Abstract
As an important pathological feature of acute pancreatitis, apoptosis may occur in multiple organs and relate directly to the progression of disease. It is mainly controlled by the apoptosis gene and also influenced by inflammatory mediators. We summarize here the roles of the main inflammatory mediators (e.g., NO, TNF-α, TGF-β1, IL-10, NF-κB) during the pathologic process of acute pancreatitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Apoptosis is known to be an active process of gene-directed cellular self-destruction and differs fundamentally from necrosis. Its biologic significance during the life process lies in its strictly control of the balance between cell proliferation and cell death. Apoptosis has characteristic morphologic changes in cell structure, including shrinkage of cell volume, nuclear pycnosis, and appearance of apoptotic bodies, with preservation of mitochondria and zymogen granules under the integrity of the cell membrane. In morphology, there is an integral cell membrane, reducing the cell volume, nuclear pycnosis, and formation of apoptotic bodies, but the mitochondria and zymogen granules remain intact. Therefore, the biggest fundamental difference between apoptosis and necrosis is that the former never or seldom induces inflammatory reactions.
Acute pancreatitis (AP) is a kind of frequent acute abdomen. It can be classified into mild acute pancreatitis (MAP) and severe acute pancreatitis (SAP), based on the state of disease, or acute edematous pancreatitis (AEP) and acute necrotizing pancreatitis (ANP), based on pathology. Most AP is self-restricted disease. About 15%–20% of patients may develop a worse state, with local complications or organ failure, and finally develop SAP. The final outcome of SAP will always be local or systemic inflammatory reactions due to the excessive generation of inflammatory mediators [1]. Currently it is believed that abnormally activated pancreatin activates these inflammatory cells inside or outside the pancreas to release inflammatory mediators when the pancreas is injured, resulting in SIRS and MOF, which is the main reason for MAP developing into SAP [2]. Many investigators believe that the cell death form of AP is necrosis. But others have found that apoptosis of pancreatic acinar cells not only is related to AP [3–5], but also participates in the onset of AP [6, 7]. Two different death forms of pancreatic acinar cells, apoptosis and cell necrosis, are related to the state of pancreatitis. Pancreatic acinar cell apoptosis could be a beneficial reaction after the onset of pancreatitis [8–10]. Meanwhile, many studies have found that apoptosis also exists in other organs, such as the liver, small intestine, kidney, lung, heart, and thymus, when SAP induces systemic complications, and its degree corresponds closely to the level of organ injury [11–16]. Apoptosis is mainly mediated by genes and also affected by some inorganic molecules, cytokines, inflammatory mediators, and toxic substances released due to cell injury in AP, as reported in many studies recently. These cell activity molecules and factors participate in the process of cell apoptosis and indirectly adjust apoptosis. They are important participants in apoptosis during AP, with functions that cannot be neglected. We summarize here the roles of the main inflammatory mediators during this pathologic process of AP.
Nitric Oxide (NO)
NO as a small inorganic molecular compound with complicated biological activities that plays an extremely important role in normal mediation of physiological function and onset of many diseases. The NO synthase catalyzing the formation of NO exists in mammalian tissues and cells, mainly in two forms: cNOS and iNOS. NO’s effects on the body are bidirectional [17]. cNOS catalyzes small doses of NO to protect cells, while the redundant NO activated by iNOS relates to the onset of many diseases [18]. Enormous amounts of NO are generated continuously 5 min after ANP occurs, injuring tissue cells and aggravating pancreatic injury by generating peroxidized nitrate or other toxic intermediate products [19]. Excessive NO can aggravate the lung injury due to ANP [20], and enormous amounts of NO-induced cytokines also can aggravate the renal injury [21, 22]. However, small doses of NO play the role of protecting function. Werner et al. [23] proved that small doses of NO can improve microcirculation disturbance during AP, protect endotheliocytes, maintain the integrity of the vessel wall, increase capillary blood flow, and directly or indirectly protect pancreatic cells. Supplying exogenous NO can markedly reduce experimental AP injury and blocking endogenous NO can markedly aggravate pancreatic injury due to many injurious factors [24].
