cholesterol was found in 35% of the treated and untreated NAFLD patients and in 33% of the HCV-positive patients. Hypertriglyceridemia was present in approximately 35% of all groups. Patients with NAFLD and HCV had a greater increase in plasma levels of ferritin compared to patients with NAFLD only, however, this difference was not statistically significant. The treatment consisted of silybin + vitamin E + phospholipids (RealSIL, IBI; Lorenzini Pharmaceutical, Italy, RA) at a dose of four pills per day, which is double the dose used in clinical practice, for 6 months. This was followed by another 6 months of follow-up without treatment. The composition of one pill was 94 mg silybin, 194 mg phophatidilcholine, and 90 mg vitamin E.
Design of the study
The study was aimed to evaluate (a) the effect on liver damage; (b) the effects on selected pathogenic mechanisms [28, 29], including an assessment of metabolic processes and plasma levels of pro-inflammatory and anti-inflammatory cytokines; and (c) the effect on liver fibrosis markers. We tested some markers for liver fibrosis that have not been validated because recent evidence suggests that the contemporaneous determination of more than one may correlate with liver histology [30].
The design of the study was as follows. All patients were asked to follow a balanced diet based on the body weight of each patient during the entire 12-month course of the study. We also evaluated the dietary intake of each patient under the basal condition and at the end of the study using a computerized program [31]. The basal data provided the basis for determining a personalized diet for each patient. Physical activity was recommended. Compliance with the treatment (diet and drug) and adverse events were recorded at 0, 2, 4, and 6 months. At 0, 6, and 12 months we evaluated the following.
-
(1)
The body mass index (BMI; weight in kilograms/height2 in meters) was determined.
-
(2)
Liver US and plasma levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), γ-glutamyl transpeptidase (γ-GT), blood glucose, and insulin were determined using commercial kits. Insulin resistance was calculated by the HOMA test [32].
-
(3)
The coordinating group evaluated the plasma levels of tumor necrosis factor (TNF)-α) and interleukin (IL)-10 (Milenia Biotech, Germany) by ELISA (ELISA human quantikine; R&D Systems, Minneapolis, MN) after collecting frozen plasma samples from all the centers at the end of enrollment. We determined plasma levels of transforming growth factor (TGF)-β, hyaluronic acid (HA), and metalloproteinase 2 (MMP-2) by ELISA (ELISA human quantikine), which were used as markers of liver fibrosis.
Adverse events were evaluated from the questionnaire, which reported signs and symptoms graded from mild to severe, possible association of symptoms with the treatment, the method used for resolution, and the necessity to stop the treatment.
Statistical analysis
The results, number (percentage) of patients with a condition, are expressed as the mean and standard deviation or the median and range. The SPSS v11.0 software was used for statistical analyses. The analysis of variance (ANOVA) and Wilcoxon test were used to evaluate the differences between data and groups. Differences in frequency were calculated by chi-square. Correlations between the results were evaluated by the Pearson bivariate correlation test. A P value ≤0.05 was considered significant [33].
Results and discussion
There were no severe or mild adverse events or dropouts in either group and study compliance was absolute. Two patients in both groups were diagnosed with diabetes after glucose load. The BMI increased (>25 kg/m2) in approximately 70% of the cases. There was an obvious preponderance of obese females, however, this gender effect was not statistically significant. None of the patients started a new physical activity and all reported good adherence to the diet. However, there was a reduction of dietary intake by the patients in both groups, but this result did not reach statistical significance (data not showed). BMI did not vary significantly between groups, with the exception of the HCV-positive treated patients. In fact, despite the dietary similarities with the other groups, only the HCV-positive treated patients showed a significant and persistent reduction of BMI values (see Table 2).
The NAFLD group (group A) showed a significant and persistent reduction in US score of liver steatosis that ranged from 2–3 at the initial time point to 1–2 at the 6- and 12-month evaluations (P < 0.01). This effect was not apparent in the other group (data not show). The plasma levels of liver enzymes were reduced in the treated patients and not in the control group, but this persisted in NAFLD patients only (Table 3). Sixty-five percent of the NAFLD and 46 percent of the HCV-positive patients had hyperinsulinemia at the basal time point. This percentage was significantly reduced in the treated NAFLD subjects (47% at 6 months and 51% at 12 months; P < 0.05). Insulinemia was significantly and persistently improved by RA treatment in both the NAFLD and the HCV groups. Similar trends were observed for the HOMA values and are summarized in Table 4. Figure 1 summarizes the percentage variation of ALT, γ-GT, insulinemia, and HOMA values with respect to the basal values in the treated patients in groups A and B. No significant variations were observed in the control group (not treated). The plasma levels of the other biochemical parameters evaluated under the basal conditions (see Table 1), even if partially improved, did not differ significantly at the end of the study.
