Abstract
Adolescents referred to community behavioral health centers (CBHC) for substance use (SU) problems report high rates of child maltreatment. Although SU and maltreatment are independent risk factors for adolescent depression, few studies have examined their interactive effects. This study examined the interactive effects of SU (alcohol and marijuana) and exposure to different types of trauma on depressed mood among 74 adolescents referred to a CBHC for SU. Hierarchical regressions controlling for sex and common adolescent comorbidities showed that sexual abuse had a stronger relationship with depressed mood than other types of maltreatment. Although SU was not independently related to depressed mood, consistent with the self-medication hypothesis, increased SU was associated with lower levels of depressed mood among adolescents with greater exposure to sexual abuse. Results suggest that teens presenting to CBHCs for SU should be assessed for multiple forms of maltreatment and for depressed mood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescents presenting to community behavioral health centers (CBHC) for substance use (SU) treatment typically have a myriad of co-occurring problems that contribute to greater overall severity and worse health-related outcomes. One of the most common and serious co-occurring problems is a history of child maltreatment, defined as the experience of physical, emotional, or sexual abuse or physical or emotional neglect (Fletcher 2009; Ford et al. 2010; Shin et al. 2013). Although effects may vary by type of abuse or neglect (Hussey et al. 2006; Shin et al. 2013), a number of early studies documented consistently high rates of maltreatment among adolescents with SU problems (Clark et al. 1997; Hamburger et al. 2008; Harrison et al. 1997; see Keyes et al. 2012b for a review; Shin et al. 2013). In the Cannabis Youth Trial (CYT; Tims et al. 2002), the largest randomized trial of adolescents presenting to outpatient community SU treatment to date, 57 % of the 600 youth reported a lifetime history of maltreatment and 20 % reported that they had experienced maltreatment within the past 90 days. Adolescents in SU treatment with a history of maltreatment have elevated risk of a range of negative outcomes including greater frequency of substance abuse and greater risk of substance dependence (Clark et al. 1997). Of particular concern, both SU and child maltreatment have been found to be independent risk factors for symptoms of depression (Fletcher 2009), substance use and dependence (O’Neil et al. 2011), depression in young adulthood (Hussey et al. 2006; Needham 2007; Shin et al. 2013), and associated problems, such as self-injurious behavior and suicidality (Brown et al. 1999).
Despite the high prevalence of maltreatment among adolescents in community-based SU treatment and the increased risk of depression associated with both concerns, the interactive effects of maltreatment and SU on adolescent depression are not well understood. One of the primary limitations of past research is that studies have not assessed whether the joint effect of maltreatment and SU is associated with an exacerbation or dampening of depression symptoms (Harrison et al. 1997). An exacerbation of depression symptoms would suggest that the two issues have a negative, synergistic effect that is greater than the additive effects of each issue. A dampening of depression symptoms would suggest that the combination of maltreatment and SU is associated with a reduction in symptoms at least in the short-term. An interactive effect would be consistent with the self-medication hypothesis, (Khantzian 1985, 1997), i.e., adolescents with a history of maltreatment might turn to substance use as a means of reducing negative affect (Bonn-Miller et al. 2007; Harrison et al. 1997; Taylor 2011). This latter hypothesis has been supported by studies demonstrating that child maltreatment precedes the initiation of SU (Clark et al. 1997) but such studies have not been consistently replicated and have not specifically assessed depression symptoms as a means of elucidating the relationship.
Another limitation of prior research is failure to consider multiple forms of child maltreatment simultaneously even though these are differentially associated with acute and long-term negative adolescent outcomes (Hodgins et al. 2014; Hussey et al. 2006; Shin et al. 2013). Several longitudinal studies of adolescents suggest that sexual abuse in particular is associated with greater risk of depression than other forms of abuse (Brown et al. 1999; Fletcher 2009). Brown and colleagues (1999) assert that it is important to simultaneously assess for multiple forms of abuse and neglect because these forms of child maltreatment frequently co-occur and may have differential negative sequelae (Keyes et al. 2012a).
Along similar lines, prior studies have also not considered the influences of the two most commonly used substances among adolescents presenting to treatment: alcohol and marijuana (Swendsen et al. 2012). Most prior studies have either measured one of these substances (Bonn-Miller et al. 2007; Clark et al. 1997) or assessed a combined indicator of substance use (e.g., alcohol vs. illicit drug use) (Mangerud et al. 2014). This approach is not consistent with several cross-sectional and longitudinal studies indicating that the two substances have differential associations with depression (Degenhardt et al. 2013; Needham 2007). Studies also suggest that binge drinking in particular, defined as consuming five or more drinks in a row, may be particularly important to examine in this cohort, since binge drinking has been associated with both a history of maltreatment and with higher levels of depressed mood (Needham 2007).
