Abstract
To explore access to secondary mental health services for New Zealand women during pregnancy and for up to 1 year post-delivery. A retrospective cohort analysis of public hospital maternity data linked to mental health collections. 27 in 1000 pregnancies were associated with access to secondary mental health services (736/27,153). Independent of ethnicity, young age (<20 years) was associated with access (RR1.84; 95 %CI 1.42–2.38; P < .0001). Smoking (1.48; 1.24–1.78; P < .0001), alcohol (1.3; 0.97–1.71; P < .0001) and substance use (3.57; 2.61–4.88; P < .0001) during pregnancy were independent risk factors associated with access. Antenatal period provides an opportunity for navigating to services to ensure timely access to secondary mental health services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Poor mental health during pregnancy and the post-natal period, including post-natal distress, is a known contributing factor of maternal morbidity and mortality (Baxter 2007; PMMRC 2012).
Post-natal distress (which includes anxiety and depression) is usually managed in the primary health care sector, and prevalence is frequently reported as being experienced by between 10 and 20 % of women during the first year of having had a baby (Austin 2003; Marcus 2009; Reid and Meadows-Oliver 2007). However, little is known about the incidence and access to services for New Zealand mothers with more severe mental illness. New Zealand has one of the highest rates of maternal suicide in the OECD, and improving access to maternal mental health services is a Government priority.
In New Zealand access to secondary mental health services for moderate to severe mental health conditions is usually through referrals (including from GPs, Lead Maternity Carers and self-referral). Management of moderate to severe mental health conditions is carried out by community based multi-disciplinary teams, and many New Zealand district health boards (DHBs) have dedicated maternal mental health teams.
Māori are the indigenous people of New Zealand, and experience a higher prevalence, earlier age of onset, and greater severity of mental illness than non-Māori (Baxter 2007; Ministry of Health 2011). Māori women experience greater severity of serious disorders (such as schizophrenia or bipolar disorder) and common mental disorders (depression, anxiety, alcohol and other drug problems) often from a younger age than others (Baxter 2007; Ministry of Health 2011). Despite this, Māori maternal mental health disorders are frequently under detected by primary health professionals, in addition, there is a significant unmet need for services (Baxter 2007; Ministry of Health 2011; Schmied et al. 2013).
With the view to better understanding the service use of pregnant women with moderate to severe mental illness, the aim of our study was to explore the access to secondary mental health services during pregnancy and for up to 1 year post delivery in a cohort of New Zealand women.
We hypothesised that access to secondary mental health services for pregnant New Zealand Māori (NZM) women would be higher than New Zealand European (NZE) women, given previous reported indicators of unmet needs for mental health services and high prevalence of mental illness for Māori. We also explored access to service by age given that young maternal age is a known risk factor for post-natal distress.
Conflicts of Interest
The authors have no conflict of interest to declare.
Materials and Methods
Primary Outcome
To compare the rate of young (< 20 years of age, and overall) NZM, NZE, Pacific, Indian, Asian and Middle Eastern Latin American and African (MELAA) women accessing secondary mental health services during pregnancy and for up to 1 year post-delivery of their infant.
Study Design
A retrospective cohort study was used, and describes maternity data (previously described, Filoche et al. 2013) linked to mental health data collections.
Study Population
The study population (20,465 individual women, representing 27,153 pregnancies) consisted of women and their infants born in the public hospital system in the Capital Coast Health District Health Board (CCDHB) region of New Zealand, over an 8 year period from 2001 to 2008. CCDHB serves a population of approximately 291,300 (3) with three maternity units. Infants born prior to 20 weeks gestation, and those born at home (planned or unplanned) were not included as these data were not available in the dataset. All infants and mothers were identified by a National Health Index number (NHI), a unique patient identifier ascribed to all New Zealand citizens at birth that is used exclusively in the health system. Anonymised data related to maternal and child hospital admissions were extracted from the CCDHB Patient Information Management System (PIMS) by the CCDHB database manager.
Maternal age, education, ethnicity, smoking, alcohol and substance use at time of the woman registering with a lead maternity carer (LMC) was obtained from the PIMS dataset, and indicated whether the woman had smoked, taken alcohol or substances other than tobacco during pregnancy. Maternal ethnicity in the New Zealand healthcare system is based on self-reported ethnicity, and was classified in line with New Zealand Census guidelines, on prioritised ethnicity, with variant of Indian as separate category (Ministry of Health 2013). Maternal ethnicity was grouped NZM, NZE, Pacific, Asian, Indian, MELAA and Other.
Access to Secondary Mental Health Services
Data regarding access to secondary mental health services were sourced from the Mental Health Information National Collection (MHINC, which covered the period between 2001 and 2008). This collection includes information pertaining to secondary care in inpatient, outpatient and community settings provided by the DHB; when the service was accessed (activity start date) and primary function of the healthcare team (team type) (Ministry of Health).
