Abstract
The sucrose breath test (SBT) was employed to noninvasively assess the efficacy of probiotics in 5-fluorouracil (5-FU)-induced intestinal mucositis. Dark Agouti rats were allocated to 5 groups (n=10): 5-FU+L. fermentum BR11, 5-FU+L. rhamnosus GG, 5-FU+B. lactis BB12, 5-FU+skim milk (SM), and saline+SM. Probiotics were administered by oral gavage for 10 days. Mucositis was induced on day 7 by intraperitoneal injection of 5-FU (150 mg/kg) or vehicle (saline). Rats were sacrificed 72 h after 5-FU injection. The SBT measured breath 13CO2 (expressed as percentage cumulative dose at 90 min; %CD90) on days 0, 7, and 10. %CD90 was significantly lower in 5-FU-treated controls compared with that in saline-treated controls on day 10. 5-FU caused an 83% reduction in sucrase and a 510% increase in MPO activity. The SBT detected damage induced by 5-FU and is a simple, noninvasive indicator of small bowel injury. The probiotics assessed offered no protection from mucositis at the dose tested.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mucositis is a debilitating side effect of chemotherapy associated with common treatment regimens for malignancy. Approximately 40% of all patients undergoing chemotherapy develop mucositis [1, 2]. Systemic effects of mucositis include diminished oral ingestion of fluids and solids which leads to dehydration, malnutrition, nausea, vomiting, abdominal pain, bloating, and diarrhea [3, 4]. Currently there is a lack of effective prophylactic or therapeutic treatments for mucositis [5, 6]. Furthermore, current approaches focus on symptoms and have been limited to rinses, barrier protectants, topical antimicrobials, cryotherapy (ice), and analgesics. A number of alternative strategies are currently being pursued, including new pharmaceuticals and bioactives such as keratinocyte growth factor [7, 8], insulin-like growth factor [9], milk-derived growth factors [10, 11], and, more recently, probiotics.
Probiotics are defined as bacteria or bacterial products that have a significant health benefit for the recipient [12]. It has become apparent that bacterial strains such as bifidobacteria and lactobacilli play an important role in maintaining barrier function within the intestine [13–15]. Bifidobacteria are capable of enhancing specific immune functions [16] and have also been demonstrated to prevent adhesion of Escherichia coli to mucosal surfaces [17] and Bifidobacterium lactis BB12 has been shown to trigger gene expression of the inflammatory mediator interleukin-6 [18]. Lactobacillus species possess beneficial physiologic effects, including antimicrobial activity, enhancement of immune potency, antitumorigenic activities, and antioxidative activity [19]. Lactobacillus rhamnosus GG has been shown to be effective in the control of diarrhea [17] and Lactobacillus fermentum BR11, a newly described organism isolated from guinea pig [20, 21], possesses antioxidant properties [21]. Lactobacillus fermentum BR11 has also been shown to provide partial protection from dextran sulfate sodium-induced colitis in rats [22].
The sucrose breath test (SBT) has been developed as a noninvasive method for determining total intestinal sucrase activity [23]. Sucrase is an enzyme found in the brush border membrane of mucosal cells lining the lumen of the small intestine [24]. It catalyzes the breakdown of sucrose into its constituent monosaccharides, glucose and fructose. Following ingestion of 13C-sucrose, these monosaccharides are transported to the liver and metabolized to liberate 13CO2, which is exhaled from the lungs and quantified using an isotope ratio mass spectrometer (IRMS). These in vivo determinations of sucrase activity are indicative of mucosal damage [23, 25]. Carcinomata and hematologic malignancies are treated primarily with antimetabolite chemotherapeutic agents such as 5-fluorouracil (5-FU) and methotrexate (MTX), which cause cell death by interfering with DNA synthesis [26]. Applicability of the SBT to the detection of intestinal mucositis induced by MTX has been demonstrated previously by Pelton et al. [23].
