Abstract
As cellular models for in vitro liver cancer and toxicity studies, HepG2 and Hep3B are the two most frequently used liver cancer cell lines. Because of their similarities they are often treated as the same in experimental studies. However, there are many differences that have been largely over-sighted or ignored between them. In this review, we summarize the differences between HepG2 and Hep3B cell lines that can be found in the literature based on PubMed search. We particularly focus on the differential gene expression, differential drug responses (chemosensitivity, cell cycle and growth inhibition, and gene induction), signaling pathways associated with these differences, as well as the factors in governing these differences between HepG2 and Hep3B cell lines. Based on our analyses of the available data, we suggest that neither HBx nor p53 may be the crucial factor to determine the differences between HepG2 and Hep3B cell lines although HBx regulates the expression of the majority of genes that are differentially expressed between HepG2 and Hep3B. Instead, the different maturation stages in cancer development of the original specimen between HepG2 and Hep3B may be responsible for the differences between them. This review provides insight into the molecular mechanisms underlying the differences between HepG2 and Hep3B and help investigators especially the beginners in the areas of liver cancer research and drug metabolism to fully understand, and thus better use and interpret the data from these two cell lines in their studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary liver cancer, predominantly hepatoblastoma (HB) and hepatocellular carcinoma (HCC), is one of the most common solid tumors, ranking fifth in incidence rate and third in cause of mortality worldwide (Calvisi et al. 2006). For in vitro studies of this particular cancer, HepG2 and Hep3B cell lines are frequently employed as experimental models because they are not only the most popularly available and well characterized liver cancer cell lines but also share many common characteristics, thus providing a unique platform for parallel comparisons. Furthermore, these two cell lines are also widely used as cellular reference models in pharmaceutical studies which aim to develop new drugs and to gain insights into drug metabolism, including knowledge about involved enzymes and the drug's inhibition or induction potential. It is important to note that the two cell lines, especially HepG2, express the majority of drug-metabolising enzymes (Knasmuller et al. 1998; Castell et al. 2006). Despite the well-known similarities, there are, however, important differences between these two cell lines. First and foremost, HepG2 and Hep3B are from different ethnic origins. They often exhibit different and even opposite outcomes in response to the same pharmacological treatment under the same experimental conditions. These differential outcomes include divergences in chemosensitivity in cytotoxicity, gene expression induction, cell cycle response and biochemical effects. These diverse differences frequently cause difficulties and even confusions for many investigators, especially the beginners who are largely overshadowed by the similarities between these two cell lines in attempts to analyze and interpret their experimental data. To highlight the differences between HepG2 and Hep3B and their underlying mechanism, we searched PubMed for all the available published reports that show differences between HepG2 and Hep3B cell lines. Based on the search results, we summarize the differences between HepG2 and Hep3B in several categories including intrinsic and drug-induced gene expressions, drug-altered cell cycle, cell growth inhibition and the signal pathways that are associated with the differential drug responses described in this review. Furthermore, we analyze the major factors that may be responsible for the differences between HepG2 and Hep3B cell lines. Covering these points, this review offers a relatively comprehensive reference of the often overlooked differences between HepG2 and Hep3B cell lines, and may be of interest to both clinical and basic scientists in liver cancer research and drug development, in particular to those beginners entering these fields.
Differences between HepG2 and Hep3B
Different originations of HepG2 and Hep3B cells
HepG2 and Hep3B were originally established by Aden et al. (1979). They were isolated from liver biopsy specimens of a 15-year-old Caucasian male from Argentina with primary HB, or an 8-year-old black male from the US with primary HCC (Aden et al. 1979; Knowles et al. 1980), respectively. Both cell lines contain distinctive rearrangements of chromosome 1, and other abnormal chromosomes. But they differ in the number of chromosomes per cell as HepG2 cells contain an average of 55 (50–56) chromosomes per cell whereas Hep3B cells, 60. In addition, HepG2 is hepatitis B virus negative and non-tumorigenic, but Hep3B is hepatitis B virus positive and tumorigenic (Knowles et al. 1980; Knasmuller et al. 1998).
Differential gene expression in HepG2 and Hep3B cells
As described previously (Knowles et al. 1980; Knasmuller et al. 1998), HepG2 and Hep3B have been extensively studied for their molecular biology and biochemistry. In recent years, substantial progress has been achieved in producing sufficient data on gene expression in HepG2 and Hep3B cell lines, by using several different assay techniques including PCR (Cheng et al. 2003), Western Blotting (Gangneux et al. 2003; Kusaba et al. 2007; Wu et al. 2010), immunoprecipitation (Bressac et al. 1990), zymography (Kim and Kim 2004), or electrophoretic mobility shift assay (EMSA) (Chiao et al. 2002). Table 1 lists all those genes that have been found to express differently in HepG2 and Hep3B cell lines. Some of these genes are essential components or intermediators of signal pathways. Therefore the disparity of expression level of these genes may be responsible for the different responses to drug treatment between HepG2 and Hep3B cells as discussed below.
Differential drug effects in HepG2 and Hep3B cells
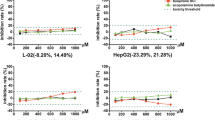
There is a great amount of experimental evidence showing that HepG2 and Hep3B cells respond differently to the same drug treatment. Table 2 shows the drug treatments that give rise to different effects on cell cycle, in terms of the cell cycle arrest at G1 or G2 stages, and apoptosis in both HepG2 and Hep3B cells, and the dependence of the effects on p53 status in HepG2 cells. Table 3 lists the drug treatments that result in different effects of growth suppression on HepG2 and Hep3B cells. Moreover, Table 4 lists drug treatments to which HepG2 and Hep3B cells react with different sensitivities, and Table 5 shows drug treatments that cause some of the genes to alter differently in HepG2 and Hep3B cells. In Table 4, a low value of the half maximal inhibitory concentration (IC50) of a drug indicates a high sensitivity to the drug treatment and vise versa, otherwise there is only a qualitative comparison available from the literature for the sensitivity to the drug treatment (low vs. high).