Data Matching
Maternal and infant data from PIMS were matched to the MHINC collection using maternal NHI numbers. Access to secondary mental health services was defined as at least one contact with secondary mental health services, as some women had multiple contacts.
Access to secondary mental health services during the pregnancy and post-partum period, which was defined for the antenatal period and for up to 1 year post-birth as the time between gestation at 0 weeks (defined relative to recorded gestational age at birth) and delivery date plus 365 days (up to and including 365 days).
In order to estimate a prior history/previous contact with secondary mental health services, access prior to pregnancy was determined by assessing whether there was an activity start date (in MHINC) within the 6 months prior to gestation (defined as 0 weeks, relative to gestation at birth).
Mental Health Conditions and Primary Diagnosis
Mental health conditions were grouped according toICD9 v1 diagnostic codes for the primary diagnosis. For example, the group we present as “bipolar and depressive psychosis” contains 40 different ICD9 codes/mental health conditions including 296.00—Bipolar I disorder, single manic episode, unspecified; and 296.23—Major depressive affective disorder, single episode, severe, without mention of “psychotic behavior”. Information pertaining to the primary diagnosis during pregnancy and the post-natal period was explored by assessing the primary diagnoses recorded in this period.
Analysis
Poisson regression was used to explore rate of access, at least one contact to secondary mental health services, associated with pregnancies of NZM, Pacific, Asian, Indian and MELAA women compared to NZE women, by age (<20 and 21–30 compared to women over the age of 30). Smoking, alcohol and substance use during pregnancy were also explored as independent risk factors associated with access. Rates of access to mental health services are reported as rates per 1000 pregnancies. The numerator is one contact with secondary mental health services during pregnancy and up to 1 year post-delivery. The denominator is the corresponding number of pregnancies in the PIMS dataset. A more in-depth statistical investigation (multivariate) was not possible for this study given the relatively small proportion of pregnancies associated with access to secondary mental health services (n = 736). Descriptive statistics, including 95 % confidence intervals are also reported when appropriate. These data were calculated with SAS® Enterprise Guide (version 6.1 SAS Institute Inc., Cary, NC, USA).
Ethical Approval
Ethical approval for the study was granted by the New Zealand Health and Disability Ethics Committee (NZ/1/CD7404).
Results
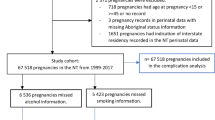
Figure 1 describes the data matching process for MHINC mental health collection with the CCDHB PIMS cohort. Between 1st July 2001 and 30th June 2008 there were 20,465 individual women, representing 27,153 pregnancies in the CCDHB cohort (PIMS data). During the corresponding time period there were 2046 individual women recorded in the MHINC dataset, representing 80,757 contacts with the various mental health service teams.
Access to Secondary Mental Health Services
27.1 per 1000 pregnancies (736/27,153) were associated with access to secondary mental services. Maternal characteristics of the women matched in the PIMS-MHINC datasets and who had at least one contact with secondary mental health services during pregnancy and for up to 1 year post-delivery are described in Table 1. Increased parity (2nd and 3rd delivery event) appeared to be associated with an increase access to service for NZM women and (>5 delivery events) for NZE women. Indication of being a smoker and substance user appeared higher for NZE women accessing services than NZM women.
Differences in access by ethnicity adjusted for age profile showed that Pacific, Asian, Indian MELAA and other ethnicities had significantly lower rates of access to services compared to NZE women (Table 2). NZM did not have significantly higher rates of access than NZE. Exploring age, independent of ethnicity showed that younger age was strongly associated with higher rates of access to secondary mental health services, with 80 % higher risk of accessing services with mothers under the age of 20. Smoking, using alcohol and substance use during pregnancy were strongly associated with access with access to secondary mental health services (Table 2); in particular substance use, representing a three and half times rate of likelihood of access than those women who did not use substances other than tobacco during pregnancy.
Access to secondary mental health services largely occurred in the post-natal period 75 % of the 736 pregnancies associated with access; and the number of contacts with services varied, with 10 contacts accounting for 50 % of the cumulative total (data not shown). 11 % women (163/1392) were not recorded as accessing secondary mental health services either 6 months before pregnancy or up to 12 months after delivery.
Care teams were more varied with younger mothers with some differences observed by ethnicity. For example, in NZE women under the age 20 care was provided most by the maternal mental health team (41 %), community team (27 %), youth specialty team (17 %) and alcohol and drug team (8 %). For NZM women under the age 20 care was provided most by the maternal mental health team (34 %), Kaupapa Māori team (20 %) and youth specialty team (8 %) and inpatient team (8 %). For pregnancies in women over the age of 21 care was most provided through the maternal mental health team (50–85 %), 15 to 25 % services provided by the community mental health team, Kaupapa Māori team provided comparable amount of service to NZM women over the age of 21 (20 %).
