Abstract
Cytokine-induced killer (CIK) cells and T cells expanded by co-stimulation with beads presenting anti-CD3 and -CD28 antibodies are both polyclonal T cells under intensive laboratory and clinical studies, but there has not been any direct comparison between both. We compared the expansion, memory T cell subsets and cytotoxicity for T cells expanded in parallel by the two methods. Bead-stimulated T cells showed superior expansion as compared to CIK cells on D14 of culture. Bead-stimulated T cells consisted of a significantly higher CD4+ subset and significantly lower CD8+ subset as compared to CIK cells, as well as a higher proportion of less terminally differentiated T cells and a higher proportion of homing molecules. On the other hand, CIK cells exhibited significantly superior cytotoxicity against two myelomonocytic leukemia cell lines (THP-1 and U937) and two RCC cell lines (786.0 and CaKi-2). The cytotoxicity on D14 against THP-1 was 58.1 % for CIK cells and 8.3 % for bead-stimulated T cells at E:T of 10:1 (p < 0.01). Cytotoxicity correlated positively with the proportion of the CD8 subset in the culture and was independent of NKG2D recognition of susceptible targets. Polyclonal T cells expanded by different methods exhibit different characteristics which may define the specific role of each in different clinical scenario. We postulate that the more potent CIK cells may offer short term benefit while bead-stimulated T cells may offer a more sustained immune response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adoptive cellular therapy with various immune effector cells is an area of intense laboratory and clinical research. Originating from the early 1980s with Lymphokine-Activated Killer cells as the prototype of immune effector cells comprising a mixture of activated Natural Killer (NK) cells and T cells, culture protocols have been refined over the years. There are now specific protocols with defined and optimized conditions to generate specific cell types, e.g. NK cells, polyclonal T cells or antigen specific T cells.
One of the popularly studied cell types is polyclonal T cell, due to the relatively low technical requirement and easy expansion, under either cytokine stimulation or paramagnetic beads presenting anti-CD3 and -CD28 antibodies. Polyclonal T cells expanded using the protocol described for cytokine-induced killer (CIK) cell culture has demonstrated potent activity against Non-Hodgkin’s lymphoma (NHL) (Schmidt-Wolf et al. 1991), chronic myeloid leukemia (CML) (Hoyle et al. 1998), chronic lymphocytic leukemia (CLL) (Lefterova et al. 2000) and acute myeloid leukemia (AML) (Linn et al. 2002), in both in vitro (Schmidt-Wolf et al. 1991; Linn et al. 2002) and in vivo (mice) experiments (Lu and Negrin 1994; Hoyle et al. 1998). Recent in vitro work has further showed the potential activity of CIK cells against cancer stem cells for melanoma (Gammaitoni et al. 2013) and sarcoma (Sangiolo et al. 2014) treatment. Over the past few years, CIK cell has entered clinical trials as adjuvant therapy for both hematological malignancies (Leemhuis et al. 2005; Jiang et al. 2005; Introna et al. 2006; Linn et al. 2012a, b), and solid tumours (Thanendrarajan et al. 2012; Mesiano et al. 2012). Clinical data are emerging on the modest but promising efficacy of autologous CIK cells against common solid tumours such as non small cell lung cancer (Li et al. 2012b), renal cell carcinoma (RCC) (Liu et al. 2012), nasopharyngeal carcinoma (Li et al. 2012a), hepatocellular carcinoma (Pan et al. 2013) and gastric cancer (Shi et al. 2012).
In contrast, polyclonal T cells expanded using anti-CD3 and anti-CD28 antibodies-coated beads which serve as artificial antigen-presenting cells providing proliferative signals to T cells, are studied in clinical trials for correcting T cell deficiency in HIV patients (Levine et al. 2002), post autologous transplant (Laport et al. 2003; Rapoport et al. 2009) and in solid tumors (Lum et al. 2001; Thompson et al. 2003; Wierda et al. 2004). In recent years, clinical studies have also made use of these bead-expanded T cells to express transduced genes of chimeric antigen receptors (Kalos et al. 2011; Brentjens et al. 2011).
With different culture methods providing different signals to T cells, it is not surprising that composition of these polyclonal T cells differ from each other. Work done separately have consistently shown that CIK cells consist of predominantly CD8+ T cells while bead-co-stimulated T cells (hereby abbreviated as Co-T cells) are in majority CD4+ T cells. While both have demonstrated cytotoxicity towards chosen targets, they have not been compared directly with each other. Here we report our work on the characterization of the T cells generated by both methods in parallel cultures to compare the expansion capacity, T cell subsets and cytotoxic potential of these two cell types.
Materials and methods
Cells and culture methods
Mononuclear cells (MNC) were obtained by Ficoll-Hypaque (GE Healthcare, Uppsala, Sweden) density gradient centrifugation of whole blood from patients with polycythemia or haemochromatosis who undergo therapeutic venesection with IRB approval, and were either directly used or frozen for culture at a later date. CIK cells were cultured based on a previously described method (Hoyle et al. 1998), which involved the timed addition of interferon gamma (Boehringer Ingelheim, Vienna, Austria) at 1,000 U/ml on D0, IL-2 (Novartis, Basel, Switzerland) at 300 U/ml and OKT3 (Janssen-Cilag, Zug, Switzerland) at 50 ng/ml on D1, followed by weekly addition of IL-2 and topping up of medium consisting of 10 % FCS (Hyclone, Logan, UT, USA)/RPMI (Invitrogen, Carlsbad, CA, USA) twice a week. Co-T cells were cultured using Dynabeads® human T-activator CD3/CD28 (Invitrogen Dynal AS, Oslo, Norway) according to manufacturer’s instructions. Beads were added to MNC at a 0.7:1 ratio (which is equivalent to a beads-to-T cell ratio of 1:1, as 70 % of the MNC comprises of T cells), with IL-2 at 30 U/ml in 10 % FCS/RPMI and regular addition of medium with IL-2 twice a week. CIK cells were counted starting from D10 (as it is known that it is too early to evaluate CIK cells on D7), D14, D20 and D26. Co-T cells were counted on D7/D8, D14, D20 and D26. To study the effect of a second stimulation with beads midway through culture, some Co-T cultures were split on D17 where one half was re-stimulated with beads at 1:1 ratio while the other half was continued in culture without re-stimulation.