Differential drug responses of signaling pathways in HepG2 and Hep3B cells
Over the decades, some relevant cellular signaling pathways in the development and maintenance of liver cancer have been deciphered. Among them, the rat sarcoma (RAS)/rat sarcoma-activated factor (RAF)/MAPK-mitogen activated protein kinase, ERK kinase (MEK)/extracellular regulated kinase (ERK) pathway (RAS/RAF/MEK/ERK), the Janus kinase (JAK)/STAT (signal tranducers and activator of transcription) pathway (JAK/STAT), and the Hedgehog (Hh) pathway during hepatocarcinogenesis are the three most well-studied pathways known to respond to drug treatments differently between HepG2 and Hep3B cells (Wiesenauer et al. 2004; Calvisi et al. 2006; Sicklick et al. 2006; Kusaba et al. 2007).
RAS/RAF/MEK/ERK pathway
The RAS/RAF/MEK/ERK pathway is one of the most significant cellular signaling cascades in the development and maintenance of liver cancer. Through a series of specific phosphorylation events, this pathway transduces extracellular signals from ligand-bound tyrosine kinase receptors, such as the epidermal growth factor receptor (EGFR), the insulin-like growth factor receptor (IGFR), the vascular endothelial growth factor receptor (VEGFR) or the platelet-derived growth factor receptor (PDGFR) into cell, starting with the activation of RAS which in turn activates serine threonine kinases of the RAF-family member (Calvisi et al. 2006). Activated RAF phosphorylates MEK kinases, which activate ERK. Once activated, ERK enters nucleus to act as a regulator of gene expression of various proteins for life processes, such as those for cell cycle progression, apoptosis, extracellular matrix remodeling, cellular motility angiogenesis and drug resistance (Wiesenauer et al. 2004). As shown in Table 1, the content of RAS, a major component of the pathway is lower in HepG2 than that in Hep3B, thus inhibitors on this pathway may induce correspondingly different outcomes in these two cell lines (Bose et al. 2011). Indeed, Wiesenauer et al. have shown that the inhibition of ERK phosphorylation and the growth suppression by ERK specific inhibitors PD098059 and U0126 are more profound in HepG2 than in Hep3B (Wiesenauer et al. 2004; Choi et al. 2008). However, the decrease in ERK protein expression by antisense knockdown is more sensitive and the cell growth is inhibited to a greater degree in Hep3B than in HepG2 cells (Wiesenauer et al. 2004). Moreover, treatment with DOX increases the level of active, phosphorylated ERK and causes apoptosis in cell lines. Treating HepG2 cells with a combination of DOX + U0126 effectively suppresses ERK phosphorylation induced by DOX and increases growth inhibition by enhancing apoptosis. In contrast, the same treatment does not enhance apoptosis or the inhibition of cell proliferation in Hep3B cells despite the level of phosphorylated ERK is decreased (Choi et al. 2008). Furthermore, vitamin K2 (VK2) activates ERK phosphorylation and inhibits cell growth in Hep3B but not in HepG2 cells (Matsumoto et al. 2006). Taken together, the differences in response to drug treatments of HepG2 and Hep3B cells may well be attributable to the RAS/RAF/MEK/ERK pathway.
JAK/STAT pathway
JAK/STAT pathway plays an important role in cellular processes like differentiation, proliferation, and apoptosis in liver cancer (Huynh 2010). STATs are latent in the cytoplasm and become activated through tyrosine phosphorylation which typically occurs through JAKs or growth factor receptor tyrosine kinases. Activated STATs translocate into nucleus and serve as transcription factors for multiple downstream target genes. In normal cells, ligand-dependent activation of STATs is transient, but in liver cancer, STAT proteins are often constitutively activated in primary tumors (Calvisi et al. 2006; Kusaba et al. 2007; Mair et al. 2011). This constitutive activation is because of the inactivation of specific STAT inhibitors, SOCSs (suppressors of cytokine signaling) which are inactivated by DNA hypermethylation in liver and other cancers (Yoshikawa et al. 2001; Niwa et al. 2005). Thus, dysfunction of the STAT inhibitors such as cytokine-inducible SH2-protein (CIS), SOCS-1, SOCS-2, SOCS-3, and SHP1 (SH2-containing phosphatases) has been shown to account for the constitutive activation of STAT-3 and -5 in liver cancer. The different levels of SOCS-1 as shown in Table 1, and perhaps other components in the pathway may determine the different chemoresistance of HepG2 and Hep3B to drug treatments. AG490 is a JAK2 specific inhibitor that inhibits the phosphorylation of STAT3 (Fuke et al. 2007; Kusaba et al. 2007). Treatment with AG490 induces cell cycle arrest in HepG2 cells but obvious apoptosis in Hep3B cells (Kusaba et al. 2007). Similarly, SRC (short for sarcoma, a proto-oncogene encoding a tyrosine kinase) family members are also involved in the constitutive activation of STAT3 in various malignances, including liver cancer (Kusaba et al. 2007; Lau et al. 2009). Therefore, treatment with SRC specific inhibitors KX2-391 and Dasatinib causes different responses between HepG2 and Hep3B cells as shown in Table 4 (Lau et al. 2009). Hence, JAK/STAT pathway is also involved in the different response of HepG2 and Hep3B cells to drug treatment.
Hedgehog pathway
The same holds true for the Hh pathway. Hh pathway plays an important role in diverse cellular development processes, including embryonic patterning, cell differentiation and organ morphogenesis (Theunissen and de Sauvage 2009; Ho and Alman 2010). It is frequently activated by mutations of the components in this pathway in multiple cancers, including liver cancer (Chang et al. 2006). Aberrant activation of Hh signaling is associated with cellular growth, survival and adult stem cell maintenance (Ho and Alman 2010). There are three mammalian Hh proteins: Sonic Hedgehog (SHH), Indian Hedgehog (IHH) and Desert Hedgehog (DHH) and three commonly studied downstream targets: PTCH1, SMO and GLI1 (Theunissen and de Sauvage 2009). This pathway is activated when SHH, IHH or DHH binds to their receptor, PTCH1. When unoccupied by ligand (SHH, IHH or DHH), PTCH1 acts as a tumor suppressor by binding to and repressing SMO, which is a proto-oncoprotein to activate transcription factors, such as GLI1 (Theunissen and de Sauvage 2009). Therefore, specific inhibition of the components in Hh pathway might be a therapeutic option for tumor treatment. Indeed, Hep3B cells respond to treatments with SMO antagonists, KAAD-cyclopamines or SHH neutralizing antibodies, which specifically inhibit the Hh signaling pathway, with suppressed cell growth and enhanced apoptosis. In contrast, HepG2 cells are resistant to the same treatments (Chang et al. 2006; Sicklick et al. 2006). Again, the different levels of SHH as shown in Table 1 (Chang et al. 2006; Sicklick et al. 2006) and other components (Huang et al. 2006) in Hh pathway may account for the differential sensitivity to the specific inhibition of Hh pathway between HepG2 and Hep3B cells.
