Abstract
Despite research suggesting that rumination may function as a cognitive avoidance strategy, few studies have examined the presence of rumination or its relationship with other cognitive avoidance strategies (e.g., thought suppression) in individuals with comorbid posttraumatic stress disorder (PTSD) and depression. In the current study, 80 veterans with unipolar depression were categorized into two groups: those with and without a comorbid PTSD diagnosis (PTSD+ and PTSD− groups, respectively). Participants completed a clinician-administered diagnostic interview and measures of clinical symptoms, rumination (brooding, reflection, depressive rumination), and thought suppression. No group differences emerged for the measures of rumination, though the PTSD+ group did report greater use of thought suppression. Diagnostic status moderated the associations between thought suppression and brooding and reflection. Specifically, thought suppression was significantly associated with brooding and reflection for individuals with comorbid depression and PTSD, but not for those with depression alone. Though the presence of rumination did not differ between the two groups, results suggest that the function of rumination may differ across depressed individuals with comorbid PTSD compared to those with depression alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posttraumatic stress and depressive disorders frequently co-occur, with a high lifetime risk of comorbidity (e.g., 50%; for a review see Flory and Yehuda 2015); additionally, they share considerable symptom overlap (e.g., anhedonia, self-blame, excessive guilt; APA 2013). Furthermore, individuals with comorbid depression and posttraumatic stress disorder (PTSD) have demonstrated higher symptom severity and greater functional impact (Campbell et al. 2007). Research has demonstrated that certain risk factors may increase vulnerability for the development of both PTSD and major depression (e.g., history of previous depressive episodes, traumatic stress severity, gender; Breslau et al. 1997; O’Donnell et al. 2004). Additional research suggests that transdiagnostic cognitive and emotional vulnerabilities may also help explain this comorbidity, such that these vulnerabilities may both predispose an individual to develop psychopathology and/or contribute to maintaining symptoms once they occur (Ehring and Watkins 2008). For example, individuals who frequently engage in cognitive avoidance strategies (i.e., strategies that allow the person to avoid other distressing thoughts or images) may be at increased risk for both PTSD and depression (Spinhoven et al. 2014, 2015). Rumination has been conceptualized as a form of cognitive avoidance, and empirical research has implicated it in the onset and maintenance of both depression and PTSD (e.g., Nolen-Hoeksema et al. 2008; Szabo et al. 2017). However, the majority of these studies have typically not considered issues of depression/PTSD comorbidity. Thus, it is unclear whether a diagnosis of comorbid PTSD is associated with differential use or function of rumination among individuals with depression.
Rumination is a well-studied cognitive style characterized by repetitive, focused attention on one’s symptoms and their repercussions (Nolen-Hoeksema 1991). Factor analytic studies have identified several ruminative processes, which may be differentiated from each other based on the content of the ruminative thoughts. Specifically, ruminative thoughts can focus on: self-criticism and/or social comparison (brooding), passive problem-solving (reflection), and/ or specific symptoms or experiences (e.g., depressive rumination; Treynor et al. 2003). All three of these ruminative processes have been linked with the onset and maintenance of posttraumatic stress and/or depressive disorders (Giorgio et al. 2010; Marroquin et al. 2010; Surrence et al. 2009). Whereas brooding and symptom-specific rumination are consistently linked with more severe PTSD and depression symptoms (e.g., Birrer and Michael 2011; Treynor et al. 2003), research on reflection is more mixed (Arditte and Joormann 2011; Surrence et al. 2009). Specifically, some studies have found that reflection may help to resolve depression over time (e.g., Arditte and Joormann 2011).
Rumination is posited to serve several functions in the context of psychopathology (for a review, see Watkins 2016). These functions include avoidance of failure experiences (e.g., thinking about past mistakes may help the individual to prevent future mistakes), self-motivation (e.g., an internal voice telling the individual that s/he isn’t good enough and must try harder), anticipating and preparing for potential criticism from others (e.g., reflecting on how an individual’s actions may influence others’ behavior and how to alter one’s own behavior so as to avoid criticism or negative responses), and avoidance of becoming an “unwanted self” (e.g., thinking about times when one behaved in a way that is inconsistent with values and serving as a reminder to “be better” in the future). Similarly, rumination may be used to characterize events as uncontrollable, which in turn justifies behavioral withdrawal and inactivity and discourages problem-solving (Nolen-Hoeksema et al. 2008). According to Nolen-Hoeksema et al. (2008), rumination negatively reinforces inactivity by preoccupying time and reducing exposure to potentially stressful and uncontrollable situations.
An additional potential function of rumination in depression is avoidance or suppression of other negative thoughts and emotions (Cribb et al. 2006; Garnefski and Kraaij 2007; Liverant et al. 2011). Similar to the avoidance theory of worry (a form of verbal processing), researchers have hypothesized that individuals engage in rumination, another form of verbal processing, because it is less acutely distressing than other more experiential forms of emotional processing (e.g., visual; Butler et al. 1995; Moulds et al. 2007; Stroebe et al. 2007). Depressed individuals may use verbal processing to dampen the intensity of sadness or other emotional responses that occur in reaction to distressing thoughts and memories (e.g., Kuo et al. 2012; Watkins and Moulds 2007). Similarly, in the context of PTSD, rumination may be used to temporarily avoid trauma-related thoughts and memories (Ehlers and Clark 2000; Ehring et al. 2008, 2009).
