Abstract
Transitional housing programs aim to improve living skills and housing stability for tenuously housed patients with mental illness. 113 consecutive Transitional Housing Team (THT) patients were matched to 139 controls on diagnosis, time of presentation, gender and prior psychiatric hospitalisation and compared using a difference-in-difference analysis for illness acuity and service use outcomes measured 1 year before and after THT entry/exit. There was a statistically significant difference-in-difference favouring THT participants for bed days (mean difference in difference −20.76 days, SE 9.59, p = 0.031) and living conditions (HoNOS Q11 mean difference in difference −0.93, SE 0.23, p < 0.001). THT cost less per participant (I$14,024) than the bed-days averted (I$17,348). The findings of reductions in bed days and improved living conditions suggest that transitional housing programs can have a significant positive impact for tenuously housed patients with high inpatient service usage, as well as saving costs for mental health services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients with severe and persistent mental illness (SPMI) (Siskind et al. 2012a) are more likely than the general population to be homeless (Folsom et al. 2005). Thirteen percent of a community sample of patients with SPMI in Australia had experienced at least one period of homelessness in the previous 15 months (Harvey et al. 2012). Homelessness and mental illness are associated with increased rates of victimization (Larney et al. 2009), physical illness (Plumb 1997) and mortality (Babidge et al. 2001). Patients with SPMI have a number of risk factors for homelessness, including functional deficits, poor independent living skills and difficulty negotiating relationships with others such as landlords (Jablensky et al. 2000). They are often in a revolving door of admission, discharge to inadequate housing, non-engagement with community services, and preventable readmission (Folsom et al. 2005; North and Smith 1993).
The provision of housing without personalised support (Siskind et al. 2012b) is unlikely to be sufficient to allow patients with SPMI to remain in stable accommodation. It must be in combination with both adequate clinical treatment and the provision of support and living skills training if sustained housing tenure is to be achieved (Newman and Goldman 2008).
There are a wide range of supported accommodation models operating internationally, varying in terms of duration of tenure, patient characteristics, housing characteristics, and service characteristics (Siskind et al. 2013). To date, comparisons between program types have been hampered by a lack of definitional clarity.
Programs such as Test and Stein’s Program in Community Living (Test and Stein 1976) from Wisconsin have been running for more than 25 years, and assist patients to gain independent living skills, achieve stable housing and reduce extended hospitalisations. An evaluation of US Veterans Affairs time-limited transitional housing services found that 78 % of patients were stably housed after 12 months (McGuire et al. 2011), a rate comparable to that of permanent supported housing programs such as Housing First (Tsemberis et al. 2004).
In Queensland, Australia, a Transitional Housing Team (THT) was established in 2005 as part of a government response to homelessness among people with mental illness. The team provided time limited housing and intensive living skills training and support to clinically case managed patients. The service was publicly funded through Australia’s universal health care system. The Australian states fund general and psychiatric hospitals and community mental health services while the federally funded Medicare system covers visits to family physicians and community specialists, although a co-payment may be required. Health insurance may also be purchased for private sector treatment.
Although studies of transitional housing have suggested it can lead to stable housing, its efficacy in reducing time spent psychiatrically hospitalized has not been studied. Further, the relative costs to mental health services of providing transitional housing has not been examined. In this study, we compared total acute psychiatric inpatient days, problems with living conditions, illness acuity and emergency department presentations for a year before entry and a year after exit from THT with a matched comparison group drawn from neighbouring hospital district mental health services without a transitional housing program. We hypothesised that when compared to controls, THT participants would have greater reductions in psychiatric inpatient bed-days, greater improvements in living conditions, greater reductions in ED presentations and lower overall costs to the mental health service.
Methods
Setting
THT services were provided to two tertiary general hospital districts of Brisbane, with a catchment population of 750,000 residents. The total population of greater Brisbane is 2,150,000. Mental health services provided by all of the hospital districts in this study used state-wide models of care which includes an acute inpatient psychiatric unit, community based multi-disciplinary outreach clinical case management teams with a staff to patient ratio of approximately 1:25 (Harvey and Fielding 2003), an Assertive Community Treatment model team (Harvey et al. 2012), a psychiatric emergency department and a home based mobile acute crisis team (Hubbeling and Bertram 2012). Further details on mental health services in Queensland are available elsewhere (Harris et al. 2012; Siskind et al. 2012a).