The current study aimed to further characterize the SBT’s ability to detect intestinal damage induced by 5-FU, and to assess the effects of Lactobacillus fermentum BR11, Lactobacillus rhamnosus GG, and Bifidobacterium lactis BB12 administration on the severity of 5-FU-induced mucositis in rats.
Methods
Animals and experimental design
Female Dark Agouti (DA) rats (body weight=146±1 g) were maintained in metabolism cages (Tecniplast USA Inc., Exton, PA, USA) for the duration of the experimental period and maintained at 25°C with a 12-h light/dark cycle. Rats were allocated to 5 groups: saline+skim milk (SM), 5-FU+SM, 5-FU+Lactobacillus fermentum BR11, 5-FU+Lactobacillus rhamnosus GG, and 5-FU+Bifido-bacterium lactis Bb12 (n=10). Metabolism data, including water and food intake and urine and fecal output, were collected for 11 days. All animals were provided ad libitum access to drinking water and a standard 18% casein-based diet [27] except during fasting periods. All animal studies were carried out in compliance with the Australian Code of Practice for the Care and Use of Animals and were approved by the Animal Ethics Committee of the Children, Youth and Women’s Health Service, Adelaide, South Australia.
5-FU-induced mucositis
Rats were administered a single dose of 5-FU (150 mg/kg; Fluorouracil Injection, Mayne Pharma Pty Ltd, Melbourne, Australia) or saline control on day 7 by intraperitoneal injection. This dose was determined in a previous study [28] in Sprague-Dawley rats in which intestinal damage was evident within 2 days of treatment, and gastrointestinal symptoms were maximal 3 days after chemotherapy administration. On this basis, rats were sacrificed on day 10 of the experimental period, 3 days after 5-FU injection.
Probiotic preparations
L. fermentum BR11 and L. rhamnosus GG were grown in De Mann/Rogosa/Sharpe (MRS) broth (Oxoid Ltd, Hampshire, England). B. lactis BB12 was grown in Brain Heart Infusion (BHI) broth (Oxoid). All bacterial broths were incubated at 37 °C, 5% CO2, for 48 h. The broths were pooled and centrifuged at 1000 rpm for 10 min and the supernatant was removed. The pellet was then resuspended in a 10% skim milk/1% glucose solution, reconstituted from Bonlac® skim milk powder (Inpak Foods, Adelaide, South Australia, Australia). The concentration of bacteria in skim milk suspensions was approximately 1×106 CFU/ml, determined by viable count. The skim milk suspensions were separated into 10 ml aliquots and stored at −80 °C.
Probiotic bacteria were administered daily by orogastric gavage. Administration began on day 0 of the trial period and continued until day 9. All rats were sacrificed on day 10. The orogastric gavage consisted of 1 ml of skim milk solution alone as a control, or 1 ml of bacteria in skim milk solution. Both the saline-injected and 5-FU-injected control groups were administered skim milk alone.
Sucrose breath test
Breath collection was performed by placing rats in a sealed 600 ml perspex container, allowing breath to accumulate for 2 min, and drawing 20 ml of breath into a syringe attached to a two-way outlet in the lid of the container [23, 25]. Rats were fasted overnight and a baseline breath sample was collected at t=0. Rats were then gavaged with 1 ml of a sucrose solution (250 mg/ml) and breath was collected every 15 min for a total of 2 h. Samples were collected in evacuated 10 ml glass tubes (Exetainer, Labco Ltd, High Wycombe, UK) and analyzed using an IRMS (Europa Scientific Automated Breath 13Carbon Analyser, Crewe, UK) for breath 13CO2, expressed as percentage cumulative dose at 90 min (%CD90). The SBT was performed before commencement of the trial (day 0), on day 7 before injection with saline or 5-FU, and before sacrifice on day 10.