If rumination is used to avoid negative emotions associated with distressing thoughts and memories, we may expect to see associations with other frequently used forms of cognitive avoidance, such as thought suppression (Wegner 1989). Indeed, some research has demonstrated an association between rumination and thought suppression in depressed individuals (Watkins and Moulds 2009). Research has suggested that brooding in particular may be associated with both behavioral and cognitive avoidance (Moulds et al. 2007), including thought suppression (Schoofs et al. 2010). In contrast, research is mixed regarding the association between reflection and cognitive avoidance. For example, in nonclinical samples, reflection has not been associated with a general measure of cognitive avoidance (Moulds et al. 2007), but has been associated with thought suppression (Schoofs et al. 2010). In a sample of current-, remitted-, and never-depressed individuals, Watkins and Moulds (2009) found a significant positive association between reflection and thought suppression. However, research on this relationship among clinically depressed individuals is limited. Furthermore, the use of different types of rumination and associations with thought suppression in the context of PTSD remains unclear.
Critically, PTSD is characterized by high levels of avoidance, and avoidance of both external (e.g., conversations, situations) and internal (e.g., emotions, thoughts) trauma cues is a hallmark feature of the disorder (APA 2013). Studies with survivors of multiple types of traumatic experiences have found that these individuals demonstrate increased use of thought suppression, as well as a strong association between thought suppression and PTSD symptoms (Ehring et al. 2008; Pietrzak et al. 2011; Shipherd and Beck 2005); a recent meta-analysis has also supported this finding (Seligowski et al. 2015). Given this, we may expect that associations between rumination and thought suppression will be particularly strong among individuals with comorbid PTSD, where the desire to avoid thinking about or encountering reminders of traumatic experiences and memories is strong and rumination is likely to serve a cognitive avoidance function.
Much of the theory and research behind rumination as a potential cognitive avoidance strategy has been developed in the context of depression without considering PTSD comorbidity. Additionally, while separate literatures have examined rumination and thought suppression in clinical samples, most studies examining the relationship between these two strategies have utilized non-clinical samples (e.g., Moulds et al. 2007; Schoofs et al. 2010). Understanding how other cognitive strategies (e.g., thought suppression) are associated with use of rumination can augment our conceptualization of the function of rumination across disorders and improve theoretical models of PTSD and PTSD/depression comorbidity. This may ultimately inform treatment approaches for attenuating rumination in this population. Thus, it is important to examine the differential associations between rumination and thought suppression in clinically depressed individuals with and without comorbid PTSD. This study examined the habitual use of rumination and thought suppression, as well as the association between these strategies, in a depressed veteran sample with (PTSD+) and without (PTSD−) comorbid PTSD. Specifically, we sought to examine this association when considering different types of rumination (brooding, reflection, and depressive rumination), given that research is limited/mixed regarding use of brooding and reflection in PTSD. In particular, we examined whether rumination was differentially associated with thought suppression as a function of diagnosis. Study hypotheses were as follows:
-
1.
Because research has demonstrated an association between rumination and symptom severity (Nolen-Hoeksema and Morrow 1991), and because we expected the PTSD+ group to endorse more severe depression and PTSD symptoms, we hypothesized that individuals in the PTSD+ group would report more frequent use of brooding, reflection, and depressive rumination compared with the PTSD− group.
-
2.
Because PTSD is characterized by high levels of avoidance (APA 2013), we hypothesized that individuals in the PTSD+ group would report more frequent use of thought suppression compared with the PTSD− group.
-
3.
Finally, because PTSD is characterized by high levels of avoidance, we also hypothesized that the associations between the subtypes of rumination and thought suppression would be stronger among individuals in the PTSD+ vs. the PTSD− group.
Methods
Participants
The study sample comprised 80 veterans. Participants were recruited via posted flyers and clinician referral in a large VA medical center in the Northeastern United States. The average age of participants was 51.18 years (SD = 11.19) and the sample was majority male (87.5%). The average years of education completed by participants was 13.70 (SD = 1.87). The sample primarily self-identified as White (78.8%), with fewer participants identifying themselves as Black or African American (12.5%), Hispanic or Latino (3.8%), Asian or Asian American (2.5%), or multiracial (2.5%).
Depression and PTSD diagnoses were made using a structured, clinician-administered interview. The PTSD+ and PTSD− groups did not differ significantly in terms of most demographic characteristics including gender (p = .53), race/ethnicity (p = .33), and marital status (p = .60). There was a trend towards significance for group differences in years of education (p = .054). The PTSD+ group was significantly younger than the PTSD− group. The mean age in the PTSD+ group was 48.37 years (SD = 11.02) vs. 54.43 years (SD = 10.63; t(78) = 2.49, p = .02) in the PTSD− group.
Study inclusion criteria included: (a) being over the age of 18; (b) the ability to read and write in English; and (c) a current diagnosis of DSM-IV major depressive disorder (93.8% of sample) and/or dysthymia (11.3% of sample). Exclusion criteria included (a) diagnosis of bipolar disorder or (b) psychotic-spectrum disorder; (c) current suicidal or homicidal intent and/or plan; (d) unstable and severe psychiatric symptoms (e.g. psychiatric hospitalization within the last 2 months); and/or (e) inability to provide informed, written consent.
Diagnostic Interview
Structured Clinical Interview—Patient Edition for DSM-IV (SCID-I/P; First et al. 2002). The SCID is a semi-structured clinical interview that was used to assess current and lifetime DSM-IV Axis I diagnoses. The SCID was used to determine diagnoses of depressive disorders and PTSD as well as exclusionary diagnoses. SCID interviews were conducted by a doctoral-level clinician to determine study diagnostic eligibility. Research supports the reliability of the SCID for assigning DSM diagnoses (Skre et al. 1991; Zanarini and Frankenburg 2001).
