Abstract
This study evaluated the effect of comorbid personality disorders on treatment outcome for male and female Veterans with posttraumatic stress disorder (PTSD). One hundred and sixty-six Veterans participated in a PTSD Residential Rehabilitation Program, which included cognitive processing therapy (CPT) provided in a combined individual and group format. Sixty-six percent of participants met criteria at pre-treatment for at least one personality disorder. No difference was found between participants with and without personality disorders on pre-treatment demographic variables, self-reported PTSD symptoms, or clinician-assessed PTSD symptoms. However, differences were found between the groups on self-reported depression symptoms. When controlling for pre-treatment self-reported depression symptoms, results indicated that both groups had significant reductions on PTSD outcome measures, regardless of the presence of a personality disorder. Additionally, a comparable number of participants with and without personality disorders no longer met criteria for PTSD following treatment. Findings suggest that Veterans with personality disorders can benefit from a CPT-based PTSD residential program.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Posttraumatic stress disorder (PTSD) affects approximately 7% of active military personnel (Department of Defense Task Force on Mental Health 2007). Research suggests that individuals with PTSD often experience adverse mental and physical health outcomes, highlighting the necessity of developing and empirically examining treatment approaches for PTSD. Among the most widely accepted and empirically supported psychosocial treatments for PTSD are cognitive-behavioral interventions (Keane et al. 2006). Cognitive-behavioral therapies (CBT) are currently recommended by experts as first-line interventions for PTSD treatment (Hembree et al. 2004), as these treatments reliably lead to the reduction of anxiety and arousal symptoms (Blake and Sonnenberg 1998). Two CBT treatments, cognitive processing therapy (CPT) and prolonged exposure (PE), are considered best practice models for the treatment of PTSD by the Department of Veterans Affairs (VA), Department of Defense, and International Society for Traumatic Stress Studies (Foa et al. 2008; Veterans Health Administration, Department of Defense 2004).
However, despite good clinical efficacy, the treatment outcome research on CBT-based interventions (e.g., CPT and PE) demonstrates that a number of individuals continue to be symptomatic at post-treatment or fail to make substantial therapeutic gains (Hembree et al. 2004). Specifically, studies of CPT and PE have shown variability in the number of participants continuing to meet diagnostic criteria for PTSD at post-treatment, including studies involving Veterans (Schnurr et al. 2007; Zayfert et al. 2002). To improve upon the efficacy of existing CBT interventions for PTSD it is important to identify individuals who are most likely to benefit from these treatments as well as those who will have less of a response and may require different or additional treatments.
One potentially important predictor of treatment outcome is the presence of one or more personality disorders. The presence of personality disorders may be particularly important as they are common in individuals with chronic PTSD, including the Veteran population (Southwick et al. 1993). For example, in an outpatient sample of Veterans with PTSD, approximately 45% had at least one personality disorder diagnosis (Dunn et al. 2004), while an inpatient sample of Veterans found an even higher prevalence of 79% with at least one personality disorder (Bollinger et al. 2000). Specifically, although no Veteran comparisons including evaluation of all personality disorders could be located, Orsillo et al. (1996) found rates of roughly 12% each of borderline PD and antisocial PD among Veterans meeting PTSD criteria. Regarding other types of trauma, a sample of treatment-seeking adult survivors of childhood sexual abuse with PTSD had similar levels of Avoidant PD (39%) and BPD (20%), but lower levels of Paranoid PD (19%) (Owens and Chard 2003). Similarly, Hembree et al.’s (2004) study with treatment-seeking sexual assault survivors found roughly similar levels of Avoidant PD (28%) among those meeting criteria for a personality disorder.
In clinical practice individuals with personality disorders are often assumed to benefit less from treatment of their Axis I conditions, relative to individuals without Axis II pathology (Newton-Howes et al. 2006; Weertman et al. 2005). Similarly, clinicians often believe that treating Axis I disorders becomes more complex in patients with Axis II disorders (Dreessen and Arntz 1998). Dreessen and Arntz (1998) reviewed 15 studies examining the impact of personality pathology on treatment for various anxiety disorders and found mixed results, with some studies indicating personality disorders have an unfavorable impact on anxiety disorder treatment and other studies reporting no effect of personality disorders. In terms of end-state functioning, the authors also emphasized that, when individuals with personality disorders have more severe symptoms at pre-treatment, they should not be expected to attain the same level of functioning as individuals without personality disorders, necessitating larger treatment gains.