Underlying mechanisms responsible for the differences between HepG2 and Hep3B cells
HBx is associated with but may not be responsible for the majority of genes expressed differently in HepG2 and Hep3B cells
In order to identify determinants of the differences between HepG2 and Hep3B, we first examined the factors that regulate the differentially expressed genes in these two cell lines. As indicated in Table 1, 11 out of the 19 differentially expressed genes are regulated in Hep3B cells by the presence of HBV, especially by the HBV x protein (HBx). HBx is a multifunctional regulator and plays a crucial role in HCC development. Its functions have been comprehensively reviewed in recent review articles (Tsai and Chung 2010; Ng and Lee 2011; Tan 2011) regarding gene transcription modulation, signal transduction pathways, cell cycle progression, cell death, protein degradation and genetic stability. As shown in Table 1 and discussed in the aforementioned reviews, all the three signal pathways known to respond differently to drug treatments as described in the previous section are regulated by HBx (Ng and Lee 2011; Arzumanyan et al. 2012). Hence, HBx is sometimes considered to be a viral oncoprotein (Koike 2009; Neuveut et al. 2010) and could be the chief regulator of the differential gene expression between HepG2 and Hep3B because it regulates the majority of those genes listed in Table 1. In order to determine whether the HBx is really responsible for the differential expression of genes in HepG2 and Hep3B cells, we examined the reported alteration of gene expression in HBx knockdown studies. Surprisingly, we found that none of the genes listed in Table 1 has been reported to be either up- or down-regulated in the human cells (Xie et al. 2011) or in mouse model (Fukuhara et al. 2012) when HBx is knocked down. This finding seems to suggest that the differential expression of genes between HepG2 and Hep3B is not simply dependent on HBx. Moreover, the expression of either TGF-β type I receptor or SOCS-1 has been shown to be independent of HBx (Shih et al. 2000; Bock et al. 2008). Therefore, HBx may not be the critical factor in governing the differential expression between HepG2 and Hep3B cells.
p53 may not be associated with the differences in HepG2 and Hep3B cells
To survey whether other factors are involved in governing the differential expression of genes between HepG2 and Hep3B cells, we focused on the connection of p53 with the expression of these genes because the transcription factor p53 is the most extensively and intensively studied tumor suppressor gene. p53 is activated in response to virtually all stress signals, including drug treatment to induce DNA damage and oncogene activation (Lane et al. 2010). The normal p53 activity is the most frequently altered in tumors (Vazquez et al. 2008; Lane et al. 2010). Furthermore, in the remaining tumors with wild-type p53, it is often inactivated through other mechanisms. Consequently, the almost universal loss of p53 activity in cancers has been spurring enormous efforts to develop p53-targeted cancer therapeutics as well as attempt to connect various experimental observations with p53 (Fuster et al. 2007; Vazquez et al. 2008; Lau et al. 2009). Because HepG2 cells are known to contain wild-type p53 and Hep3B cells are p53 deficient, it is, therefore, natural to ask whether p53 plays a critical role in the observed differences in gene expression and in response to drug treatments between the p53 wild-type containing HepG2 cells and the p53-deficient Hep3B cells. This question can be answered by comparing the drug treatment effects on HepG2 cells after p53 knockdown and/or on Hep3B cells after p53 restoration by over-expression. In p53 knockdown studies using cDNA microarray assays to obtain a global analysis of endogenous p53 target genes, it has been shown that only Fas/Apo-1 and TGFβ type I receptor (Goldstein et al. 2012), cyclin D1 (Lefort et al. 2007), or none (Chau et al. 2009) is responsive to p53 knockdown.
Furthermore, in order to determine whether the differential drug responses between HepG2 and Hep3B cells are dependent on the status of p53 or not, we analyzed the published data of differential responses against drug treatments in HepG2 and Hep3B cells as shown in Table 2. The different effects of drug treatment include cell cycle arrest at G1 or G2 stages, and apoptosis in both HepG2 and Hep3B cells, and the dependence of the effects on p53 status in HepG2 cells. Among the 19 reports available, we found that 17 of them do not give direct evidence of p53 dependence of the differential drug responses in HepG2 and Hep3B cells, the other two reports give direct but contradictory evidence regarding the dependence on p53 of the differential drug responses in HepG2 and Hep3B cells. The inconclusive or even contradictory findings could simply be due to the fact that the p53-dependence has not been well examined by experiments. But it may also be possible or even more likely that the differential drug responses between HepG2 and Hep3B cell are not dependent on p53 status at all, hence, no publishable positive results have been obtained.
Based on the above discussion, we postulate that p53 may not be the most critical factor to contribute to determining the differential gene expression and responses to pharmacological and therapeutic treatment between HepG2 and Hep3B cell lines. Instead, these differences between these two cell lines may well be due to their different origins.
The different origins of biopsy specimens may be responsible for the differences between HepG2 and Hep3B
HepG2 and Hep3B cell lines are derived from different sources of biopsy specimens. HepG2 was isolated from liver biopsy specimens of primary HB, whereas Hep3B was from primary HCC (Aden et al. 1979; Knowles et al. 1980). According to a hierarchical hepatic cellular lineage model for liver cell maturation and liver cancer development, HB is derived from neonatal liver stem cells with more potential and HCC is arisen from more differentiated mature hepatocytes in liver lobule (Sell and Leffert 2008). Hence, HepG2 and Hep3B come from different differentiation stages in liver cell lineage, which may well explain the differences between them.