Immunophenotyping
Monoclonal antibodies used included antiCD8 PE, antiCD56 PE, antiCD27 PE, antiCD28 FITC, anti-CD62L FITC, anti-MICA/B PE (BD Pharmingen, San Jose, CA, USA); anti-CD3 FITC, anti-CD4 FITC, anti-CD4 PC5, anti-CD8 PC5, (Beckman Coulter, Brea, CA, USA), anti-CD45RA FITC (eBioscience, San Diego, CA, USA), and anti-CCR7 PE (R&D Systems, Minneapolis, MN, USA) antibodies. Monoclonal antibody combinations included CD4/CD8, CD3/CD56, and 3-colour combinations: CD4 or CD8 with CD28/CD27 to differentiate between early, intermediate and late effector T cells, CD4 or CD8 with CCR7/CD45RA to measure the proportion of CCR7+CD45RA− central memory T cells. Flow cytometry was done for cells on D0, D7 or D8 (for Co-T cells only), D10 (for CIK cells only), D14 and D26, using BD FACSCalibur (San Jose, CA, USA) or Beckman Coulter CyAn flow cytometer (Brea, CA, USA), and analysed on “The Flowing Software” (http://www.flowingsoftware.com/).
Cytotoxicity assay
Cytotoxicity was studied in a 4 h Chromium release assay as previously described (Linn et al. 2002). Briefly effector cells were suspended with chromium51 (PerkinElmer, Houston, TX, USA)—labelled target at E:T ratio of 2.5:1, 10:1 and 40:1 and radioactivity of supernatant measured on a gamma counter (Hewlett Packard, Palo Alto, CA, USA). Percentage of cytotoxicity was calculated upon the difference between maximum release (lysed by white cell lysis buffer) and spontaneous release. Target cells used included 2 myelomonocytic leukemia cell lines THP-1 and U937, and 2 renal cell carcinoma (RCC) cell lines CaKi-2 and 786.0. In blocking assays, purified anti-NKG2D (clone 1D11, Biolegend, San Diego, CA, USA) at 20 μg/ml was added to CIK cells for 30 min before co-incubation with targets.
Statistical analysis
Data on parallel CIK and Co-T cultures were compared using two-tailed paired Student’s t test, where p < 0.05 was taken as being statistically significant. Correlation test was done using online software “Statpages” .
Results
A total of 9 sets of parallel cultures were done. The first batch consisting of 5 sets of cultures was done on fresh MNC while the second batch of 4 sets was done on thawed MNC. Starting cell number varied between 7 and 12 million MNC per culture.
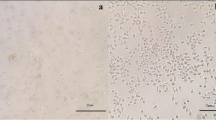
Cell expansion
Expansion of CIK cells and Co-T cells in the first 5 sets generated from fresh samples was comparable at a median of 4.33 fold (range 3.42–5.99) and 4.62 fold (range 1.23–6.13), respectively, on D14 for total cell number. This was a median of 6.59 fold (range 4.55–7.56) and 4.18 fold (range 2.04–6.69), respectively, when analysed for the expansion of CD3 subset. Culture was terminated after D14 for Co-T cells and after D20 for CIK cells. Due to the suboptimal expansion of Co-T cells, the subsequent 4 sets were done on thawed cells as suggested in the technical product data sheet. With this modification, the expansion of Co-T cells improved to reach a median of 17.92 fold (range 12.2–25.6) on D14, 26.4 fold (range 12.5–53.4) on D20 and 29.7 fold (range 14.0–94.9) by D26. This was significantly higher than CIK cells on D14 which expanded a median of 3.53 fold (range 0.72–9.23), see Fig. 1. The expansion of CD3 subset on D14 was also higher in Co-T cells with a median of 38.45 fold (31.67–39.41) as compared to 6.83 fold (3.24–24.16) for CIK cells. However both became comparable thereafter as the expansion of CIK cells increased markedly after D14, reaching a median of 17.2 fold (range 13.6–5.34) on D20 and 26.8 fold (range 19.2–34.5) on D26, not significantly different from Co-T cells at these two latter time points.
Comparison of fold expansion of total cell number and CD3 cells between CIK and Co-T cultures (n = 9) on D14. UPN 3 and 5 and 6 could not be analysed for CD3 fold expansion due to missing data on %CD3+ cells on D0 for UPN3 and 5, and missing data on %CD3+ cells of CIK on D14 for UPN6. Co-T cells expanded significantly better than CIK cells in terms of both total cell number and CD3+ subset, for the 4 sets of cultures started from thawed MNC
Comparison of T cell subsets in CIK and Co-T cells
CD3+CD56+ subset
Co-expression of CD3 and CD56 is the hallmark of CIK cells. We found that the CD3+CD56+ NK-like T cell subset was significantly higher in CIK cells as compared to Co-T cells at various time-points. This was a median of 3.46 % (range 0.79–4.63 %) for Co-T on D7/8 and a median of 8.13 % (range 3.63–27.3 %) for CIK on D10; 6.35 % (range 2.58–26.93 %) for Co-T and 19.68 % (range 9.07–59.71 %) for CIK on D14, and 12.59 % (range 6.73–18.42 %) for Co-T and 26.59 (range 20.2–32.98) for CIK on D26, see Fig. 2a. CD3−CD56+NK cells remained at low level below 5 % and did not differ between CIK and Co-T cells.