Within PTSD research a few studies have examined the effects of personality disorders on treatment outcome for cognitive-behavioral therapy. In the first, Feeny et al. (2002) examined the impact of borderline personality characteristics (BPC) on treatment outcome for PE among 72 women with assault-related PTSD. Participants underwent a diagnostic assessment at pre- and post-treatment; however, assessment of personality disorders was reserved until post-treatment to prevent possible bias in diagnosing a personality disorder in the presence of an Axis I condition. Findings demonstrated that women with and without BPC showed significant reductions in PTSD severity, depression, and anxiety, as well as improvement in social functioning. Contrary to their hypotheses, both groups appeared to benefit from treatment. In particular, no statistically significant group differences emerged on PTSD diagnostic status between women with BPC and those without. However, compared with the non-BPC group, fewer women with BPC met criteria for good end-state functioning at the conclusion of treatment, indicating relatively less improvement than participants without personality pathology. Good end-state functioning was determined through the use of several measures and defined using scores of 20 or below on an interview measure of PTSD, 40 or below on self-reported anxiety, and 10 or below on self-reported depression (Feeny et al. 2002). Clarke et al. (2008) also examined the impact of BPC on treatment outcome for CBT among females with rape-related PTSD. The findings of this study indicated that individuals with higher BPC scores also had higher PTSD severity at the pre-treatment assessment. However, despite these higher scores, individuals with BPC were just as likely to complete and respond to treatment. It is important to note that both of these studies (Clarke et al. 2008; Feeny et al. 2002) focused on Borderline Personality characteristics, rather than meeting full criteria for a diagnosis of Borderline Personality Disorder.
A major limitation of the Feeny et al. (2002) study was the low number of participants with BPC. Sixty women without BPC undergoing active treatment were compared to only eight women with BPC to obtain results for this study. The small number of women with BPC limited the cell sizes in some of the comparisons, and thus reduced power of the study to detect small to medium-sized effects. Two years following the Feeny et al. (2002) publication, Hembree et al. (2004) published similar research involving a larger number of participants with a broader range of personality disorders. Instead of focusing exclusively on borderline personality disorder, Hembree and colleagues examined participants with any type of Axis II pathology. In this study, 46 female sexual assault survivors without personality pathology were compared to 29 women with one or more personality disorder diagnoses. Participants were evaluated at pre-treatment and post-treatment; however, assessment of personality disorders was again delayed until post-treatment.
Results showed that women with and without personality disorders appeared to benefit comparably from treatment, similar to the Feeny et al. (2002) study. Specifically, 66% of participants with personality disorders no longer met the criteria for PTSD compared to 78% in the non-personality disordered group (difference not statistically significant). However, women with personality disorders achieved significantly inferior end-state functioning compared to women without personality disorders in the sample. Good end-state functioning was defined as a post-treatment interview PTSD score of 15 or below and self-reported depression and anxiety scores of 10 or less (Hembree et al. 2004). Seventy-six percent of participants without a personality disorder achieved good end-state functioning, compared with only 41% from the group diagnosed with a comorbid personality disorder. Hembree et al. (2004) concluded that comorbid personality disorder diagnoses may diminish treatment outcome for PE in terms of end-state functioning, but that both groups seemed to benefit from therapy.
Finally, van Minnen et al. (2002) examined potential predictors of treatment outcome, including personality disorder diagnoses, for two samples of patients with PTSD who were being treated with PE. The two groups consisted of patients from a university outpatient clinic setting and a community mental health center. Participants were assessed at pre- and post-treatment sessions. Results indicated that personality disorder diagnoses were not a predictor of treatment outcome or whether a patient dropped out of treatment prematurely.
The primary purpose of the current study was to evaluate the impact of personality disorders on treatment outcome for a residential PTSD program employing individual and group CPT and to further the literature on identification of individuals who are likely to succeed in this therapy modality. This study is the first, to our knowledge, to address this research question among Veterans and also within a residential PTSD program setting. Because CPT and PE demonstrated comparable efficacy in a recent randomized clinical trial (Resick et al. 2002), it was anticipated that the results of this study would be similar to the findings of Feeny et al. (2002) and Hembree et al. (2004). One weakness of prior research has been the examination of personality traits, rather than full criteria for personality disorders. We sought to improve upon these methods by assessing full criteria for all personality disorders, not just borderline personality disorder characteristics. We hypothesized that (1) the PD+ and PD− groups would differ on study measures assessing psychopathology, with PD+ participants reporting higher levels of psychological symptoms. It was also expected that (2) both groups would benefit from treatment, as found in the prior studies, but PD+ participants would evidence less improvement following treatment relative to PD− participants. Furthermore, we predicted that (3) consistent with previous research, there would not be a statistically significant difference with regard to post-treatment PTSD diagnostic status between PD+ and PD− participants.