Furthermore, a recent comprehensive proteome profiling study (Slany et al. 2010) has shown that in cytoplasmic proteome, HepG2 retains much more hepatocyte-related features, while Hep3B, more fibroblasts-related features and more mesenchymal proteins indicative for epithelial to mesenchymal transition (EMT). In secretome, HepG2 cells express a proteome profile with a quite considerable number of and amount of plasma proteins characteristic for hepatocytes, and Hep3B cells contain few and relatively small amounts of these proteins. Moreover, Hep3B cells secrete five proteins that are characteristic for mesenchymal cells and may be marker proteins for EMT, notably, the follistatin-related protein 1, which is usually found in mesenchymal cells, such as fibroblasts. Therefore, it has been suggested that HepG2 is closer to hepatocyte, whereas Hep3B to fibroblast (Slany et al. 2010). Apparently, hepatocytes and fibroblasts are developmentally unrelated and differ in various functional and phenotypic characteristics, but are often experimentally exchangeable. Mouse fibroblasts can be induced directly to hepatocyte-like (iHep) cells by over-expression of a Forkhead box A protein (Foxa), either alone or in combination with GATA-binding protein 4 (Gata4) without the need for liver progenitor stage (Huang et al. 2011; Sekiya and Suzuki 2011). However, an intermediate EMT stage is needed to induce fibroblasts from hepatocytes by treatment of TGF-beta in liver fibrosis (Zeisberg et al. 2007). Therefore, it seems that Hep3B cells are hepatocytes with EMT, but HepG2 cells are hepatocytes without EMT. EMT is a rapid and reversible change of phenotype of the cells from polarized and epithelial to fibroblastoid and mesenchymal cells (Saulnier et al. 2010). It has an important role in the development of many tissues during embryogenesis, but can also be recapitulated during pathological progression, such as fibrosis and tumorogenesis, including in HCC. EMT may also occur during the transformation, immortalization or in vitro culture of hepatocytes (Slany et al. 2010). Multiple factors such as miRNAs, epigenetic modifications as well as transcriptional factors have been identified to be involved in EMT (Thiery and Sleeman 2006; De Craene and Berx 2013), and differences of these factors may also account for the differences between HepG2 and Hep3B cell lines.
Implications
As a conventional practice to draw scientifically sound and more generalized conclusions, scientists in cancer research and drug development usually use more than one cell line in their assessments. In liver cancer, HepG2 and Hep3B cell lines sharing similarities represent a mainstay of liver cancer biology. Therefore, they are frequently employed in experimental manipulations, including drug treatment, mechanistic studies, and various high-throughput applications. However, different or inconsistent outcomes, which we summarized in Tables 1, 2, 3, 4 and 5 in this review, have resulted from comparative analyses of these two cell lines. Covering the main differences, this review would be of interest to the community of both clinical and basic scientists in both cancer research and drug development, in particular to those beginners entering these fields.
HBx has been widely recognized to be essential for viral replication and to contribute to hepatocarcinogenesis. It regulates the expression of many genes involved in various life processes, therefore, HBV infection, in particular the expression of HBx has been suggested to contribute to the differential gene expression and hence account for differences in drug responses and signal transduction between HepG2 and Hep3B. Similarly, transcriptional factor p53 plays a critical role in directly or indirectly regulating a large number of target genes in genomic stability, cell cycle, senescence, apoptosis, DNA repair and recombination. Like in many other studies, we attempted to link the differences in other gene expression and drug responses between HepG2 and Hep3B cells to differential expression levels of p53 between the two cell lines. However, based on our analyses, neither HBx nor p53 is found to be the crucial determinant of the differences between HepG2 and Hep3B.
Instead of HBx or p53 alone, multiple factors associated with the phenotypic characteristics of the two cell lines from different origins are more likely to be responsible for the differences between HepG2 and Hep3B cell lines. Phenotypically, HepG2 is more hepatocytic and Hep3B is more fibroblastic with EMT from hepatocytes. According to a hierarchical cell lineage model, HB (HepG2) is derived from neonatal liver stem cells with more potential, and HCC (Hep3B), from more differentiated mature hepatocytes in liver lobule. Therefore, the substantial differences between HepG2 and Hep3B could be accounted for by the differences of the maturation of liver cancer cells and complex process of EMT due to the different origins of biopsy specimens, rather than by a single “master molecule” or “hub molecule”, if it exists.
Conclusions
In conclusion, HepG2 and Hep3B are two liver cancer cell lines with a wide range of differences in ethnic origins, biology, genetics and biochemistry. These differences may lead to differential responses to pharmacological agents in these two cell lines, including different signaling responses to specific inhibitors, varied chemosensitivity to therapeutic drugs, as well as diverse effects on cell cycle progression induced by the different treatments. Based on the evidence available, we propose that the difference in the origins of biopsy specimens and associated multiple factors, rather than a single protein such as HBx or p53, may be the critical contributors to govern these differences between HepG2 and Hep3B cell lines.