Tissue collection
Animals were sacrificed by CO2 asphyxiation and cervical dislocation on day 10. The abdomen was opened by a midline surgical incision and the jejunum separated from the duodenum at the ligament of Treitz, as described previously [10]. The gut, from stomach to anus, was removed and placed on an ice-cold glass slab. The length of the duodenum, small intestine, and colon was recorded. All gastrointestinal organs were flushed of contents and weighed. Two centimeter segments of duodenum, small intestine, and colon were collected and fixed in 10% buffered formalin for histologic analysis. Segments (4 cm) directly adjacent to the histologic samples were snap-frozen in liquid nitrogen and stored at −80 °C for later homogenization and biochemical analyses. Sampling sites in the small intestine corresponded to 10% (proximal jejunum), 25%, 50%, 75%, and 90% (distal ileum) of the intestinal length. Heart, lungs, kidneys, spleen, liver, and thymus were removed, weighed, and discarded.
Biochemical analyses
Intestinal samples from the proximal jejunum and distal ileum were thawed in 1.5 ml of 10 mM phosphate buffer (pH 6.0) and homogenized for 2 min at 17,000 rpm. Aliquots of homogenate (200 μl) were stored at −80°C until required for sucrase and myeloperoxidase assays. In vitro determination of active intestinal sucrase allows direct analysis of brush border integrity [25, 29] in different regions of the intestine. Endogenous sucrase activity was assessed by a modification of the method described previously by Dahlqvist [30]. Intestinal homogenates were thawed on ice and a minimum of two dilutions were performed for each sample, which were plated in triplicate and corrected for background absorbance. Glucose standards were used to obtain a standard curve. Plates were read using a microtiter plate reader (MR7000, Dynatech Laboratories Inc., Chantilly, VA, USA) with the test filter set at 490 nm and the reference filter set at 690 nm. Tablecurve 2D software (Systat Software Inc., Point Richmond, CA, USA) was used to calculate glucose concentration.
Myeloperoxidase (MPO) is an intracellular enzyme found in neutrophils [31], cells which are the principal component of acute inflammatory cell infiltrates. Levels of MPO were determined by a modification of the procedure described by Krawisz et al. [31]. Intestinal homogenates were thawed and centrifuged at 15,000 rpm for 12 min (Heraeus Biofuge Pico, Kendro Laboratory Products, Langenselbold, Germany). The supernatant was discarded and the pellet was resuspended in 200 μl of 0.5% hexadecyltrimethylammonium bromide (HTAB) buffer (pH 6.0) (Sigma Chemical Co., St Louis, MO, USA) to release MPO from neutrophil primary granules. Samples were then centrifuged at 15,000 rpm for 5 min to remove cellular debris and 50 μl of each supernatant was plated in duplicate. Optical density was read immediately following addition of a freshly prepared O-dianisidine-based reaction mixture (200 μl/well) at 1 min intervals for 15 min using a microplate reader (MR7000) with the test filter set at 450 nm.
Histological analysis
Tissue samples were transferred into 70% alcohol after 24 h in 10% buffered formalin, routinely processed, and embedded in paraffin wax. Transverse sections (5 μm) of proximal jejunum were stained using hematoxylin and eosin. A light microscope (SM-Lux, Leitz Wetzlar, Germany) was used to perform semiquantitative histologic examination and images were acquired using a digital camera (Sony, Tokyo, Japan). Sections were assessed in a blinded manner using a set of 11 parameters to obtain an overall score of damage severity (semiquantitative; maximum score=33) as described previously [32, 33]. These parameters included villus atrophy, crypt loss or disruption, and inflammatory cell infiltration.
Statistical analysis
Statistical analyses were performed using the GraphPad Prism 4.0 software package (GraphPad Software, San Diego, CA, USA). Parametric data, including organ wet weights and lengths, breath 13CO2 levels (%CD90), sucrase levels, and MPO levels, were analyzed using one-way analysis of variance (ANOVA) and Tukey’s post-hoc tests. Daily metabolic data were analyzed using two-way ANOVA and Bonferroni post-hoc tests. Nonparametric data, including severity scores, were analyzed using the Kruskal−Wallis test with Dunn’s post-hoc tests comparing all data sets. Observed differences were considered significant if P < 0.05.