Method
Participants
Participants for this study were 184 adult patients admitted to a PTSD residential program in a Veterans Affairs Medical Center located in the Midwest between May 2005 and April 2007. During this time, 13 patients (7%) either dropped out of treatment or were dismissed from the program due to behavioral or substance problems. An additional 5 participants were removed from analyses due to subthreshold PTSD. Of the 166 treatment completers (participants who completed the 7 weeks of the treatment program and met diagnostic criteria for PTSD), 75% were male and 25% were female. The most frequently reported index traumas among study participants were combat (54%) and sexual assault (24%), followed by other traumatic events (22%; physical assault, childhood sexual abuse, transportation accident, etc.).
The mean age for the sample was 51 years (SD = 9.44), and the mean education level was 13.33 years (SD = 1.86). The ethnic composition consisted of: 63% Caucasian, 36% African-American, and 1% Native American. Nineteen percent were married, 39% were divorced, 16% were single, 17% were remarried, 7% separated, and 1% widowed. Sixteen percent reported they were employed either full- or part-time, 34% were unemployed, 33% were disabled, 14% were retired, and 3% were students/other. A majority of participants (56%) served in the military during the Vietnam era, 24% served post-Vietnam, 15% were Persian Gulf War Veterans, 3% served in Iraq/Afghanistan, and (2%) served in other service eras.
Inclusionary criteria for admission into the program were that participants had current PTSD and were referred to the program by a mental health practitioner. Exclusionary criteria included: current psychosis, active substance dependence, pending legal issues, and severe medical problems that would have prevented full attendance in the program. Participants were not excluded due to the presence of any comorbid psychiatric conditions, except untreated psychotic disorders. The same inclusion and exclusion criteria were used for both admission into the program and participation in the study. Archival data from the residential patients were obtained for the study. Patient information was extracted from files and computerized records available on all participants admitted to the program during the selected 2-year period.
Measures
Clinician-Administered Measures
Clinician-Administered PTSD Scale (CAPS; Blake et al. 1990)
The CAPS assesses all of the PTSD diagnostic criteria outlined in the DSM-IV-TR (American Psychological Association [APA] 2000). The CAPS is used to assess the frequency and severity of each of the 17 PTSD symptoms. Scores for each symptom are determined by adding the frequency and intensity ratings. All 17 items are then summed to obtain a total severity score (Blanchard et al. 1995).
Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II; First et al. 1997)
The SCID-II is a semi-structured interview designed to assess Axis II disorders. Scores on each item of the SCID-II are rated by clinicians on a scale of one (absent) to three (present). The number of present items is then summed for each disorder, and this score is checked against the number of items required in the DSM-IV-TR to make a diagnosis (First et al. 1997).
Self-Report Measures
Beck Depression Inventory: Second Edition (BDI-II; Beck et al. 1996)
The BDI-II is an extensively used instrument for assessing depressive symptoms in adults. The BDI-II consists of 21 items that are rated on a four-point Likert-type scale ranging from zero to three (higher scores indicate greater symptomatology), for a maximum score of 63. The BDI-II has been shown to have high internal consistency (coefficient alpha ranging from .92 to .93), and good test–retest reliability (r = .93).
PTSD Checklist Stressor Specific Version (PCL-S; Weathers et al. 1991)
The PCL is an extensively used self-report measure of PTSD symptoms. The PCL-S asks participants to rate their symptoms in relation to a specific traumatic stressor (for this study, the specific stressor was participants’ index trauma). Items on the PCL-S directly correspond with the 17 diagnostic criteria for PTSD and each item is rated on a five-point Likert-type scale ranging from 1 (not at all) to 5 (extremely). The PCL has demonstrated strong psychometric properties, including good test–retest reliability (.96) and validity (kappa = .64; Weathers et al. 1993).
Procedure
The current research was conducted in full compliance with the guidelines of the university Institutional Review Board, as well as the local VAMC Research and Development Division. Upon entry into the program Veterans were administered a battery of assessment instruments to evaluate their pre-treatment psychiatric status, including those used in the current study. All assessment and treatment procedures were conducted at the PTSD clinic, which is a setting that specializes in the provision of empirically-based treatments for individuals with anxiety-related psychopathology. Assessment measures were given by clinicians (i.e., psychologists, social workers, supervised psychology trainees) who had received extensive training and supervision in the administration of psychological tests. Upon completion of the 7-week program participants were re-evaluated using the same measures administered at pre-treatment. All assessment instruments were given at the pre-treatment and post-treatment assessments, including the SCID-II, used to determine Axis II conditions.