Mental Health Conditions
After “Other” diagnosis (which includes diagnosis not recorded or deferred e.g. V71.09—observation for other suspected mental condition); the next common primary diagnoses were associated with bipolar and depressive psychosis, drug related mental conditions and acute stress (Table 3). Many women had more than one primary diagnosis. There did not appear to be a difference in diagnosis by ethnicity.
Discussion
The findings from this descriptive retrospective cohort study indicated that in 27 of every 1000 pregnancies, the mother accessed secondary mental health services. Broadly taken, of the 60,000 pregnancies each year in New Zealand, 1600 (approximately 3 %) of them would require maternal access to secondary mental services, however—our findings are based on those women already accessing services, and therefore could reflect the system’s capacity, rather than the actual need for access services, which is likely to be much higher. Our results also indicated that for some women (11 %) who had accessed secondary mental health services, that they had not accessed services leading up to a pregnancy or for 1 year after delivery. The reasons for these “lost” women are not known, it is possible that these women are being cared for by primary health care services and no longer have a need for secondary level care; elucidating why this is happening would warrant further investigation given the high rates of maternal suicide in New Zealand (Baxter 2007; PMMRC 2012), and also as means to improve advocacy and care for women with moderate to severe mental health conditions (Megnin-Viggars et al. 2015). It is pertinent at this stage to raise that there is an emerging evidence base highlighting potential barriers in accessing mental health services, in particular screening for mental health concerns, as partner, friends or family telling them that their emotions were ‘normal’; desiring to handle their mood problems on their own; preferring to discuss feelings with their significant others; and not knowing what emotions are ‘normal’ or ‘not normal’ during pregnancy (Kingston et al. 2015).
Most women in our cohort had more than one contact with service providers (in most cases, the maternal mental health team). Access to service mostly occurred in the post-natal period with a non-specific mental health condition being associated with access. This “Other” group due to sheer size is likely to be the most “relevant” category as it would cover not chronic, highly impairing mental illness. Bipolar and depressive psychosis and acute stress associated conditions were indicated as leading diagnoses for women in our cohort, which are known mental health conditions associated with pregnancy, but at <35 % combined total ascribed, were not the major conditions associated with access. These data likely reflect the complexity in ascribing mental health diagnoses; and that using diagnosis data as means to informing service usage is probably less useful than contact information.
Access to services was substantially higher in pregnant/post-partum women under the age of 20 (Reid and Meadows-Oliver 2007) and access to service appeared to be associated with alcohol, smoking and substance the latter being higher NZE women. Our data indicate that access rates have been comparable for both NZM and NZE women. However, we would have expected this rate to be higher amongst Māori women given the reported high needs of mental health services for this group (Baxter 2007). Access to services for Pacific and Asian women was low, and may represent an area of unmet need and would warrant further investigation given the increasing population in New Zealand and assessment of culturally appropriate services for these women (Waldie et al. 2015). It is also possible that lower access for these women reflects cultural aspects of support, as seen with Pacific families offering a positive influence in promoting abstinence or responsible drinking for young people (Suaalii-Sauni et al. 2012).
In terms of informing service provision for women needing access to secondary mental health services, our data suggests young age and substance use are strong indicators of service use. There is compelling evidence that young women under the age of 20 are engaging early in their pregnancy with primary health carers, but that they experience delays in accessing antenatal care (Makowharemahihi et al. 2014). Our data suggest that the same may be happening for access to secondary mental health services, but would need further investigation. The antenatal period could provide a window of opportunity for maternity carers to discuss mental health matters and navigate care to appropriate providers in order for timely access to services in the event of care being needed; however assessment of service need will likely require health professionals to be educationally prepared in order to deliver the assessment/care that is empathetic and sensitive to women who are disclosing personal information, as highlighted by Rollans et al. (2013).
Study Limitations
This is a descriptive study and as such we cannot draw any definitive associations between pregnancy and the onset of episodes of poor mental health. This study is based around the antenatal and post-natal period and although we have constructed variables to explore the access to secondary services prior to the corresponding pregnancy we do not have prior mental health history. MHINC data does not include referral dates, but its successor PRIMHD does, and further studies could explore timely access and/or utility of clinical diagnosis to services.
To our knowledge this is the first study in New Zealand, and one of the few international studies (for example Riordan et al. 2012), that has used linked data to explore access to secondary mental health services during and after pregnancy. Our data has indicated a high level of access to services during pregnancy particularly for women under the age of 20, and areas of possible unmet need, for example in Pacific and Asian women, where access to services was very low. Furthermore our data suggests that women with a history of accessing services are not accessing services during pregnancy, a time when episodes of poor mental health are more likely to recur (Megnin-Viggars et al. 2015; Ministry of Health 2011).