Results
Body weight and gastrointestinal organs
Between days 0 and 10, rats administered 5-FU+SM showed a significant loss in body weight (P < 0.05) compared with saline+SM-treated controls (Table 1). Body weight loss in all three probiotic-treated groups was significantly greater than in saline+SM-treated rats (P < 0.05) but not different than in 5-FU+SM-treated rats (Table 1).
All organ weights were adjusted for body weight to eliminate this parameter as a source of variation. Small intestine weight was reduced by 17% in 5-FU+SM-treated rats compared with saline+SM-treated rats (P < 0.001; Table 1). Small intestine weight was also reduced in 5-FU+L. fermentum- (18%), 5-FU+L. rhamnosus- (10%), and 5-FU+B. lactis-treated (18%) rats. Cecum weight increased following 5-FU+SM (45%), 5-FU+L. fermentum (35%), and 5-FU+B. lactis (46%) treatment compared with saline+SM treatment. 5-FU+L. fermentum and 5-FU+B. lactis treatment displayed significant increases in colon weight compared with saline+SM, 16% and 23%, respectively. 5-FU-treated rats did not display a decrease in small intestine length compared with saline+SM-treated rats (P>0.05; Table 2). 5-FU+L. fermentum- and 5-FU+B. lactis-treated rats did display a decrease in small intestine length compared with saline+SM-treated rats, 8% and 6%, respectively. Colon length was decreased in 5-FU+SM- (16%), 5-FU-L. fermentum- (9%), 5-FU+L. rhamnosus- (9%), and 5-FU+B. lactis -treated (12%) rats compared with saline+SM-treated controls (Table 2). There was no significant difference in small intestine and colon length between any of the three probiotic-treated groups and the 5-FU+SM-treated controls (Table 2).
Adjusted thymus weight was significantly decreased in 5-FU+SM-treated rats compared with saline+SM (0.050±0.003 vs. 0.136±0.016, % thymus weight/body weight; P < 0.001). Thymus weight was also significantly decreased in 5-FU+L. fermentum- (0.056±0.003), 5-FU+L. rhamnosus- (0.062±0.004), and 5-FU+B. lactis-treated (0.053±0.003) rats. Spleen weight was significantly decreased in 5-FU+SM-treated rats compared with saline+SM (0.168±0.005 vs. 0.233±0.004, % spleen weight/body weight; P < 0.001). Spleen weight was also significantly decreased in 5-FU+L. fermentum- (0.172±0.005), 5-FU+L. rhamnosus- (0.163±0.004), and 5-FU+B. lactis-treated (0.158±0.005) rats.
Noninvasive sucrose breath test
On days 0 and 7 there was no significant difference in breath 13CO2 (%CD90) between 5-FU+SM- and saline+SM-treated rats (Fig. 1A). On day 10, however, breath 13CO2 in the 5-FU+SM-treated rats exhibited a 63% reduction compared with that in saline+SM-treated controls (P < 0.001; Fig. 1B). There was no significant difference in %CD90 values between any of the probiotic-treated groups and 5-FU+SM-treated rats on days 0 and 7 (Fig. 1A). On day 10, the %CD90 of all three probiotic-treated groups were significantly lower (P < 0.001) than saline+SM-treated controls although they were not significantly different than that of 5-FU+SM–treated rats (Fig. 1B).