Treatment
The residential treatment program utilized CPT in the group and individual combined format (Chard et al. 2009). The CPT group met twice per week for an average of 12 group sessions with each group session lasting 90 min. Participants also met with their individual therapists twice per week, except for the first and last weeks when they met with their therapists only once and participated in assessments during the other time periods. The average number of individual therapy sessions was 13 with each session lasting 50–60 min. Group and individual treatment were provided by the residential treatment program staff and all individual therapists were trained in CPT by one of the manual authors who also conducted individual and group supervision for the therapists.
In addition to CPT, psychoeducational group therapy sessions were held on a daily basis, with participants attending approximately 15 groups per week. All members of each cohort attended the same groups, providing consistency in treatment received. Each group session lasted 60–90 min. Group topics included anger management, PTSD education, communication, nutrition, self-defeating behaviors, etc. Modules of dialectical behavior therapy (DBT; Linehan 1993), such as distress tolerance, were also included to increase coping skills.
Data Analytic Plan
Several data analytic strategies will be employed to determine the influence of personality disorder diagnosis on PTSD treatment outcome among Veterans in a residential program. First, the sample includes both female and male Veterans, so t tests and χ2 analyses will be conducted to determine any significant differences on pre-treatment and study variables. Once these analyses have been conducted, two groups will be created from the existing dataset: (1) Veterans who met diagnostic criteria for at least one personality disorder, based on the SCID-II at the pre-treatment assessment (PD+) and (2) Veterans who did not meet diagnostic criteria for a personality disorder at the pre-treatment assessment (PD−). These groups will be used for all subsequent analyses. Following the creation of this grouping variable, t tests and χ2 analyses will be used to investigate pre-treatment and study variables for significant differences. The main study analysis investigating the influence of personality disorder diagnosis on PTSD treatment outcome will involve a repeated measures multivariate analysis of covariance (MANCOVA), where depression will be entered as a covariate and clinician-assessed and self-reported PTSD symptom severity will serve as the outcome variables. Lastly, clinical improvement will be assessed with the following analyses: (1) a χ2 analysis for PTSD diagnostic status (2) mean differences on PTSD symptom measures (3) mean change on PTSD symptom measures (4) post-treatment mean differences on self-reported depression severity, and (5) descriptive data regarding personality disorder diagnostic status at post-treatment.
Results
Gender Differences
There were no significant differences between males and females on pre-treatment CAPS scores t(163) = .28, ns; PCL scores t(159) = .83, ns; or BDI scores t(162) = −.10, ns, so participants were grouped for further analyses. There were also no significant differences on post-treatment CAPS scores t(162) = −.29, ns; PCL scores t(161) = 1.50, ns; or presence of Axis II disorder χ2(1) = .80, ns. However, there were significant differences on post-treatment BDI scores t(159) = 2.11, P < .05, with males (M = 26.52, SD = 15.39) scoring higher on the measure than females (M = 20.93, SD = 12.69).
Sample Characteristics
Of the 166 Veterans included in the sample, 110 (66%) were diagnosed with at least one personality disorder at pre-treatment. The most common personality disorder diagnosis was Paranoid (45%), followed by Avoidant (30%), Borderline (14.5%), Obsessive–Compulsive (11%), Passive-Aggressive (4%), Depressive (6%), Dependent (5%), and Antisocial (3%). There were three cases of Narcissistic (2%) and two cases of Schizotypal (1%). Fifty-six (30%) of the PD+ participants were diagnosed with one personality disorder, Forty-one (22%) were diagnosed with two personality disorders, and 16 (9%) were diagnosed with three or more personality disorders.
Pre-Treatment Comparisons
To examine pre-treatment group differences, χ2 analyses were performed to determine differences between the PD+ and PD− groups on the categorical variables and t tests were employed to compare the groups on continuous measures. Results of the χ2 analyses demonstrated that the PD+ and PD− groups did not significantly differ in terms of gender, χ2(1) = 1.19, ns; ethnicity (white/other), χ2(1) = 1.14, ns; marital status (married/other), χ2(1) = 3.62, P = .06, ns; employment status (employed/other), χ2(1) = 1.90, ns; or service era (Vietnam/other), χ2(1) = .11, ns. The groups also did not significantly differ with regard to whether or not participants had a past history of alcohol abuse/dependence χ2(2) = 3.22, ns; drug abuse/dependence χ2(2) = 4.98, P = .08; or current major depressive disorder χ2(1) = .90, ns. Also, the PD+ and PD− groups did not significantly differ with regard to residential treatment drop-out, χ2(1) = .01, ns. Independent samples t tests indicated that no significant differences emerged between the groups pertaining to age t(165) = .55, ns; education t(165) = 1.38, ns; or percent service connection for PTSD t(165) = 1.42, ns.