a Comparison of %CD3+CD56+ NK-like T cell subsets in CIK and Co-T cells over time (n = 6). Proportion of CD3+CD56+ NK-like T cell was consistently higher in CIK cells than in Co-T cells at all time points studied for all 6 sets of comparison. b Comparison of CD4+ and CD8+ subsets in CIK and Co-T cells over time (n = 6). CIK cells had higher proportion of CD8+ subset and lower proportion of CD4+ subset than Co-T cells at all time points studied for all 6 sets of comparison
CD4+ and CD8+ subsets
Consistent with what was previously described, CIK cells contained significantly higher CD8+ subset and correspondingly lower CD4+ subset than Co-T cells. The difference was observed early, being statistically significant between Co-T cells on D7/8 and CIK cells on D10, and was maintained throughout the whole period of culture on D14 and D26. See Fig. 2b for the evolution of CD4+ and CD8+ subsets of CIK and Co-T cells over time.
Memory T cell subsets
TCM subset
Serial immunophenotyping was done on CIK and Co-T cells to compare the memory T cell (TMEM) subsets in both CD4+ and CD8+ populations, respectively. At early phase of culture (D7/8 for Co-T cells and D10 for CIK cells), there was generally a rise in CD45RA− CCR7+ central memory T cells (TCM), which declined over time to a level below the starting proportion. Generally Co-T cells expressed a higher TCM subset than their CIK counterpart. This reached statistical significance for the CD4+ subset (p = 0.05), see Fig. 3a, but not for the CD8+ subset (p = 0.08) of Co-T cells on D14, in comparison with CIK cells.
a Comparison of CD45RA−CCR7+ TCM subset between CIK and Co-T cells over time (n = 6), showing the higher proportion of TCM in the CD4+ subset in Co-T cells as compared to CIK cells. b Comparison of CD27+CD28+ early TE subset between CIK and Co-T cells over time (n = 6), showing the higher proportion of early TE in the CD8+ subset in Co-T cells as compared to CIK cells. c Comparison of CD62L expression between CIK and Co-T cells over time (n = 6), showing the higher proportion of CD62L expression in the CD4+ subset in Co-T cells as compared to CIK cells
TE subsets
As for effector T cell subsets (TE), the early TE as represented by a CD27+CD28+ phenotype was generally highest in the pre-culture MNC and consistently higher in CD4+ subset as compared to CD8+ subset, and declined progressively over the culture period. Throughout the culture period, CD8+ Co-T cells had a significantly higher (p = 0.013) early TE as compared to CD8+ CIK cells, see Fig. 3b, while that for CD4+ subsets did not reach statistical significance (p = 0.09).
Lymph node homing potential
We also studied the expression of CD62L which is a molecule with capacity to home to lymph nodes. CD62L was highly expressed in pre-culture MNC, especially so in the CD4+ subset as compared to CD8+ subsets. The expression decreased over time in culture for both CIK cells and Co-T cells, but was significantly lower in CIK cells as compared to Co-T cells in the CD4+ subset (p = 0.026), see Fig. 3c, and to a lesser extent in the CD8+ subset but not reaching statistical significance (p = 0.087).
Comparison of cytotoxicity between CIK cells and Co-T cells
Cytotoxicity against leukemia and RCC cell lines
We assessed cytotoxicity by Chromium release assay against the myelomonocytic leukemia cell lines THP-1 and U937. This was done in parallel for CIK and Co-T cultures on D14 and D26. CIK cells demonstrated remarkably superior cytotoxicity over Co-T cells at both time-points, see Fig. 4a. Cytotoxicity assay was also done against RCC cell lines 786.0 and CaKi-2 to compare between CIK and Co-T in the killing of non-haematological targets. Despite generally lower susceptibility of the two RCC cell lines as compared to THP-1 and U937 to cell-mediated cytotoxicity, CIK cells were still significantly more potent as compared to Co-T cells, in the 2 sets of CIK and Co-T on D17 against the 2 RCC targets, see Fig. 4b.
a Comparison of cytotoxicity against THP-1 between CIK and Co-T cells on D14 (n = 8) and D26 (n = 2), showing consistently higher cytotoxicity of CIK cells. Median cytotoxicity on D14 was 58.1 % for CIK cells and 8.3 % for Co-T cells, at E:T of 10:1. This was 74.7 and 23.0 %, respectively, at E:T of 40:1, p < 0.01. b Comparison of cytotoxicity against 2 RCC cell lines between CIK and Co-T cells (n = 2), showing higher cytotoxicity of CIK cells
Mediator of cytotoxicity
In an attempt to explain the superior cytotoxicity of CIK cells over Co-T cells, we postulated that it was due to the larger proportion of CD8+ cells in CIK as compared to Co-T cell culture that conferred the more potent target killing. In fact we demonstrated a significant positive correlation between %CD8+ subset and %cytotoxicity (R = 0.532, p < 0.012), as shown in Fig. 5a. As NKG2D is found only in CD8+ T cells and absent in CD4+ T cells, we investigated whether NKG2D is the receptor responsible for recognition of THP-1 and U937. Blocking experiments showed that blocking with antiNKG2D MoAb did not abrogate CIK killing of these 2 targets, see Fig. 5b. Furthermore, FACS analysis for MICA/B showed only 12–13 % expression of MICA/B on both THP-1 and U937, see Fig. 5c. Paradoxically, the RCC cell lines 786.0 and CaKi-2 with relatively poor susceptibility to CIK-mediated killing were uniformly positive in MICA/B antigen, see Fig. 5d.