A final limitation of prior studies has been a lack of control for psychiatric comorbidity, such as externalizing behaviors and anxiety that frequently co-occurs with maltreatment and SU (Hodgins et al. 2014). As noted by Keyes and colleagues (2012a), when studying the co-occurrence of maltreatment and SU it is important to account for psychiatric comorbidity because maltreatment is related to multiple psychiatric disorders (Green et al. 2010; Widom et al. 2007) and SU disorders are highly co-morbid with other forms of psychopathology (Kessler et al. 2012). It is especially important to account for symptoms of anxiety and disruptive behavior disorders (DBD), as these conditions frequently co-occur in adolescence, with adolescent depression and SU (Hodgins et al. 2014; Kessler et al. 2012; Merikangas et al. 2010), and among those with trauma histories (Whitson et al. 2012).
The goal of the current study is to evaluate the joint effect of maltreatment and SU on depressed mood in a sample of adolescents presenting for SU treatment in a CBHC. To address the aforementioned limitations of prior research, the current study: separately examines the relationship between SU and maltreatment for alcohol and marijuana; tests the effects of multiple forms of maltreatment concurrently, and controls for symptoms of anxiety and DBD. We focused on alcohol and marijuana because they are the two most common substances used by adolescents (Swendsen et al. (2012), and we focused on binge drinking in particular because of its association with increased trauma exposure and symptoms of depression (Needham 2007; Shin et al. 2009). In addition, we control for the effects of sex, since it is well established that rates of maltreatment, SU, and depression differ between boys and girls across both community and clinical samples (Fletcher 2009; Hodgins et al. 2014; Needham 2007; O’Neil et al. 2011).
Our approach is guided by two primary hypotheses based on prior literature. First, we expect the interaction of maltreatment and SU to have a significant dampening effect on depression symptoms, consistent with the self-medication hypothesis (Khantzian 1985, 1997). Second, we expect sexual abuse in particular to have stronger associations with depression symptoms than other types of child maltreatment (Brown et al. 1999).
Methods
Participants and Procedures
Participants were recruited from an outpatient program specifically for adolescents with comorbid mental health and substance use problems in a CBHC in the northeast region of the United States. All adolescents who began treatment in the program were invited to participate in the study; 74 out of 88 (84 %) agreed to participate. After written informed consent and assent were obtained from parents and adolescents respectively, an assessment battery was administered. The study was approved by the university human subjects’ protection committee.
Measures
Self-reported history of trauma exposure was measured by the Childhood Trauma Questionnaire (CTQ; Bernstein et al. 2003), a 28-item questionnaire made up of five subscales: emotional neglect, physical neglect, emotional abuse, physical abuse, and sexual abuse. Each subscale consists of five items rated on a likert-type scale ranging from 1 = “never true” to 5 = “very often true”. Reported reliability in multiple samples range from α = . 61 (physical neglect) to .94 (sexual abuse) (Bernstein et al. 2003). Cronbach’s alpha for this sample was α = .76.
Depressed mood was measured by the 21-item Beck Depression Inventory-II (BDI-II: Beck et al. 1996). The BDI is a widely used measure of symptoms associated with depressed mood experienced in the two weeks prior to baseline assessment and has shown high internal consistency (α = .87) among a group of substance using adolescents (Subramaniam et al. 2009). Each symptom is scored from 0 to 3, depending on absence or presence (severity) of the symptom. Higher scores reflect more severe depressed mood, with a score of 19 indicating a clinically elevated level.
The Child Behavior Checklist parent version (Achenbach and Rescorla 2001) was used to measure externalizing and anxiety symptoms. The CBCL is a widely used parent-report measure of behavioral and emotional problems for youth aged 6–18 that generates scale scores for internalizing (e.g., anxious, depressive, and overcontrol) and externalizing (e.g., aggressive, hyperactive, noncompliant, and undercontrolled) problems. To prevent redundancy with our focus on depression, we used only the anxiety subscale as the measure of internalizing problems and used the full externalizing scale to indicate externalizing problems. For each scale, t-scores of 65 or above indicate clinically significant impairment. The CBCL anxiety and externalizing scales have been found to have good reliability in large clinical samples of children and youth (alphas from .77 to .81) and have demonstrated the ability to differentiate between youth with and without anxiety as well as youth with anxiety and youth with externalizing disorders (Seligman et al. 2004; Nakamura et al. 2009).
