Abstract
Our aım was to evaluate effects of metformin, rosiglitazone, and diet with exercise in nonalcoholic fatty liver disease. Forty-seven patients (mean age, 44±10 years; 17 female) whose ALT levels had been high for at least 6 months and with hepatosteatosis detected by liver biopsy and/or USG were enrolled in this study. Of these, 12 were treated with 850 mg/day metformin (group 1), 11 with 4 mg/day rosiglitazone (group 2), and 24 with diet and exercise (group 3) for 1 year. ALT normalization at months 6 and 12 was accepted as treatment response. Liver biopsy was performed in all patients in groups 1 and 2 before treatment and 12 patients (4 in group 1, 8 in group 2) after treatment; but in group 3 it was performed only in patients who approved this procedure (12 patients). Body mass index did not change in groups 1 and 2, but it decreased significantly in group 3 (30±3 to 28±2 kg/m2) at month 12. Treatment response rate was 33.3, 54.5, and 54.2% in groups 1, 2, and 3, respectively, at month 6. This rate was 22.2, 37.5, and 41.2 in groups 1, 2, and 3, respectively, at month 12. Rate of steatosis and stage of fibrosis did not change after treatment. Diet with exercise seems to be superior to metformin and rosiglitazone. Decreasing treatment response at month 12 compared to month 6 may be due to fluctuations of ALT levels. Treatment response should be evalulated histologically.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nonalcoholic fatty liver disease (NAFLD) was first described in obese nondiabetic women who did not use alcohol in 1980 by Ludwig [1]. Macrovesicular steatosis with Mallory's hyaline and mixed inflammatory infiltrate and focal hepatocyte necrosis were shown in these patients' liver biopsies. NAFLD is a clinicopathologic term that reflects liver damage over a wide spectrum: from simple steatosis to steatohepatitis and cirrhosis [2–5]. The prevalance of NAFLD is 10–24% in the general population. NAFLD is a common cause of asymptomatic elevation of aminotransferase levels, in up to 90% of cases, once other causes of liver disease are excluded [2]. Worldwide, the importance of NAFLD is increasing, because of its high prevalance and possible progressive course. In the literature, there are many studies on the pathogenesis and treatment of NAFLD in recent years. Obesity, type II diabetes mellitus, and hyperlipidemia are the main causes of NAFLD. Insulin resistance is important in the pathogenesis. Diet and exercise are effective to the treatment of insulin resistance [6–8]. However, many drugs such as gemfibrozil, clofibrate [9], ursodeoxycholic acid, acetylcysteine, vitamin E, metformin [10–12], and thiazolidinediones (troglitazone, rosiglitazone, pioglitazone) [13–17] have been investigated for the treatment of NAFLD. Drugs that improve insulin sensitivity are the most popular agents in this area. But there is no accepted effective medication in the treatment of NAFLD and there is no published study that compares the effects of diet with exercise to those of drugs that improve insulin resistance alone. We aimed to evaluate and compare the effects of metformin, rosiglitazone, and diet with exercise in NAFLD.
Materials and methods
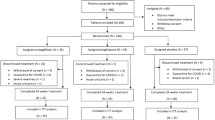
Forty-seven patients whom aminotransferase levels had been high for at least 6 months and who had hepatosteatosis detected by liver biopsy (35 patients) and/or USG (12 patients) were enrolled in this study. Other causes of liver diseases were excluded (viral, autoimmune, and metabolic). Patients had not used alcohol in the past and did not use it during the study period.
Patients taking another drug were excluded from this study. Metformin and rosiglitazone were given to consequtive patients who agreed to the control liver biopsy. Diet with exercise was planned for patients who did not agree to control liver biopsy. Of the patients, 12 were treated with 850 mg/day metformin (group 1), 11 with 4 mg/day rosiglitazone (group 2), and 24 with diet and exercise (group 3) for 1 year. Exercise was planned as walking briskly for a minimum of 30 min at least 2 days per week. Extra meals were put away and amounts of main meals (breakfast, noon, evening) were decreased. We planned to work together with a dietician for patients who did not lose weight at evaluations, but no one needed a dietician's help.