The BMI can affect liver steatosis, plasma insulin levels, and liver enzymes. Patients were divided on the basis of BMI improvement and differences, in terms of the percentage of patients with improved steatosis, insulin levels, and liver enzymes, were noted between the treated and the untreated groups. These data indicated that treatment with RA affected insulinemia, ALT, and/or γ-GT independently by modification of the BMI (Table 5).
We investigated two cytokines, TNF-α, a pro-inflammatory cytokine, and IL-10, an anti-inflammatory cytokine. We found that under the basal condition the sporadic increase in TNF-α was not statistically different from the normal values reported. Both during and at the end of the study, no significant variations were observed for TNF-α values in either group. IL-10 values were reduced, but then significantly increased at the end of treatment in group A. However, IL-10 values returned to the basal level at the 12-month follow-up (basal, 42 ± 23 pg/ml; 6 months, 63 ± 33 pg/ml [P < 0.05 vs. basal]; and 12 months, 36 ± 11.7 pg/ml).
Plasma indexes of liver fibrosis differed between the NAFLD and the HCV groups. The HCV patients (group B) showed a high level of the liver fibrosis marker HA at the basal time point compared to group A. Overall, the RA treatment significantly reduced plasma levels of HA and the other fibrosis markers. However, this reduction in the markers for liver fibrosis only persisted to the 12-month follow-up for group B. Table 6 summarizes the mean values of the plasma markers of fibrosis for all groups. A significant correlation among the indexes of fibrosis, BMI, insulinemia, plasma levels of TGF-β and TNF-α, degree of steatosis, and γ-GT (P < 0.01) was found; TGF-β levels also correlated with TNF-α and IL-10 (P < 0.01). A significant direct correlation was also observed among some indexes of fibrosis (Table 7).
There are two main drawbacks to this study: (1) it was an open study without the use of placebo, and (2) tt was not possible to define a “therapeutic” efficacy for the new compound silybin + vitamin E + phospholipids for liver damage because there was no histological evaluation for liver damage before and after treatment. However, each patient was individually compared to the basal time point and an untreated control group was included. In addition, it was reasonable to consider that 6 months of treatment may have been unable to modify liver histology. Despite the study's shortcomings, our data suggest that this new compound may be useful in clinical practice. The important results were the significant improvement of insulin resistance and plasma levels of liver fibrosis markers in patients, with an absence of any adverse effects.
The occurrence of liver steatosis and its progression to fibrosis and cirrhosis are a long process that includes multiple consecutive steps. This metabolic syndrome is associated with metabolic changes such as weight fluctuations, insulin resistance, diabetes, and hyperlipidemia. Changes in molecular mediators, such as various peptides, hormones, and cytokines, as well as cellular messengers, such as free radicals that are capable of inducing lipid peroxidation, are all factors involved in this intricate puzzle [34, 35]. An ideal treatment for NAFLD would reduce the extent of liver damage and/or its progression directly or via modulation of the pathophysiological events. Therefore, drugs for the treatment of NAFLD should reduce body weight, improve insulin resistance and the levels of other metabolic alterations, reduce the linkage between adipose tissue and liver function by acting as anti-inflammatory and/or immunomodulatory agents, and modulate the progression of liver steatosis to inflammation and fibrosis by blocking oxidative stress.
NAFLD patients are generally overweight or obese. A hypocaloric diet is the first component of any weight-loss regimen. Lifestyle modifications, such as a low-fat diet and physical exercise, and/or administration of weight reducing agents are associated with an improvement in liver enzymes, cholesterol, IL-6, IL-8, TNF-α, and plasma HA levels in about 40% of overweight patients with NAFLD [36–39]. Our results are in agreement with those studies. Diet affects insulin resistance and lipid peroxidation and, thus, affects liver steatosis and fibrosis [37, 40–42]. We found a significant direct correlation among BMI, steatosis score, and markers of liver fibrosis. However, diet is only one factor involved in the modulation of fatty liver, and not all patients are overweight. In our study, BMI was improved in a small percentage of the cases as consequence of diet. However, there was no difference between treated and untreated groups. The improvement of BMI was more marked in the treated patients and persisted in those who were HCV positive. These results suggest that RA interferes with body weight gain, and the persistent ameliorative effect on BMI in the HCV patients is due to a different pathophysiological effect on the liver in these patients, more than to better compliance to the diet. We are unable to conclusively explain these results at this time.