iNOS induced by cytokines and bacterial toxin can synthesize and release endogenous NO. Fehsel et al. [25] found through experiments that both exogenous and endogenous NO can effectively induce thymic cell apoptosis. They also conjectured that NO can result in many other types of apoptosis. Hence investigators began to study the relationship between NO and apoptosis. Many studies found that the serum NO level dropped during AP and the degree of decrease correlated directly with that state of illness. A low NO level always indicates severe inflammation and a poor prognosis. Kaneto et al. [26], who studied B cells separated from the rat pancreas, found that a high NO concentration can induce apoptosis. Raising the serum NO level can reduce AP inflammatory reactions and enhance the survival of laboratory animals. Liu et al. [27], who treated mice with ANP with exogenous NO generator and suppressor, found that the NO content in the exogenous NO generator group had a longer average survival time, while in the NO suppressor group the NO content dropped more markedly, with severe necrosis and a decreased average survival time. Therefore, it is believed that NO participates in the mediation and evolution of AP, maybe because NO promotes partial pancreas acinus apoptosis and restricts the extension of inflammatory reactions. NO can induce pancreatic apoptosis via a series of pathways [28], mainly it can (a) adjust apoptosis to improve pancreatic microcirculation through sGC-cGMP; (b) induce apoptosis and inhibit the aggregation of neutrophils (PMNs) in the pancreas through reactive oxygen intermediates (ROIs); (c) induce apoptosis to control infection by destroying energy metabolism; and (d) adjust apoptosis and the expression of p53 through gene mediation.
Tumor Necrosis Factor-α (TNF-α)
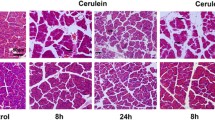
As a cytokine mainly secreted by activated monocytes/macrophages, TNF-α has multiple biological activities and is closely related to the state of pancreatitis. The serum TNF-α level of SAP patients is higher than that of MAP patients, and the TNF-α level of all patients is markedly higher than that of controls but drops markedly after treatment [29]. TNF-α is closely related to apoptosis. Bhatia et al. [30], who found expression of TNF-α in serum and pancreatic tissue of rats with AP, believe that TNF-α can alleviate AP by inducing pancreatic acinar apoptosis. Yasuda et al. [31], who found expression of TNF-α mRNA in the pancreatic tissue of mice with AP, believe that TNF-α can reduce the generation of digestive enzymes and induce pancreatic acinar apoptosis to protect the body and improve prognosis. Chang et al. [32], who studied the relation between AP pancreatic apoptosis and TNF-α, found that apoptosis cells of rats in the pancreatitis group increased progressively 1 hr after operation and began to decrease 6 hr later, with apoptosis at 6 hr markedly higher than that at 3 and 12 hr. The TNF-α concentration at 3 and 6 hr was markedly lower than that at 1 hr, and that at 12 hr was markedly higher than that at 6 hr. Change et al. believe that TNF-α plays an important role in AP pathogenesis by inducing pancreatic apoptosis, and activation is related to TNF-α concentration. Zhang et al. [33] believe that serum TNF-α has dual regulating effects on apoptosis, namely, a low concentration of TNF-α can induce apoptosis and promote healing of inflammation, but a high concentration of TNF-α will cause pancreatic acinus cell necrosis. Malka et al. [34], observing AR4-2J cells treated with TNF-α at different concentrations, found that only TNF-α at >10 μg/L can induce apoptosis of AR4-2J cells and maximum apoptosis (40%) is reached at 100 μg/L. The inducing effect of TNF-α at 10–100 ng/ml is time and dose dependent. TNF-α receptors exist on the pancreatic acinar cell membrane and induce cell apoptosis combined with a low concentration of TNF-α from activated mononuclear macrophages. A high level of TNF-α will further stimulate a series of cascade effects, inducing expression of interleukin (IL)-1, IL-6, IL-8, etc. [33]. Overactivated cytokines cause pancreatic cell necrosis and, finally, cause injury of the pancreas and other tissues, while no pancreatic apoptosis is observed in AP animals without TNF-α receptor [16]. The TNF-α antagonist applied by Kimura et al. [9] to the pancreatitis rat model induced by cerulein can inhibit pancreatic apoptosis. TNF-α also participates in the apoptosis process of other organs during AP. Zhang et al. [35–37] found overexpressed TNF-α gene in lung injury due to ANP and a negative correlation between lung apoptosis index and TNF-α mRNA level. Therefore, they believe that the overgenerated TNF-α partially causes delayed apoptosis of neutrophilic granulocytes. The mechanism of TNF-α-induced apoptosis might be that TNF-α activates Fasl ligand on the T cell surface, then the activated Fasl ligand combines with TNF-α receptor on the pancreatic cell membrane to cause apoptosis. Satoh et al. [38] believe that TNF-α also can cause damage to the cytoskeletal structure by activating PTK-2, which is enriched by proline and induces the cell death signal via various mechanisms mediated by protein kinase C to induce apoptosis.