A series of two-tailed independent samples t tests revealed that the PD+ (n = 110) and PD− (n = 57) groups did not significantly differ on the pre-treatment CAPS score total t(164) = .87, ns; or pre-treatment PCL score t(163) = −1.04, ns. However, the groups did significantly differ on pre-treatment BDI scores t(160) = −2.36, P < .05, with the PD+ Veterans endorsing higher symptom distress (M = 36.24, SD = 9.78) than PD− Veterans (M = 32.34, SD = 10.52). Due to significant differences on pre-treatment BDI scores between PD+/PD− participants, pre-treatment self-reported depression severity score were used as a covariate in multivariate analyses.
Effects of Treatment
A RM MANCOVA was conducted to determine the effects of PD diagnostic status on treatment outcome, controlling for pre-treatment self-reported depression severity score. The mean scores and standard deviations for both groups at pre- and post-treatment are displayed in Table 1. The RM MANCOVA results demonstrated a significant within-subjects effect for time, F(2, 153) = 14.11, P < .000, partial η 2 = .16, d = 1.0. These results show that the PD+ and PD− groups significantly decreased their scores on PTSD outcome measures following the course of treatment, indicating a reduction in PTSD symptoms. Specifically, the univariate tests showed that scores on both the CAPS, F(1, 154) = 27.64, P < .000, partial η 2 = .15, d = 1.0; and the PCL, F(1,154) = 10.80, P < .001, partial η 2 = .07, d = .90 significantly decreased over the course of residential treatment. A significant between-subjects effect was also found for depression, F(2, 153) = 32.88, P < .000, partial η 2 = .30, d = 1.0, suggesting that the groups significantly differed on pre-treatment self-reported depression symptoms.
No significant interactions resulted from the analyses. Specifically, the group x time interaction, F(2, 153) = .76, ns, partial η 2 = .01, d = .24; and depression x time interaction, F(2, 153) = 1.12, ns, partial η 2 = .01, d = .18, did not yield significant results Overall findings suggest that when controlling for depression, the PD+ and PD− groups were as likely to make therapeutic gains.
Clinical Improvement and Post-treatment Comparisons
A statistically significant difference was not found between the PD+ and PD− groups on the number of participants who met diagnostic criteria for PTSD at post-treatment. Results of a χ2 analysis indicated that only 45% of the 56 PD− participants met criteria for PTSD at post-treatment, whereas 49% of the 110 PD+ participants met criteria for PTSD after treatment. This difference was not statistically significant, χ2(1) = .24, ns, and indicates that the groups were comparable in their rates of meeting diagnostic criteria for PTSD following treatment. Additionally, mean differences on the outcome measures were investigated. Independent t tests indicated that the PD+ and PD− groups did not significantly differ on the post-treatment CAPS total score t(163) = −.10, ns, or post-treatment PCL score t(162) = −.27, ns.
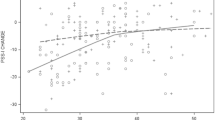
Clinical improvement was considered in terms of participants who no longer met PTSD diagnostic criteria as measured by the CAPS, in addition to the mean change in symptom scores on the PTSD outcome measures. The mean on the CAPS for the PD− decreased by 44% (35 points) from a total score (78) above the recommended diagnostic cut-off (e.g., 45; Blake et al. 1990) to a total score (43) below the recommended diagnostic cut-off. For the PD+ group, the mean on the CAPS decreased by 43% (33 points) from a total score (76) above the recommended diagnostic cut-off to a total score (43) below the recommended diagnostic cut-off. Independent t tests did not reveal a statistically significant difference on the mean CAPS change score between the groups, t(163) = −.10, ns.
Clinical improvement was also assessed on self-report measures of PTSD and depression symptoms. The mean for the PD− group on the PCL decreased by 14% (9 points) from a total score of 65 to a score of 56 (50 is the recommended cut-off for diagnosis; Weathers et al. 1993). For the PD+ group, the mean score on the PCL decreased by 15% (10 points) from a total score of 67 to a score of 57. The difference between the groups on mean change of PCL scores from pre-treatment to post-treatment was not significant, t(163) = −.27, ns. Although individuals with a personality disorder diagnosis endorsed greater depression severity at pre-treatment, the groups did not differ on post-treatment depression severity, t(160) = −.67, ns. Taken together, these findings highlight the lack of significant differences between the groups on measures of self-reported PTSD and depression symptoms following residential PTSD treatment.