Self-reported binge-drinking frequency was assessed using an item from the Adolescent Drinking Questionnaire (ADQ; Jessor et al. 1989), which rated frequency of binge drinking over the past month on a scale from 1 (Did not binge drink) to 8 (Everyday). Days of MJ use over the prior 3 months was measured using the Timeline Follow Back Interview (Sobell and Sobell 1995), a retrospective assessment of substance use that has shown satisfactory reliability and validity across numerous studies (see Sobell and Sobell 2003 for a review). Possible answers ranged from 0 to 90 days.
Data Analysis
Preliminary analyses examined whether the key study variables (e.g., binge drinking and marijuana use frequency, CTQ scales, CBCL, and BDI scores) differed as a function of demographic variables (e.g., sex, age, race, ethnicity) to determine which covariates to retain in the analysis.
Two hierarchical regression analyses (one for binge drinking frequency and one for MJ frequency) were conducted to explore the main and interactive effects of substance use frequency and traumatic exposure frequency on adolescent BDI scores. In step one, the key covariates - sex and the CBCL subscales (anxiety and externalizing behavior) - were entered. In step two, the five CTQ scales and substance use frequency (binge drinking or MJ) were entered to determine their main effects on BDI. To optimize model fit, backwards elimination with a criterion of p < .20 was used to sequentially remove CTQ dimensions until the most parsimonious model was obtained. Interaction variables between the remaining CTQ dimensions and the substance use variable (e.g., CTQ dimension X binge drinking or marijuana) were entered in the third and final step.
As recommended by Holmbeck (2002), all variables were centered to reduce multicollinearity between the main effect and interaction terms. Significant interactions were probed using simple slopes, consistent with the recommendations of Aiken and West (1991). Specifically, significant interactions predicting BDI were interpreted by plotting simple regression lines at one standard deviation above and below the mean of the moderator. Version 22 of the Statistical Package for the Social Sciences (SPSS) was employed for all analyses.
Results
Sample Characteristics
Demographic and clinical characteristics of the final sample of 74 adolescents are presented in Table 1. In general, the sample reported subclinical BDI and CBCL anxiety scores; CBCL externalizing scores were in the clinical range. Participants reported low levels of binge drinking frequency over the 90 days prior to baseline (Median category = less than once per month, range from never to 4–6 times per week), and moderate levels of MJ use frequency (M = 33.1 days, SD = 36.06, range from 0 to 90 days); there was representation across the full range of substance frequency. Relative to boys, girls reported higher levels of depressed mood (M = 16.3, SD = 12.53 vs. 10.8, SD = 9.13, t = 2.17, p < .05), and greater frequency of physical abuse (M = 8.72, SD = 4.72 vs. 6.84 SD = 3.00, t = 2.02, p < .05), emotional abuse (M = 13.15, SD = 6.01 vs. 9.77, SD = 4.40, t = 2.71, p < .01) and sexual abuse (M = 8.35, SD = 6.24 vs. 5.23, SD = 1.22, t = 3.23, p < .01). No differences were found between boys and girls on any of the other variables, and no differences were found on any of the key study variables as a function of age or race/ethnicity. Thus, sex was the only demographic covariate included in the regressions.
Regression Analyses
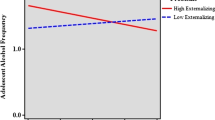
The first hierarchical regression examined the main and interactive effects of trauma frequency and binge drinking frequency on BDI. In Step 1, there were significant effects for sex (β = .27, t = 2.53, p < .05) and both CBCL subscales (Externalizing β = −.32, t = −2.70, p < .01; Anxiety β = .47, t = 4.01, p < .001). In Step 2, two of the five CTQ variables remained after backwards elimination and both had significant main effects on BDI: Sexual abuse, (β = .27, t = 2.34, p < .05) and Emotional neglect (β = .24, t = 2.18, p < .05). Binge drinking frequency did not have a significant main effect on BDI (β = .01, t = −.07, p > .05). In the third step of the model there was a significant sexual abuse x binge drinking interaction effect (β = −.28, t = −2.70, p < .01). The interactive effect of emotional neglect X binge drinking was not significant and model comparisons using the F-change test indicated that removing this term improved model fit. The final model is depicted in Table 2 and accounted for 45 % of the variance in BDI scores.