At the first visit, physical examination (including body mass index [BMI]) and biochemical analysis (glucose, blood urea nitrogen [BUN], creatinine, alanine aminotransferase [ALT], aspartate aminotransferase [AST], alkaline phosphatase [ALP], γ-glutamyl transpeptidase [GGT], triglycerides, cholesterol, HDL, LDL, insulin, C-peptide, transferrin saturation, ferritin, and whole blood count) were done in all patients. Insulin resistance (IR) was determined by homeostasis model assessment (HOMA) (fasting insulin [μU/ml]×fasting glucose [mmol/L]/22.5) [18]. Values >1.64 were accepted as IR. Patients were monitored monthly in groups 1 and 2, and every 3 months in group 3. At every evaluation, physical examination and glucose, BUN, creatinine, ALT, AST, ALP, GGT, and whole blood count were reevaluated. At month 12, all biochemical tests were reanalyzed. ALT normalization was accepted as treatment response and evaluated at months 6 and 12. Before treatment, all patients in groups 1 and 2 underwent liver biopsy and 12 of them (4 in group 1, 8 in group 2) had a control biopsy after treatment. In group 3, liver biopsy was performed only for patients who accepted the procedure before treatment (12 patients).
Liver biopsies were obtained by Menghini technique using a 16-G Braun needle. Tissue sections were fixed in buffered formalin and cut from paraffin-embedded blocks. They were stained with hematoxylin/eosin, Masson's trichrome, and Prussian blue. Histological findings were evaluated by Brunt et al's [19] classification for NAFLD. All biopsy specimens were evaluated blindly by a single pathologist.
Statistical analyses were done with SPSS 10.0, Windows version. Categorical variables were evaluated by multicolumn chi-square test and continual variables analyzed by one-way ANOVA, post hoc multiple comparision, and Tukey's b tests among the groups. Pre- and posttreatment biochemical parameters were evaluated by paired t test in each group. Histological findings were evaluated by Wilcoxon signed ranks test, Kruskal-Wallis test, and Kendall's τ–b correlation where appropriate.
This study was performed after approval by the committee of Istanbul University, Istanbul Medical Faculty, Department of Internal Medicine and Division of Gastroenterohepatology.
Results
Baseline characteristics of patients were similar in all groups, except ALP and glucose levels. Demographic and biochemical features of patients are reported in Table 1. Rates of diabetic patients were 16.6, 9.1, and 20.8% in groups 1, 2, and 3, respectively. Impaired glucose (fasting glucose >110 mg/dl) tolerance rates were 33.3, 9.1, and 8.3% in groups 1, 2, and 3, respectively. Hypertriglyceridemia (>150 mg/dl) and hypercholesterolemia (>200 mg/dl) rates were 50% and 58.8% in group 1, and 18% and 45.4% in group 2, and both of them were 54.1% in group 3, respectively.
All patients were obese (>28 kg/m2) in group 1. Overweight (>25 kg/m2) patient rates were 81% and 91% in groups 2 and 3, respectively. Obesity rates were 66.6, 54.5, and 70.8%, in groups 1, 2, and 3 and IR rates (by HOMA >1.64) were 90, 60, and 83.3% in groups 1, 2, and 3, respectively.
Ferritin levels were <300 ng/ml in all groups. Also, transferrin saturations were under 45% in all patients, except for two in group 1.
BMI did not change in groups 1 and 2, but decreased significantly in group 3 (30 ± 3 to 28 ± 2 kg/m2) at month 12 (P < 0.05) (Fig. 1). A positive correlation was detected between BMI and ALT levels (r = 0.268, P = 0.042). At month 6, mean ALT levels were 57.5 ± 15.9, 40 ± 20, and 45 ± 19 IU/L in groups 1, 2, and 3 and the treatment response rate was 33.3, 54.5, and 54.2% in groups 1, 2, and 3, respectively (P > 0.05, not significant). Treatment response rates were higher in groups 3 and 2 than in group 1. At month 12, these rates were 22.2, 37.5, and 41.2% in groups 1, 2, and 3, respectively (P > 0.05; Fig. 2 and Table 2). At the end of treatment IR did not change in any of the groups.