References
Aden DP, Fogel A, Plotkin S, Damjanov I, Knowles BB (1979) Controlled synthesis of HBsAg in a differentiated human liver carcinoma-derived cell line. Nature 282:615–616
Arce F, Gatjens-Boniche O, Vargas E, Valverde B, Diaz C (2005) Apoptotic events induced by naturally occurring retinoids ATRA and 13-cis retinoic acid on human hepatoma cell lines Hep3B and HepG2. Cancer Lett 229:271–281
Arima T, Nakao K, Nakata K, Ishikawa H, Ichikawa T, Hamasaki K, Ishii N, Eguchi K (2002) Transactivation of human alpha-fetoprotein gene by X-gene product of hepatitis B virus in human hepatoma cells. Int J Mol Med 9:397–400
Arzumanyan A, Sambandam V, Clayton MM, Choi SS, Xie G, Diehl AM, Yu DY, Feitelson MA (2012) Hedgehog signaling blockade delays hepatocarcinogenesis induced by hepatitis B virus X protein. Cancer Res 72:5912–5920
Benn J, Schneider RJ (1994) Hepatitis B virus HBx protein activates Ras-GTP complex formation and establishes a Ras, Raf, MAP kinase signaling cascade. Proc Natl Acad Sci USA 91:10350–10354
Bock CT, Toan NL, Koeberlein B, le Song H, Chin R, Zentgraf H, Kandolf R, Torresi J (2008) Subcellular mislocalization of mutant hepatitis B X proteins contributes to modulation of STAT/SOCS signaling in hepatocellular carcinoma. Intervirology 51:432–443
Bose S, Sakhuja P, Bezawada L, Agarwal AK, Kazim SN, Khan LA, Sarin SK, Ramakrishna G (2011) Hepatocellular carcinoma with persistent hepatitis B virus infection shows unusual downregulation of Ras expression and differential response to Ras mediated signaling. J Gastroenterol Hepatol 26:135–144
Bressac B, Galvin KM, Liang TJ, Isselbacher KJ, Wands JR, Ozturk M (1990) Abnormal structure and expression of p53 gene in human hepatocellular carcinoma. Proc Natl Acad Sci USA 87:1973–1977
Caja L, Sancho P, Bertran E, Fabregat I (2011) Dissecting the effect of targeting the epidermal growth factor receptor on TGF-beta-induced-apoptosis in human hepatocellular carcinoma cells. J Hepatol 55:351–358
Calvisi DF, Ladu S, Gorden A, Farina M, Conner EA, Lee JS, Factor VM, Thorgeirsson SS (2006) Ubiquitous activation of Ras and Jak/Stat pathways in human HCC. Gastroenterology 130:1117–1128
Carmona-Cuenca I, Roncero C, Sancho P, Caja L, Fausto N, Fernandez M, Fabregat I (2008) Upregulation of the NADPH oxidase NOX4 by TGF-beta in hepatocytes is required for its pro-apoptotic activity. J Hepatol 49:965–976
Castell JV, Jover R, Martinez-Jimenez CP, Gomez-Lechon MJ (2006) Hepatocyte cell lines: their use, scope and limitations in drug metabolism studies. Expert Opin Drug Metab Toxicol 2:183–212
Chang C, Hsu LC, Dave V, Yoshida A (1998) Expression of human aldehyde dehydrogenase-3 associated with hepatocellular carcinoma: promoter regions and nuclear protein factors related to the expression. Int J Mol Med 2:333–338
Chang J, Hsu Y, Kuo P, Kuo Y, Chiang L, Lin C (2005) Increase of Bax/Bcl-XL ratio and arrest of cell cycle by luteolin in immortalized human hepatoma cell line. Life Sci 76:1883–1893
Chang UM, Li CH, Lin LI, Huang CP, Kan LS, Lin SB (2006) Ganoderiol F, a ganoderma triterpene, induces senescence in hepatoma HepG2 cells. Life Sci 79:1129–1139
Chau BN, Diaz RL, Saunders MA, Cheng C, Chang AN, Warrener P, Bradshaw J, Linsley PS, Cleary MA (2009) Identification of SULF2 as a novel transcriptional target of p53 by use of integrated genomic analyses. Cancer Res 69:1368–1374
Cheng AS, Chan HL, Leung WK, Wong N, Johnson PJ, Sung JJ (2003) Specific COX-2 inhibitor, NS-398, suppresses cellular proliferation and induces apoptosis in human hepatocellular carcinoma cells. Int J Oncol 23:113–119
Cheng AS, Chan HL, Leung WK, To KF, Go MY, Chan JY, Liew CT, Sung JJ (2004) Expression of HBx and COX-2 in chronic hepatitis B, cirrhosis and hepatocellular carcinoma: implication of HBx in upregulation of COX-2. Mod Pathol 17:1169–1179
Cheng SB, Wu LC, Hsieh YC, Wu CH, Chan YJ, Chang LH, Chang CM, Hsu SL, Teng CL, Wu CC (2012) Supercritical carbon dioxide extraction of aromatic turmerone from Curcuma longa Linn. induces apoptosis through reactive oxygen species-triggered intrinsic and extrinsic pathways in human hepatocellular carcinoma HepG2 cells. J Agric Food Chem 60:9620–9630
Chi TY, Chen GG, Lai PB (2004) Eicosapentaenoic acid induces Fas-mediated apoptosis through a p53-dependent pathway in hepatoma cells. Cancer J (Sudbury, Mass) 10:190–200
Chiao PJ, Na R, Niu J, Sclabas GM, Dong Q, Curley SA (2002) Role of Rel/NF-kappaB transcription factors in apoptosis of human hepatocellular carcinoma cells. Cancer 95:1696–1705
Choi J, Yip-Schneider M, Albertin F, Wiesenauer C, Wang Y, Schmidt CM (2008) The effect of doxorubicin on MEK-ERK signaling predicts its efficacy in HCC. J Surg Res 150:219–226
Chung TW, Lee YC, Kim CH (2004) Hepatitis B viral HBx induces matrix metalloproteinase-9 gene expression through activation of ERK and PI-3 K/AKT pathways: involvement of invasive potential. FASEB J 18:1123–1125
Cruickshank SM, Southgate J, Selby PJ, Trejdosiewicz LK (1998) Expression and cytokine regulation of immune recognition elements by normal human biliary epithelial and established liver cell lines in vitro. J Hepatol 29:550–558
De Craene B, Berx G (2013) Regulatory networks defining EMT during cancer initiation and progression. Nat Rev Cancer 13:97–110