a Correlation between %CD8+ subset and % cytotoxicity showing a positive correlation with R of 0.532, p < 0.012. b Cytotoxicity of CIK cells against U937 and THP1 without and with blocking of NKG2D receptor (n = 2), showing a lack of effect of NKG2D blocking on cytotoxicity against these 2 targets. c Expression of MICA/B on myelomonocytic cell lines THP-1 and U937. d Expression of MICA/B on RCC cell lines 786.0 and CaKi-2
Effect of re-stimulation with beads for Co-T cultures
Four sets of Co-T cultures were each split into two halves on D17 where one half was re-stimulated with beads at 1:1 ratio, while the other half was continued in culture. We found no difference in the expansion and cytotoxicity between Co-T cells stimulated once (Co-Tx1) or twice (Co-Tx2), when assessed at D26, ie 9 days after re-stimulation, see Fig. 6a. Re-stimulation resulted in an increase in CD4+ subset and decrease in CD8+ subset. The CD3+CD56+ subset decreased after re-stimulation but did not reach statistical significance, see Fig. 6b.
a Comparison of cytotoxicity on D26 between cultures stimulated once and twice with beads (restimulated on D17, n = 4), showing lack of consistent or significant difference in the cytotoxicity whether T cells were stimulated once or twice with beads. b Comparison of %CD8+ and %CD3+CD56+ subset between cultures stimulated once and twice with beads (n = 4). T cells stimulated twice with beads showed a consistent reduction in the proportion of CD8+ and CD3+CD56+ subsets
Discussion
Polyclonal T cells expanded by cytokine stimulation such as CIK cells, or by stimulation with paramagnetic beads presenting CD3 and CD28 antibodies such as Co-T cells, have both been used in clinical cancer trials. The choice of either is largely dependent on the availability and expertise of individual centre rather than consideration for the suitability of each for specific purposes. While the characteristic of CIK and Co-T cells has been described extensively in work done on each, they have not been directly compared to assess how significant the differences are. In this study we followed the reported methodology to culture in parallel both CIK cells (Hoyle et al. 1998) and Co-T cells (Laport et al. 2003; Levine et al. 1998). By comparing their growth, T cell subsets and functional characteristics, we demonstrated a few fundamental differences between these two cell types.
Rapid and early expansion of Co-T cell is one of the remarkable features of CD3/CD28 beads, with expansion exceeding 100 fold (Porter et al. 2006; Laport et al. 2003; Thompson et al. 2003; Lum et al. 2001; Garlie et al. 1999), much higher than that achievable in CIK cultures (Niam et al. 2011; Leemhuis et al. 2005; Laport et al. 2011; Linn et al. 2012a, b). Our results using thawed cells is consistent with this, showing significantly superior expansion of Co-T over CIK cells on D14, while the expansion of CIK cells largely occured after D14, consistent with our previous observation (Niam et al. 2011). Studies into optimizing culture condition of Co-T e.g. re-simulation with beads have shown conflicting results with some others reporting increased proliferation with re-stimulation (Levine et al. 1997) while others have found that re-stimulation negatively affected the culture (Li and Kurlander 2010), and in fact early beads removal enhanced expansion and viability (Garlie et al. 1999). The wide range in fold expansion amongst the numerous published work on Co-T cells underscore the effect of subtle variation in methodology, e.g. culture medium used, cell density, feeding schedule, IL-2 concentration etc., on expansion. In this study, in order to follow standardized protocols, we cultured at a cell density and IL-2 concentration according to the Dynabeads® Human T-Activator CD3/CD28 product instruction for Co-T cell expansion. Similarly for CIK cell cultures, we followed the standard cytokine condition widely and uniformly used for its expansion. While the IL-2 concentration is different between the two cultures, they are based on standard conditions for the culture of each cell type. However, research done over the years with some modifications in the culture conditions has brought significant improvement in the function of such polyclonal T cells. For example, IL-15 in place of IL-2 generated CIK cells that are able to kill primary ALL cells previously known to be resistant to standard CIK cells (Rettinger et al. 2012). Such IL-15 activated CIK cells were further shown to be safe for infusion into haplo-identical transplant recipients at a high dose without causing graft vs host disease (Rettinger et al. 2013), which is of great clinical relevance. Manipulation of cytokine conditions shortly before cytotoxicity assay is another means of potentiating the cytotoxicity of CIK cells, such as overnight incubation with interferon-alpha could increase cytotoxicity of cord blood-derived CIK cells against ALL targets (Durrieu et al. 2012). Addition of high dose IL-2, IL-12, especially stimulation with human T-activator CD3/CD28 beads for 24 h could upregulate chemokine receptor expression of CIK cells resulting in enhanced in vivo trafficking and cytotoxicity in mice bearing colorectal cancer (Zou et al. 2014).
It is known that CIK cells are enriched for CD8+ T cells in contrast to Co-T cells which preferentially expand CD4+ subset under co-stimulation with CD28. In addition, the “NK-like T cell” subset co-expressing CD3 and CD56 mediating non-MHC restricted cytotoxicity, which has been consistently shown to be highly expressed in CIK cells, is also found to be higher in CIK than in Co-T cells. Together these differences in the composition of polyclonal T cells could explain the much superior cytotoxicity of CIK cells over that of Co-T cells. The higher proportion of CD8+ cells in CIK cells raises the possibility of an NKG2D dependent mechanism of target recognition as NKG2D is expressed on CD8+ but not CD4+ T cells. Interestingly and consistent with our previous experiments (Linn et al. 2009), this was found not to be the case, as blockade of NKG2D did not abrogate cytotoxicity. Corroborating with this, THP-1 and U937 which are very susceptible to CIK-mediated cytotoxicity express only very low levels of the NKG2D ligand MICA/B, while both RCC cell lines with poor susceptibility to CIK cells express high levels of MICA/B. This is contrary to that reported by others on CIK cells, where NKG2D was demonstrated to be an important receptor for recognition of plasmacytoma (Verneris et al. 2004) and ovarian tumour cells (Karimi et al. 2005). This suggests that there is more than one mechanism in the CIK cell recognition of tumour targets, such as TRAIL mediated cytotoxicity which were not studied in this current work, but has been described by others (Durrieu et al. 2012; Kuçi et al. 2010). Our previous work showed that CIK-mediated cytotoxicity of allogeneic targets are non-MHC restricted but still involves recognition through T cell receptor (Linn et al. 2009). Therefore the superiority in target killing of CIK cells consisting of a higher proportion of CD8+ T cells may simply be due to the more potent cytotoxicity of CD8+ subset as compared to the weaker cytotoxicity of CD4 subset. In fact, infusion of CIK cells with higher CD8+ subset was shown to be associated with superior survival in patients with liver, lung and colorectal cancers (Pan et al. 2014), which may be a result of the higher cytotoxicity mediated by this subset.