Transforming Growth Factor-β1 (TGF-β1)
Mostly related to apoptosis, TGF-β1 is a multifunctional cell growth factor regulating cell proliferation, cell differentiation, and intercellular matrix expression. Meanwhile, as a positive apoptosis trigger factor closely related to apoptosis, it can also inhibit the proliferation of various cells such as hepatic and gastrointestinal epithelial cells. Findings from the rat AP model proved that TGF-β1 induced by macrophages is an important factor in apoptosis of hepatic cells in AP [39, 40]. Takeyama et al. [41], have studied rats with SAP, found that ascites of SAP can induce hepatic apoptosis. IL-1 converting enzyme inhibitor can relieve hepatic apoptosis and hepatic cell injury and neutralize TGF-β to partially stop apoptosis. So researchers believe that the occurrence of hepatic apoptosis is related to the TGF-β in ascites of SAP. The TGF-β1 found in the AP rat model induced by cerulein can eliminate damaged acinar cells by promoting acinar apoptosis to alleviate inflammatory reactions of AP. Inhibiting TGF-β not only can alleviate pancreatic fibrosis but also can protect from chronic injury due to excessive pancreatic cell apoptosis. This indicates that TGF-β1 can also promote pancreatic acinar apoptosis [42]. TIEG (early gene induced by TGF-β), a zinc finger-coding gene controlled by TGF-β related to pancreatitis apoptosis, exists in external secretory duct cells and glandular cells of normal human pancreas [43]. Studies show that TIEG expression and the apoptotic rate increase in external secretory pancreas cells treated with TGF-β [44]. This indicates that the mechanism of TGF-β-induced apoptosis is possibly inducement of increasd TIEG expression. In addition, some researchers [45] believe that TGF-β1 is not the key factor, though it can induce pancreatic cell apoptosis, because TGF-β1 was markedly expressed in SAP rat studies without the role of expression like that of the Bax gene protein. It relates to multiple factors and pathways of pancreatic apoptosis.
Interleukin-10
The cytokine IL-10, one kind of multiple effective immunomodulatory factor with the feature of inhibiting the synthesis of the Th1 cell clone, mainly generated by the Th2 cell. It is closely related to AP. It can regulate inflammation by inhibiting the generation of NO and TNF and release of oxygen free radicals and reducing the functions of polynuclear granulocytes, mononuclear granulocytes, and macrophages. Endogenous or exogenous IL-10 can protect the pancreas by inhibiting the activity of monocytes and macrophages to stop the release of pro-inflammatory factor and regulating systemic immune reactions and inflammatory reactions. Rongione et al. [46] found that the plasma amylase concentration drops markedly, pancreatic edema, inflammatory infiltration, and cavitation are decreased, and no TNF-α can be measured in plasma after the injection of IL-10 in rats with AP induced by cerulein. This indicates that IL-10 administration during AP can alleviate the degree of pancreatitis. Recent studies show that this protective effect may be related to the promotion of apoptosis. Gu et al. [47] found that the expression of Bcl-2 in hepatic tissue is increased, and the expression of Bax and hepatic apoptosis decreased, when rats with AP were treated with IL-10 at an early stage. This indicates that IL-10 may change the expression of the apoptosis control gene to promote apoptosis. Zhang et al. [48] divided SAP model rats into an IL-10 prevention group (injection of 150 kU IL-10 intraperitoneally 1 hr before operation and thereafter administration of IL-10 every 2 hr), an IL-10 treatment group (injection of 150 kU IL-10 intraperitoneally 1 hr after operation and thereafter IL-10 administration every 2 hr), and a control group. They found that the level of necrosis in the group treated with IL-10 was markedly lower than that in the control group; amylase, lipase, and iNOS levels were also markedly lower than those in the control group; the expression of TGF-β1 was high in the prevention and treatment groups; and the rate of apoptosis was markedly increased. Therefore, they believe that IL-10 not only can induce massive expression of TGF-β1 and reduce iNOS generation to block SAP progress, but also can reduce necrosis by inducing pancreatic apoptosis to control the degree of inflammation. The mechanism of IL-10-promoted apoptosis is still unclear. It may be related to changing the apoptosis gene expression, increasing the local TGF-β1 concentration, and inhibiting the release of inflammatory mediators.
Nuclear Factor-κB (NF-κB)
Initially extracted from the B-lymphocyte nucleus, NF-κB is a transcription factor mainly participating in the control of inflammatory molecule expression [49, 50]. As a protein able to bind to the κB series of some gene initiator and enhancer regions, it can initiate or enhance gene transcription [51–54]. It also exists in various cells, participating in the control of numerous biological and pathological processes and playing a role in inflammatory reactions, apoptosis, etc., as a pleiotropia and polyphony control factor. In recent years, the role of NF-κB in the pathogenesis of AP has become a hotspot of research. Some animal studies have shown that during AP, NF-κB inhibitor can inhibit the expression and release of inflammatory factors, increase apoptosis of pancreatic cells, reduce necrosis, alleviate the pathogenetic condition of animal models with SAP, and reduce the mortality of experimental animals [55–57]. Pei et al. [58, 59], in rat experiments, found that NF-κB participates in the onset of edematous and necrotizing pancreatitis. And NF-κB expression in edematous pancreatitis is markedly lower than that in necrotizing pancreatitis. Therefore, NF-κB has some anti-apoptotic effect.