Biochemically assessed sucrase activity
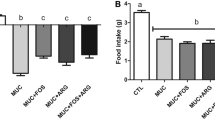
Proximal jejunum sucrase activity in 5-FU+SM-treated rats was 83% lower compared with saline+SM-treated controls (P < 0.001; Fig. 2A). Distal ileum sucrase activity in 5-FU+SM-treated rats was below the sensitivity of the assay. In saline + SM-treated rats, sucrase activity in the distal ileum was 11% of proximal jejunum values (P < 0.001). There was no significant difference in jejunal sucrase activity between any of the three probiotic-treated groups and 5-FU+SM-treated controls (Fig. 2A). Breath 13CO2 levels (%CD90) and sucrase activity values from proximal jejunum homogenates were compared directly by linear regression and a strong correlation was found between these two parameters (r 2=0.77, P < 0.0001).
A Sucrase activity and B MPO activity in the proximal jejunum (white columns) and the distal ileum (black columns) of female Dark Agouti rats. Columns represent means + SEM. A significant difference compared with saline+SM in the jejunum is denoted by c (P < 0.001), and +, #, and ^ denote a significant difference compared with saline+SM in the ileum, P < 0.05, P < 0.01, and P < 0.001, respectively
MPO activity and small intestine histology
MPO activity in proximal jejunum was not significantly different from the distal ileum in saline+SM-treated rats (Fig. 2B). MPO activity in the proximal jejunum and distal ileum of 5-FU+SM-treated rats was increased by 510% (P < 0.001) and 129% (P < 0.05), respectively, compared with saline+SM-treated rats (Fig. 2B). MPO activity in both the proximal jejunum and distal ileum did not vary significantly in any of the three probiotic treatment groups when compared with 5-FU+SM-treated rats (Fig. 2B).
Examples of histologic images from normal (saline+SM) and damaged (5-FU+SM) proximal jejunum are shown in Fig. 3. The median severity score increased by 14.5 in 5-FU+SM-treated rats (P < 0.001) compared with saline+SM-treated controls, but none of the three probiotic-treated groups displayed a significant difference in severity score compared with 5-FU+SM–treated rats (Fig. 4).
Discussion
There is currently a lack of effective therapeutic interventions for the treatment of chemotherapy-induced mucositis. We used the noninvasive sucrose breath test to assess three potential probiotic strains for their capacity to reduce the severity of small intestinal mucositis. Consistent with previous studies in rats, 5-FU caused a significant decrease in body weight and weights of the thymus, spleen, and small intestine [29], further causing a significant increase in damage severity in the jejunum.
In the current study, 5-FU-induced intestinal damage was readily detectable by the SBT. Pelton et al. [23], using the SBT, reported diminished sucrase activity in rats subcutaneously injected with the related antimetabolite methotrexate as indicated by a significant reduction in breath 13CO2 and biochemically determined sucrase activity. Breath 13CO2 in the present study was strongly correlated with biochemically assessed sucrase activity. Clarke et al. [25] used the SBT to investigate the effects of methotrexate in rats and found that breath 13CO2 was significantly lower 72 h after methotrexate injection. Moreover, these investigators also reported that sucrase activity, assessed biochemically, was significantly decreased in the proximal jejunum [25], consistent with the current study. These investigators further reported a strong correlation between jejunal sucrase activity and breath 13CO2 (r 2=0.89) [25], again consistent with the current study, further supporting the SBT as a reliable, noninvasive marker of intestinal damage.
The probiotic Lactobacillus rhamnosus GG and probiotic compound VSL#3 have previously been shown to reduce levels of MPO in the colitis setting [34] and prevent recurrence of colitis after antibiotic treatment [35], and the probiotic Bifidobacterium infantis has been shown to be effective in the treatment of irritable bowel syndrome [12]. At the doses tested, the probiotics investigated in the current study could not prevent the intestinal damage caused by administration of 5-FU. The probiotics were ineffective at preventing overall body weight loss and thymus, spleen, and small intestine weight loss, and they could not prevent small intestine damage as assessed by the SBT, sucrase, and myeloperoxidase activity. Possible explanations for the lack of efficacy may have included the dosage, timing and duration of delivery, or lack of suitability of the strains used for the mucositis setting.