Work done on adoptive cellular therapy in recent years have established the paradigm that T cells that are less differentiated, while lower in potency, are more highly proliferative in vivo as compared to terminally differentiated T cells which are more potent but do not persist long term in vivo (Gattinoni et al. 2005). The proportion of CD27+CD28+ early TE, as well as CCR7+CD45RA− TCM were generally higher in Co-T cells as compared to their CIK counterpart at the same time-points, in both CD4+ and CD8+ subsets and reaching statistical significance in some of them. Based on these observations we postulate that Co-T cells may behave more like the former while CIK cells are more representative of the latter. The higher CD62L may also imply better homing to lymph nodes. Certainly these are just inference from phenotypic expression and needs to be proven by in vivo studies, e.g. using gene-transduced CIK and Co-T cells to visualize in vivo persistence and response to antigenic re-challenge.
Both Co-T and CIK cells have been studied in clinical trials. Co-T cells have been shown to result in normalization of TCRVβ receptor repertoire and lymphocytosis in patients post-autologous haemopoietic stem cell transplant (autoHSCT) for NHL (Laport et al. 2003)) and in HIV patients (Levine et al. 2002). In combination with pneumococcal vaccination post autoHSCT for multiple myeloma (MM), it has facilitated restoration of CD4 function and T cell response against vaccinated and non-vaccinated antigens (Rapoport et al. 2005). In the treatment of malignancies, Co-T cells given without other concomitant therapy to patients with CLL was shown to reduce spleen and lymph node size but not lymphocytosis (Wierda et al. 2004). Earlier phase I trials demonstrated safety but no efficacy in patients with various solid tumours (Thompson et al. 2003; Lum et al. 2001). Other studies investigated safety and feasibility when incorporated into autoHSCT for CML (Rapoport et al. 2004) and MM (Borrello et al. 2004), where efficacy will be difficult to demonstrate. Of note, it has also been used in allogeneic haemopoietic stem cell transplant (alloHSCT) as an activated donor lymphocyte infusion (DLI), showing feasibility and safety (Porter et al. 2006).
Similarly, CIK cells have gained widespread popularity internationally (Hontscha et al. 2011) and showed some modest promise in clinical trials. It has been used in post autoHSCT for Hodgkin’s disease and NHL showing safety and a modest efficacy (Leemhuis et al. 2005). Autologous CIK cells have shown variable degree of efficacy in clinical trials for solid tumours (Mesiano et al. 2012), including lung (Li et al. 2012b), liver (Pan et al. 2013), renal (Liu et al. 2012), nasopharyngeal (Li et al. 2012a) and gastric cancers (Shi et al. 2012). Investigators from China reported remarkable superiority in combination with chemotherapy for acute leukemia as compared to chemotherapy alone (Jiang et al. 2005). We have confirmed feasibility and safety but failed to demonstrate efficacy of autologous CIK cells in patients with AML post autoHSCT or CML in minimal residual disease state (Linn et al. 2012b). In contrast, allogeneic CIK cells used after alloHSCT appear to be promising. Similar to the experience of Co-T as a form of activated DLI, allogeneic CIK cells have demonstrated safety (Laport et al. 2011) and anecdotal superiority (Introna et al. 2007; Linn et al. 2012a) over un-manipulated DLI in the treatment of haematological malignancies post alloHSCT, without increased risk of GVHD, although response was not sustainable in some of them. In fact, CIK cells may have a real advantage over Co-T cells in the allogeneic setting, as the CD3+CD56+ subset, which is much higher in CIK cells, lack alloreactivity against HLA mismatched target in comparison to its CD3+CD56− counterpart while possessing superior tumoricidal activity (Sangiolo et al. 2008).
While currently available clinical data indicate that there is much room for improvement for both cell types, there is a theoretical complementary role for both with possibility of improving efficacy. While CIK cells provide the more potent and immediate cytotoxicity against tumour cells, Co-T cells offer a larger number to restore immunity and the possibility of long term proliferative capacity due to its less differentiated TMEM profile. The unique characteristics of each may define the specific indication for preference of one over the other in different clinical settings. In situations where the polyclonal T cells are used as a vehicle for short term expression of transduced genes, or used with bispecific antibodies for redirecting to tumour target, CIK cells with their higher potency may be the preferred effector cells. On the other hand, for the purpose of immune reconstitution post autoHSCT or in immunodeficiency states, Co-T cells may offer a longer sustainability after adoptive transfer. Combining both methods such as that explored by Zou et al. (2014) by co-incubating matured CIK cells with beads to exploit the best of both is also worth further exploration. We believe that our comparison of the two prototypes of polyclonal T cells generated under standard protocols enables understanding of the unique fundamental characteristics of each and provides the basis for exploration to improve the culture method to overcome the weakness and enhance the strength of each, thereby optimizing the outcome of adoptive cellular therapy with polyclonal T cells.