Figure 1 depicts the simple slope analysis of the binge drinking by sexual abuse interaction for those one standard deviation (SD) above and below the CTQ sexual abuse mean. As depicted in the figure, for those one SD below the mean, as binge-drinking frequency increased, the level of BDI symptoms increased (β = 1.87, t = .20, p > .05). By contrast, yet consistent with our expectations, for those one SD above the mean, as binge drinking frequency increased the level of BDI symptoms decreased (β = −.95, t = −.11, p > .05). Of note, the interaction was significant, but the coefficients in the simple slope regressions were not, indicating that the two simple slopes were significantly different from each other, even though independently neither of the slopes was significantly different than zero.
The second hierarchical regression tested the main and interactive effects of trauma frequency and MJ frequency on BDI. Step 1 was identical to the model for binge drinking frequency and the results were the same. In Step 2, two of the five CTQ variables again remained and were significant: Sexual abuse (β = .27, t = 2.40, p < .05) and Emotional neglect (β = .24, t = 2.28, p < .05). Marijuana frequency did not have a significant main effect on BDI scores (β = .03, t = .26, p > .05). In Step 3, the MJ use × sexual abuse interaction term was significant (β = −.33, t = −3.24, p < .01). Similar to the binge-drinking model, the MJ use X emotional neglect interaction term was not significant and dropping it improved model fit. The final regression model is depicted in Table 3 and accounted for 47 % of the variance in BDI scores.
Figure 2 depicts the simple slope plots of the marijuana by sexual abuse interaction for those one SD above and below the CTQ sexual abuse exposure mean. As shown in the figure, the pattern of results was similar to that found for binge drinking. For those one SD below the mean, as marijuana frequency increased, BDI scores increased (β = .10, t = .12, p > .05). By contrast, yet consistent with our hypotheses and the self-medication hypothesis, for those one SD above the mean, as marijuana frequency increased, the BDI scores decreased (β = −.10, t = .12, p > .05). Similar to the analysis for binge drinking, the slopes of the simple regression lines were significantly different from one another, even though neither was significantly different from zero.
Discussion
Results of this study provide mixed support for our hypotheses. Consistent with our expectations, specific forms of trauma exposure were independently related to depressed mood above and beyond the effects of behavior problem and anxiety symptoms, with sexual abuse having the most significant effect followed by emotional neglect. Our results are partially consistent with the findings of the Adolescent Health Study (Fletcher 2009), which showed that sexual abuse increased the odds of being depressed in adolescence for both boys and girls, although in that study physical abuse and not emotional neglect were independently related to depressed mood. Brown et al. (1999), however, found that sexual abuse increased the odds of depression over physical abuse or neglect (emotional and physical). When combined with prior literature, our results demonstrate the importance of examining the effects of specific forms of child maltreatment and controlling for other common emotional and behavioral problems (Keyes et al. 2012a).
As expected, girls reported higher levels of depression than boys, as well as a history of abuse, which is consistent with findings in the literature indicating that both abuse and depression are more likely among girls than they are among boys (Brown et al. 1999; Clark et al. 1997; Hodgins et al. 2014; Kessler et al. 2012; Needham 2007). Contrary to our expectations, neither binge drinking nor MJ use was independently related to depressed mood after accounting for abuse history, and behavior problem and anxiety symptoms. This finding adds to the literature as prior studies reporting a relationship between binge drinking or marijuana use and depression did not take into account these relevant factors (Needham 2007), yet the clinical reality is that these tend to co-occur (Kessler et al. 2012; Mangerud et al. 2014) especially among those with a trauma history (Hodgins et al. 2014).
In support of our hypotheses, and consistent with the self-medication hypothesis (Khantzian 1985, 1997), there was an interactive effect between sexual abuse and two types of substance use (both binge drinking and marijuana use), after controlling for sex, externalizing behaviors and anxiety: at higher levels of sexual abuse exposure, higher levels of substance use were associated with lower depressed mood. This is consistent with the literature suggesting that sexual abuse, in particular, is associated with binge-drinking and marijuana use (Shin et al. 2009; Tims et al. 2002). Our results are also consistent with past research indicating that adolescents with an abuse history use substances in order to self-regulate and deal with distress (Bonn-Miller et al. 2007; Harrison et al. 1997; Shin et al. 2012; Taylor 2011; Vilhena-Churchill and Goldstein 2014), although our data supported this relationship only for sexual abuse and not for other types of abuse. Of note, the interactive effects between SU and sexual abuse must be interpreted with caution, as the slopes of the simple regression lines were not significant, although the interactions were. Our ability to detect significant simple slopes may have been limited by our small sample; replication in larger samples is warranted.