Self-Report Measures
Beck Depression Inventory, Second Edition (BDI-II; Beck et al. 1996) is a 21-item inventory that assesses depressive symptom severity over the past 2 weeks. Items are rated on a 4-point Likert scale ranging from 0 to 3. Summary scores range from 0 to 63, with higher scores indicating greater depression severity. The BDI-II has demonstrated high internal consistency, validity, and good test–retest reliability (Beck et al. 1996; Dozois et al. 1998).
PTSD Checklist—Civilian Version (PCL-C; Weathers et al. 1994) is used to measure severity of PTSD symptomatology in a civilian population. The measure consists of 17 Likert items that correspond to DSM-IV PTSD symptoms. Respondents rated the degree to which they were bothered by symptoms in the past month from 1 (not at all) to 5 (extremely). Scores range from 17 to 85, with higher scores indicating greater PTSD symptom severity. The PCL-C has demonstrated acceptable test–retest reliability and good internal consistency (Wilkins et al. 2011). A total symptom severity score was calculated in addition to PCL-C subscale scores that correspond to the four PTSD symptom clusters: re-experiencing, hyperarousal, avoidance, and emotional numbing (Flack et al. 2000).
Mood and Anxiety Symptom Questionnaire—Anhedonia Subscale (MASQ-AD; Watson et al. 1995). The MASQ-AD subscale was used to assess anhedonia. This subscale consists of 22 items developed to assess reduced positive affect and loss of interest. Items are rated on a scale from 1 to 5 and scores for the MASQ-AD range from 22 to 110, with higher scores indexing greater anhedonia levels. The MASQ-AD subscale has demonstrated good reliability and validity (Watson et al. 1995).
Ruminative Response Scale (RRS; Nolen-Hoeksema and Morrow 1991) is a 22-item subscale of the Response Styles Questionnaire. The RRS assesses the tendency to ruminate in response to depressed mood. Items focus on the meaning of rumination, feelings related to depressed mood, as well as symptoms, consequences, and causes of depressed mood. Items are rated on a four-point Likert scale ranging from 1 to 4. The measure consists of three subscales: brooding, reflection, and depressive rumination. The brooding subscale consists of 5 items and measures the tendency to engage in thinking focused on passive comparison of one’s current situation with perceived standards. Scores on this subscale range from 5 to 20, with higher scores indicating higher use of brooding. The reflection subscale consists of 5 items and measures levels of self-reflective thinking and internal cognitive problem solving. Scores on this subscale range from 5 to 20, with higher scores indicating higher use of reflection. The 12-item depressive rumination subscale assesses the tendency to engage in rumination specifically related to the symptoms of depression (inclusion of subscale items derived from Treynor et al. 2003). Scores on this subscale range from 12 to 48, with higher scores indicating higher use of depressive rumination. All subscales have demonstrated adequate to good internal consistency and validity and moderate test–retest reliability (Bagby et al. 2004; Nolen-Hoeksema and Morrow 1991; Treynor et al. 2003).
White Bear Suppression Inventory (WBSI; Wegner and Zanakos 1994). The WBSI is a 15-item measure developed to assess the trait-level tendency to suppress or avoid unpleasant thoughts. Items are rated on a 5-point Likert scale ranging from 1 to 5. Scores range from 15 to 75, with higher scores indicating greater use of thought suppression. The WBSI has demonstrated adequate test–retest reliability, internal consistency, and convergent validity (Wegner and Zanakos 1994).
Study Procedure
All study procedures were performed in compliance with the local institutional review board. This was followed by completion of the SCID to assess study eligibility. Participants then completed a packet of self-report questionnaires assessing clinical symptoms, rumination, and thought suppression.
Data Analytic Plan
Data were screened for skewness, kurtosis, and the presence of univariate outliers (scores ≥ 3 SD above or below the mean) prior to analyses. Data were found to be normally distributed and no outliers were identified. Four participants had missing PCL-C data and were excluded from the analyses involving the PCL-C.
Analyses were performed using SPSS statistical software version 20.0 (SPSS Inc., Chicago, IL, USA). Due to the significant difference in age between the PTSD+ and PTSD− groups, all analyses examining diagnostic group differences controlled for age as a covariate. Univariate Analyses of Variance (ANOVAs) were used to examine differences between diagnostic groups with regards to self-reported symptom severity and cognitive styles. Pearson’s correlation coefficients were computed to examine the relationship between rumination (RRS) and thought suppression (WBSI) across the sample. Hierarchical linear regression analyses were performed to examine diagnosis as a moderator of the relationship between thought suppression and rumination. Rumination was included as the outcome of interest, while diagnoses and thought suppression were included as predictors. Moderation analyses were computed following the approach outlined by Holmbeck (2002). Prior to computing the interaction terms and running the regression equation, diagnosis was coded dichotomously (0 = PTSD−, 1 = PTSD+). Age and thought suppression, continuous variables, were centered to reduce potential multicollinearity. Hierarchical regression analyses were run separately using each of the three RRS subscales (brooding, reflection, and depressive rumination) as dependent variables.
The covariate (age) was entered in the first step. The predictor (thought suppression) and moderator (diagnosis) were entered in the second step, followed by the interaction of thought suppression and diagnosis in the third step. Following Holmbeck’s (2002) method for probing moderation, a second regression equation was computed. This regression equation was identical to the first regression; however, diagnosis was recoded (− 1 = PTSD−, 0 = PTSD+). The recoded diagnosis variable was used to compute a new thought suppression × diagnosis interaction term and as a main effect in this second regression equation. These two regression equations allowed for the computation of the conditional effects of thought suppression on rumination for individuals with and without PTSD separately.