Change in diagnostic status regarding Axis II conditions was also evaluated. Although diagnostic status for Axis II conditions at the pre-treatment assessment was used for the majority of analyses, Axis II diagnostic status was also collected at the post-treatment assessment. At the pre-treatment assessment, 110 (51%) of the sample met criteria for an Axis II condition, with 76 (36%) meeting criteria at the post-treatment assessment. Thirty-six individuals (17%) had an Axis II disorder at the pre-treatment assessment, but no longer met criteria at the post-treatment assessment. Six (3%) individuals did not meet criteria for an Axis II disorder at the pre-treatment assessment, but did meet criteria at the post-treatment assessment.
Discussion
The primary objective of the current research was to examine the influence of personality disorders on PTSD treatment by extending two studies that previously explored the impact of personality disorders on treatment outcome for PE (i.e., Feeny et al. 2002; Hembree et al. 2004). Several findings emerged from this study, which expand upon previous research findings. As hypothesized, the PD+ and PD− groups did not differ on pre-treatment demographic variables or measures of PTSD, although PD+ participants scored significantly higher on self-report measures of depression. The difference on self-reported symptoms of depression among the PD+ and PD− participants is consistent with the results from the Clarke et al. (2008) study. Furthermore, this finding supports prior research suggesting that individuals with personality disorders exhibit high levels of general psychopathology given the extensive comorbidity, and perhaps overlap, with Axis I disorders (Kessler et al. 1995). Results are also consistent with findings of Feeny et al. (2002), which showed that PD+ participants did not significantly differ from PD− participants on pre-treatment measures of PTSD, including the PTSD Symptom Scale—Interview (PSS-I; Foa et al. 1993). The findings of both of these studies suggest that clinician and self-report ratings of PTSD symptoms are not markedly different for participants with and without personality pathology at pre-treatment.
The investigators also hypothesized that while the PD+ and PD− groups would both benefit from treatment, the PD− participants would achieve significantly greater therapeutic gains. However, the findings only partially supported these predictions, as both groups of participants benefited from treatment as evidenced by statistically significant reductions across measures of psychopathology from pre- to post-treatment on the CAPS and PCL. These findings slightly differ from the findings of Feeny et al. (2002) and Clarke et al. (2008), who showed that although individuals with personality disorders significantly reduced their symptoms over the course of treatment, those without personality disorders evidenced greater treatment gains. It is possible that controlling for depression severity and using personality diagnosis assessed as pre-treatment, rather than post-treatment, may have contributed to this difference in findings and suggests that depression symptoms may be more influential on treatment outcome as compared to personality disorder diagnosis.
Post-treatment PTSD diagnostic status was also examined to determine the differential effects of treatment for the PD+ and PD− participants. We predicted that no significant differences would emerge with regard to post-treatment PTSD diagnostic status between the PD+ and PD− participants, which was supported by the results. Specifically, findings indicated that at post-treatment approximately 49% of the PD+ participants continued to meet criteria for PTSD, whereas only 45% of the PD− participants still met criteria for this diagnosis. These results are comparable to findings from both Feeny et al. (2002) and Hembree et al. (2004), in which no difference was found between the groups on PTSD diagnostic status at post-treatment.
Overall, the results of this study suggest that Veterans with personality disorder diagnoses score higher on measures of self-reported depression at pre-treatment but not on measures of clinician-assessed and self-reported PTSD symptoms at either pre- or post-treatment. This finding indicates that Veterans with personality disorders were still able to benefit from a PTSD residential program providing individual and group CPT. These results support the position of Dreessen and Arntz (1998), who suggested that it is inadvisable to exclude individuals with personality disorders from Axis I treatment because they do seem to benefit. However, it should be noted that individuals with personality disorders seem to consistently present with more severe depression symptoms at pre-treatment. Despite the greater depression severity at pre-treatment for individuals with personality disorders, they were able to attain the same level of symptom reduction as individuals without personality disorder diagnoses, suggesting that these individuals may actually be evidencing greater therapeutic gains.