Several limitations of this study should be noted. First, due to the cross-sectional nature of the study we cannot make causal claims regarding the relationship among depressed mood, traumatic experiences and substance use. While it is plausible that teens employed substance use as a way to cope with trauma-related distress or sequelae, it is also possible that substance use led directly to higher frequency of trauma exposure through, for example, increased involvement in high-risk situations or poor decision-making. Future studies should employ longitudinal designs in order to delineate the temporal order of these relationships. The generalizability of the results is also constrained by the sample, which had modest levels of substance use, sub-clinical symptoms of depression and anxiety, but clinical levels of disruptive behaviors. It is not known whether a similar relationship among the variables would be found among adolescents with different symptom profiles.
Notwithstanding these limitations, this study advances our knowledge by demonstrating that trauma exposure and substance use have an interactive effect on symptoms of depressed mood among adolescents presenting for substance use treatment at a CBHC. Thus, results of our study highlight the clinical utility of assessing for binge drinking and marijuana use among adolescents with a history of child maltreatment, as well as the value of assessing for a maltreatment history among those who abuse substances as these variables may interact in a manner that maintains or reinforces symptoms over time.
References
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families.
Aiken, L. S., & West, S. G. (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the beck depression inventory-II. San Antonio, TX: Psychological Corporation.
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., et al. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect, 27, 169–190.
Bonn-Miller, M. O., Vujanovic, A. A., Feldner, M. T., Bernstein, A., & Zvolensky, M. J. (2007). Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event-exposed marijuana users. Journal of Traumatic Stress, 20, 577–586.
Brown, J., Cohen, P., Johnson, J. G., & Smailes, E. M. (1999). Childhood abuse and neglect: Specificity and effects on adolescent and young adult depression and suicidality. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1490–1496.
Clark, D. B., Lesnick, L., & Hegedus, A. M. (1997). Traumas and other adverse life events in adolescents with alcohol abuse and dependence. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1744–1751.
Degenhardt, L., Coffey, C., Romaniuk, H., Swift, W., Carlin, J. B., Hall, W. D., & Patton, G. C. (2013). The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. Addiction, 108, 124–133.
Fletcher, J. M. (2009). Childhood mistreatment and adolescent and young adult depression. Social Science and Medicine, 68, 799–806.
Ford, J. D., Elhai, J. D., Connor, D. F., & Frueh, B. C. (2010). Poly-victimization and risk of posttraumatic, depressive, and substance use disorders and involvement in delinquency in a national sample of adolescents. Journal of Adolescent Health, 46, 545–552.
Green, J. G., McLaughlin, K. A., Berglund, P., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2010). Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication (NCS-R) I: associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 62, 113–123.
Hamburger, M. E., Leeb, R. T., & Swahn, M. H. (2008). Childhood maltreatment and early alcohol use among high-risk adolescents. Journal of Studies on Alcohol and Drugs, 69, 291–295.
Harrison, P. A., Fulkerson, J. A., & Beebe, T. J. (1997). Multiple substance use among adolescent physical and sexual abuse victims. Child Abuse and Neglect, 21, 529–539.
Hodgins, S., Lövenhag, S., Rehn, M., & Nilsson, K. W. (2014). A 5-year follow-up study of adolescents who sought treatment for substance misuse in Sweden. European Child and Adolescent Psychiatry, 23, 347–360.
Holmbeck, G. N. (2002). Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology, 27, 87–96.
Hussey, J. M., Chang, J. J., & Kotch, J. B. (2006). Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics, 118, 933–942.
Jessor, R., Donovan, J. E., & Costa, F. M. (1989). Health Behavior Questionnaire. Boulder, CO: University of Colorado.
Kessler, R. C., Avenevoli, S., Costello, E. J., Georgiades, K., Green, J. G., Gruber, M. J., et al. (2012). Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry, 69, 372–380.
Keyes, K. M., Eaton, N. R., Krueger, R. F., McLaughlin, K. A., Wall, M. M., Grant, B. F., & Hasin, D. S. (2012a). Childhood maltreatment and the structure of common psychiatric disorders. The British Journal of Psychiatry, 200, 107–115.
Keyes, K. M., Hatzenbuehler, M. L., Grant, B. F., & Hasin, D. S. (2012b). Stress and alcohol: Epidemiologic evidence. Alcohol Research Current Reviews, 34, 391–400.