Results
Clinical Symptoms
Mean BDI-II scores indicated a high level of clinical depression (M = 30.04, SD = 9.43) and mean PCL-C scores indicated a high level of PTSD symptoms (M = 53.28, SD = 12.02) across the sample. As expected given diagnostic differences between the groups, participants in the PTSD+ group endorsed significantly higher levels of specific PTSD symptoms as compared to the PTSD− group. For the individual PTSD symptom clusters, individuals with a PTSD diagnosis reported more re-experiencing and hyperarousal symptoms compared to individuals without a PTSD diagnosis. However, there were no significant differences between the groups with regards to avoidance or emotional numbing symptoms. The groups also did not differ with regard to depression symptom severity or levels of anhedonia (see Table 1).
Cognitive Styles
Participants in the PTSD+ and PTSD− groups did not differ with regard to reported use of rumination across the brooding, reflection, and depression rumination subscales of the RRS (Table 1). In contrast, there were group differences with regard to the use of thought suppression. Specifically, the PTSD+ group had higher scores on the WBSI (Table 1). Thought suppression was significantly correlated with brooding (r = .42, p < .001), reflection (r = .23, p = .04), and depressive rumination (r = .33, p = .003) across the sample.
Moderation Analyses
Brooding
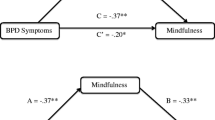
In the hierarchical regression model predicting brooding, Step 1 was not significant, F(1, 78) = 1.76, p = .19, R2 = .02. In Step 1, age (β = − 0.05, t = − 1.33, p = .19) was not significantly associated with brooding. Step 2 was significant, F(3, 76) = 5.76, p = .001, R2 = .19; ∆R2 = .16, p = .001. In Step 2, PTSD diagnosis was not significantly associated with brooding (β = 0.06, t = 0.08, p = .94), while thought suppression was significantly associated (β = 0.11, t = 3.69, p < .001). Step 3 was also significant, F(4, 75) = 5.75, p < .001, R2 = .24; ∆R2 = .05, p = .03. The interaction effect was significant, suggesting that diagnostic group moderated the relationship between thought suppression and brooding (β = 0.13, t = 2.20, p = .03). As depicted in Fig. 1, there was a significant positive association between thought suppression and brooding for the PTSD+ group (β = 0.18, p < .001), while this association was not significant for the PTSD− group (β = 0.05, p = .16).
Regression lines for the associations between thought suppression and rumination (brooding, reflection, and depressive rumination) as moderated by diagnosis and controlling for age. Regression lines indicate variability in rumination at 1 standard deviation (SD) above and below the mean level of thought suppression for the PTSD+ and the PTSD− groups. PTSD+ n = 43, PTSD− n = 37; RRS Ruminative Response Scale, WBSI White Bear Suppression Inventory. *p < .01, **p < .001
Reflection
In the hierarchical regression model predicting reflection, Step 1 was not significant F(1, 78) = 1.30, p = .26, R2 = .02. In Step 1, age (β = − 0.04, t = − 1.14, p = .26) was not significantly associated with reflection. Step 2 was also not significant, F(3, 76) = 1.74, p = .17. R2 = .06; ∆R2 = .05, p = .15. Step 3 was significant, F(4, 75) = 3.06, p = .02, R2 = .14; ∆R2 = .08, p = .01. As with brooding, the significant interaction effect suggested that diagnostic group moderated the relationship between thought suppression and reflection (β = 0.16, t = 2.57, p = .01). As depicted in Fig. 1, there was a significant positive association between thought suppression and reflection in the PTSD+ group (β = 0.16, p = .002), but not in the PTSD− group (β = − 0.006, p = .88).
Depressive Rumination
In the hierarchical regression model predicting depressive rumination, Step 1 was not significant F(1, 78) = 0.01, p = .92, R2 = .000. In Step 1, age (β = − 0.007, t = − 0.10, p = .92) was not significantly associated with depressive rumination. Step 2 was significant, F(3, 76) = 3.21, p = .03, R2 = .11; ∆R2 = .11, p = .01. In Step 2, PTSD diagnosis was not significantly associated with depressive rumination (β = 0.99, t = 0.64, p = .52), while thought suppression was significantly associated (β = 0.16, t = 2.69, p = .009). Step 3 was also significant, F(4, 75) = 2.80, p = .03, R2 = .13; ∆R2 = .02, p = .22. The interaction effect was not significant (β = 0.15, t = 1.23, p = .23), suggesting that the association between thought suppression and depressive rumination did not differ significantly between individuals in the PTSD+ (β = 0.25, p = .009) and PTSD− (β = 0.10, p = .22) groups (see Fig. 1).
Discussion
This study examined the presence of and associations between rumination and thought suppression among clinically depressed veterans with and without PTSD. Results indicated that there were no group differences in rumination, suggesting that both groups utilized rumination with similar frequency. This was true for various forms of rumination, including brooding, reflection, and depressive rumination. This finding supports research indicating that PTSD and depressive disorders are each characterized by frequent utilization of rumination (Ehring et al. 2008). However, our results suggest that a diagnosis of comorbid PTSD with depression is not associated with increased frequency of rumination use, and supports the conceptualization of rumination as a transdiagnostic cognitive vulnerability factor present in multiple disorders.