Histological findings are listed in Table 3. Periportal hepatocellular glycogenated nuclei were detected in 25% of patients. After treatment, the rate of macrovesicular steatosis regressed from 58.75 to 52.5% in all groups, with a regression from 68.8±10.3 to 58.8±13.7% (P=0.066) in group 1 and from 53.8±13.7 to 49.4±25.9% (P=0.329) in group 2. The regression rate of steatosis was not significantly different between these two groups (P=0.07). In group 2, fibrosis decreased in two of eight patients (stage 3 to 2, stage 4 to 3) and progressed in one patient (stage 1 to stage 2) (Figs. 3A and 3B and 4A and 4B).
Posttreatment histological findings are listed in Table 4. There was no correlation between rate of macrovesicular steatosis and treatment response (r=–0.052, P=0.879) and serum ALT levels (r=0.038, P=0.899).
Monthly ALT levels were also evaluated in patients who had a control liver biopsy (Fig. 5). Monthly treatment response rates were 50, 66.6, 50, 33.3, 41.6, 66.6, 58.3, 50, 41.6, 50, 50, and 41.6% in 1 year, respectively.
Discussion
To date, NAFLD has been accepted as a benign disease. Based on the increasing published cases and studies, NAFLD is thought to be a serious disease, which can lead to cirrhosis [3, 4]. The natural history is still unclear.
Especially in patients with high ALT levels, theraupetic approaches are still being investigated. There is no accepted standard medication in the treatment of NAFLD. Because IR has an important role, nowadays drugs that improve insulin sensitivity such as metformin and thiazolidinedione (troglitazone, rosiglitazone, pioglitazone) are the most popular agents [13–17]. Also, there is no reported study that compares the efficacy of drugs with that of diet and exercise. In this study, we evaluated the effects of metformin, rosiglitazone, and diet with exercise in the treatment of NAFLD.
To evaluate the real efficacy of drugs, we did not put the patients treated with metformin or rosiglitazone on a diet. In medication groups, nobody lost weight after treatment and the BMI did not change. In the study by Tetri-Neuschwander et al [15] on the effects of rosiglitazone on NASH, the BMI increased after treatment (from 34.1 to 36.4 kg/m2). Another study on vitamins E and C reported similar results for BMI (increasing after treatment) [20]. Overweight and obesity are accepted as risk factors for NAFLD. Thus, if the BMI changes after treatment, we cannot actually evaluate drugs' efficacy. We believe that the unchanged BMI after treatment in groups 1 and 2 provided a correct comparison of medication and diet with exercise. Although the BMI did not change in groups 1 and 2, a statistically significant decrease was detected in group 3. This shows that the observed effects in groups 1 and 2 depend only on the medications. BMI has not been evaluated in any study in the literature from this perspective [13].
IR was analyzed by HOMA [18] because it is an easy and reliable method. In our cases, IR did not change after treatment in any group.
In the literature, Marchesini et al. [11] first studied metformin on humans. They treated 20 patients with metformin (1500 mg/day for 4 months) and ALT levels returned to normal in 50% of patients. Uygun et al. [12] and Kadayıfcı [21] reported similar results. They randomized 36 patients into two groups (diet alone and metformin, 1700 mg/day, plus diet for 6 months). At the end of treatment, metabolic and histologic improvement (except fibrosis) was detected in patiens treated with metformin plus diet. In our study, ALT normalization rate was 22.2% at month 12. Compared with other studies, this rate is low. This result may be due to the low metformin dose used in our study or the diet in addition to metformin therapy, which could have increased the response rate in other studies. We thought that one variable's effect could be evaluated only in the case where other variables remained unchanged. For this reason, we did not give the diet to the patients in medication groups. In metformin group, only four patients underwent control liver biopsy. In these patients, after treatment, the percentage of macrovesicular steatosis decreased (from 68.8±10.3 to 58.8±13.7%; P=0.066). This result is not statistically significant. If the number of patients had been higher in our group, the result might have been significant.