Liver steatosis is a consequence of an altered balance between fat accumulation and oxidation, both of which are regulated by insulin. Fatty liver is frequently associated with insulin resistance, and type 2 diabetes is associated with a two- to fivefold increased risk to develop NAFLD [43, 44]. Other authors have evaluated the effect of insulin-sensitizing agents on patients with NAFLD by examining a variety of clinical and histological parameters. Chronic treatment with metformin showed a beneficial effect on the histology, insulin resistance, and biochemical parameters of liver damage [45–48]. Pioglitazone prevented the activation of hepatic stellate cells in vitro and in rats with liver cirrhosis induced by a choline-deficient diet by reducing the expression of type I procollagen, MMP-2, and tissue inhibitor of metalloprotease (TIMP)-1 and TIMP-2 [49]. Sanyal et al. [50] evaluated the efficacy of an antioxidant (vitamin E) plus pioglitazone compared to vitamin E alone. The combined therapy produced a significant decrease in steatosis, cytologic ballooning, Mallory's hyaline accumulation, and pericellular fibrosis. There are less conclusive results with rosiglitazone. In a recent study [51], rosiglitazone improved insulin sensitivity, reduced liver fat content, and improved hepatic histology and liver enzyme levels. However, patients contemporaneously followed a specified diet and engaged in physical exercise. Six months after treatment the liver enzyme levels returned to the basal values. The long-term safety and the real benefits of insulin-sensitizing agents require further well-controlled studies [9].
Silybin affects intrahepatic glucose and lipid metabolism by stabilizing the mitochondrial membrane and increasing the ATP content, which reduces the gluconeogenesis from lactate. It also reduces insulin resistance in humans, although no data are available regarding these effects in NAFLD patients [52–54].
Many investigators are currently focusing their attention on the possibility of reversing liver fibrosis by reducing the activation of hepatic stellate cells, inducing hepatic stellate cell apoptosis, or inducing degradation of collagen deposits [55, 56]. The main activators of hepatic stellate cells are reactive oxygen species and the products of lipid peroxidation. Therefore, antioxidants may be useful antifibrotic agents [35]. Betaine, a naturally occurring metabolite of choline, α-tocopherol, and vitamin C significantly improved liver fibrosis, but not steatosis and inflammation, in humans [57–60].
Silybin acts both as an antioxidant and as an antifibrotic agent. These two effects are mostly independent. Silybin acts as a radical scavenger by increasing the levels of superoxide dismutase and glutathione peroxidase and reducing malonyldialdehyde and 4-hydroxynonenal [61, 62]. Silybin also inhibits the production of TNF-α, IFN-γ, IL-2, and IL-4 and increases the expression of IL-10 and iNOS [63]. Silybin increases the expression of matrix MMPs, reduces the expression of TIMP-1, up-regulates the mRNA expression of TGF-β, and suppresses the proliferation of hepatic stellate cells as an antifibrotic agent [64].
Silybin is rapidly absorbed in humans when conjugated with a phytosome [21]. This new complex contains a large quantity of phosphatidilcholine, which prevents the development of liver fibrosis in rats [65]. The complex also contains a lesser quantity of vitamin E. Silybin reduces collagen accumulation and lipid peroxidation in rats with induced fibrosis and ameliorates liver damage in patients with chronic hepatitis in this complexed form [22, 23]. In rats, the antifibrotic action of RA is associated with a decrease in BMI [22]. The mechanism of this effect is unknown. It could have been mediated by the action of silybin on insulin resistance. In fact, it has recently been stressed that silybin inhibits the activation of IKK-β, which is a crucial mediator of insulin signaling induced by excessive exposure of tissue to free fatty acids and by hypertrophy of adipocytes [54].
The ameliorative effect of silybin in treated diabetic and cirrhosis patients may be due to its action on glucose and lipid metabolism [53]. In the liver, a high dose of silybin inhibits the activation of NF-κB and its related pathways [66, 67]. It is known that a relationship exists between BMI, insulin, and liver fibrosis and the activation and release of some growth factors, such as TGF [68].