In contrast to the findings for rumination, individuals with comorbid depression and PTSD (PTSD+ group) engaged in more frequent thought suppression compared to depressed individuals without PTSD (PTSD− group). This suggests that the presence of comorbid PTSD is associated with greater reliance on this cognitive avoidance strategy compared to depression alone. These findings are consistent with previous research, which highlights thought suppression as a frequently used maladaptive cognitive avoidance strategy in PTSD (Seligowski et al. 2015). Notably, groups did not differ with regards to depression symptom severity or anhedonia, which suggests that these findings were not driven by greater depression symptom severity in the PTSD+ group.
Importantly, we found that a diagnosis of comorbid PTSD moderated the association between thought suppression and both brooding and reflection, but not depressive rumination. The moderation analyses revealed that thought suppression was significantly associated with brooding and reflection only among depressed individuals with comorbid PTSD. However, although the association between thought suppression and depressive rumination was significant across all participants, the magnitude of the association between thought suppression and depressive rumination did not differ for depressed individuals with PTSD vs. depressed individuals without PTSD. This suggests that the relationship between thought suppression and rumination may differ depending on both an individual’s diagnoses, as well as the content and focus of their ruminative thoughts. Thus, identifying the content of ruminative thoughts may be important to accurately characterize the nature of associations between rumination and other maladaptive cognitive avoidance strategies, particularly given that different disorders may be associated with different ruminative content (e.g., depressive rumination in unipolar depression vs. trauma-related rumination in PTSD; Ehring et al. 2008; Michael et al. 2007).
One possible interpretation of the moderation results is that the function of rumination differs among depressed individuals with comorbid PTSD compared to individuals with depression alone. Specifically, among depressed individuals with comorbid PTSD, brooding and reflection may function as cognitive avoidance strategies, hence their significant associations with thought suppression. This is consistent with research and theory which suggests that engaging in thought suppression, including suppression of intrusive trauma memories, may lead to a paradoxical increase in these thoughts and memories (Abramowitz et al. 2001; Harvey and Bryant 1998; Shipherd and Beck 1999). The increased availability of negative thoughts may, in turn, trigger a ruminative process (Gold and Wegner 1995; Watkins and Moulds 2009; Wenzlaff and Luxton 2003). Within the context of PTSD, ruminating on aversive traumatic content may activate intrusive images and memories (e.g., Birrer et al. 2007), which may then lead individuals with PTSD to increase efforts to suppress thoughts. In this way, the observed association between rumination and thought suppression among individuals with PTSD could reflect the presence of a vicious cycle in which attempts to avoid distressing cognitions through rumination and thought suppression exacerbate and maintain symptoms. However, it is important to note that the cross-sectional design of our study prevents empirical evaluation of this potential interpretation of study findings. In particular, causal relationships cannot be determined, and future experimental and longitudinal studies are needed to test this hypothesis.
Interestingly, the moderation analyses indicated non-significant associations between thought suppression and both brooding and reflection in the PTSD− group, despite research suggesting a link between thought control strategies, including thought suppression, and rumination in depression (e.g., Watkins and Moulds 2009). One possible explanation is that brooding and reflection serve other functions among veterans with clinical depression. The literature on the possible functions of rumination in depression (e.g., seeking insight, self-motivation, planning, justifying inaction, or problem-solving) suggests that rumination may serve multiple functions for one individual, and many of these functions are not necessarily independent (Watkins 2016). Additional research is needed to directly examine multiple functions of rumination among individuals with depression, PTSD, and comorbid depression/PTSD to further delineate diagnostic group differences.
Despite some literature indicating that reflection can be used adaptively (e.g., Arditte and Joormann 2011), findings have been mixed, with other studies demonstrating associations between reflection and increased depressive symptom severity (e.g., Surrence et al. 2009). Our results indicate that greater use of reflection was associated with greater use of thought suppression among the PTSD+ group. The passive problem-solving that is characteristic of reflection may, therefore, be associated with use of other maladaptive cognitive strategies when an individual has comorbid PTSD. Differentially, the association between reflection and thought suppression in the PTSD− group was not significant. Though outside the scope of the current study, it would be interesting to examine if reflection may be used more adaptively in the context of depression alone.
Study findings should be interpreted in the context of several limitations. First, the sample only included depressed individuals with and without PTSD and did not include a non-depressed group with PTSD or a healthy control group. However, this limitation was mitigated by our ability to compare two groups with similar levels of depression, thus allowing us to examine the unique association between rumination and thought suppression within PTSD. Nevertheless, these findings warrant replication in future studies that include these additional diagnostic groups. Second, as this was a veteran sample composed mostly of men, caution should be taken in generalizing to other populations, including women, particularly in light of the literature indicating gender differences in the use rumination and thought suppression (Johnson and Whisman 2013; Robichaud et al. 2003). Third, this study utilized self-report measures of habitual use of rumination and thought suppression in a cross-sectional design. Experimental studies that examine in-vivo use of these strategies would help elucidate their functions in response to acute negative emotions and PTSD symptoms (e.g., re-experiencing symptoms) and a longitudinal design would allow for more definitive conclusions about causality. Fourth, this study used DSM-IV criteria to diagnose PTSD and depressive disorders. Within DSM-5, the PTSD diagnosis includes a separate cluster of symptoms highlighting alterations in mood and cognition (Cluster D), including experiences of self-blame and the negative impact of the trauma on views of the self and others (APA 2013). Critics have argued that many of these symptoms overlap with depressive symptoms and make it difficult to differentiate between depressive processes and those specific to PTSD (Friedman et al. 2011). However, the findings from this study suggest a unique function of brooding and reflective cognitive strategies in PTSD separate from depression. Replication of study findings using the new diagnostic criteria will allow us to better understand the relationships between thought processes (e.g., cognitive avoidance strategies) and thought content (e.g., self-criticism, past life experiences) as factors that may contribute to the onset and maintenance of PTSD in its current form.