There has been extensive investigation of the probiotics Lactobacillus rhamnosus GG and Bifidobacterium lactis BB12. Administration of probiotic mixtures containing Lactobacillus rhamnosus GG to humans has resulted in a reduction of abdominal bloating [36], symptom score in patients with irritable bowel syndrome [37], risk of antibiotic-associated diarrhea [38], and treatment-related symptoms in addition to a greater success of eradication in H. pylori treatment [39]. However, the current study was unable to reproduce the positive gastrointestinal effects in humans exhibited by Lactobacillus rhamnosus GG and Bifidobacterium lactis BB12.
A recent study by Tooley et al. [40] showed that treatment with the probiotic Streptococcus thermophilus TH-4 reduced the severity of MTX-induced mucositis in Dark Agouti rats with SBT and sucrase activity values comparable to that of normal rats, while MTX treatment alone decreased these parameters. These investigators reported that Streptococcus thermophilus TH-4-treated rats also had a lower MPO activity compared with MTX-treated rats, indicating less inflammation in the small intestine. The study by Tooley et al. highlighted the capability for the SBT to detect the preventative effects of Streptococcus thermophilus TH-4 in a mucositis model, confirming that the SBT could be used to rapidly and noninvasively screen novel therapies for mucositis [40]. Coupled with the current study, this emphasizes the importance of screening large numbers of bacterial strains, since not all strains would necessarily be beneficial in mucositis setting.
In conclusion, the sucrose breath test is an effective indicator of 5-FU-induced intestinal damage. However, at the doses tested, none of the three probiotic strains examined exhibited any demonstrable protective effect on the mucosa of the chemotherapy-damaged small intestine. To detect any potential beneficial effects of Lactobacillus fermentum BR11, Lactobacillus rhamnosus GG, or Bifidobacterium lactis BB12 in the treatment of chemotherapy-induced mucositis, additional studies could investigate the use of viable bacteria at a higher dosage, differing timing regiments, and combinations of the three probiotics.
References
Sonis ST, Eilers JP, Epstein JB, LeVeque FG, Liggett Jr WH, Mulagha MT, Peterson DE, Rose AH, Schubert MM, Spijkervet FK, et al. (1999) Validation of a new scoring system for the assessment of clinical trial research of oral mucositis induced by radiation or chemotherapy. Cancer 85:2103–2113
Pico J-L, Avila-Garavito A, Naccache P (1998) Mucositis: its occurrence, consequences, and treatment in the oncology setting. Oncologist 3:446–451
Khan SA, Wingard JR (2001) Infection and mucosal injury in cancer treatment. J Natl Cancer Inst Monogr 31–36
Keefe DMK (2004) Gastrointestinal mucositis: a new biological model. Support Care Cancer 12:6–9
Clarke J, Butler R, Howarth G, Read L, Regester G (2002) Exposure of oral mucosa to bioactive milk factors reduces severity of chemotherapy-induced mucositis in the hamster. Oral Oncol 38:478–485
Sonis ST (2004) A biological approach to mucositis. J Support Oncol 2:21–32; discussion 35–36
Freytes CO, Ratanatharathorn V, Taylor C, Abboud C, Chesser N, Restrepo A, Arango J, Odenheimer D (2004) Phase I/II randomized trial evaluating the safety and clinical effects of repifermin administered to reduce mucositis in patients undergoing autologous hematopoietic stem cell transplantation. Clin Cancer Res 10:8318–8324