There are limited numbers of studies on rosiglitazone in the literature. In some studies, necroinflammation improved and fibrosis regressed in type II diabetes mellitus [14] and NASH [15] with rosiglitazone therapy. Mayerson et al. [14] treated type II diabetic patients with rosiglitazone (4 mg/tid) and they showed decreasing hepatosteatosis by proton NMR. Tetri-Neuschwander et al. [15] treated 30 patients diagnosed with NASH with rosiglitazone (4 mg/tid) for 48 week. They reported regression of necroinflammation and improvement of serum ALT levels in 45% of 22 patients completing the therapy. They also observed an improvement in IR. In our study, we treated 11 patients with rosiglitazone (4 mg/day) for 1 year. Serum ALT levels returned to normal in 37.5% of eight patients completing 1 year of therapy. In the rosiglitazone group, a control liver biopsy was performed in all patients completing therapy. Although macrovesicular steatosis did not change, serum ALT levels returned to normal in two patients. In this group, fibrosis regressed in two patients, and serum ALT level returned to normal in one of them at the end of treatment. Fibrosis progressed in one patient with a high ALT level at the end of treatment. Although it is difficult to evaluate rosiglitazone's effects on fibrosis in a few patients, we think serum ALT levels are insufficient to assess treatment response. There was no correlation between the rate of macrovesicular steatosis and serum ALT levels after treatment. In our study, the normalization rate of serum ALT levels was lower compared with that in other studies; this may be due to the low doses of drugs or unchanged BMI.
Statistically significantly decreasing rate of hepatosteatosis and improvement of serum ALT levels with diet and exercise were detected in 15 obese patients [8]. In this study, BMI decreased after treatment in control group, but not in treated groups. Similar results were reported with diet and exercise in obese rats. In these rats while macrovesicular steatosis regressed, inflammation did not [22]. Although there have not been many studies, diet and exercise is the only therapy that is suggested in routine treatment of NAFLD. In our study, a positive correlation was detected between BMI and ALT levels (r=0.268, P=0.042). This is compatible with the literature.
In the study by Bacon et al. [23] transferrin saturation was between 58% and 78% in 6% of patients and ferritin levels were 218–1060 ng/ml in 55% of patients diagnosed with NAFLD. Also, Angulo et al. [24] reported similar results. In both of these studies the hepatic iron concentration did not increase. In our study, serum ferritin levels were <300 ng/ml in all patients. Transferrin saturation was <45% in all but two patients in the metformin group. These two patients were nonresponders to metformin therapy. All biopsy specimens were evaluated for iron accumulation before and after treatment and no accumulation was detected.
In our study, the decrease in treatment response rate at month 12 may be due to fluctuations in serum ALT levels. These fluctuations can be seen in the natural course. Ipekci et al. [25] reported that fluctuated serum ALT levels did not reflect treatment response. Our results also support this study. After treatment, histological findings were not correlated with serum ALT levels. For this reason, therapy response of drugs should be evaluated with histology if possible. However, this is so difficult that only 12 patients agreed to control liver biopsy in our study. We should evaluate treatment response with serum ALT levels not just once but with serial ALT controls at least three times in a month.
In conclusion, diet with exercise seems to be superior to metformin and rosiglitazone. Treatment response rate is similar with metformin and rosiglitazone. Diet and exercise is safe and cost-effective and is the only acceptable therapy for today.
References
Ludwig J, Viggiano TR, McGill DB, Oh BJ (1980) Nonalcoholic steatohepatitis. Mayo clinic experiences with a hitherto unnamed disease. Mayo Clin Proc 55:434–438
Day CP, James OFW (1998) Hepatic steatosis: innocent bystander or guilty party? Hepatology 27:1463–1466
Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ (1999) Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology 29:664–669
Bugianesi E, Leone N, Vanni E, Marchesini G, Brunello F, Carucci P, Musso A, De Paolis P, Capussotti L, Salizzoni M, Rizzetto M (2002) Expanding the natural history of non-alcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology 123:134–140
Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ (1999) Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology 116:1413–1419
Drenick EJ, Simmons F, Murphy JF (1970) Effect on hepatic morphology of treatment of obesity by fasting, reducing diets and small bowel bypass. N Engl J Med 282:829–834
Andersen T, Gluud C, Franzmann MB, Christoffersen P (1991) Hepatic effects of dietary weight loss in morbidly obese patients. J Hepatol 12:224–229
Ueno T, Sugawara H, Sujaku K, Hashimoto O, Tsuji R, Tamaki S, Torimura T, Inuzuka S, Sata M, Tanikawa K (1997) Therapeutic effects of restricted diet and exercise in obese patients with fatty liver. J Hepatol 27:103–107
Laurin J, Lindor KD, Crippin JS, Gossard A, Gores GJ, Ludwig J, Rakela J, McGill DB (1996) Ursodeoxycholic acid or clofibrate in the treatment of non-alcoholic-induced steatohepatitis: A pilot study. Hepatology 23:1464–1467
Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenky-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE (2001) Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 108:1167–1174
Marchesini G, Brizi M, Bianchi G, Tomassetti S, Zoli M, Melchionda N (2001) Metformin in nonalcoholic steatohepatitis. Lancet 358:893–894
Uygun A, Kadayifci A, Isik AT, Ozgurtas T, Deveci S, Tuzun A, Yesilova Z, Gulsen M, Dagalp K (2004) Metformin in the treatment of patients with nonalcoholic steatohepatitis. Aliment Pharmacol Ther 19:537–544
Caldwell SH, Hespenheide EE, Redick JA, Iezzoni JC, Battle EH, Sheppard BL (2001) A pilot study of thiazolidinedione, troglitazone, in non-alcoholic steatohepatitis. Am J Gastroenterol 96:519–525
Mayerson, Hundal RS, Dufour S, Lebon V, Befroy D, Cline GW, Enocksson S, Inzucchi SE, Shulman GI, Petersen KF (2002) The effects of rosiglitazone on insulin sensitivity, lipolysis and hepatic and skeletal muscle triglyceride content in patients with type 2 diabetes. Diabetes 51:797–802
Tetri-Neuschwander BA, Brunt EM, Wehmeier KR, Oliver D, Bacon BR (2003) Improved nonalcoholic steatohepatitis after 48 weeks of treatment with the PPAR-γ ligand rosiglitazone. Hepatology 38:1008–1017
Day CP (2003) Management future targets in NAFLD. In ``Non Alcoholic Fatty Liver Disease'' President's premeeting syllabus. 38th annual meeting of the European Association for the study of the liver; Tozun N, Avsar E (eds). Istanbul, A & G Agency, pp 58–65.
Promrat K, Lutchman G, Uwaifo GI, Freedman RJ, Soza A, Heller T, Doo E, Ghany M, Premkumar A, Park Y, Liang TJ, Yanovski JA, Kleiner DE, Hoofnagle JH (2004) A pilot study of pioglitazone treatment for nonalcoholic steatohepatitis. Hepatology 39:188–196
Chitturi S, Abeygunasekera S, Farrell GC, Holmes-Walker J, Hui JM, Fung C, Karim R, Lin R, Samarasinghe D, Liddle C, Weltman M, George J (2002) NASH and insulin resistance: insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology 35:373–379
Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR (1999) Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol 94:2467–2474
Harrison SA, Torgerson S, Hayashi PH, Ward J, Schenker S (2003) Vitamin E and vitamin C treatment improves fibrosis in patients with nonalcoholic steatohepatitis. Am J Gastroenterol 98:2485–2490
Kadayıfcı A (2003) Nonalcoholic steatoepatitis: Role of leptin in pathogenesis and benefits of metformin in treatment. Am J Gastronterol 98:2330
Lin HZ, Yang SQ (2003) Current biochemical studies of nonalcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH) suggest a new therapeutic approach. Am J Gastroenterol 98:495–499
Fan JG, Zhong L, Xu ZJ, Tia LY, Ding XD, Li MS, Wang GL (2003) Effects of low calori diet on steatohepatitis in rats with obesity and hyperlipidemia. World J Gastroenterol 9:2045–2049
Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA (1994) Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology 107:1103–1109
Angulo P, Keach JC, Batts KP, Lindor KD (1999) Independent predictors of liver fibrosis in patients with non-alcoholic steatohepatitis. Hepatology 30:1356–1362
Ipekci SH, Basaranoglu M, Sonsuz A (2003) The fluctuation of serum levels of aminotransferase in patients with nonalcoholic steatohepatitis. J Clin Gastroenterol 18:1220–1221
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akyüz, F., Demir, K., Özdil, S. et al. The Effects of Rosiglitazone, Metformin, and Diet with Exercise in Nonalcoholic Fatty Liver Disease. Dig Dis Sci 52, 2359–2367 (2007). https://doi.org/10.1007/s10620-006-9145-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9145-x