Data from this work show that the complex silybin + vitamin E + phospholipids improves liver damage, particularly insulin resistance and plasma markers of liver fibrosis. Whether the results are related to a direct effect of this complex on the activation of hepatic stellate cells or mediated via its antioxidant or metabolic activity remains unknown at the moment. Therefore, we suggest that further evaluation of silybin conjugated with vitamin E and phospholipids in controlled trials to assess its possible therapeutic use as a complementary approach to the treatment of patients with chronic liver damage, particularly when other drugs have failed, is warranted.
References
Patrick L (1999) Hepatitis C: epidemiology and review of complementary/alternative medicine treatments. Altern Med Rev 4:220–238
Bean P (2002) The use of alternative medicine in the treatment of hepatitis C. Am Clin Lab 21:19–21
Neuschwander-Tetri BA, Caldwell SH (2003) Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology 37:1202–1219
Loguercio C, De Simone T, D’Auria MV, de Sio I, Federico A, Tuccillo C, Abbatecola AM, Del Vecchio Blanco C, Italian AISF Clinical Group (2004) Non-alcoholic fatty liver disease: a multicentre clinical study by the Italian Association for the Study of the Liver. Dig Liver Dis 36:398–405
Lonardo A, Adinolfi LE, Loria P, Carulli N, Ruggiero G, Day CP (2004) Steatosis and hepatitis C virus: mechanism and significant for hepatic and extrahepatic disease. Gastroenterology 126:586–597
Ramesh S, Sanyal AJ (2004) Hepatitis C and nonalcoholic fatty liver disease. Semin Liver Dis 24:399–413
Younossi ZM, McCullough AJ, Ong JP, Barnes DS, Post A, Tavill A, Bringman D, Martin LM, Assmann J, Gramlich T, Mullen KD, O’Shea R, Carey WD, Ferguson R (2004) Obesity and non-alcoholic fatty liver disease in chronic hepatitis C. J Clin Gastroenterol 38:705–709
Lin HZ, Yang SQ, Chuckaree C, Kuhajda F, Ronnet G, Diehl AM (2000) Metformin reverts fatty liver disease in obese, leptin-deficient mice. Nat Med 6:998–1003
Cadranel JF, Jouannaud V, Loison S (2004) Improving insulin resistance: certain progress in the management of patients with non-alcoholic steatohepatitis … but the story continues. Gastroenterol Clin Biol 28:265–267
Laurin J, Lindor KD, Crippin JS, Gossard A, Gores GJ, Ludwig J, Rakela J, McGill DB (1996) Ursodeoxycolic acid or clofibrate in the treatment of non alcohol induced steatohepatitis; a pilot study. Hepatology 23:1464–1467
Lazaridis KN, Gores GJ, Lindor KD (2001) Ursodeoxycolic acid “mechanism of action and clinical use in hepatobilary disorders.” J Hepatol 35:134–146
Wellington K, Jarvis B (2001) Silymarin: a review of its clinical properties in the management of hepatic disorders. Bio Drugs 15:465–489
Lang I, Nekam K, Gonzalez-Cabello R, Muzes G, Gergely P, Feher J (1990) Hepatoprotective and immunological effects of antioxidant drugs. Tokai J Exp Clin Med 15:123–127
Feher J, Lang I, Nekam K, Muzes G, Deak G (1988) Effect of free radical scavengers on superoxide dismutase (SOD) enzyme in patients with alcoholic cirrhosis. Acta Med Hung 45:265–276
Lucena MI, Andrade RJ, de la Cruz JP, Rodriguez-Mendizabal M, Blanco E, Sanchez de la Cuesta F (2002) Effects of silymarin MZ-80 on oxidative stress in patients with alcoholic cirrhosis. Results of a randomized, double-blind, placebo-controlled clinical study. Int J Clin Pharmacol Ther 40:2–8
Liu J, Manheimer E, Tsutani K, Gluud C (2003) Medicinal herbs for hepatitis C virus infection: a Cochrane hepatobiliary systematic review of randomized trials. Am J Gastroenterol 98:538–544
Velussi M, Cernigoi AM, De Monte A, Dapas F, Caffau C, Zilli M (1997) Long-term (12 months) treatment with an anti-oxidant drug (silymarin) is effective on hyperinsulinemia, exogenous insulin need and malondialdehyde levels in cirrhotic diabetic patients. J Hepatol 26:871–879