This study contains several noteworthy strengths. Findings from the current study contribute to the research base of understanding variability in response to a PTSD residential treatment program providing CPT. No prior research appears to have explicitly explored this topic, focused on the Veteran population, or investigated CPT rather than PE. A second strength of this research is the large sample size relative to other studies of a similar nature. For example, the study conducted by Feeny et al. (2002) included only eight participants with either sub-threshold or full personality disorder diagnoses. In this study, 110 participants met full criteria for at least one personality disorder and were compared with 57 non-PD participants. The current study also improved upon prior research by examining all personality disorders, rather than focusing solely on borderline personality disorder characteristics. Finally, this research was not conducted as part of a controlled study, which allowed for a broader range of inclusionary criteria. These participants presented with complex problems and trauma histories, and may typify patients encountered in a community mental health setting. As such, the results may be more applicable and generalizable (Chard 2005).
A major limitation of this work was the reliance on a categorical approach to define personality pathology (i.e., disorders were present vs. absent). Recent forays into personality research suggest that personality dysfunction may be better characterized using dimensional models. Also, it should be noted that the Veterans receiving residential PTSD treatment in the program received not only individual CPT, but also received group CPT as well as numerous other psychoeducational groups. The amount of therapy received by Veterans is likely more than individuals receive based on the CPT manual for outpatients, supportive outpatient therapy, and perhaps other residential programs, which may affect generalizability. Furthermore, as the study was conducted as part of clinical care, inter-rater reliability was not calculated for diagnostic decisions based on the assessment instruments. Additional limitations in this study regard the use of archival clinical records, lack of randomization, unequal group size, and limited ethnic representation.
The limitations inherent in this study provide insight into directions for future research. First, the results suggest that both participants with and without personality pathology are able to benefit from a PTSD residential program providing CPT in an individual and group format. This finding is particularly encouraging given that at least two prior studies have also suggested that participants with personality pathology experience psychological symptom reduction from CBT (i.e., Feeny et al. 2002; Hembree et al. 2004; Clarke et al. 2008). Future studies should examine whether the inclusion of therapeutic elements specifically designed to target personality disorder symptoms would be helpful for PTSD/PD+ individuals, such as the affect regulation techniques described by Linehan (1993). In addition future studies should attempt to replicate these findings with Veterans in outpatient treatment to account for the effects that the residential milieu may have contributed.
The current study supports the use of CPT in a residential program as an effective treatment for PTSD in patients with and without personality disorder diagnoses. In addition, this research demonstrated that Veterans with personality disorders can experience meaningful changes in their functioning, despite research suggesting these individuals to be particularly treatment recalcitrant. The employment of empirically valid treatment approaches, such as CPT, is particularly important in light of the high prevalence of PTSD in Veterans of all eras and the increasing number of Veterans returning from Iraq and Afghanistan with a diagnosis of PTSD.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association. text revision.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation.
Blake, D. D., & Sonnenberg, R. T. (1998). Outcome research on behavioral and cognitive-behavioral treatments for trauma survivors. In V. M. Folette, J. I. Ruzek, & F. R. Abueg (Eds.), Cognitive-behavioral therapies for trauma (pp. 15–47). New York, NY: The Guilford Press.
Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Charney, D. S., & Keane, T. M. (1990). The clinician-administered PTSD scale-IV. Boston: National Center for PTSD, Behavioral Sciences Division.
Blanchard, E. B., Hickling, E. J., Taylor, A. E., Forneris, C. A., Loos, W., & Jaccard, J. (1995). Effects of varying scoring rules of the clinician-administered PTSD scale (CAPS) for the diagnosis of posttraumatic stress disorder in motor vehicle accident victims. Behaviour Research and Therapy, 33, 471–475.
Bollinger, A. R., Riggs, D. S., Blake, D. D., & Ruzek, J. I. (2000). Prevalence of personality disorders among combat veterans with posttraumatic stress disorder. Journal of Traumatic Stress, 13, 255–270.
Chard, K. M. (2005). An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology, 73, 965–971.
Chard, K. M., Resick, P. A., Monson, C. M., & Kattar, K. (2009). Cognitive processing therapy therapist group manual: Veteran/military version. Washington, DC: Department of Veteran’s Affairs.
Clarke, S. B., Rizvi, S. L., & Resick, P. A. (2008). Borderline personality characteristics and treatment outcome in cognitive-behavioral treatments for PTSD in female rape victims. Behavior Therapy, 39, 72–78.
Department of Defense Task Force on Mental Health. (2007). An achievable vision: Report of the department of defense task force on mental health. Falls Church, VA: Defense Health Board.
Dreessen, L., & Arntz, A. (1998). The impact of personality disorders on treatment outcome of anxiety disorders: Best-evidence synthesis. Behaviour Research and Therapy, 36, 483–504.