THT Program Description
THT was based on the place-train model that houses patients first, and then provides support for independent living skills (Corrigan and McCracken 2005). Services varied according to patient’s needs and included specific living skills training such as cooking, shopping, diet, cleaning, laundry, and using public transport, as well as relapse prevention, crisis management and linkage to community service agencies. THT staff were based off-site and provided 12 h per week of in-reach support available over extended hours and weekends. Staff included occupational therapists, nurses and non-clinical support workers.
THT participants were provided with social housing for the duration of their time in the program, funded by the Queensland Department of Housing. Participants shared two bedroom apartments in geographically dispersed sites across the inner city suburbs. Patients were provided with assistance to identify permanent housing options prior to discharge from THT. The THT program had a planned 6-month duration, but could be briefly extended, if necessary, particularly if more time was needed to identify safe housing.
THT participants could enter the program directly from the community (a Step-Up from community care) or could be discharged from an acute psychiatric inpatient unit directly to THT housing (a Step Down from inpatient care). The program was targeted at adults with SPMI who were homeless or at risk of homelessness, and who were willing to engage in a rehabilitation program. Sobriety was not a prerequisite, but alcohol and substance use was not permitted in THT housing.
THT staff were employed by the public mental health service and co-located with the public mental health service. THT participants also received clinical case management as usual from the public mental health service, which included assessment, linkage with psychopharmacological services, monitoring and treatment planning from their geographical catchment continuing care team.
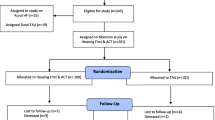
Study Design
This study used a retrospective quasi-experimental study comparing an intervention group to a control group. The intervention group were all THT program participants from two contiguous hospital districts who consecutively entered the program for the first time after 1 April 2006 and exited before 31 March 2009. Controls were drawn from two geographically adjacent hospital district mental health services that did not provide a transitional housing service. Both the intervention group and controls received similar clinical services from the public mental health districts. Length of stay for acute psychiatric hospitalization, 28-day readmission rates and staff full time equivalents per 100,000 population were broadly similar across all hospital district mental health services, as were the economic measures of the populations served.
Data Sources
The intervention group and controls were identified from a set of linked, de-identified, administrative datasets: Queensland Hospital Admitted Patient Data Collection (QHAPDC) which provided data on dates of admission and discharge, clinical diagnosis, age, gender, indigenous status, marital status; Consumer Integrated Mental Health Application (CIMHA) and Outcome Information System (OIS) which provided data on consumer outcome measures; and the Emergency Department Information System (EDIS) which provided data on presentations to emergency departments. Data were extracted on the intervention groups and controls for the year before the index date (defined as the date of admission for the hospitalization immediately preceding a participant’s first entry into THT for Step-Down patients, the date of first entry into THT for Step-Up patients, and the date of admission to hospital for controls), and for a year following the exit date (defined as the date a THT participant exited their first stay in THT accommodation, or the date a control was discharged from hospital).
Control Selection Process
A two-stage process was used to select controls. The variables to be used to match controls to the intervention group were gender, period of entry grouped into 6 half year time periods: 1 April to 30 September and 1 October to 31 March; diagnosis, in three categories: psychosis (ICD 10 codes F20-29); affective disorders (F30-39); and other disorders (including anxiety (F40-43, personality disorders (F60), pervasive developmental disorders (F84) and substance use disorders (F10-19)); and psychiatric admission in the prior year. In the first stage, under the terms of our ethics application, the data custodian provided the authors with a de-identified list of all patients with an admission to the neighbouring hospitals from 1 April 2006 to 30 March 2009, with information only on gender, diagnosis and date of admission. This list comprised all potential controls. Using SPSS version 20, THT participants were randomly matched to up to 4 controls on index date, gender and diagnosis category to create a control group pool. Each control had to match the THT participant exactly on index date, gender and diagnosis category. If there were more matched controls than required for THT participants with the same three criteria, a maximum of four controls were selected at random for each THT participant. Each control could only be selected once.
In stage 2, the data custodian provided data on clinical diagnosis; acute psychiatric hospitalisations; Health of the Nation Outcome Scale (HoNOS); and emergency department encounters for THT participants and the pool of controls. An enriched sub-group of controls was randomly selected from the control group pool so as to contain the same proportion of persons with at least one admission in the year prior to the index date as did the THT participant group. All further analyses were conducted using this enriched control sub-group, hereafter referred to as the controls.