Spielberger R, Stiff P, Bensinger W, Gentile T, Weisdorf D, Kewalramani T, Shea T, Yanovich S, Hansen K, Noga S, et al. (2004) Palifermin for oral mucositis after intensive therapy for hematologic cancers. N Engl J Med 351:2590–2598
Howarth GS (2003) Insulin-like growth factor-I and the gastrointestinal system: therapeutic indications and safety implications. J Nutr 133:2109–2112
Howarth GS, Francis GL, Cool JC, Xu X, Byard RW, Read LC (1996) Milk growth factors enriched from cheese whey ameliorate intestinal damage by methotrexate when administered orally to rats. J Nutr 126:2519–2530
Harsha WT, Kalandarova E, McNutt P, Irwin R, Noel J (2006) Nutritional supplementation with transforming growth factor-beta, glutamine, and short chain fatty acids minimizes methotrexate-induced injury. J Pediatr Gastroenterol Nutr 42:53–58
O’Mahony L, McCarthy J, Kelly P, Hurley G, Luo F, Chen K, O’Sullivan GC, Kiely B, Collins JK, Shanahan F, et al. (2005) Lactobacillus and Bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology 128:541–551
Isolauri E (2001) Probiotics in human disease. Am J Clin Nutr 73:1142S–1146S
Mombelli B, Gismondo MR (2000) The use of probiotics in medical practice. Int J Antimicrob Agents 16:531–536
Madsen K, Cornish A, Soper P, McKaigney C, Jijon H, Yachimec C, Doyle J, Jewell L, De Simone C (2001) Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterology 121:580–591
Park SY, Ji GE, Ko YT, Jung HK, Ustunol Z, Pestka JJ (1999) Potentiation of hydrogen peroxide, nitric oxide, and cytokine production in RAW 264.7 macrophage cells exposed to human and commercial isolates. Int J Food Microbiol 46:231–241
Bezkorovainy A (2001) Probiotics: determinants of survival and growth in the gut. Am J Clin Nutr 73:S399–S405
Ruiz PA, Hoffmann M, Szency S, Blaut M, Haller D (2005) Innate mechanisms of Bifidobacterium lactis to activate transient pro-inflammatory host response in intestinal epithelial cells after the colonization of germ-free rats. Immunology 115:441–450
Kullisaar T, Zilmer M, Mikelsaar M, Vihalemm T, Annuk H, Kairane C, Kilk A (2002) Two antioxidative lactobacilli strains as promising probiotics. Int J Food Microbiol 72:215–224
Hung J, Cooper D, Turner MS, Walsh T, Giffard PM (2003) Cystine up take prevents production of hydrogen peroxide by Lactobacillus fermentum BR11. FEMS Microbiol Lett 69:5855–5863
Rush CM, Hafner LM, Timms P (1994) Genetic modification of a vaginal strain of Lactobacillus fermentum and its maintenance within the reproductive tract after intravaginal administration. J Med Microbiol 41:272–278
Geier MS, Butler RN, Howarth GS (2005) Differential efficacy of probiotic species in amelioration of dextran sulphate sodium-induced colitis in rats. Gastroenterology 128:A603–A604
Pelton NS, Tivey DR, Howarth GS, Davidson GP, Butler RN (2004) A novel breath test for the non-invasive assessment of small intestinal mucosal injury following methotrexate administration in the rat. Scand J Gastroenterol 39:1015–1016
Semenza G, Dahlqvist A (1985) Disaccharides of small-intestinal mucosa. J Pediatr Gastroenterol Nutr 4:857–867
Clarke JM, Pelton NC, Bajka BH, Howarth GS, Read LC, Butler RN (2006) Use of the (13)c-sucrose breath test to assess chemotherapy-induced small intestinal mucositis in the rat. Cancer Biol Ther 5:34–38
McCarthy GM, Awde JD, Ghandi H, Vincent M, Kocha WI (1998) Risk factors associated with mucositis in cancer patients receiving 5-fluorouracil. Oral Oncol 34:484–490