Dunn, N. J., Yanasek, E., Schillaci, J., Simotas, S., Rehm, L. P., Souchek, J., et al. (2004). Personality disorders in veterans with posttraumatic stress disorder and depression. Journal of Traumatic Stress, 17, 75–82.
Feeny, N. C., Zoellner, L. A., & Foa, E. B. (2002). Treatment outcome for chronic PTSD among female assault victims with borderline personality characteristics: A preliminary examination. Journal of Personality Disorders, 16, 30–40.
First, M. B., Gibbon, M., Spitzer, R. L., Williams, J. B. W., & Benjamin, L. S. (1997). User’s guide for the structured clinical interview for DSM-IV axis II personality disorders (SCID-II). Washington, DC: American Psychiatric Press, Inc.
Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (2008). Effective treatments for PTSD, Practice guidelines from the international society for traumatic stress studies (2nd ed.). New York: Guilford Press.
Foa, E. B., Riggs, D. S., Dancu, C. V., & Rothbaum, B. O. (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress, 6, 459–473.
Hembree, E. A., Cahill, S. P., & Foa, E. B. (2004). Impact of personality disorders on treatment outcome for female assault survivors with chronic posttraumatic stress disorder. Journal of Personality Disorders, 18, 117–127.
Keane, T. M., Marshall, A. D., & Taft, C. T. (2006). Posttraumatic stress disorder: Etiology, epidemiology and treatment outcome. Annual Review of Clinical Psychology, 2, 161–197.
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060.
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. New York, NY: The Guilford Press.
Newton-Howes, G., Tyrer, P., & Johnson, T. (2006). Personality disorder and the outcome of depression: A meta-analysis of published studies. British Journal of Psychiatry, 188, 13–20.
Orsillo, S. M., Weathers, F. W., Litz, B. T., Steinberg, H. R., Huska, J. A., & Keane, T. M. (1996). Current and lifetime psychiatric disorders among veterans with war zone-related posttraumatic stress disorder. Journal of Nervous and Mental Disease, 184, 307–313.
Owens, G. P., & Chard, K. M. (2003). Comorbidity and psychiatric diagnoses among women reporting child sexual abuse. Child Abuse and Neglect, 27, 1075–1082.
Resick, P. A., Nishith, P., Weaver, T. L., Astin, M. C., & Feuer, C. A. (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70, 867–879.
Schnurr, P. P., Friedman, M. J., Engel, C. C., Foa, E. B., Shea, M. T., Chow, B. K., et al. (2007). Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. Journal of the American Medical Association, 297(8), 820–830.
Southwick, S. M., Yehuda, R., & Giller, E. L. (1993). Personality disorders in treatment-seeking combat Veterans with posttraumatic stress disorder. American Journal of Psychiatry, 150, 1020–1023.
van Minnen, A., Arntz, A., & Keijsers, G. P. J. (2002). Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behaviour Research and Therapy, 40, 439–457.
Veterans Health Administration, Department of Defense. (2004). VA/DoD clinical practice guideline for the management of post-traumatic stress. Version 1.0. Washington, DC: Veterans Health Administration, Department of Defense.
Weathers, F. W., Huska, J. A., & Keane, T. M. (1991). PCL-S for DSM-IV. Boston: National Center for PTSD–Behavioral Science Division.
Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., & Keane, T. M. (1993). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Poster presented at the 9th annual meeting of the International Society for Traumatic Stress Studies. San Antonio, TX: International Society for Traumatic Stress Studies.
Weertman, A., Arntz, A., Schouten, E., & Dreessen, L. (2005). Influences of beliefs and personality disorders on treatment outcome in anxiety disorder patients. Journal of Consulting and Clinical Psychology, 73, 936–944.
Zayfert, C., Becker, C. B., & Gillock, K. L. (2002). Managing obstacles to the utilization of exposure therapy with PTSD patients. In L. Van de Creek & T. L. Jackson (Eds.), Innovations in clinical practice: A source book (pp. 201–222). Sarasota, FL: Professional Resource Press.
Acknowledgments
We would like to thank the staff of the PTSD and Anxiety Disorders Clinic at the Cincinnati VAMC for the collection and entry of the data used for these analyses, in addition to the psychological care they provide to Veterans. We would specifically like to recognize Dr. Greg Bailey for his data assistance on this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walter, K.H., Bolte, T.A., Owens, G.P. et al. The Impact of Personality Disorders on Treatment Outcome for Veterans in a Posttraumatic Stress Disorder Residential Treatment Program. Cogn Ther Res 36, 576–584 (2012). https://doi.org/10.1007/s10608-011-9393-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-011-9393-8