Measures Used
The combined data extract included information on: clinical diagnosis; acute psychiatric hospitalisations; Health of the Nation Outcome Scale (HoNOS); and emergency department encounters. HoNOS was developed by the British Royal College of Psychiatrists, for monitoring mental health outcomes in routine clinical practice (Wing et al. 1998). The instrument has 12 items. Extensive routine use of this instrument indicates that it is simple to use, applicable to a wide range of psychotic and non-psychotic disorders, covers clinical and social functioning, acceptable to clinicians, sensitive to change and reliable in studies in several countries including the UK (Bebbington et al. 1999), Canada (Kisely et al. 2007) and Australia (Pirkis et al. 2005).
We used the highest HoNOS rating during each time period, as multiple HoNOS ratings could be available for a given patient in each time period. The total HoNOS score was used as a measure overall illness acuity. Higher scores indicate higher acuity. Of the individual items, question two (Q2) measures non-accidental self harm, question three (Q3) measures substance abuse and question 11 (Q11) measures problems with living conditions. The individual questions are rated 0–4, with scores of 2 and above considered to be clinically significant (Burgess et al. 2009). Dichotomizing the scores for the individual questions to below two versus two or above allowed the calculation of rates of clinically significant problems.
Hospital bed-days in the year before the index date and the year after exit were calculated as the cumulative number of nights spent in psychiatric hospitalisation in the year before entry and the year after exit. The measure of emergency department (ED) presentations was the total number of presentations to ED for any condition in the year before the index date and the year after exit.
Statistical Analysis
THT Participants Compared to Controls
For the year prior to the index date, demographic, service utilisation and clinical characteristics of THT participants versus controls were compared using t tests, χ2, or Mann–Whitney U tests, as appropriate.
A difference-in-difference analysis was undertaken to compare THT participants and controls on each measure of outcome (Gilmer et al. 2009). A difference-in-difference study design uses a two-part model to compare change in outcomes for the year before entry to the year after exit between THT participants and controls. The first step calculated the change in outcome measures over time. The value for each measure of outcome for each individual for the year before the index date was deducted from the value of the measure of outcome in the year after exit to create a difference-in-outcome variable. Difference-in-outcome variables were calculated separately for the THT participant group and the control group. In the second step, the mean difference-in-outcome variable was compared between participant and control groups using t tests.
Outcomes examined were mean bed-days, ED presentations, and HoNOS measures of illness acuity, suicidal ideation, substance abuse, and problems with living conditions. For example, the number of inpatient bed-days for the year prior to the index date and the year after exit were calculated for THT participants and controls. Bed-days in the year before the index date were deducted from bed-days in the year after exit to create a difference-in-bed-days variable. The difference-in-bed-days for THT participants was compared to the difference-in-bed-days for controls using a t test. This process was repeated for each outcome of interest.
An advantage of a difference-in-difference analysis is that it takes into account differences in baseline scores, and creates a more symmetrically distributed variable for comparison between the intervention and control groups.
To account for the differences between the control and intervention groups, a regression adjusted analysis of the difference-in-difference, accounting for the effects of age, pre-program bed-days and total HoNOS score was conducted using a linear regression model. Change in bed-days was also adjusted for additional re-entries into THT.
Since the THT participants had, on average, appreciably more bed-days in the year prior to the index date than controls, regression to the mean could be postulated as accounting for the greater absolute reduction in mean bed-days in favour of the THT group. Two methods were used to explore this possibility. Firstly a mean percentage change in bed-days for the THT participants and controls was calculated by dividing the mean difference-in-bed-days by the mean bed-days in the year before the index date. The standard error of the difference of the log of the ratios was calculated to test significance. Secondly, a difference-in-difference sub-analysis of all THT participants and controls with 14 or more bed-days in the year prior to the index date was conducted comparing change in bed-days between for prolonged admission THT participants and controls.
A sensitivity analysis using the bed-days in the year before the entry date for THT participants, instead of bed-days in the year before index date, was conducted for prior bed-days and HoNOS scores, and for difference-in-bed-days. An additional sensitivity analysis comparing the bed-days in the 6 months prior to the index date, with the bed days in the 6 months after leaving THT for program participants, and the second 6 months after discharge from hospital for controls was undertaken.
A difference-in-difference analysis was undertaken comparing step-up and step-down THT participants in the year before the index date and the year after exit on change in bed days, change in HoNOS score, change in problems with living conditions and change in ED presentations.