Overall, our findings are consistent with the hypothesis that rumination, particularly brooding and reflection, functions as a cognitive avoidance strategy in individuals with comorbid depression and PTSD. Future mediational and experimental studies are needed to further explicate the functions of rumination in individuals with depression, PTSD, and other relevant disorders. Clinically, study results support the need to assess and understand the content and function of ruminative thoughts among individuals with depression and PTSD to inform treatment for this group. Specifically, psychotherapeutic treatments for PTSD emphasize reduction of trauma-related avoidance behaviors (both behavioral and cognitive) to promote recovery (e.g., Cooper et al. 2017; Cukor et al. 2009; Foa et al. 2008). Study results offer further support for the conceptualization of certain types of rumination as cognitive avoidance/suppressive strategies in PTSD, suggesting that this may be an important adjunctive clinical target. Several techniques have been shown to be effective at reducing thought suppression and PTSD symptoms (e.g., acceptance of distressing thoughts, exposure to trauma memories, cognitive restructuring to challenge distortions). However, it is currently unclear whether such strategies would also be effective for reducing rumination in individuals with PTSD. Alternative strategies may be needed to help break the cycle of rumination prior to or in conjunction with other empirically-supported intervention techniques.
References
Abramowitz, J. S., Tolin, D. F., & Street, G. P. (2001). Paradoxical effects of thought suppression: A meta-analysis of controlled studies. Clinical Psychology Review, 21(5), 683–703. https://doi.org/10.1016/S0272-7358(00)00057-X.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: American Psychiatric Association.
Arditte, K. A., & Joormann, J. (2011). Emotion regulation in depression: Reflection predicts recovery from a major depressive episode. Cognitive Therapy and Research, 35(6), 536–543. https://doi.org/10.1007/s10608-011-9389-4.
Bagby, R. M., Rector, N. A., Bacchiochi, J. R., & McBride, C. (2004). The stability of the Response Styles Questionnaire Rumination Scale in a sample of patients with major depression. Cognitive Therapy and Research, 28(4), 527–538. https://doi.org/10.1023/B:COTR.0000045562.17228.29.
Beck, A. T., Steer, R. A., Ball, R., & Ranieri, W. (1996). Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. Journal of Personality Assessment, 67(3), 588–597. https://doi.org/10.1207/s15327752jpa6703_13.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory—second edition (BDI-II). San Antonio: The Psychological Corporation.
Birrer, E., & Michael, T. (2011). Rumination in PTSD as well as in traumatized and non-traumatized depressed patients: A cross-sectional clinical study. Behavioural and Cognitive Psychotherapy, 39(4), 381–397. https://doi.org/10.1017/S1352465811000087.
Birrer, E., Michael, T., & Munsch, S. (2007). Intrusive images in PTSD and in traumatised and non-traumatised depressed patients: A cross-sectional clinical study. Behaviour Research and Therapy, 45(9), 2053–2065. https://doi.org/10.1016/j.brat.2007.03.005.
Breslau, N., Davis, G. C., Peterson, E. L., & Schultz, L. (1997). Psychiatric sequelae of posttraumatic stress disorder in women. Archives of General Psychiatry, 54(1), 81–87. https://doi.org/10.1001/archpsyc.1997.01830130087016.
Butler, G., Wells, A., & Dewick, H. (1995). Differential effects of worry and imagery after exposure to a stressful stimulus: A pilot study. Behavioural and Cognitive Psychotherapy, 23(1), 45–56. https://doi.org/10.1017/S1352465800017628.
Campbell, D. G., Felker, B. L., Liu, C. F., Yano, E. M., Kirchner, J. E., Chan, D., … Chaney, E. F. (2007). Prevalence of depression-PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine, 22(6), 711–718. https://doi.org/10.1007/s11606-006-0101-4.
Cooper, A. A., Clifton, E. G., & Feeny, N. C. (2017). An empirical review of potential mediators and mechanisms of prolonged exposure therapy. Clinical Psychology Review, 56, 106–121. https://doi.org/10.1016/j.cpr.2017.07.003.
Cribb, G., Moulds, M. L., & Carter, S. (2006). Rumination and experiential avoidance in depression. Behaviour Change, 23(3), 165–176. https://doi.org/10.1375/bech.23.3.165.
Cukor, J., Spitalnick, J., Difede, J., Rizzo, A., & Rothbaum, B. O. (2009). Emerging treatments for PTSD. Clinical Psychology Review, 29(8), 715–726. https://doi.org/10.1016/j.cpr.2009.09.001.
Dozois, D. J. A., Dobson, K. S., & Ahnberg, J. L. (1998). A psychometric evaluation of the Beck Depression Inventory-II. Psychological Assessment, 10(2), 83–89. https://doi.org/10.1037/1040-3590.10.2.83.
Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. https://doi.org/10.1016/S0005-7967(99)00123-0.
Ehring, T., Frank, S., & Ehlers, A. (2008). The role of rumination and reduced concreteness in the maintenance of posttraumatic stress disorder and depression following trauma. Cognitive Therapy and Research, 32(4), 488–506. https://doi.org/10.1007/s10608-006-9089-7.
Ehring, T., Fuchs, N., & Klasener, I. (2009). The effects of experimentally induced rumination versus distraction on analogue posttraumatic stress symptoms. Behavior Therapy, 40(4), 403–413. https://doi.org/10.1016/j.beth.2008.10.001.