There are various anti-apoptotic pathwayss of NF-κB, as follows. (a) NF-κB regulates the transcription of numerous genes and expression of proteins including adhesion factors and cytokines. Satoh et al. [60] found that activation of NF-κB increases markedly, with positive time dependence, after the occurrence of SAP. Abnormal activation of NF-κB can promote the transcription of pro-inflammatory factors (TNF-α, IL-1, IL-6). As an extracellular stimulating signal, TNF-α and IL-1 also can activate NF-κB expression and further promote inflammatory reactions. During SAP, activation of hepatic NF-κB prompts the expression of ICAM-1, which causes aggregation of polymorphonuclear granulocytes in hepatic tissue and results in hepatic injury [61]. The adhesion factors and cytokines induced by NF-κB can inhibit acinar cell apoptosis, promote inflammation, and cause injury to other organs besides the pancreas. (b) NF-κB can induce TNF-α to inhibit pancreatic cell apoptosis. TNF-α can combine with the TNF-α receptor on the acinar cell membrane and then induce NF-κB to generate and release TNF-α [62] to injure tissues. TNF-α can inhibit the activation of apoptotic protease caspase-δ. NF-κB can inhibit pancreatic apoptosis by manipulating the activation of caspase-δ [63]. (c) NF-κB is related to the apoptosis control gene. Haddad et al. [64], studying alveolus \(\parallel\) epithelium apoptosis, found that NF-κB can increase BCL-2 expression, decrease BAX, and participate in the anti-apoptotic process. Wang et al. [65] proved that NF-κB can activate A1/BFI-1 of the BCL-2 family to have an anti-apoptotic effect. Therefore, NF-κB mainly increases BCL-2 and BCL-XL genes to initiate the anti-apoptotic process. Meanwhile, it also inhibits the expression of P53 and BAX genes and thus inhibits induction of apoptosis [66].
Other inflammatory mediators
Generated by pancreatic cells or duct cells, platelet activating factor (PAF) can activate neutrophilic granulocytes to release hydrogen peroxide, NO, etc., and then cause cell necrosis or apoptosis and, finally, cell death. When PAF antagonist (BN52021) is used to treat rats with pancreatitis induced by cerulein, both apoptosis and cell necrosis decrease [67]. The adhesion molecule is also related to apoptosis. During ANP, abnormal expression of the cellular adhesion molecule damages the connection between epithelial cells and the cell matrix to participate in and increases intestinal mucosal epithelial apoptosis [68]. IL-1 plays an important role in the pathogenesis of AP. There is a positive correlation between IL-1 concentration and mortality [69]. Fink et al. [70] found that the IL-6 level dropped and pancreatic injury was markedly alleviated when they injected antiserum into rats with pancreatitis induced by cerulein to eliminate neutrophilic granulocytes and macrophages to reduce IL-1β in pancreatic tissue. Other laboratory evidence proves that IL-1β converting enzyme inhibitor can markedly alleviate the degree of AP in rats and increase their survival. Rau et al. [71] found that this effect is related to the level of inhibition of acinar cell necrosis, but the mechanism is still unclear. It may be related to apoptosis. IL-6 is also an important inflammatory mediator during AP and its level in the SAP rat model climbs markedly [72]. Yu et al. [73], using emodin to treat rats with SAP, found that emodin can markedly inhibit the release of TNF-α and IL-6, induce apoptosis of injured pancreatic cells, and thus improve the degree of SAP. But the precise relation between IL-6 and acinar apoptosis is still unclear and further studies are needed. IL-8, leukotriene, phospholipase A2, thromboxane A2, etc., also are important inflammatory mediators in AP [74], but their precise mechanisms in apoptosis are still unclear.
As a complicated biological phenomenon, apoptosis is controlled by the apoptosis gene and influenced by various inducing factors. Current reports all prove that inducing apoptosis by various methods during AP can control the progression of SAP and is beneficial for treatment. But this is still in the preliminary phase of study. We can understand the onset of the AP process by studying the relation between inflammatory mediators and apoptosis during AP and, thereby, find effective therapies and improve the clinical treatment of SAP.