Cost Analysis
All costs were converted from Australian Dollars (AU$) and expressed in 2009 international dollars (I$) in order to facilitate comparison across different settings and interventions. International dollars are a hypothetical currency that reflects each country’s purchasing power relative to the US dollar (US$) [“WHO CHOICE (Choosing Interventions That Are Cost-Effective)”]. In 2009, the purchasing power of I$1 was US$1 and AU$1.44 (“PPPs and Exchange Rates”).
A cost analysis was undertaken using a cost minimisation approach. Using hospital inpatient pricing data, the cost of a psychiatric inpatient bed-day in 2009 was estimated to be I$773.79. The cost of THT outpatient care per day was derived by dividing the total annual program costs to the mental health service for 2008–2009 by the number of available places per day (I$91.84 per day). Cost of adjusted bed-days averted per THT participant was compared to the cost to the mental health service for provision of THT. These costs were adjusted to include re-entry into THT.
All analyses were conducted using SPSS for Mac, version 20 (Chicago, IL: SPSS Inc., 2011).
Ethics
Ethics approval was granted from the Metro South Human Research Ethics Committee (HREC), Metro North HREC, University of Queensland School of Population Health Research Ethics Committee and Queensland Health Research and Governance Unit.
Results
Demographic, Service Utilisation and Clinical Characteristics of Participants
Summary characteristics for Transitional Housing Team (THT) participants and matched controls are presented in Table 1. One hundred and thirteen patients had first admissions to THT during the study period and were included in the analysis. Using the two stage matching protocol, the potential control group was reduced from 10,008 to 401 in stage one, and to 139 in stage two. All further analyses were conducted using the 139 patient stage two control group, hereafter referred to as the controls. There was no statistically significant difference between the THT participants and controls on gender, diagnosis, marital status, indigenous status, time of index hospitalization, or presence of any admission in the year before index date. THT participants were 4.3 years younger than controls (p = 0.002). Median days in hospital for admitted patients in the year before index date were statistically significantly longer for THT participants. THT participants had a higher illness acuity and a higher percentage of any emergency department (ED) presentations than controls.
Further analysis of THT participants compared to controls showed that THT participants were more likely to have an admission longer than 2 weeks (61.1 vs 38.1 %, χ2 = 13.13, df = 1, p < 0.001), had more problems with living conditions (Health of the Nation Outcome Scale (HoNOS) Q11 ≥ 2, 90.7 vs 53.4 %, χ2 = 36.64, df = 1, p < 0.001), and higher rates of substance abuse (HoNOS Q3 ≥ 2, 76.3 vs 59.7 %, χ2 = 7.41, df = 1, p < 0.001). Both groups had similar risks of non-accidental self harm (HoNOS Q2 ≥ 2, 38.8 vs 40.6 %, χ2 = 0.79, df = 1, p = 0.779).
Forty-one (36.3 %) of the THT participants entered the program directly as a step-up from the community while 72 (63.7 %) of THT participants entered as a step-down from the inpatient unit. There were no statistically significant differences between the step-up and step-down groups for age, gender, diagnosis, marital status, indigenous status, time of index hospitalization, illness acuity, problems with living conditions, substance abuse or self harm. The step-up group were more likely to have been admitted in the year prior to the index data (92.7 vs 61.1 %, χ2 = 13.08, df = 1, p < 0.001) and had a higher median inpatient bed days in the year before the index date with the step-up group having a median of 38 days [Interquartile Range (I.Q.R.) 20.5–65.5] and step down group having a median of 13 days (I.Q.R. 0–52.5), (Mann–Whitney U test, p = 0.002). There was no statistically significant difference between the step-up and step-down groups for number of bed days in the year prior to the entry date.
Change in Outcomes Over Time for THT Participants and Controls
There was a statistically significant difference-in-difference for bed-days [−20.76 days, standard error (SE) = 9.71, t = 2.14, p = 0.034] and problems with living conditions [−0.93, SE = 0.23, t = 4.06 p < 0.001] (Table 2). These results indicate that THT participants had a 20.76 day greater reduction in inpatient bed-days per participant compared to controls, and a 0.93 greater reduction on the problems with living conditions scale.