References
Austin, M. P. (2003). Perinatal mental health: Opportunities and challenges for psychiatry Australasian. Psychiatry, 11, 399–403.
Baxter, J. (2007). Mental health: Psychiatric disorder and suicide. In: B. Robson & R. Harris (Eds.), Hauora: Māori Standards of Health IV. Wellington: Te Rōpū Rangahau Hauora a Eru Pōmare.
Filoche, S. K., Garrett, S., Stanley, J., Rose, S., Robson, B., Elley, C. R., & Lawton, B. (2013). Wāhine hauora: Linking local hospital and national health information datasets to explore maternal risk factors and obstetric outcomes of New Zealand Māori and non-Māori women in relation to infant respiratory admissions and timely immunisations. BMC Pregnancy and Childbirth, 13, 145.
Kingston, D., Austin, M.-P., Heaman, M., McDonald, S., Lasiuk, G., Sword, W., Giallo, R., et al. (2015). Barriers and facilitators of mental health screening in pregnancy. Journal of Affective Disorders, 186, 350–357. doi:10.1016/j.jad.2015.06.029.
Makowharemahihi, C., Lawton, B. A., Cram, F., Ngata, T., Brown, S., & Robson, B. (2014). Initiation of maternity care for young Māori women under 20 years of age. The New Zealand Medical Journal, 127(1393), 52–61.
Marcus, S. M. (2009). Depression during pregnancy: Rates, risks and consequences—Motherisk update 2008. The Canadian Journal of Clinical Pharmacology, 16, e15–e22.
Megnin-Viggars, O., Symington, I., Howard, L. M., & Pilling, S. (2015). Experience of care for mental health problems in the antenatal or postnatal period for women in the UK: A systematic review and meta-synthesis of qualitative research. Archives of Womens Mental Health. doi:10.1007/s00737-015-0548-6.
Ministry of Health. (2011). Healthy beginnings: Developing perinatal and infant mental health services in New Zealand. Wellington: Ministry of Health.
Ministry of Health. (2013). Ethnicity data protocols for the health and disability sector. Wellington: Ministry of Health.
Ministry of Health Programme for the Integration of Mental Health Data (PRIMHD) data dictionary and datamart diagram.
PMMRC. (2012). Sixth annual report of the Perinatal and Maternal Mortality Review Committee: Reporting mortality 2010. Health Quality and Safety Commission 2012: Wellington.
Reid, V., & Meadows-Oliver, M. (2007). Postpartum depression in adolescent mothers: An integrative review of the literature. Journal of Pediatric Health Care, 21, 289–298. doi:10.1016/j.pedhc.2006.05.010.
Riordan, D. V., Morris, C., Hattie, J., & Stark, C. (2012). Family size and perinatal circumstances, as mental health risk factors in a Scottish birth cohort. Social Psychiatry and Psychiatric Epidemiology, 47, 975–983. doi:10.1007/s00127-011-0405-5.
Rollans, M., Schmied, V., Kemp, L., & Meade, T. (2013). Digging over that old ground: An Australian perspective of women’s experience of psychosocial assessment and depression screening in pregnancy and following birth. BMC Womens Health, 13, 18. doi:10.1186/1472-6874-13-18.
Schmied, V., Johnson, M., Naidoo, N., Austin, M. P., Matthey, S., Kemp, L., Mills, A., et al. (2013). Maternal mental health in Australia and New Zealand: A review of longitudinal studies. Women and Birth: Journal of the Australian College of Midwives. doi:10.1016/j.wombi.2013.02.006.
Suaalii-Sauni, T., Samu, K. S., Dunbar, L., Pulford, J., & Wheeler, A. (2012). A qualitative investigation into key cultural factors that support abstinence or responsible drinking amongst some Pacific youth living in New Zealand. Harm Reduction Journal 9, 36. doi:10.1186/1477-7517-9-36.
Waldie, K. E., Peterson, E. R., D’Souza, S., Underwood, L., Pryor, J. E., Atatoa Carr, P. E., Grant, C. C., et al. (2015). Depression symptoms during pregnancy: Evidence from growing up in New Zealand. Journal of Affective Disorders, 186, 66–73. doi:10.1016/j.jad.2015.06.009.
Acknowledgments
This research was funded in part by the Health Research Council and by a University of Otago Research Grant. The authors thank Karin Isherwood and Terry Smith for clinical and data input advice.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Filoche, S.K., Lawton, B. & Stanley, J. Access to Secondary Mental Health Services in a Cohort of New Zealand Mothers. Community Ment Health J 52, 964–971 (2016). https://doi.org/10.1007/s10597-016-0042-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-016-0042-2