References
Norman J (1998) The role of cytokine in the pathogenesis of acute pancreatitis. Am J Surg 175:76–83 [PMID: 9445247]
Wang ZF, Pang CE, Liu SG (1998) Role of inflammatory mediators in acute pancreatitis. Shijie Huaren Xiaohua Zazhi 6:170–171 [in Chinese]
Kaiser AM, Saluja AK, Lu L, Yamanaka K, Yamaguchi Y, Steer ML (1996) Effects of cycloheximide on pancreatic endonuclease activity, apoptosis, and severity of acute pancreatitis. Am J Physiol 271:C982–C993 [PMID: 8843729]
Gukovskaya AS, Perkins P, Zaninovic V, Sandoval D, Rutherford R, Fitzsimmons T, Pandol SJ, Poucell-Hatton S (1996) Mechanisms of cell death after pancreatic duct obstruction in the opssum and the rat. Gastroenterology 110:875–884 [PMID: 8608898]
Kaiser AM, Saluja AK, Sengupta A, Saluja M, Steer ML (1995) Relationship between severity, necrosis, and apoptosis in five models of experimental acute pancreatitis. Am J Physiol 269:C1295–C1304 [PMID: 7491921]
Yuan YZ, Gong ZH, Lou KX, Tu SP, Ju ZK, Xu JY (2000) Mechanism of somatostatin and octreotide in apoptosis of acute pancreatitis pancreatic cells. Chin Crit Care Med 12:402–405
Wu ZJ, Zhang YD, Lei ZM, Yu SH (2003) Discussion on role of apoptosis in pathogenesis of rat with acute pancreatitis. China J Modern Med 13:13–15
Fujimoto K, Hosotani R, Doi R, Wada M, Lee JU, Koshiba T, Miyamoto Y, Imamura M (1997) Role of neutrophils in cerulein-induced pancreatitis in rats: possible involvement of apoptosis. Digestion 58:421–430 [PMID: 9383632]
Kimura K, Shimosegawa T, Abe R, Masamune A, Satoh A, Takasu A, Koizumi M, Toyota T (1998) Low doses of lipopolysaccharide upregulate acinar apoptosis in cerulein pancreatitis. Pancreas 17:120–126 [PMID: 9700941]
Shang D, Yang PM, Xin Y, Chen HL, Liu Z (2001) Role of pancreatic acinar cell apoptosis in course of rat with acute pancreatitis and expression of apoptosis controlling gene. J Hepatopancreatobil Surg 13:152–155
Hori Y, Takeyama Y, Ueda T, Shinkai M, Takase K, Kuroda Y (2000) Macrophage-derived transforming growth factor-beta1 induces hepatocellular injury via apoptosis in rat severe acute pancreatitis. Surgery 127:641–649 [PMID: 10840359]
Xu LJ, Yang C, Miao Y (2002) Role of apoptosis in intestinal mucosa barrier dysfunction of empirical acute pancreatitis rat. Hebei Med 8:577–580 [in Chinese]
Zhang N (1999) Apoptosis of renal tubular cell in empirical severe acute pancreatitis. Foreign Med Surg 26:311 [in Chinese]
Liu XM, Liu QG, Pang CE, Xu GF, Zhang T, Huang JY, Zhang M (2003) Influence of blood vessel endothelium apoptosis on lung injury accompanying rat with severe acute pancreatitis. J 4th Military Med Univ 24:1677–1679 [in Chinese]
Chen W, Liu XL (2003) Changes of cardiac damage, myocardial Bcl-2 and Bax gene expression in severe acute pancreatitis rat and protecting effect of anisodamine. Jiangsu Med J 29:424–426 [in Chinese]
Takeyama Y, Nishikawa J, Ueda T, Hori Y (1998) Thymic atrophy caused by thymocyte apoptosis in experimental severe acute pancreatitis. J Surg Res 78:97–102 [PMID: 9733625]
Wink DA, Mitchell JB (1998) Chemical biology of nitric oxide: insights into regulatory, cytotoxic, and cytoprotective mechanisms of nitric oxide. Free Radic Biol Med 25:434–456 [PMID: 9741580]
Zhang ZX, Sun JB (2001) Dual biological effect of NO and acute pancreatitis. J Capital Univ Med Sci 22:282–284 [in Chinese]
Zhao M, Chen RF, Zhou YJ, Wang XC (2003) Role of endogenous NO in pathogenesis of acute hemorrhagic necrotizing pancreatitis. J Capital Univ Med Sci 24:243–246 [in Chinese]
Cheng S, Zhao J, He SG, Song MM, Li ZH, Zhang YW (2003) Role of NO in lung injury of acute necrotizing pancreatitis rat. Chin J Surg 41:336–339
Ren XB, He ZP, Wen L (2001) Role of NO in pancreatic and renal injury of acute hemorrhagic necrotizing pancreatitis rat. J Third Military Med Univ 23:1081–1083 [in Chinese]