Changes in outcomes were adjusted for age, as well as bed-days and highest total HoNOS in the year before the index date (as appropriate) using a linear regression model. ED presentations in the year before the index date were not predictive of changes in bed-days within both THT participants and controls, and were not adjusted for. Reduction in bed-days was statistically significantly greater for THT participants when adjusted for age and highest total HoNOS in the year before the index date (β = −22.42, SE = 11.20, t = −2.00, p = 0.047). When problems with living conditions was included with age and highest total HoNOS in the year before the index date, the reduction in number of bed days for THT participants was similar to the unadjusted analysis, but was no longer statistically significant due to the inflation of the standard error (β = −20.52, SE = 12.36, t = −1.66, p = 0.098). Change in problems with living conditions remained significantly lower for the THT participants when adjusted for age, and bed-days in the year before the index date (β = −0.85, SE = 0.23, t = −3.67, p < 0.001). Change in non-accidental self-injury score and substance abuse score all remained non-statistically significantly different when adjusted for age and bed-days in the year before the index date.
As THT participants had a higher number of bed-days than controls in the year before the index date, there was potentially a greater opportunity for higher absolute reductions in bed-days, via regression to the mean. To explore this possibility, firstly the mean percentage change in bed-days for THT participants (reduction of 42.2 %) and controls (increase of 12.1 %) was calculated. The mean percentage reduction in bed-days was significantly greater for THT participants when compared to controls (−54.3 %, p = 0.038).
Secondly, a subset of all THT participants and controls with prolonged admissions (a total of 14 days or more bed-days) in the year prior to the index date was compared. The mean bed-days for THT participants reduced from 65.13 days in the year before index to 28.47 days, (n = 70, p < 0.001) compared to controls (63.54 to 50.21 days, N = 57, p = 0.323). The difference-in-difference was a 23.32 day greater reduction (SE = 16.56, t = 1.44, p = 0.153) for THT participants compared to controls, comparable to the value for the difference-in-difference for the entire sample. Although this did not reach statistical significance because of the smaller numbers in the sub-sample, it suggests that the reduction in bed-days for the THT participants is not solely due to regression to the mean.
As THT participants spent a mean of 150.24 (SE = 7.49) days in the program, their exit date was several months after the controls had been discharged from hospital. To examine whether this may have affected our results, we conducted a sensitivity analysis comparing the bed-days in the 6 months prior to the index date, with the bed days in the 6 months after leaving THT for program participants, and the second 6 months after discharge from hospital for controls. Using a difference-in-difference analysis, the reduction in bed days remained significantly greater for THT participants, with 16.49 days fewer in hospital than controls (SE = 5.33, t = 3.09, p = 0.002).
As the three THT participants who re-entered the THT program within one year of program exit may have had a reduced opportunity for hospital readmission, change in bed-days was adjusted for re-entry into THT. Change in bed-days remained statistically significantly different between the THT participant and control groups (β = −22.54, SE = 9.76, t = −2.31, p = 0.022).
Sensitivity Analysis on Index Versus Entry Date
Outcome measures 1 year before entry date were compared to outcome measures 1 year before index date for the THT participants, resulting in statistically significantly higher bed-days (72.35 vs 41.24 p < 0.001), highest total HoNOS (24.03 vs 23.15 p < 0.001) and highest question 11 HoNOS (3.32 vs 3.07 p < 0.001). The difference-in-difference in bed-days between THT participants and controls using entry date was 57.87 days lower for THT participants (SE = 10.14, p < 0.001).
Comparison of Step-Up and Step-Down THT Participants
Step-up THT participants had statistically significantly greater reductions in illness acuity (−9.77, SE = 2.20, t = −3.17, p = 0.002) and problems with living conditions (−1.12, SE = 0.36, t = −3.09, p = 0.003) when compared to step-up THT participants in a difference-in-difference analysis of the year before the index date and the year after the exit date. Change in bed-days and change in ED presentations were not statistically significantly different. When step-up THT participants were compared to the controls in a difference-in-difference analysis, step-up THT participants had statistically significantly greater reductions in bed-days (−37.02 days, SE = 11.96, t = −3.10, p = 0.003), illness acuity (−4.17, SE = 1.81, t = −2.20, p = 0.032) and problems with living conditions (−1.61, SE = 2.20, t = −5.28, p < 0.001). There was no statistically significant difference in change in ED presentations. When step-down THT participants were compared to the controls in a difference-in-difference analysis, the change scores were not statistically significantly different, but showed change in the same direction as for the step-up THT participants when compared to controls.
Costs Analysis
THT participants spent a mean of 150.24 (SE = 7.49) days in the program. The reduction in acute psychiatric inpatient bed-days associated with THT participation, adjusted for total HoNOS score and age, led to a savings to the mental health services of I$17,348.29 per THT participant. This was higher than the cost to the mental health services of the THT program of I$13,797.49 per participant. If the cost of the bed-days of THT participants who re-entered into THT within one year of exit is included, the program cost increases to I$14,024.37 per THT participant.