References
Borrello IM, Vij R, Vescio RA, Martin TG, Siegel D, Berenson JR, Janmohamed F, Bonyhadi M, Berenson RJ, Frohlich MW (2004) A phase I/II study of Xcellerated T cells after autologous peripheral blood stem cell transplantation in patients with multiple myeloma. J Clin Oncol 22:2540 (2004 ASCO Annual Meeting Proceedings, July 15 Supplement)
Brentjens RJ, Rivière I, Park JH, Davila ML, Wang X, Stefanski J, Taylor C, Yeh R, Bartido S, Borquez-Ojeda O, Olszewska M, Bernal Y, Pegram H, Przybylowski M, Hollyman D, Usachenko Y, Pirraglia D, Hosey J, Santos E, Halton E, Maslak P, Scheinberg D, Jurcic J, Heaney M, Heller G, Frattini M, Sadelain M (2011) Safety and persistence of adoptively transferred autologous CD19-targeted T cells in patients with relapsed or chemotherapy refractory B-cell leukemias. Blood 118:4817–4828
Durrieu L, Gregoire-Gauthier J, Dieng MM, Fontaine F, le Deist F, Haddad E (2012) Human interferon-alpha increases the cytotoxic effect of CD56(+) cord blood-derived cytokine-induced killer cells on human B-acute lymphoblastic leukemia cell lines. Cytotherapy 14:1245–1257
Gammaitoni L, Giraudo L, Leuci V, Todorovic M, Mesiano G, Picciotto F, Pisacane A, Zaccagna A, Volpe MG, Gallo S, Caravelli D, Giacone E, Venesio T, Balsamo A, Pignochino Y, Grignani G, Carnevale-Schianca F, Aglietta M, Sangiolo D (2013) Effective activity of cytokine-induced killer cells against autologous metastatic melanoma including cells with stemness features. Clin Cancer Res 19:4347–4358
Garlie NK, LeFever AV, Siebenlist RE, Levine BL, June CH, Lum LG (1999) T cells coactivated with immobilized anti-CD3 and anti-CD28 as potential immunotherapy for cancer. J Immunother 22:336–345
Gattinoni L, Klebanoff CA, Palmer DC, Wrzesinski C, Kerstann K, Yu Z, Finkelstein SE, Theoret MR, Rosenberg SA, Restifo NP (2005) Acquisition of full effector function in vitro paradoxically impairs the in vivo antitumor efficacy of adoptively transferred CD8+ T cells. J Clin Investig 115:1616–1626
Hontscha C, Borck Y, Zhou H, Messmer D, Schmidt-Wolf IGH (2011) Clinical trials on CIK cells: first report of the international registry on CIK cells (IRCC). J Cancer Res Clin Oncol 137:305–310
Hoyle C, Bangs CD, Chang P, Kamel O, Mehta B, Negrin RS (1998) Expansion of Philadelphia chromosome-negative CD3(+)CD56(+) cytotoxic cells from chronic myeloid leukemia patients: in vitro and in vivo efficacy in severe combined immunodeficiency disease mice. Blood 92:3318–3327
Introna M, Franceschetti M, Ciocca A, Borleri G, Conti E, Golay J, Rambaldi A (2006) Rapid and massive expansion of cord blood-derived cytokine-induced killer cells: an innovative proposal for the treatment of leukemia relapse after cord blood transplantation. Bone Marrow Transpl 38:621–627
Introna M, Borleri G, Conti E, Franceschetti M, Barbui AM, Broady R, Dander E, Gaipa G, D’Amico G, Biagi E, Parma M, Pogliani EM, Spinelli O, Baronciani D, Grassi A, Golay J, Barbui T, Biondi A, Rambaldi A (2007) Repeated infusions of donor-derived cytokine-induced killer cells in patients relapsing after allogeneic stem cell transplantation: a phase I study. Haematologica 92:952–959
Jiang H, Liu KY, Tong CR, Jiang B, Lu DP (2005) The efficacy of chemotherapy in combination with auto-cytokine-induced killer cells in acute leukemia. Zhonghua Nei Ke Za Zhi 44:198–201
Kalos M, Levine BL, Porter DL, Katz S, Grupp SA, Bagg A, June CH (2011) T cells with chimeric antigen receptors have potent antitumor effects and can establish memory in patients with advanced leukemia. Sci Transl Med 3:95ra73
Karimi M, Cao TM, Baker JA, Verneris MR, Soares L, Negrin RS (2005) Silencing human NKG2D, DAP10, and DAP12 reduces cytotoxicity of activated CD8+ T cells and NK cells. J Immunol 175:7819–7828
Kuçi S, Rettinger E, Voss B, Weber G, Stais M, Kreyenberg H, Willasch A, Kuçi Z, Koscielniak E, Klöss S, von Laer D, Klingebiel T, Bader P (2010) Efficient lysis of rhabdomyosarcoma cells by cytokine-induced killer cells: implications for adoptive immunotherapy after allogeneic stem cell transplantation. Haematologica 95:1579–1586
Laport GG, Levine BL, Stadtmauer EA, Schuster SJ, Luger SM, Grupp S, Bunin N, Strobl FJ, Cotte J, Zheng Z, Gregson B, Rivers P, Vonderheide RH, Liebowitz DN, Porter DL, June CH (2003) Adoptive transfer of costimulated T cells induces lymphocytosis in patients with relapsed/refractory non-Hodgkin lymphoma following CD34+ -selected hematopoietic cell transplantation. Blood 102:2004–2013
Laport GG, Sheehan K, Baker J, Armstrong R, Wong RM, Lowsky R, Johnston LJ, Shizuru JA, Miklos D, Arai S, Benjamin JE, Weng WK, Negrin RS (2011) Adoptive immunotherapy with cytokine-induced killer cells for patients with relapsed hematologic malignancies after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transpl 17:1679–1687