Tome LA, Yu L, de-Castro I, Campos SB, Seguro AC (1999) Beneficial and harmful effects of L-arginine on renal ischaemia. Nephrol Dial Transplant 14:1139–1145 [PMID: 10344352]
Werner J, Fernandez-del-Castillo C, Rivera JA, Kollias N, Lewandrowski KB, Rattner DW, Warshaw AL (1998) On the protective mechanisms of nitric oxide in acute pancreatitis. Gut 43:401–407 [PMID: 9863487]
Zhang ZX, Sun JB, Li F, Zhang SW, Cui YQ, Sun HC, Liu S (2000) Pancreatic protecting effect of endogenous NO on rat with acute necrotizing pancreatitis. Chin J Gen Surg 15:606–608
Fehsel K, Kroncke KD, Meyer KL, Huber H, Wahn V, Kolb-Bachofen V (1995) Nitric oxide induces apoptosis in mouse thymocytes. J Immunol 155:2858–2865 [PMID: 7673702]
Kaneto H, Fujii J, Seo HG, Suzuki K, Matsuoka T, Nakamura M, Tatsumi H, Yamasaki Y, Kamada T, Taniguchi N (1995) Apoptoic cell death triggered by nitric oxide in pancreatic β-cells. Diabetes 44:733–738 [PMID: 7540572]
Liu ML, Zhen SY, Fang XY (2001) Empirical study on NO treatment of acute necrotizing pancreatitis. J Bengbu Med Coll 26:95–96 [in Chinese]
Cheng Y (2002) Role of NO-induced apoptosis in acute pancreatitis. Foreign Med Surg 29:343–346 [in Chinese]
Chen K, liang J, Tang B, Ye WT, Wang WM, Zhu B (2000) Determination of serum TNF-α, IL-6 and IL-8 contents in acute pancreatitis patients. Shanghai J Immunol 20:169–171 [in Chinese]
Bhatia M, Wallig MA, Hofbauer B, Lee HS, Frossard JL, Steer ML, Saluja AK (1998) Induction of apoptosis in pancreatic acinar cells reduces the severity of acute pancreatitis. Biochem Biophys Res Commun 246:476–483 [PMID: 9610387]
Yasuda H, Kataoka K, Ichimura H, Mitsuyoshi M, Iida T, Kita M, Imanishi J (1999) Cytokine expression and induction of acinar cell apoptosis after pancreatic duct ligation in mice. J Interferon Cytokine Res 19:637–644 [PMID: 10433]
Chang H, Yan JS, Wang PY, Yan JL (2002) Relation between pancreatic apoptosis and peripheral plasma TNF-α in rat acute pancreatitis. J Hepatopancreatobil Surg 14:215–216 [in Chinese]
Zhang YH, Zhou L, Huang LM (2004) Role of apoptosis and TNF in pathogenesis of rat acute pancreatitis. Guizhou Med 28:1081–1083
Malka D, Vasseur S, Bodeker H, Ortiz EM, Dusetti NJ, Verrando P, Dagorn JC, Iovanna JL (2000) Tumor necrosis factor alpha triggers antiapoptotic mechanisms in rat pancreatic cells through pancreatitis-associated protein activation. Gastroenterology 119:816–828 [PMID: 10982776]
Zhang G, Xiu RL, liu Z, Yang X, Tong WS, Zhang ZD, Qiao AY (2003) Preliminary discussion on lung cell apoptosis status in empirical acute pancreatitis and its meaning. China J Modern Med 13:10–13
Zhang G, Zhang ZD, Xiu RL (2000) Relation between TNF-α gene expression and apoptosis and acute pancreatitis complicated with lung injury. Chin J Surg 38:671
Zhang G, Xiu RL, Yang X, Liu Z, Zhang ZD, Liu XB (2002) Empirical study on relation between TNF-α gene expression and apoptosis and acute pancreatitis complicated with lung injury. Zhonghua Xiaohua Zazhi 22:22–25 [in Chinese]
Satoh A, Gukovskaya AS, Edderkaoui M, Daghighian MS, Reeve JR Jr, Shimosegawa T, Pandol SJ (2005) Tumor necrosis factor-alpha mediates pancreatitis responses in acinar cells via protein kinase C and proline-rich tyrosine kinase 2. Gastroenterology 129:639–651 [PMID: 16083718]
Hori Y, Takeyama Y, Ueda T, Shinkai M, Takase K, Kuroda Y (2000) Macrophage-derived transforming growth factor-beta1 induces hepatocellular injury via apoptosis in rat severe acute pancreatitis. Surgery 127:641–649 [PMID: 10840359]
Li HY, Chen RF, Liu GZ, Wang Y, Wang XC (2004) Hepatic transforming growth factor β1 and hepatic cell apoptosis in empirical acute hemorrhagic necrotizing pancreatitis. Chin J Pathophysiol 20:1256–1260
Takeyama Y, Hori Y, Takase K, Ueda T, Yamamoto M, Kuroda Y (2000) Apoptotic cell death of hepatocytes in rat experimental severe acute pancreatitis. Surgery 127:55–64 [PMID: 10660759]