Discussion
Statement of Principal Findings
In this study, we compared participants of a transitional housing program to matched controls, and found that THT averted 22.42 psychiatric inpatient bed-days per THT participant after adjustment for age and HoNOS score. THT also resulted in a greater improvement in living conditions. The cost of providing the program was lower than the cost of the bed-days averted.
Strengths and Weaknesses
To the best of the authors’ knowledge, this study presented here is the first evaluation of a transitional housing program for patients with severe and persistent mental illness that attempts to conduct an analysis of costs to mental health services.
This study used a retrospective quasi-experimental design, and included all first time participants using THT. There were no research exclusion criteria, and as such this analysis reflects real world clinical practice.
The data came from de-identified administrative data-extracts. Administrative data has inherent limitations, including risk of recording bias and missing data. Datasets used primarily for billing, including inpatient data and ED presentations, provided close to a complete capture of data. HoNOS data were available for more than 84 % of all participants across all time periods. Ideally, routinely collected data on patient contact with case managers and psychiatrists would have been compared between groups, and included as a component of service costs. When the data on service contact was reviewed, the authors discovered that this routine data was inconsistently collected, rendering it unable to be analysed. Changes in the way Australian public community mental health services are funded may include the need for accurate collection of service contact. It would be useful to include accurate service contact data in future evaluations of housing programs.
When comparing patients served by different hospital districts, there is a risk that differences between districts could be a source of confounders. Although this may be a risk in this study, the mental health patient populations for all hospital districts in this study were similar, with comparable rates of social disadvantage. The demographics of patients served by all hospital districts in this study were similar. All hospital districts used state-wide models of care for mental health inpatient, outpatient and emergency department services. Data on adjusted length of stay and adjusted 28 day readmission rates were broadly similar in the referring and neighbouring hospital districts mental health services.
An advantage of a retrospective quasi-experimental study is that it allows exploration of differences between the THT participants and the broader population of acute mental health service users. This provides information to services planners on the patient population using THT, and can inform further research on appropriate target populations for transitional housing services.
There were demographic and service usage differences between the THT participants and controls. THT participants had higher psychiatric inpatient bed-day usage in the year before entry date and higher rates of ED usage compared to controls. This is in keeping with the existing evidence on high service usage for homeless and tenuously housed patients (Folsom et al. 2005).
We attempted to address these baseline differences between participants and controls as the higher number of bed-days in the year before their index date for THT participants may provide a greater opportunity for reduction in bed-days in the year after exit. Three strategies were used to address these differences. Firstly, we undertook an evaluation of the mean percentage change in bed-days. Secondly, we examined the difference-in-difference in bed-days for patients with extended admissions in the year before entry. Thirdly, a sensitivity analysis of difference-in-difference of bed-days using entry date instead of the index date more than doubled the reduction in bed-days for THT participants compared to controls. The results of these verifications suggested that the reductions in bed-days for THT participants are a true program effect over and above regression to the mean, and may err on the side of being conservative.
THT participants were more likely to have problems with living conditions than controls. When we attempted to control for this in the regression adjusted analysis of the difference-in-difference, the reduction in bed-days for THT participants was of a similar magnitude to the unadjusted difference-in-difference analysis, but was insufficiently powered to show significance.
When the controls were compared to the step-up and step-down groups respectively, the step-up group had greater reductions in bed-days, illness acuity and problems with living conditions. Step-up THT participants had a higher number of bed days in the year before the index date, but not before the date of entry to THT. This suggests that the step-up and step-down groups are similar, with the step-up group spending a period of time in tenuous housing between hospital and entering THT, and the step-down group going directly from hospital to THT. We have taken a conservative approach to our analysis, and used the index date as the comparison date. As such, the hospital bed-days immediately prior to entry into THT for the step-down group are not counted as hospital bed-days prior to the index date. Although it is possible that transitional housing services may be more effective for patients currently living tenuously in the community than for current inpatients, it is more likely that these differences are an artefact of the analysis, and should be treated cautiously.
A final limitation is the use of a cost minimilisation approach limited to services provided by the public mental health system. Our analysis did not include state and federal costs associated with the housing stock or any potential changes in social security benefits or incarcerations, as this data was not available to the researchers. Changes in costs for clinical case management as usual could not be calculated because of limitations in the data relating to clinical community service contact.