Fuchs EC, Weyhenmeyer R, Weiner OH (1997) Effects of silybin and of a synthetic analogue on isolated rat hepatic stellate cells and myofibroblasts. Arzneimittelforschung 47:1883–1887
Dehmlow C, Murawski N, de Groot H (1996) Scavenging of reactive oxygen species and inhibition of arachidonic acid metabolism by silibinin in human cells. Life Sci 58:1591–1600
Buzzelli G, Moscarella S, Giusti A, Duchini A, Marena C, Lampertico M (1993) A pilot study on the liver protective effect of silybin-phosphatidylcholine complex (IdB1016) in chronic active hepatitis. Int J Clin Pharmacol Ther Toxicol 31:456–460
Zhao J, Agarwal R (1999) Tissue distribution of silibinin, the major active constituent of silymarin, in mice and its association with enhancement of phase II enzymes: implications in cancer chemoprevention. Carcinogenesis 20:2101–2108
Di Sario A, Bendie E, Taffetani S (2003) Realsil, a new sylibin-phospatidylcoline complex, reduces dimethylnitrosamine-induced hepatic fibrosis in the rat. J Hepatol 38:P76
Federico A, Trappoliere M, Tuccillo C, de Sio I, Di Leva A, Del Vecchio Blanco C, Loguercio C (2006) A new silybin–vitamin E–phospholipid complex improves insulin resistance and liver damage in patients with non alcoholic fatty liver disease: preliminary observations. Gut (in press)
Joseph AE, Saverymuttu SH, al-Sam S, Cook MG, Maxwell JD (1991) Comparison of liver histology with ultrasonography in assessing diffuse parenchimal liver disease. Clin Radiol 9:91–94
Liu CJ, Jeng YM, Chen PJ, Lai MY, Yang HC, Huang WL, Kao JH, Chen DS (2005) Influence of metabolic syndrome, viral genotype and antiviral therapy on superimposed fatty liver disease in chronic hepatitis C. Antivir Ther 10:405–415
Reid AE (2001) Nonalcoholic steatohepatitis. Gastroenterology 121:710–723
Adam JM, Tarigan NP (2004) Comparison of the World Health Organization (WHO) two-step strategy and OGTT for diabetes mellitus screening. Acta Med Indones 36:3–7
Angulo P (2002) Nonalcoholic fatty liver disease. N Engl J Med 346:1221–1231
Marchesini G, Bugianesi E, Forlani G, et al. (2003) Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 37:917–923
Rosenberg WM, Voelker M, Thiel R, Becka M, Burt A, Schuppan D, Hubscher S, Roskams T, Pinzani M, Arthur MJ, European Liver Fibrosis Group (2004) Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology 127:1704–1713
Guglielmi FW, Panella C, Buda A, Budillon G, Caregaro L, Clerici C, Conte D, Federico A, Gasbarrini G, Guglielmi A, Loguercio C, Losco A, Martines D, Mazzuoli S, Merli M, Mingrone G, Morelli A, Nardone G, Zoli G, Francavilla A (2005) Nutritional state and energy balance in cirrhotic patients with or without hypermetabolism. Dig Liver Dis 37:681–688
Melchionda N, Forlani G, Marchesini G, Baraldi L, Natale S (2002) WHO and ADA criteria for the diagnosis of diabetes mellitus in relation to body mass index. Insulin sensitivity and secretion in resulting subcategories of glucose tolerance. Int J Obes Relat Metab Disord 26:90–96
Armitage P, Berry G (1994) Statistical methods in medical research. Blackwell Science, Oxford
Loguercio C, Federico A (2003) Oxidative stress in viral and alcoholic hepatitis. Free Rad Biol Med 34:1–10
Mehta K, Van Thiel DH, Shah N, Mobarhan S (2002) Nonalcoholic fatty liver disease: pathogenesis and the role of antioxidants. Nutr Rev 60:289–293
Kugelmas M, Hill DB, Vivian B, Marsano L, McClain CJ (2003) Cytokines and NASH: a pilot study of the effects of lifestyle modification and vitamin E. Hepatology 38:413–419