Doria M, Klein N, Lucito R, Schneider RJ (1995) The hepatitis B virus HBx protein is a dual specificity cytoplasmic activator of Ras and nuclear activator of transcription factors. EMBO J 14:4747–4757
Fuke H, Shiraki K, Sugimoto K, Tanaka J, Beppu T, Yoneda K, Yamamoto N, Ito K, Masuya M, Takei Y (2007) Jak inhibitor induces S phase cell-cycle arrest and augments TRAIL-induced apoptosis in human hepatocellular carcinoma cells. Biochem Biophys Res Commun 363:738–744
Fukuhara Y, Suda T, Kobayashi M, Tamura Y, Igarashi M, Waguri N, Kawai H, Aoyagi Y (2012) Identification of cellular genes showing differential expression associated with hepatitis B virus infection. World J Hepatol 4:139–148
Fuster JJ, Sanz-Gonzalez SM, Moll UM, Andres V (2007) Classic and novel roles of p53: prospects for anticancer therapy. Trends Mol Med 13:192–199
Gangneux C, Daveau M, Hiron M, Derambure C, Papaconstantinou J, Salier JP (2003) The inflammation-induced down-regulation of plasma Fetuin-A (alpha2HS-Glycoprotein) in liver results from the loss of interaction between long C/EBP isoforms at two neighbouring binding sites. Nucleic Acids Res 31:5957–5970
Ganten TM, Haas TL, Sykora J, Stahl H, Sprick MR, Fas SC, Krueger A, Weigand MA, Grosse-Wilde A, Stremmel W, Krammer PH, Walczak H (2004) Enhanced caspase-8 recruitment to and activation at the DISC is critical for sensitisation of human hepatocellular carcinoma cells to TRAIL-induced apoptosis by chemotherapeutic drugs. Cell Death Differ 11:S86–S96
Gao Y, Lin LP, Zhu CH, Chen Y, Hou YT, Ding J (2006) Growth arrest induced by C75, A fatty acid synthase inhibitor, was partially modulated by p38 MAPK but not by p53 in human hepatocellular carcinoma. Cancer Biol Ther 5:978–985
Goldstein I, Ezra O, Rivlin N, Molchadsky A, Madar S, Goldfinger N, Rotter V (2012) p53, a novel regulator of lipid metabolism pathways. J Hepatol 56:656–662
Ho L, Alman B (2010) Protecting the hedgerow: p53 and hedgehog pathway interactions. Cell Cycle (Georgetown, Tex) 9:506–511
Horvath E, Lakatos P, Balla B, Kosa JP, Tobias B, Jozilan H, Borka K, Horvath HC, Kovalszky I, Szalay F (2012) Marked increase of CYP24A1 mRNA level in hepatocellular carcinoma cell lines following vitamin D administration. Anticancer Res 32:4791–4796
Huang S, He J, Zhang X, Bian Y, Yang L, Xie G, Zhang K, Tang W, Stelter AA, Wang Q, Zhang H, Xie J (2006) Activation of the hedgehog pathway in human hepatocellular carcinomas. Carcinogenesis 27:1334–1340
Huang P, He Z, Ji S, Sun H, Xiang D, Liu C, Hu Y, Wang X, Hui L (2011) Induction of functional hepatocyte-like cells from mouse fibroblasts by defined factors. Nature 475:386–389
Huber BE, Wirth PJ, Newbold JE (1991) Effects of human lymphoblastoid interferon on proliferation, gene expression and tumourigenicity of human hepatoma cell lines. Drugs Exp Clin Res 17:281–291
Huynh H (2010) Molecularly targeted therapy in hepatocellular carcinoma. Biochem Pharmacol 80:550–560
Jelkmann WE, Fandrey J, Frede S, Pagel H (1994) Inhibition of erythropoietin production by cytokines. Implications for the anemia involved in inflammatory states. Ann N Y Acad Sci 718:300–309; discussion 309–311
Jung HY, Park SH, Yoo YD, Kim JS, Kim YH (2005) CDK2/4 regulate retinoic acid-induced G1 arrest in hepatocellular carcinoma cells. Hepatol Res 31:143–152
Kim JR, Kim CH (2004) Association of a high activity of matrix metalloproteinase-9 to low levels of tissue inhibitors of metalloproteinase-1 and -3 in human hepatitis B-viral hepatoma cells. Int J Biochem Cell Biol 36:2293–2306
Kim HR, Park HJ, Park JH, Kim SJ, Kim K, Kim J (2004) Characteristics of the killing mechanism of human natural killer cells against hepatocellular carcinoma cell lines HepG2 and Hep3B. Cancer Immunol Immunother (CII) 53:461–470
Klein A, Guhl E, Tzeng YJ, Fuhrhop J, Levrero M, Graessmann M, Graessmann A (2003) HBX causes cyclin D1 overexpression and development of breast cancer in transgenic animals that are heterozygous for p53. Oncogene 22:2910–2919
Knasmuller S, Parzefall W, Sanyal R, Ecker S, Schwab C, Uhl M, Mersch-Sundermann V, Williamson G, Hietsch G, Langer T, Darroudi F, Natarajan AT (1998) Use of metabolically competent human hepatoma cells for the detection of mutagens and antimutagens. Mutat Res 402:185–202
Knowles BB, Howe CC, Aden DP (1980) Human hepatocellular carcinoma cell lines secrete the major plasma proteins and hepatitis B surface antigen. Science (New York, NY) 209:497–499
Kobsel N, Ramadori G (1994) Human hepatoma cells synthesize and secrete lysozyme: modulation by cytokines. Hepatology (Baltimore, Md) 19:1182–1188
Koike K (2009) Hepatitis B virus X gene is implicated in liver carcinogenesis. Cancer Lett 286:60–68
Koike K, Takaki A, Tatsukawa M, Suzuki M, Shiraha H, Iwasaki Y, Sakaguchi K, Shiratori Y (2006) Combination of 5-FU and IFNalpha enhances IFN signaling pathway and caspase-8 activity, resulting in marked apoptosis in hepatoma cell lines. Int J Oncol 29:1253–1261
Krohne TU, Shankara S, Geissler M, Roberts BL, Wands JR, Blum HE, Mohr L (2001) Mechanisms of cell death induced by suicide genes encoding purine nucleoside phosphorylase and thymidine kinase in human hepatocellular carcinoma cells in vitro. Hepatology (Baltimore, Md) 34:511–518