Comparisons to Other Studies
In the published literature there are only a limited number of evaluations of transitional housing programs, and these studies do not explore costs. An evaluation of three transitional housing programs available for US Veterans Affairs (VA) patients: a VA staffed transitional program on VA grounds; a VA contracted community supported housing program; and a national competitive grant funded supported housing program; did not demonstrate that program configuration could predict difference in health status or housing outcomes (McGuire et al. 2011). Cost analyses were not undertaken.
Evaluations of program costs were limited to crisis houses and permanent supported housing programs. In a recent systematic review of short term residential alternatives to acute psychiatric hospitalisation, studies of crisis houses that included cost analyses tended to find the crisis house to be of lower cost than traditional hospitalisation (Lloyd-Evans et al. 2009). An evaluation of a Housing First permanent supported housing program in San Diego found reductions in inpatient costs for program participants when compared to controls (Gilmer et al. 2009). This evaluation of Housing First did not include costs associated with housing stock and did not compare reductions in inpatient costs to costs of the program.
Transitional Housing Program Evolution and Research
THT participants had higher rates of substance abuse problems than controls both in the year before entry and in the year after exit. THT does not currently have an integrated drug and alcohol treatment service as part of the program. Given that over three quarters of THT participants had clinically significant substance abuse problems, it would be important for future iterations of transitional housing programs to incorporate targeted drug and alcohol treatment services.
A modification of ED presentations was one of the prior hypotheses of this study. There was no comparative reduction in ED presentations for THT participants in the difference-in-difference analysis. Previous studies have found that homeless patients with SPMI have higher rates of ED presentations (Folsom et al. 2005). Rates of ED presentations were significantly higher for THT participants than controls for both the year before entry and year after exit. Although confounding due to differences between the hospital districts is possible, comparisons of the availability of primary care and community mental health services make this unlikely. Our hypothesis is that the THT participants had become habituated to presenting at the ED, and that the THT program was ineffective in reducing this habituation. Future iterations of transitional housing programs may benefit from providing additional timely crisis interventions, and services to improve participants’ linkages to primary care clinics.
Conclusions
The findings of reductions in bed-days and improved living conditions suggest that transitional housing programs can have a significant positive impact for tenuously housed patients with high inpatient service usage at a cost saving to the public mental health system. Greater emphasis on treatment of substance abuse and ED diversion is needed for this patient population.
References
Babidge, N. C., Buhrich, N., & Butler, T. (2001). Mortality among homeless people with schizophrenia in Sydney, Australia: A 10-year follow-up. Acta Psychiatrica Scandinavica, 103(2), 105–110.
Bebbington, P., Brugha, T., Hill, T., Marsden, L., & Window, S. (1999). Validation of the health of the nation outcome scales. The British Journal of Psychiatry, 174(5), 389–394.
Burgess, P., Trauer, T., Coombs, T., McKay, R., & Pirkis, J. (2009). What does ‘clinical significance’ mean in the context of the health of the nation outcome scales? Australasian Psychiatry: Bulletin of Royal Australian and New Zealand College of Psychiatrists, 17(2), 141–148.
Corrigan, P. W., & McCracken, S. G. (2005). Place first, then train: An alternative to the medical model of psychiatric rehabilitation. Social Work, 50(1), 31–39.
Folsom, D. P., Hawthorne, W., Lindamer, L., Gilmer, T., Bailey, A., Golshan, S., et al. (2005). Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. The American Journal of Psychiatry, 162(2), 370–376.
Gilmer, T. P., Manning, W. G., & Ettner, S. L. (2009). A cost analysis of san diego county’s REACH program for homeless persons. Psychiatric Services (Washington, DC), 60(4), 445–450.
Harris, M. G., Buckingham, W. J., Pirkis, J., Groves, A., & Whiteford, H. (2012). Planning estimates for the provision of core mental health services in Queensland 2007 to 2017. Australian and New Zealand Journal of Psychiatry, 46(10), 982–994.
Harvey, C. A., & Fielding, J. M. (2003). The configuration of mental health services to facilitate care for people with schizophrenia. The Medical Journal of Australia, 178(Suppl), S49–S52.
Harvey, C., Killackey, E., Groves, A., & Herrman, H. (2012a). A place to live: Housing needs for people with psychotic disorders identified in the second Australian national survey of psychosis. Australian and New Zealand Journal of Psychiatry, 46(9), 840–850.
Harvey, C., Killaspy, H., Martino, S., & Johnson, S. (2012b). Implementation of assertive community treatment in Australia: Model fidelity, patient characteristics and staff experiences. Community Mental Health Journal, 48(5), 652–661.