Leemhuis T, Wells S, Scheffold C, Edinger M, Negrin RS (2005) A phase I trial of autologous cytokine-induced killer cells for the treatment of relapsed Hodgkin disease and non-Hodgkin lymphoma. Biol Blood Marrow Transpl 11:181–187
Lefterova P, Schakowski F, Buttgereit P, Scheffold C, Huhn D, Schmidt-Wolf IG (2000) Expansion of CD3+CD56+ cytotoxic cells from patients with chronic lymphocytic leukemia: in vitro efficacy. Haematologica 85:1108–1109
Levine BL, Bernstein WB, Connors M, Craighead N, Lindsten T, Thompson CB, June CH (1997) Effects of CD28 costimulation on long-term proliferation of CD4+ T cells in the absence of exogenous feeder cells. J Immunol 159:5921–5930
Levine BL, Cotte J, Small CC, Carroll RG, Riley JL, Bernstein WB, Van Epps DE, Hardwick RA, June CH (1998) Large-scale production of CD4+ T cells from HIV-1-infected donors after CD3/CD28 costimulation. J Hematother 7:437–448
Levine BL, Bernstein WB, Aronson NE, Schlienger K, Cotte J, Perfetto S, Humphries MJ, Ratto-Kim S, Birx DL, Steffens C, Landay A, Carroll RG, June CH (2002) Adoptive transfer of costimulated CD4+ T cells induces expansion of peripheral T cells and decreased CCR5 expression in HIV infection. Nat Med 8:47–53
Li Y, Kurlander RJ (2010) Comparison of anti-CD3 and anti-CD28-coated beads with soluble anti-CD3 for expanding human T cells: differing impact on CD8 T cell phenotype and responsiveness to restimulation. J Transl Med 8:104
Li JJ, Gu MF, Pan K, Liu LZ, Zhang H, Shen WX, Xia JC (2012a) Autologous cytokine-induced killer cell transfusion in combination with gemcitabine plus cisplatin regimen chemotherapy for metastatic nasopharyngeal carcinoma. J Immunother 35:189–195
Li R, Wang C, Liu L, Du C, Cao S, Yu J, Wang SE, Hao X, Ren X, Li H (2012b) Autologous cytokine-induced killer cell immunotherapy in lung cancer: a phase II clinical study. Cancer Immunol Immunother 61:2125–2133
Linn YC, Lau LC, Hui KM (2002) Generation of cytokine-induced killer cells from leukaemic samples with in vitro cytotoxicity against autologous and allogeneic leukaemic blasts. Br J Haematol 116:78–86
Linn YC, Lau SKJ, Liu BH, Ng LH, Yong HX, Hui KM (2009) Characterization of the recognition and functional heterogeneity exhibited by cytokine-induced killer cell subsets against acute myeloid leukaemia target cell. Immunology 126:423–435
Linn YC, Niam M, Chu S, Choong A, Yong HX, Heng KK, Hwang W, Loh Y, Goh YT, Suck G, Chan M, Koh M (2012a) The anti-tumour activity of allogeneic cytokine-induced killer cells in patients who relapse after allogeneic transplant for haematological malignancies. Bone Marrow Transpl 47:957–966
Linn YC, Yong HX, Niam M, Lim TJ, Chu S, Choong A, Chuah C, Goh YT, Hwang W, Loh Y, Ng HJ, Suck G, Chan M, Koh M (2012b) A phase I/II clinical trial of autologous cytokine-induced killer cells as adjuvant immunotherapy for acute and chronic myeloid leukemia in clinical remission. Cytotherapy 14:851–859
Liu L, Zhang W, Qi X, Li H, Yu J, Wei S, Hao X, Ren X (2012) Randomized study of autologous cytokine-induced killer cell immunotherapy in metastatic renal carcinoma. Clin Cancer Res 18:1751–1759
Lu PH, Negrin RS (1994) A novel population of expanded human CD3+ CD56+ cells derived from T cells with potent in vivo antitumor activity in mice with severe combined immunodeficiency. J Immunol 153:1687–1696
Lum LG, LeFever AV, Treisman JS, Garlie NK, Hanson JP Jr (2001) Immune Modulation in Cancer Patients After Adoptive Transfer of Anti-CD3/Anti-CD28-Costimulated T Cells-Phase I Clinical Trial. J Immunother 24:408–419
Mesiano G, Todorovic M, Gammaitoni L, Leuci V, Giraudo Diego L, Carnevale-Schianca F, Fagioli F, Piacibello W, Aglietta M, Sangiolo D (2012) Cytokine-induced killer (CIK) cells as feasible and effective adoptive immunotherapy for the treatment of solid tumors. Expert Opin Biol Ther 12:673–684
Niam M, Linn YC, Fook Chong S, Lim TJ, Chu S, Choong A, Yong HX, Suck G, Chan M, Koh M (2011) Clinical scale expansion of cytokine-induced killer cells is feasible from healthy donors and patients with acute and chronic myeloid leukemia at various stages of therapy. Exp Hematol 39(897.e1):903.e1
Pan K, Li YQ, Wang W, Xu L, Zhang YJ, Zheng HX, Zhao JJ, Qiu HJ, Weng DS, Li JJ, Wang QJ, Huang LX, He J, Chen SP, Ke ML, Wu PH, Chen MS, Li SP, Xia JC, Zeng YX (2013) The efficacy of cytokine-induced killer cell infusion as an adjuvant therapy for postoperative hepatocellular carcinoma patients. Ann Surg Oncol 20:4305–4311
Pan K, Wang QJ, Liu Q, Zheng HX, Li YQ, Weng DS, Li JJ, Huang LX, He J, Chen SP, Ke ML, Zeng YX, Xia JC (2014) The phenotype of ex vivo generated cytokine-induced killer cells is associated with overall survival in patients with cancer. Tumour Biol 35:701–707