Nagashio Y, Ueno H, Imamura M, Asaumi H, Watanabe S, Yamaguchi T, Taguchi M, Tashiro M, Otsuki M (2004) Inhibition of transforming growth factor beta decreases pancreatic fibrosis and protects the pancreas against chronic injury in mice. Lab Invest 84:1610–1618 [PMID: 15502860]
Subramaniam M, Harris SA, Oursler MJ, Rasmussen K, Riggs BL, Spelsberg TC (1995) Identification of a novel TGF-beta-regulated gene encoding a putative zinc finger protein in human osteoblasts. Nucleic Acids Res 23:4907–4912 [PMID: 8532536]
Tachibana I, Imoto M, Adjei PN, Gores GJ, Subramaniam M, Spelsberg TC, Urrutia R (1997) Overexpression of the TGFβ-regulated zinc finger encoding gene, TIEG, induces apoptosis in pancreatic epithelial cells. J Clin Invest 99:2365–2374 [PMID:9153278]
Xu GF, Liu QG, Liu XM, Zhang T (2003) Study on apoptosis of rat severe acute pancreatitis. J 4th Military Med Univ 24:908–910 [in Chinese]
Rongione AJ, Kusske AM, kwan K, Ashley SW, Reber HA, McFadden DW (1997) Interleukin 10 reduces the severity of acute pancreatitis in rats. Gastroenterology 112:960–967 [PMID: 9041259]
Gu JC, Wang Y, Zhang ZT, Xue JG, Li JS, Zhou YZ (2004) Influence of exogenous interleukin-10 on expression of hepatic Bcl-2, Bax and hepatic cell apoptosis in acute hemorrhagic necrotizing pancreatitis rat. Chin J Hepatobil Surg 10:260–262
Zhang HJ, Wang X (2004) Study on protecting effect of interleukin 10 in severe acute pancreatitis. J Shanxi Med Univ 35:327–330 [in Chinese]
Li YY, Gao JF (2001) Acute pancreatitis and NF-κB. Shijie Huaren Xiaohua Zazhi 9:420–421 [in Chinese]
Suk K, Yeou Kim S, Kim H (2001) Regulation of IL-8 production by IFN gamma and PGE2 in mouse microglial cells: involvement of NF-κB pathway in the regulatory processes. Immunol Lett 77:79–85 [PMID: 11377701]
Izumi T, Saito Y, Kishimoto I, Harada M, Kuwahara K, Hamanaka I, Takahashi N, Kawakami R, Li Y, Takemura G, Fujiwara H, Garbers DL, Mochizuki S, Nakao K (2001) Blockade of the natriuretic peptide receptor guanylyl cyclase-A inhibits NF-kappaB activation and alleviates myocardial ischemia/reperfusion injury. J Clin Invest 108:203–213 [PMID: 11457873]
Antonelli A, Bianchi M, Crinelli R, Gentilini L, Magnani M (2001) Modulation of ICAM-1 expression in ECV304 cells by macrophage-released cytokines. Blood Cell Mol Dis 27:978–991 [PMID: 11831864]
Ginis I, Jaiswal R, Klimanis D, Liu J, Greenspon J, Hallenbeck JM (2002) TNF-alpha-induced tolerance to ischemic injury involves differential control of NF-kappaB transactivation: the role of NF-kappaB association with p300 adaptor. J Cereb Blood Flow Metab 22:142–152 [PMID: 11823712]
Wright G, Singh IS, Hasday JD, Farrance IK, Hall G, Gross AS, Roger TB (2002) Endotoxin stress-response in cardiomyocytes: NF-kappaB activation and tumor necrosis factor-alpha expression. Am J Physiol Heart Circ Physiol 282:872–879 [PMID: 11834481]
Dunn JA, Li C, Ha T, Kao RL, Browder W (1997) Therapeutic modification of nuclear factor kappa B binding activity and tumor necrosis factor-alpha gene expression during acure biliary pancreatitis. Am Surg 63:1036–1043 [PMID: 9393250]
Gukovsky I, Gukovskaya AS, Blinman TA, Zaninovic V, Pandol SJ (1998) Early NF-kappa B activation is associated with hormone-induced pancreatitis. Am J Physiol 275:G1402–G1414 [PMID: 984377]
Bai XW, Sun B (2004) Severe acute pancreatitis and nuclear factor. J Harbin Med Univ 38:488–489 [in Chinese]
Pei HH, Yang ZA, Qin ZY, Feng YQ (2002) Significance of NF-κB expression in rat with acute necrotizing pancreatitis. Chin J Gen Surg 17:752
Pei HH, Yang ZA, Qin ZY, Feng YQ (2002) Significance of NF-κB expression in two kinds of empirical pancreatitis. Chin J Crit Care Med 22:72–73
Satoh A, Shimosegawa T, Fujita M (1999) Inhibition of nuclear factor-kB activation improves the survival of rats with taurocholate pancreatitis. Gut 44:253–258 [PMID: 9895386]