Ehring, T., & Watkins, E. R. (2008). Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy, 1(3), 192–205. https://doi.org/10.1521/ijct.2008.1.3.192.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (2002). Structured clinical interview for DSM-IV TR axis I disorders, research version, patient edition with psychotic screen (SCID-I/P W/PSY SCREEN). New York: Biometrics Research, New York State Psychiatric Institute.
Flack, W. F. Jr., Litz, B. T., Hsieh, F. Y., Kaloupek, D. G., & Keane, T. M. (2000). Predictors of emotional numbing, revisited: A replication and extension. Journal of Traumatic Stress, 13(4), 611–618. https://doi.org/10.1023/A:1007806132319.
Flory, J. D., & Yehuda, R. (2015). Comorbidity between post-traumatic stress disorder and major depressive disorder: Alternative explanations and treatment considerations. Dialogues in Clinical Neuroscience, 17(2), 141–150.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (2008). Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (2nd ed.). New York: Guilford Press.
Friedman, M. J., Resick, P. A., Bryant, R. A., & Brewin, C. R. (2011). Considering PTSD for DSM-5. Depression and Anxiety, 28(9), 750–769. https://doi.org/10.1002/da.20767.
Garnefski, N., & Kraaij, V. (2007). The cognitive emotion regulation questionnaire. European Journal of Psychological Assessment, 23, 141–149. https://doi.org/10.1027/1015-5759.23.3.141.
Giorgio, J. M., Sanflippo, J., Kleiman, E., Reilly, D., Bender, R. E., Wagner, C. A., … Alloy, L. B. (2010). An experiential avoidance conceptualization of depressive rumination: Three tests of the model. Behaviour Research and Therapy, 48(10), 1021–1031. https://doi.org/10.1016/j.brat.2010.07.004.
Gold, D. B., & Wegner, D. M. (1995). Origins of ruminative thought: Trauma, incompleteness, nondisclosure, and suppression. Journal of Applied Social Psychology, 25(14), 1245–1261. https://doi.org/10.1111/j.1559-1816.1995.tb02617.x.
Harvey, A. G., & Bryant, R. A. (1998). The effect of attempted thought suppression in acute stress disorder. Behaviour Research and Therapy, 36(6), 583–590. https://doi.org/10.1016/S0005-7967(98)00052-7.
Holmbeck, G. N. (2002). Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology, 27(1), 87–96. https://doi.org/10.1093/jpepsy/27.1.87.
Johnson, D. P., & Whisman, M. A. (2013). Gender differences in rumination: A meta-analysis. Personality and Individual Differences, 55(4), 367–374. https://doi.org/10.1016/j.paid.2013.03.019.
Kuo, J. R., Edge, I. G., Ramel, W., Edge, M. D., Drabant, E. M., Dayton, W. M., & Gross, J. J. (2012). Trait rumination is associated with enhanced recollection of negative words. Cognitive Therapy and Research, 36(6), 722–730. https://doi.org/10.1007/s10608-011-9430-7.
Liverant, G. I., Kamholz, B. W., Sloan, D. M., & Brown, T. A. (2011). Rumination in clinical depression: A type of emotional suppression? Cognitive Therapy and Research, 35(3), 253–265. https://doi.org/10.1007/s10608-010-9304-4.
Marroquin, B. M., Fontes, M., Scilletta, A., & Miranda, R. (2010). Ruminative subtypes and coping responses: Active and passive pathways to depressive symptoms. Cognition and Emotion, 24(8), 1446–1455. https://doi.org/10.1080/02699930903510212.
Michael, T., Halligan, S. L., Clark, D. M., & Ehlers, A. (2007). Rumination in posttraumatic stress disorder. Depression and Anxiety, 24(5), 307–317. https://doi.org/10.1002/da.20228.
Moulds, M. L., Kandris, E., Starr, S., & Wong, A. C. (2007). The relationship between rumination, avoidance and depression in a non-clinical sample. Behaviour Research and Therapy, 45(2), 251–261. https://doi.org/10.1016/j.brat.2006.03.003.
Nolen-Hoeksema, S. (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology, 100(4), 569–582. https://doi.org/10.1037/0021-843X.100.4.569.
Nolen-Hoeksema, S., & Morrow, J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology, 61(1), 115–121. https://doi.org/10.1521/pedi.2010.24.5.651.
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3(5), 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x.
O’Donnell, M. L., Creamer, M., & Pattison, P. (2004). Posttraumatic stress disorder and depression following trauma: Understanding comorbidity. American Journal of Psychiatry, 161(8), 1390–1396. https://doi.org/10.1176/appi.ajp.161.8.1390.
Pietrzak, R. H., Harpaz-Rotem, I., & Southwick, S. M. (2011). Cognitive-behavioral coping strategies associated with combat-related PTSD in treatment-seeking OEF-OIF Veterans. Psychiatry Research, 189(2), 251–258. https://doi.org/10.1016/j.psychres.2011.07.019.
Robichaud, M., Dugas, M. J., & Conway, M. (2003). Gender differences in worry and associated cognitive-behavioral variables. Journal of Anxiety Disorders, 17(5), 501–516. https://doi.org/10.1016/S0887-6185(02)00237-2.
Schoofs, H., Hermans, D., & Raes, F. (2010). Brooding and reflection as subtypes of rumination: Evidence from confirmatory factor analysis in nonclinical samples using the Dutch Ruminative Response Scale. Journal of Psychopathology and Behavioral Assessment, 32(4), 609–617. https://doi.org/10.1007/s10862-010-9182-9.