Dixon JB, Bhathal PS, Hughes NR, O’Brien PE (2004) Nonalcoholic fatty liver disease: improvement in liver histological analysis with weight loss. Hepatology 39:1647–1654
Loguercio C, De Girolamo V, de Sio I, Tuccillo C, Ascione A, Baldi F, Budillon G, Cimino L, Di Carlo A, Di Marino MP, Morisco F, Picciotto F, Terracciano L, Vecchione R, Verde V, Del Vecchio Blanco C (2001) Nonalcoholic fatty liver disease in an area of southern Italy: main clinical, histological and pathophysiological aspects. J Hepatol 35:568–574
Harrison SA, Fincke C, Helinski D, Torgerson S, Hayashi P (2004) A pílot study of orlistat treatment in obese, non-alcoholic steatohepatitis patients. Aliment Pharmacol Ther 20:623–628
Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, Faga E, Silli B, Pagano G (2003) Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology 37:909–916
Huang MA, Greenson JK, Chao C, Anderson L, Peterman D, Jacobson J, Emick D, Lok AS, Conjeevaram HS (2005) One-year intense nutritional counseling results in histological improvement in patients with non-alcoholic steatohepatitis: a pilot study. Am J Gastroenterol 100:1072–1081
Solga S, Alkhuraishe AR, Clark JM, Torbenson M, Greenwald A, Diehl AM, Magnuson T (2004) Dietary composition and nonalcoholic fatty liver disease. Dig Dis Sci 49:1578–1583
Gupte P, Amarapurkar D, Agal S, Baijal R, Kulshrestha P, Pramanik S, Patel N, Madan A, Amarapurkar A, Hafeezunnisa (2004) Non-alcoholic steatohepatitis in type 2 diabetes mellitus. J Gastroenterol Hepatol 19:854–858
Friis-Liby I, Aldenborg F, Jerlstad P, Rundstrom K, Bjornsson E (2004) High prevalence of metabolic complications in patients with non-alcoholic fatty liver disease. Scand J Gastroenterol 39:864–869
Nair S, Diehl AM, Wiseman M, Farr GH Jr, Perrillo RP (2004) Metformin in the treatment of non-alcoholic steatohepatitis: a pilot open label trial. Aliment Pharmacol Ther 20:23–28
Uygun A, Kadayifci A, Isik AT, Ozgurtas T, Deveci S, Tuzun A, Yesilova Z, Gulsen M, Dagalp K (2004) Metformin in the treatment of patients with non-alcoholic steatohepatitis. Aliment Pharmacol Ther 19:537–544
Bugianesi E, Gentilcore E, Manini R, Natale S, Vanni E, Villanova N, David E, Rizzetto M, Marchesini G (2005) A randomized controlled trial of metformin versus vitamin E or prescriptive diet in nonalcoholic fatty liver disease. Am J Gastroenterol 100:1082–1090
Schwimmer JB, Middleton MS, Deutsch R, Lavine JE (2005) A phase 2 clinical trial of metformin as a treatment for non-diabetic paediatric non-alcoholic steatohepatitis. Aliment Pharmacol Ther 21:871–879
Kawaguchi K, Sakaida I, Tsuchiya M, Omori K, Takami T, Okita K (2004) Pioglitazone prevents hepatic steatosis, fibrosis, and enzyme–altered lesions in rat liver cirrhosis induced by a choline-deficient L-amino acid-defined diet. Biochem Biophys Res Commun 315:187–195
Sanyal AJ, Mofrad PS, Contos MJ, Sargeant C, Luketic VA, Sterling RK, Stravitz RT, Shiffman ML, Clore J, Mills AS (2004) A pilot study of vitamin E versus vitamin E and pioglitazone for the treatment of nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol 2:1107–1115
Neuschwander-Tetri BA, Brunt EM, Wehmeier KR, Oliver D, Bacon BR (2003) Improved nonalcoholic steatohepatitis after 48 weeks of treatment with the PPAR-gamma ligand rosiglitazone. Hepatology 38:1008–1017
Rolo AP, Oliveira PJ, Moreno AJ, Palmeira CM (2003) Protection against post-ischemic mitochondrial injury in rat liver by silymarin or TUDC. Hepatol Res 26:217–224
Lirussi F, Beccarello A, Zanette G, De Monte A, Donadon V, Velussi M, Crepaldi G (2002) Silybin-beta-cyclodextrin in the treatment of patients with diabetes mellitus and alcoholic liver disease. Efficacy study of a new preparation of an anti-oxidant agent. Diabetes Nutr Metab 15:222–231