Kuo PL, Lin TC, Lin CC (2002) The antiproliferative activity of aloe-emodin is through p53-dependent and p21-dependent apoptotic pathway in human hepatoma cell lines. Life Sci 71:1879–1892
Kusaba M, Nakao K, Goto T, Nishimura D, Kawashimo H, Shibata H, Motoyoshi Y, Taura N, Ichikawa T, Hamasaki K, Eguchi K (2007) Abrogation of constitutive STAT3 activity sensitizes human hepatoma cells to TRAIL-mediated apoptosis. J Hepatol 47:546–555
Lamboley C, Bringuier AF, Feldmann G (2000) Apoptotic behaviour of hepatic and extra-hepatic tumor cell lines differs after Fas stimulation. Cell Mol Biol (Noisy-le-Grand, France) 46:13–28
Lan YH, Chang FR, Liaw CC, Wu CC, Chiang MY, Wu YC (2005) Digoniodiol, deoxygoniopypyrone A, and goniofupyrone A: three new styryllactones from Goniothalamus amuyon. Planta Med 71:153–159
Lane DP, Cheok CF, Lain S (2010) p53-based cancer therapy. Cold Spring Harb Perspect Biol 2:a001222
Lau GM, Lau GM, Yu GL, Gelman IH, Gutowski A, Hangauer D, Fang JW (2009) Expression of Src and FAK in hepatocellular carcinoma and the effect of Src inhibitors on hepatocellular carcinoma in vitro. Dig Dis Sci 54:1465–1474
Lee TK, Lau TC, Ng IO (2002a) Doxorubicin-induced apoptosis and chemosensitivity in hepatoma cell lines. Cancer Chemother Pharmacol 49:78–86
Lee YS, Jin DQ, Kwon EJ, Park SH, Lee ES, Jeong TC, Nam DH, Huh K, Kim JA (2002b) Asiatic acid, a triterpene, induces apoptosis through intracellular Ca2+ release and enhanced expression of p53 in HepG2 human hepatoma cells. Cancer Lett 186:83–91
Lefort K, Mandinova A, Ostano P, Kolev V, Calpini V, Kolfschoten I, Devgan V, Lieb J, Raffoul W, Hohl D, Neel V, Garlick J, Chiorino G, Dotto GP (2007) Notch1 is a p53 target gene involved in human keratinocyte tumor suppression through negative regulation of ROCK1/2 and MRCKalpha kinases. Genes Dev 21:562–577
Li J, Shen F, Wu D, Wei LX, Wang YZ, Shi LH, Zou Y, Wu MC (2007) Expression level of Bcl-XL critically affects sensitivity of hepatocellular carcinoma cells to LIGHT-enhanced and interferon-gamma-induced apoptosis. Oncol Rep 17:1067–1075
Liang X, Liu Y, Zhang Q, Gao L, Han L, Ma C, Zhang L, Chen YH, Sun W (2007) Hepatitis B virus sensitizes hepatocytes to TRAIL-induced apoptosis through Bax. J Immunol (Baltimore, Md: 1950) 178:503–510
Lin CP, Liu JD, Chow JM, Liu CR, Liu HE (2007) Small-molecule c-Myc inhibitor, 10058-F4, inhibits proliferation, downregulates human telomerase reverse transcriptase and enhances chemosensitivity in human hepatocellular carcinoma cells. Anticancer Drugs 18:161–170
Liu P, Menon K, Alvarez E, Lu K, Teicher BA (2000) Transforming growth factor-beta and response to anticancer therapies in human liver and gastric tumors in vitro and in vivo. Int J Oncol 16:599–610
Mair M, Blaas L, Osterreicher CH, Casanova E, Eferl R (2011) JAK-STAT signaling in hepatic fibrosis. Front Biosci (Landmark edition) 16:2794–2811
Majer BJ, Mersch-Sundermann V, Darroudi F, Laky B, de Wit K, Knasmuller S (2004) Genotoxic effects of dietary and lifestyle related carcinogens in human derived hepatoma (HepG2, Hep3B) cells. Mutat Res 551:153–166
Malgaretti N, Bruno L, Pontoglio M, Candiani G, Meroni G, Ottolenghi S, Taramelli R (1990) Definition of the transcription initiation site of human plasminogen gene in liver and non hepatic cell lines. Biochem Biophys Res Commun 173:1013–1018
Matsumoto K, Okano J, Nagahara T, Murawaki Y (2006) Apoptosis of liver cancer cells by vitamin K2 and enhancement by MEK inhibition. Int J Oncol 29:1501–1508
Miao J, Chen GG, Chun SY, Lai PP (2006) Hepatitis B virus X protein induces apoptosis in hepatoma cells through inhibiting Bcl-xL expression. Cancer Lett 236:115–124
Moehler M, Blechacz B, Weiskopf N, Zeidler M, Stremmel W, Rommelaere J, Galle PR, Cornelis JJ (2001) Effective infection, apoptotic cell killing and gene transfer of human hepatoma cells but not primary hepatocytes by parvovirus H1 and derived vectors. Cancer Gene Ther 8:158–167
Muller M, Strand S, Hug H, Heinemann EM, Walczak H, Hofmann WJ, Stremmel W, Krammer PH, Galle PR (1997) Drug-induced apoptosis in hepatoma cells is mediated by the CD95 (APO-1/Fas) receptor/ligand system and involves activation of wild-type p53. J Clin Investig 99:403–413
Murata M, Matsuzaki K, Yoshida K, Sekimoto G, Tahashi Y, Mori S, Uemura Y, Sakaida N, Fujisawa J, Seki T, Kobayashi K, Yokote K, Koike K, Okazaki K (2009) Hepatitis B virus X protein shifts human hepatic transforming growth factor (TGF)-beta signaling from tumor suppression to oncogenesis in early chronic hepatitis B. Hepatology (Baltimore, Md) 49:1203–1217
Neuveut C, Wei Y, Buendia MA (2010) Mechanisms of HBV-related hepatocarcinogenesis. J Hepatol 52:594–604
Ng SA, Lee C (2011) Hepatitis B virus X gene and hepatocarcinogenesis. J Gastroenterol 46:974–990
Nishikawa Y, Wang Z, Kerns J, Wilcox CS, Carr BI (1999) Inhibition of hepatoma cell growth in vitro by arylating and non-arylating K vitamin analogs. Significance of protein tyrosine phosphatase inhibition. J Biol Chem 274:34803–34810
Niwa Y, Kanda H, Shikauchi Y, Saiura A, Matsubara K, Kitagawa T, Yamamoto J, Kubo T, Yoshikawa H (2005) Methylation silencing of SOCS-3 promotes cell growth and migration by enhancing JAK/STAT and FAK signalings in human hepatocellular carcinoma. Oncogene 24:6406–6417