Seligowski, A. V., Lee, D. J., Bardeen, J. R., & Orcutt, H. K. (2015). Emotion regulation and posttraumatic stress symptoms: A meta-analysis. Cognitive Behaviour Therapy, 44(2), 87–102. https://doi.org/10.1080/16506073.2014.980753.
Shipherd, J. C., & Beck, J. G. (1999). The effects of suppressing trauma-related thoughts on women with rape-related posttraumatic stress disorder. Behaviour Research and Therapy, 37(2), 99–112. https://doi.org/10.1016/S0005-7967(98)00136-3.
Shipherd, J. C., & Beck, J. G. (2005). The role of thought suppression in posttraumatic stress disorder. Behavior Therapy, 36(3), 277–287. https://doi.org/10.1016/S0005-7894(05)80076-0.
Skre, I., Onstad, S., Torgersen, S., & Kringlen, E. (1991). High interrater reliability for the Structured Clinical Interview for DSM-III-R Axis I (SCID-I). Acta Psychiatrica Scandinavica, 84(2), 167–173. https://doi.org/10.1111/j.1600-0447.1991.tb03123.x.
Spinhoven, P., Drost, J., de Rooij, M., van Hemert, A. M., & Penninx, B. W. (2014). A longitudinal study of experiential avoidance in emotional disorders. Behavior Therapy, 45(6), 840–850. https://doi.org/10.1016/j.beth.2014.07.001.
Spinhoven, P., Penninx, B. W., Krempeniou, A., van Hemert, A. M., & Elzinga, B. (2015). Trait rumination predicts onset of Post-Traumatic Stress Disorder through trauma-related cognitive appraisals: A 4-year longitudinal study. Behaviour Research and Therapy, 71, 101–109. https://doi.org/10.1016/j.brat.2015.06.004.
Stroebe, M., Boelen, P. A., van den Hout, M., Stroebe, W., Salemink, E., & van den Bout, J. (2007). Ruminative coping as avoidance: A reinterpretation of its function in adjustment to bereavement. European Archives of Psychiatry and Clinical Neuroscience, 257(8), 462–472. https://doi.org/10.1007/s00406-007-0746-y.
Surrence, K., Miranda, R., Marroquin, B. M., & Chan, S. (2009). Brooding and reflective rumination among suicide attempters: Cognitive vulnerability to suicidal ideation. Behaviour Research and Therapy, 47(9), 803–808. https://doi.org/10.1016/j.brat.2009.06.001.
Szabo, Y. Z., Warnecke, A. J., Newton, T. L., & Valentine, J. C. (2017). Rumination and posttraumatic stress symptoms in trauma-exposed adults: A systematic review and meta-analysis. Anxiety Stress and Coping, 30(4), 396–414. https://doi.org/10.1080/10615806.2017.1313835.
Treynor, W., Gonzalez, R., & Nolen-Hoeksema, S. (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27(3), 247–259. https://doi.org/10.1023/A:1023910315561.
Watkins, E., & Moulds, M. L. (2007). Reduced concreteness of rumination in depression: A pilot study. Personality and Individual Differences, 43(6), 1386–1395. https://doi.org/10.1016/j.paid.2007.04.007.
Watkins, E. R. (2016). Rumination-focused cognitive-behavioral therapy for depression. New York: Guilford Press.
Watkins, E. R., & Moulds, M. L. (2009). Thought control strategies, thought suppression, and rumination in depression. International Journal of Cognitive Therapy, 2(3), 235–251. https://doi.org/10.1521/ijct.2009.2.3.235.
Watson, D., Weber, K., Assenheimer, J. S., Clark, L. A., Strauss, M. E., & McCormick, R. A. (1995). Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology, 104(1), 3–14. https://doi.org/10.1037/0021-843X.104.1.3.
Weathers, F. W., Litz, B. T., Herman, D., Huska, J., & Keane, T. M. (1994). The PTSD checklist—civilian version (PCL-C). Boston: National Center for PTSD.
Wegner, D. M. (1989). White bears and other unwanted thoughts: Suppression, obsession, and the psychology of mental control. New York: Penguin Press.
Wegner, D. M., & Zanakos, S. (1994). Chronic thought suppression. Journal of Personality, 62(4), 616–640. https://doi.org/10.1111/j.1467-6494.1994.tb00311.x.
Wenzlaff, R. M., & Luxton, D. D. (2003). The role of thought suppression in depressive rumination. Cognitive Therapy and Research, 27(3), 293–308. https://doi.org/10.1023/A:1023966400540.
Wilkins, K. C., Lang, A. J., & Norman, S. B. (2011). Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and Anxiety, 28(7), 596–606. https://doi.org/10.1002/da.20837.
Zanarini, M. C., & Frankenburg, F. R. (2001). Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Comprehensive Psychiatry, 42(5), 369–374. https://doi.org/10.1053/comp.2001.24556.
Funding
This work was supported by a Department of Veteran Affairs Career Development Award-II awarded to Gabrielle Liverant, Ph.D.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Laina E. Rosebrock, Kimberly A. Arditte Hall, Alora Rando, Suzanne L. Pineles, Gabrielle I. Liverant declare that they have no conflict of interest.
Ethical Approval
The research conducted in this study was continuously approved by the VA IRB board. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rosebrock, L.E., Arditte Hall, K.A., Rando, A. et al. Rumination and Its Relationship with Thought Suppression in Unipolar Depression and Comorbid PTSD. Cogn Ther Res 43, 226–235 (2019). https://doi.org/10.1007/s10608-018-9935-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-018-9935-4