Shi L, Tian FZ, Huang DR (2003) Hepatic NF-κB’s regulation of ICAM-1 expression and its significance in acute pancreatitis rat. Shijie Huaren Xiaohua Zazhi 11:1505–1507 [in Chinese]
Gukovskaya AS, Gukovsky I, Zaninovic V, Song M, Sandoval D, Gukovsky S, Pandol SJ (1997) Pancreatic acinar cells produce, release and respond to tumor necrosis factor-alpha. Role in regulating cell death and pancreatitis. J Clin Invest 100:1853–1862 [PMID: 9312187]
Weber CK, Adler G (2001) From acinar cell damage to systemic inflammatory response: current concepts inpancreatitis. Pancreatology 1:356–362 [PMID: 12120214]
Haddad JJ, Land SC (2000) The differential expression of apoptosis factors in the alveolar epithelium is redox sensitive and requires NF-kappaB (RelA)-selective targeting. Biochem Biophys Res Commun 271:257–267 [PMID: 10777712]
Wang CY, Guttridge DC, Mayo MW, Baldwin AS (1999) NF-kappaB induces expression of the Bcl-2 homologue A1/Bfl-1 to preferentially suppress chemotherapy-induced apoptosis. Mol Cell Biol 19:5923–5929 [PMID: 10454539]
Zhen JS (2002) Study progress on death methods of nuclear factor and acinar cell. Chin J Gastroenterol Hepatol 11:284–287 [in Chinese]
Sandoval D, Gukovskaya A, Reavey P, Gukovsky S, Sisk A, Braquet P, Pandol SJ, Poucell-Hatton S (1996) The role of neutrophilis and platelet-activating factor in mediating experimental pancreatitis. Gastroenterology 111:1081–1091 [PMID: 8831604]
Wang XP, Wang BX, Wu K, Xu XF (2001) Role of apoptosis in early intestinal mucosa epithelial cell death of acute necrotizing pancreatitis. Zhonghua Xiaohua Zazhi 21:267–270 [in Chinese]
Norman JG, Fink G, Franz M, Guffey J, Carter G, Davison B, Sexton C, Glaccum M (1996) Active interleukin-1 receptor required for maximal progression of acute pancreatitis. Ann Surg 223:163–169 [PMID: 8597510]
Fink GW, Norman JG (1996) Intrapancreatic interleukin-1beta gene expression by specific l eukocyte populations during acute pancreatitis. J Surg Res 63:369–373 [PMID: 8661228]
Rau B, Paszkowski A, Lillich S, Baumgart K, Moller P, Beger HG (2001) Differential effects of caspase-1/interleukin-1 beta-converting enzyme on acinar cell necrosis and apoptosis in severe acute experimental pancreatitis. Lab Invest 81:1001–1013 [PMID: 11454989]
Yu SH, Lei ZM, Zhang PM, Gao JY (2002) Dynamic changes of cytokines and pancreatic acinar cell apoptosis in acute stage of severe acute pancreatitis acute. Chongqing Med J 31:970–972 [in Chinese]
Yu SH, Lei ZM, Zhang PM, Chen YB (2003) Influence of emodin on TNF-α, IL-6 and pancreatic acinar cell apoptosis of rat severe pancreatitis. Chinese J Integr Tradit West Med 9:209–211
Zhu WM, Li JS (2000) Relations among severe acute pancreatitis, inflammatory cytokines and inflammatory mediators. J Med Postgrad 13:106–109 [in Chinese]
Acknowledgments
This work was supported by technological foundation projects for traditional Chinese medical science of Zhejiang province (Nos. 2003C130 and 2004C142), a foundation project for medical science and technology of Zhejiang province (No. 2003B134), a grave foundation project for technological and development of Hangzhou (No. 2003123B19), an intensive foundation project for technology of Hangzhou (No. 2004Z006), a foundation project for medical science and technology of Hangzhou (No.2003A004), and a foundation project for technology of Hangzhou (No. 2005224).
Author information
Authors and Affiliations
Corresponding author
Additional information
We claim that this review is original, and we do not have any financial interest in a company or its competitor, and that all authors meet the criteria for authorship.
Rights and permissions
About this article
Cite this article
Zhang, XP., Lin, Q. & Zhou, YF. Progress of Study on the Relationship Between Mediators of Inflammation and Apoptosis in Acute Pancreatitis. Dig Dis Sci 52, 1199–1205 (2007). https://doi.org/10.1007/s10620-006-9388-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9388-6