Oliviero S, Morrone G, Cortese R (1987) The human haptoglobin gene: transcriptional regulation during development and acute phase induction. EMBO J 6:1905–1912
Park SG, Chung C, Kang H, Kim JY, Jung G (2006) Up-regulation of cyclin D1 by HBx is mediated by NF-kappaB2/BCL3 complex through kappaB site of cyclin D1 promoter. J Biol Chem 281:31770–31777
Qin LF, Ng IO (2002) Induction of apoptosis by cisplatin and its effect on cell cycle-related proteins and cell cycle changes in hepatoma cells. Cancer Lett 175:27–38
Richards CD, Brown TJ, Shoyab M, Baumann H, Gauldie J (1992) Recombinant oncostatin M stimulates the production of acute phase proteins in HepG2 cells and rat primary hepatocytes in vitro. J Immunol (Baltimore, Md: 1950) 148:1731–1736
Saulnier N, Piscaglia AC, Puglisi MA, Barba M, Arena V, Pani G, Alfieri S, Gasbarrini A (2010) Molecular mechanisms underlying human adipose tissue-derived stromal cells differentiation into a hepatocyte-like phenotype. Dig Liver Dis 42:895–901
Sekiya S, Suzuki A (2011) Direct conversion of mouse fibroblasts to hepatocyte-like cells by defined factors. Nature 475:390–393
Sell S, Leffert HL (2008) Liver cancer stem cells. J Clin Oncol 26:2800–2805
Shih WL, Kuo ML, Chuang SE, Cheng AL, Doong SL (2000) Hepatitis B virus X protein inhibits transforming growth factor-beta-induced apoptosis through the activation of phosphatidylinositol 3-kinase pathway. J Biol Chem 275:25858–25864
Shin EC, Shin JS, Park JH, Kim H, Kim SJ (1999) Expression of fas ligand in human hepatoma cell lines: role of hepatitis-B virus X (HBX) in induction of Fas ligand. Int J Cancer 82:587–591
Sicklick JK, Li YX, Jayaraman A, Kannangai R, Qi Y, Vivekanandan P, Ludlow JW, Owzar K, Chen W, Torbenson MS, Diehl AM (2006) Dysregulation of the Hedgehog pathway in human hepatocarcinogenesis. Carcinogenesis 27:748–757
Slany A, Haudek VJ, Zwickl H, Gundacker NC, Grusch M, Weiss TS, Seir K, Rodgarkia-Dara C, Hellerbrand C, Gerner C (2010) Cell characterization by proteome profiling applied to primary hepatocytes and hepatocyte cell lines Hep-G2 and Hep-3B. J Proteome Res 9:6–21
Su F, Schneider RJ (1996) Hepatitis B virus HBx protein activates transcription factor NF-kappaB by acting on multiple cytoplasmic inhibitors of rel-related proteins. J Virol 70:4558–4566
Tan YJ (2011) Hepatitis B virus infection and the risk of hepatocellular carcinoma. World J Gastroenterol (WJG) 17:4853–4857
Theunissen JW, de Sauvage FJ (2009) Paracrine Hedgehog signaling in cancer. Cancer Res 69:6007–6010
Thiery JP, Sleeman JP (2006) Complex networks orchestrate epithelial-mesenchymal transitions. Nat Rev Mol Cell Biol 7:131–142
Thongtan T, Panyim S, Smith DR (2004) Apoptosis in dengue virus infected liver cell lines HepG2 and Hep3B. J Med Virol 72:436–444
Tsai WL, Chung RT (2010) Viral hepatocarcinogenesis. Oncogene 29:2309–2324
Varghese L, Agarwal C, Tyagi A, Singh RP, Agarwal R (2005) Silibinin efficacy against human hepatocellular carcinoma. Clin Cancer Res 11:8441–8448
Vazquez A, Bond EE, Levine AJ, Bond GL (2008) The genetics of the p53 pathway, apoptosis and cancer therapy. Nat Rev Drug Discov 7:979–987
Wenger RH, Marti HH, Bauer C, Gassmann M (1998) Optimal erythropoietin expression in human hepatoma cell lines requires activation of multiple signalling pathways. Int J Mol Med 2:317–324
Wiesenauer CA, Yip-Schneider MT, Wang Y, Schmidt CM (2004) Multiple anticancer effects of blocking MEK-ERK signaling in hepatocellular carcinoma. J Am Coll Surg 198:410–421
Wilson GM, Roberts EA, Deeley RG (1997) Modulation of LDL receptor mRNA stability by phorbol esters in human liver cell culture models. J Lipid Res 38:437–446
Wu JM, Xu Y, Skill NJ, Sheng H, Zhao Z, Yu M, Saxena R, Maluccio MA (2010) Autotaxin expression and its connection with the TNF-alpha-NF-kappaB axis in human hepatocellular carcinoma. Mol Cancer 9:71
Xie HY, Cheng J, Xing CY, Wang JJ, Su R, Wei XY, Zhou L, Zheng SS (2011) Evaluation of hepatitis B viral replication and proteomic analysis of HepG2.2.15 cell line after knockdown of HBx. Hepatobiliary Pancreat Dis Int (HBPD INT) 10:295–302
Yoshikawa H, Matsubara K, Qian GS, Jackson P, Groopman JD, Manning JE, Harris CC, Herman JG (2001) SOCS-1, a negative regulator of the JAK/STAT pathway, is silenced by methylation in human hepatocellular carcinoma and shows growth-suppression activity. Nat Genet 28:29–35
Yu FL, Liao MH, Lee JW, Shih WL (2004) Induction of hepatoma cells migration by phosphoglucose isomerase/autocrine motility factor through the upregulation of matrix metalloproteinase-3. Biochem Biophys Res Commun 314:76–82
Zeisberg M, Yang C, Martino M, Duncan MB, Rieder F, Tanjore H, Kalluri R (2007) Fibroblasts derive from hepatocytes in liver fibrosis via epithelial to mesenchymal transition. J Biol Chem 282:23337–23347
Acknowledgment
This work is supported by Changzhou University Startup Grant (ZMF13020053).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Qiu, GH., Xie, X., Xu, F. et al. Distinctive pharmacological differences between liver cancer cell lines HepG2 and Hep3B. Cytotechnology 67, 1–12 (2015). https://doi.org/10.1007/s10616-014-9761-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10616-014-9761-9