Khantzian, E. J. (1985). The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry, 142, 1259–1264.
Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review Of Psychiatry, 4, 231–244.
Mangerud, W. L., Bjerkeset, O., Holmen, T. L., Lydersen, S., & Indredavik, M. S. (2014). Smoking, alcohol consumption, and drug use among adolescents with psychiatric disorders compared with a population based sample. Journal of Adolescence, 37, 1189–1199.
Merikangas, K. R., He, J., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., et al. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49, 980–989.
Nakamura, B. J., Ebesutani, C., Bernstein, A., & Chorpita, B. F. (2009). A psychometric analysis of the Child Behavior Checklist DSM-Oriented Scales. Journal of Psychopathology and Behavioral Assessment, 31, 178–189.
Needham, B. L. (2007). Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Social Science and Medicine, 65, 1166–1179.
O’Neil, K. A., Conner, B. T., & Kendall, P. C. (2011). Internalizing disorders and substance use disorders in youth: Comorbidity, risk, temporal order, and implications for intervention. Clinical Psychology Review, 31, 104–112.
Seligman, L. D., Ollendick, T. H., Langley, A. K., & Baldacci, H. B. (2004). The utility of measures of child and adolescent anxiety: A meta-analytic review of the Revised Children’s Manifest Anxiety Scale, the State-Trait Anxiety Inventory for Children, and the Child Behavior Checklist. Journal of Clinical Child and Adolescent Psychology, 33, 557–565.
Shin, S., Edwards, E., & Heeren, T. (2009). Child abuse and neglect: Relations to adolescent binge drinking in the national longitudinal study of Adolescent Health (AddHealth) Study. Addictive Behaviors [serial online]., 34, 277–280.
Shin, S. H., Hong, H. G., & Wills, T. A. (2012). An examination of pathways from childhood maltreatment to adolescent binge drinking. The American Journal on Addictions, 21, 202–209.
Shin, S. H., Miller, D. P., & Teicher, M. H. (2013). Exposure to childhood neglect and physical abuse and developmental trajectories of heavy episodic drinking from early adolescence into young adulthood. Drug and Alcohol Dependence, 127, 31–38.
Sobell, L., & Sobell, M. B. (1995). Alcohol timeline followback user’s manual. Toronto: Addiction Research Foundation.
Sobell, L. C., & Sobell, M. B. (2003). Alcohol consumption measures. In P. Allen & V. B. Wilson (Eds.), Assessing alcohol problems: A guide for clinicians and researchers (2nd ed., pp. 75–99). Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism.
Subramaniam, G., Harrell, P., Huntley, E., & Tracy, M. (2009). Beck Depression Inventory for depression screening in substance-abusing adolescents. Journal of Substance Abuse Treatment, 37, 25–31.
Swendsen, J., Burstein, M., Case, B., Conway, K. P., Dierker, L., He, J., & Merikangas, K. R. (2012). Use and abuse of alcohol and illicit drugs In US adolescents: Results of the National Comorbidity Survey-Adolescent Supplement. Archives of General Psychiatry, 69, 390–398.
Taylor, O. D. (2011). Adolescent depression as a contributing factor to the development of substance use disorders. Journal of Human Behavior in The Social Environment, 21, 696–710.
Tims, F. M., Dennis, M. L., Hamilton, N., Buchan, B. J., Diamond, G., Funk, R., & Brantley, L. B. (2002). Characteristics and problems of 600 adolescent cannabis abusers in outpatient treatment. Addiction, 97(Supplement 1), 46–57.
Vilhena-Churchill, N., & Goldstein, A. L. (2014). Child maltreatment and marijuana problems in young adults: Examining the role of motives and emotion dysregulation. Child Abuse and Neglect, 38, 962–972.
Whitson, M. L., Connell, C. M., Bernard, S., & Kaufman, J. S. (2012). An examination of exposure to traumatic events and symptoms and strengths for children served in a behavioral health system of care. Journal of Emotional And Behavioral Disorders, 20, 193–207.
Widom, C. S., DuMont, K., & Czaja, S. J. (2007). A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry, 64, 49–56.
Conflict of interest
Authors have no conflicts of interest. This study was approved by the University’s IRB.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gomez, J., Becker, S., O’Brien, K. et al. Interactive Effect of Child Maltreatment and Substance Use on Depressed Mood Among Adolescents Presenting to Community-Based Substance Use Treatment. Community Ment Health J 51, 833–840 (2015). https://doi.org/10.1007/s10597-015-9894-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-015-9894-0