McCarty MF (2005) Potential utility of natural polyphenols for reversing fat-induced insulin resistance. Med Hypotheses 64:628–635
Bataller R, Brenner DA (2001) Hepatic stellate cells as a target for the treatment of liver fibrosis. Semin Liver Dis 21:437–451
Di Sario A, Bendia E, Macarri G, Candelaresi C, Taffetani S, Marzioni M, Omenetti A, De Minicis S, Trozzi L, Benedetti A (2004) The anti-fibrotic effect of pirfenidone in rat liver fibrosis is mediated by downregulation of procollagen α1(I), TIMP-1 and MMP-2. Dig Liver Dis 36:744–751
Abdelmalek MF, Angulo P, Jorgensen RA, Sylvestre PB, Lindor KD (2001) Betaine, a promising new agent for patients with nonalcoholic steatohepatitis: results of a pilot study. Am J Gastroenterol 96:2711–2717
Oliveira CP, Gayotto LC, Tatai C, Della Nina BI, Lima ES, Abdalla DS, Lopasso FP, Laurindo FR, Carrilho FJ (2003) Vitamin C and vitamin E in Prevention of nonalcoholic fatty liver disease (NAFLD) in choline deficient diet fed rats. Nutr J 2:9
Harrison SA, Torgerson S, Hayashi P, Ward J, Schenker S (2003) Vitamin E and vitamin C treatment improves fibrosis in patients with nonalcoholic steatohepatitis. Am J Gastroenterol 98:2485–2490
Hasegawa T, Yoneda M, Nakamura K, Makino I, Terano A (2001) Plasma transforming growth factor-beta1 level and efficacy of alpha-tocopherol in patients with non-alcoholic steatohepatitis: a pilot study. Aliment Pharmacol Ther 15:1667–1672
Kravchenko LV, Morozov SV, Tutel’yan VA (2003) Effects of flavonoids on the resistance of microsomes to lipid peroxidation in vitro and ex vivo. J Hepatol 39:333–340
Valenzuela A, Lagos C, Schmidt K, Videla LA (1985) Silymarin protection against hepatic lipid peroxidation induced by acute ethanol intoxication in the rat. Biochem Pharmacol 34:2209–2212
Schumann J, Prockl J, Kiemer AK, Vollmar AM, Bang R, Tiegs G (2003) Silibinin protects mice from T cell-dependent liver injury. J Hepatol 39:333–340
Jia JD, Bauer M, Cho JJ, Ruehl M, Milani S, Boigk G, Riecken EO, Schuppan D (2001) Antifibrotic effect of silymarin in rat secondary biliary fibrosis is mediated by downregulation of procollagen alpha1(I) and TIMP-1. J Hepatol 35:392–398
Ma X, Zhao J, Lieber CS (1996) Polyenylphosphatidylcholine attenuates non-alcoholic hepatic fibrosis and accelerates its regression. J Hepatol 24:604–613
Manna SK, Mukhopadhyay A, Van NT, Aggarwal BB (1999) Silymarin suppresses activation of NFkB, c–Jun–N–Terminal kinase and apoptosis. J Immunol 163:6800–6809
Yoo HG, Jung SN, Hwang YS, Park JS, Kim MH, Jeong M, Ahn SJ, Ahn BW, Shin BA, Park RK, Jung YD (2004) Involvement of NFkB and caspases in silibinin-induced apoptosis of endothelial cells. Int J Mol Med 13:81–86
Wright TL, Rocky DC (2004) Liver disease: from bench to bedside. Postgraduate course. American Association for the Study of Liver Diseases, Boston (abstr book)
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Other members of the Real Sud Group: L. Cimino, Federico II University, Naples; V. De Girolamo and A. Marone, Ascalesi Hospital, Naples; C. De Stefano, S. Carlo Hospital, Potenza; G. De Stefano, Madonna delle Grazie Hospital, Matera; D. Disalvo and B. Provenzano, Villa D’Agri Hospital, Potenza; P. Esposito and A. Simonetti, Second University, Naples; M. D. Iannece and R. Pempinello, Cotugno Hospital, Naples; R. Iorio, Giugliano Hospital, Naples; S. Monastra and M. Di Pierro, S. Gennaro Hospital, Naples.
Rights and permissions
About this article
Cite this article
Loguercio, C., Federico, A., Trappoliere, M. et al. The Effect of a Silybin-Vitamin E-Phospholipid Complex on Nonalcoholic Fatty Liver Disease: A Pilot Study. Dig Dis Sci 52, 2387–2395 (2007). https://doi.org/10.1007/s10620-006-9703-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9703-2