Tomas FM, Knowles SE, Owens PC, Read LC, Chandler CS, Gargosky SE, Bllard FJ (1991) Effects of full-length and truncated insulin-like growth factor-I on nitrogen balance and muscle protein metabolism in nitrogen-restricted rats. J Endocrinol 128:97–105
Xian CJ, Howarth GS, Cool JC, Foster BK (2004) Effects of acute 5-fluorouracil chemotherapy and insulin-like growth factor-I pretreament on growth plate cartilage and metaphyseal bone in rats. Bone 35:739–749
Cool JC, Dyer JL, Xian CJ, Butler RN, Geier MS, Howarth GS (2005) Pre-treatment with insulin-like growth factor-I partially ameliorates 5-fluorouracil-induced intestinal mucositis in rats. Growth Horm IGF Res 15:72–82
Dahlqvist A (1968) Assay of intestinal disaccharides. Anal Biochem 22:99–107
Krawisz JE, Sharon P, Stenson WF (1984) Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Gastroenterology 87:1344–1350
Geier MS, Tenikoff D, Yazbeck R, McCaughan GW, Abbott CA, Howarth GS (2005) Development and resolution of experimental colitis in mice with targeted deletion of dipeptidyl peptidase IV. J Cell Physiol 204:687–692
Howarth GS, Xian CJ, Read LC (2000) Predisposition to colonic dysplasia is unaffected by continuous administration of insulin-like growth factor-I for twenty weeks in a rat model of chronic inflammatory bowel disease. Growth Factors 18:119–133
Shibolet O, Karmeli F, Eliakim R, Swennen E, Brigidi P, Gionchetti P, Campieri M, Morgenstern S, Rachmilewitz D (2002) Variable response to probiotics in two models of experimental colitis in rats. Inflammatory Bowel Dis 8:399–406
Dieleman LA, Goerres MS, Arends A, Sprengers D, Torrice C, Hoentjen F, Grenther WB, Sartor RB (2003) Lactobacillus GG prevents recurrence of colitis in HLA-B27 transgenic rats after antibiotic treatment. Gut 52:370–376
Di Stefano M, Miceli E, Armellini E, Missanelli A, Corazza GR (2004) Probiotics and functional abdominal bloating. J Clin Gastroenterol 38:S102–S103
Kajander K, Hatakka K, Poussa T, Farkkila M, Korpela R (2005) A probiotic mixture alleviates symptoms in irritable bowel syndrome patients: a controlled 6-month intervention. Aliment Pharmacol Ther 22:387–394
Hawrelak JA, Whitten DL, Myers SP (2005) Is Lactobacillus rhamnosus GG effective in preventing the onset of antibiotic-associated diarrhoea: a systematic review. Digestion 72:51–56
Myllyluoma E, Veijola L, Ahlroos T, Tynkkynen S, Kankuri E, Vapaatalo H, Rautelin H, Korpela R (2005) Probiotic supplementation improves tolerance to Helicobacter pylori eradication therapy—a placebo-controlled, double-blind randomized pilot study. Aliment Pharmacol Ther 21:1263–1272
Tooley K, Howarth G, Lymn K, Lawrence A, Butler R (2006) Oral ingestion of Streptococcus thermophilus diminishes severity of small intestinal mucositis in methotrexate treated rats. Cancer Biol Ther 5(6):593–600
Acknowledgments
The authors thank Kerry Lymn, Roger Yazbeck, Joanne Ball, Stamatiki Kritas, Geoffrey Matthews, Lynn Scarman, and Dr. Coung Tran for assistance with the animal experiments, histologic processing, biochemical analyses, and proofreading. Dr. Andrew Lawrence and the staff of the CYWHS Microbiology Department are thanked for their assistance with microbial culture. Thanks are also extended to Inpak Foods, Royal Park, South Australia, for their generous donation of Bonlac® skim milk powder.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mauger, C.A., Butler, R.N., Geier, M.S. et al. Probiotic Effects on 5-Fluorouracil-Induced Mucositis Assessed by the Sucrose Breath Test in Rats. Dig Dis Sci 52, 612–619 (2007). https://doi.org/10.1007/s10620-006-9464-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9464-y