Hubbeling, D. & Bertram, R. (2012). Crisis resolution teams in the UK and elsewhere. Journal of Mental Health (Abingdon, England), 21(3), 285–295.
Jablensky, A., McGrath, J., Herrman, H., Castle, D., Gureje, O., Evans, M., et al. (2000). Psychotic disorders in urban areas: An overview of the study on low prevalence disorders. Australian and New Zealand Journal of Psychiatry, 34(2), 221–236.
Kisely, S., Campbell, L. A., Crossman, D., Gleich, S., & Campbell, J. (2007). Are the health of the nation outcome scales a valid and practical instrument to measure outcomes in north America? A three-site evaluation across Nova Scotia. Community Mental Health Journal, 43(2), 91–107.
Larney, S., Conroy, E., Mills, K. L., Burns, L., & Teesson, M. (2009). Factors associated with violent victimisation among homeless adults in Sydney, Australia. Australian and New Zealand Journal of Public Health, 33(4), 347–351.
Lloyd-Evans, B., Slade, M., Jagielska, D., & Johnson, S. (2009). Residential alternatives to acute psychiatric hospital admission: Systematic review. The British Journal of Psychiatry : The Journal of Mental Science, 195(2), 109–117.
McGuire, J., Rosenheck, R. A., & Kasprow, W. J. (2011). Patient and program predictors of 12-month outcomes for homeless veterans following discharge from time-limited residential treatment. Administration and Policy in Mental Health, 38(3), 142–154.
Newman, S., & Goldman, H. (2008). Putting housing first, making housing last: Housing policy for persons with severe mental illness. The American Journal of Psychiatry, 165(10), 1242–1248.
North, C. S., & Smith, E. M. (1993). A systematic study of mental health services utilization by homeless men and women. Social Psychiatry and Psychiatric Epidemiology, 28(2), 77–83.
Pirkis, J., Burgess, P., Kirk, P., Dodson, S., & Coombs, T. (2005). Review of standardised measures used in the national outcomes and casemix collection (NOCC). Canberra: Australian Mental Health Outcomes and Classification Network.
Plumb, J. D. (1997). Homelessness: Care, prevention, and public policy. Annals of Internal Medicine, 126(12), 973–975.
PPPs and Exchange Rates. PPPs and exchange rates. Retrieved September 13, 2013, from http://stats.oecd.org/Index.aspx?datasetcode=SNA_TABLE4.
Siskind, D., Harris, M., Buckingham, B., Pirkis, J., & Whiteford, H. (2012a). Planning estimates for the mental health community support sector. Australian and New Zealand Journal of Psychiatry, 46(6), 569–580.
Siskind, D., Harris, M., Pirkis, J., & Whiteford, H. (2012b). Personalised support delivered by support workers for people with severe and persistent mental illness: A systematic review of patient outcomes. Epidemiology and Psychiatric Sciences, 21(1), 97–110.
Siskind, D., Harris, M., Pirkis, J., & Whiteford, H. (2013). A domains-based taxonomy of supported accommodation for people with severe and persistent mental illness. Social Psychiatry and Psychiatric Epidemiology, 48(6), 875–894.
Test, M. A., & Stein, L. I. (1976). Training in community living: A follow-up look at a gold-award program. Hospital & Community Psychiatry, 27(3), 193–194.
Tsemberis, S., Gulcur, L., & Nakae, M. (2004). Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health, 94(4), 651–656.
WHO CHOICE (Choosing Interventions That Are Cost-Effective). WHO CHOICE (choosing interventions that are cost-effective). Retrieved September 13, 2013, from http://www.who.int/choice/en/.
Wing, J. K., Beevor, A. S., Curtis, R. H., Park, S. B., Hadden, S., & Burns, A. (1998). Health of the nation outcome scales (HoNOS). Research and development. The British Journal of Psychiatry: The Journal of Mental Science, 172, 11–18.
Acknowledgments
We would like to acknowledge the Queensland Directorate of Mental Health for access to de-identified data extracts and assistance in data linkage, Dr. Cathy Mihalopoulos for advice on economic analysis and the staff of the Transitional Housing Team.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siskind, D., Harris, M., Kisely, S. et al. A Retrospective Quasi-Experimental Study of a Transitional Housing Program for Patients with Severe and Persistent Mental Illness. Community Ment Health J 50, 538–547 (2014). https://doi.org/10.1007/s10597-013-9654-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-013-9654-y