Porter DL, Levine BL, Bunin N, Stadtmauer EA, Luger SM, Goldstein S, Loren A, Phillips J, Nasta S, Perl A, Schuster S, Tsai D, Sohal A, Veloso E, Emerson S, June CH (2006) A phase 1 trial of donor lymphocyte infusions expanded and activated ex vivo via CD3/CD28 costimulation. Blood 107:1325–1331
Rapoport AP, Levine BL, Badros A, Meisenberg B, Ruehle K, Nandi A, Rollins S, Natt S, Ratterree B, Westphal S, Mann D, June CH (2004) Molecular remission of CML after autotransplantation followed by adoptive transfer of costimulated autologous T cells. Bone Marrow Transpl 33:53–60
Rapoport AP, Stadtmauer EA, Aqui N, Badros A, Cotte J, Chrisley L, Veloso E, Zheng Z, Westphal S, Mair R, Chi N, Ratterree B, Pochran MF, Natt S, Hinkle J, Sickles C, Sohal A, Ruehle K, Lynch C, Zhang L, Porter DL, Luger S, Guo C, Fang HB, Blackwelder W, Hankey K, Mann D, Edelman R, Frasch C, Levine BL, Cross A, June CH (2005) Restoration of immunity in lymphopenic individuals with cancer by vaccination and adoptive T-cell transfer. Nat Med 11:1230–1237
Rapoport AP, Stadtmauer EA, Aqui N, Vogl D, Chew A, Fang HB, Janofsky S, Yager K, Veloso E, Zheng Z, Milliron T, Westphal S, Cotte J, Huynh H, Cannon A, Yanovich S, Akpek G, Tan M, Virts K, Ruehle K, Harris C, Philip S, Vonderheide RH, Levine BL, June CH (2009) Rapid immune recovery and graft-versus-host disease-like engraftment syndrome following adoptive transfer of Costimulated autologous T cells. Clin Cancer Res 15:4499–4507
Rettinger E, Kuçi S, Naumann I, Becker P, Kreyenberg H, Anzaghe M, Willasch A, Koehl U, Bug G, Ruthardt M, Klingebiel T, Fulda S, Bader P (2012) The cytotoxic potential of interleukin-15-stimulated cytokine-induced killer cells against leukemia cells. Cytotherapy 14:91–103
Rettinger E, Bonig H, Wehner S, Lucchini G, Willasch A, Jarisch A, Soerensen J, Esser R, Rossig C, Klingebiel T, Bader P (2013) Feasibility of IL-15-activated cytokine-induced killer cell infusions after haploidentical stem cell transplantation. Bone Marrow Transpl 48:1141–1143
Sangiolo D, Martinuzzi E, Todorovic M, Vitaggio K, Vallario A, Jordaney N, Carnevale-Schianca F, Capaldi A, Geuna M, Casorzo L, Nash RA, Aglietta M, Cignetti A (2008) Alloreactivity and anti-tumor activity segregate within two distinct subsets of cytokine-induced killer (CIK) cells: implications for their infusion across major HLA barriers. Int Immunol 20:841–848
Sangiolo D, Mesiano G, Gammaitoni L, Leuci V, Todorovic M, Giraudo L, Cammarata C, Dell’Aglio C, D’Ambrosio L, Pisacane A, Sarotto I, Miano S, Ferrero I, Carnevale-Schianca F, Pignochino Y, Sassi F, Bertotti A, Piacibello W, Fagioli F, Aglietta M, Grignani G (2014) Cytokine-induced killer cells eradicate bone and soft-tissue sarcomas. Cancer Res 74:119–129
Schmidt-Wolf IG, Negrin RS, Kiem HP, Blume KG, Weissman IL (1991) Use of a SCID mouse/human lymphoma model to evaluate cytokine-induced killer cells with potent antitumor cell activity. J Exp Med 174:139–149
Shi L, Zhou Q, Wu J, Ji M, Li G, Jiang J, Wu C (2012) Efficacy of adjuvant immunotherapy with cytokine-induced killer cells in patients with locally advanced gastric cancer. Cancer Immunol Immunother 61:2251–2259
Thanendrarajan S, Kim Y, Schmidt-Wolf I (2012) New adoptive immunotherapy strategies for solid tumours with CIK cells. Expert Opin Biol Ther 12:565–572
Thompson JA, Figlin RA, Sifri-Steele C, Berenson RJ, Frohlich MW (2003) A phase I trial of CD3/CD28-activated T cells (Xcellerated T cells) and interleukin-2 in patients with metastatic renal cell carcinoma. Clin Cancer Res 9:3562–3570
Verneris MR, Karami M, Baker J, Jayaswal A, Negrin RS (2004) Role of NKG2D signaling in the cytotoxicity of activated and expanded CD8+ T cells. Blood 103:3065–3072
Wierda WG, Kipps TJ, Castro J, Keating MJ, Bole J, Anderson B, Meyer J, Anderson K, Berenson R J, Frohlich MW (2004) A Phase I/II trial of CD3/CD28 activated T cells in patients with chronic lymphocytic leukemia (CLL). J Clin Oncol 22:2566 (2004 ASCO Annual Meeting Proceedings (Post-Meeting Edition), July 15 Supplement)
Zou Y, Li F, Hou W, Sampath P, Zhang Y, Thorne SH (2014) Manipulating the expression of chemokine receptors enhances delivery and activity of cytokine-induced killer cells. Br J Cancer 110:1992–1999
Acknowledgments
The authors would like to thank their laboratory colleagues in Singapore General Hospital and National Cancer Center for their kind assistance in one way or other. This work was supported by funding from SingHealth Foundation PTC02/2007/005.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chan, WC., Linn, YC. A comparison between cytokine- and bead-stimulated polyclonal T cells: the superiority of each and their possible complementary role. Cytotechnology 68, 735–748 (2016). https://doi.org/10.1007/s10616-014-9825-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10616-014-9825-x