Abstract
To assess the cost of illness of generalized anxiety disorder (GAD) in a primary healthcare setting in Spain. A cross-sectional, retrospective study was conducted. The sample comprised patients diagnosed with GAD according to ICD-10 criteria and a control group. Healthcare/non-healthcare resource utilization was recorded retrospectively for the 12 months prior to the study visit. Costs were estimated from a societal perspective. Two models have been produced to study the variables that influence the cost of the illness both, without and with controls. The study enrolled 456 patients [76.8 % women, 49.2 (17.0) years] with GAD and 74 controls without GAD [42.5 % women, 47.9 (16.7) years]. 67.8 % of subjects were on combination therapy (antidepressant + anxiolytic); 6 % were using 2 or more drugs to treat anxiety; and 23.4 % were on monotherapy. Total annual average costs were higher in the GAD group (€7,739 vs. €2,609), with mean costs attributable to GAD of €5,139 (healthcare costs: €1,329, indirect costs: 75 % of total cost, approximately). Age and health status measured by Hamilton Anxiety Rating Scale and clinical global impression were related to costs. The improvements in quality of life measured by EQ-5D index are associated to lower cost. GAD treated in Spanish primary healthcare settings generated considerable healthcare costs and, particularly, loss-of-productivity costs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The National Institute of Mental Health defines generalized anxiety disorder (GAD) as an anxiety disorder characterized by chronic anxiety, exaggerated worry and tension, even when there is little or nothing to provoke it. People who suffer from GAD generally expect the worst to happen, and worry too much about money, health, family, and work, even when there are no signs of problems. These patients also find it difficult to relax and concentrate. They usually suffer from sleeping disorders. GAD is often accompanied by physical symptoms such as fatigue, tremors, muscle tension, headaches, irritability, excessive perspiration, etc. (Wittchen et al. 1994; NIMH 2005). There is often an existing co-morbidity such as another anxiety disorder, depression, or substance abuse (Souetre et al. 1994; Lobo and Campos 1997). GAD is commonly treated with medications.
In Europe and the United States, GAD and substance abuse have a high annual life-prevalence of approximately 2 and 5 %, respectively (Fricchione 2004; Lieb et al. 2005). The European Study of the Epidemiology of Mental Disorders (ESEMeD), conducted in 6 European countries, found that 14 % of Europeans develop some anxiety disorder (not necessarily GAD) at some point in their life (Alonso et al. 2004). In addition, GAD is a common anxiety disorder in the population above 65 years of age. It is estimated that more than half of the patients with anxiety disorders visit primary healthcare (PHC) centers (Wittchen 2002). A study by the World Health Organization, following the ICD-10 criteria, found the prevalence of generalized anxiety disorder to be 7.9 % in a sample of 25,916 patients recruited in PHC centers in 14 countries (Goldberg and Lecrubier 1995). The existing studies on PHC in Spain estimate the prevalence of GAD to range between 4.5 and 7.3 % (Chocron Bentata et al. 1995; Lobo and Campos 1997).
The aim of cost and burden of illness studies is to quantify the effects of an illness on the well-being of those who suffer from it and to society at large. Cost of illness includes both the direct and indirect costs incurred as a result of illness. The direct costs include the monetary cost of healthcare and costs incurred for non-healthcare resources used as a result of an illness. Indirect costs include the productivity loss that can be attributed to the illness. The procedure for quantifying costs involves, firstly, measuring the use of each resource in specified units, and secondly, converting those units in monetary terms with the aid of unitary costs or prices in order to arrive at a composite estimate. A small number of studies have been conducted to estimate the costs of mental disorders in Spain. These include the cost of mental disorders in the Canary Islands in the year 2002 (Lopez-Bastida et al. 2004), the cost of schizophrenia (Haro et al. 1998; Salvador-Carulla et al. 1999; Vazquez-Poloet al. 2005), the cost of vascular dementia compared with Alzheimer-type dementia (Sicras et al. 2005), the cost of the ambulatory resources of Alzheimer disease (Boada et al. 1999), the cost of schizophrenic relapses (Peiro et al. 2004), and a specific study of anxiety disorders that addresses the cost-offset of panic disorders for the year 1992 (Salvador-Carulla et al. 1995).
The impact of GAD (use of health care resources, loss of well-being, etc.) is assumed to be considerable. The indirect costs imposed by GAD include the loss of productivity and employee absenteeism. These costs can be considerable given the high prevalence of GAD (Souetre et al. 1994; Candilis and Pollack 1997; Andlin-Sobocki and Wittchen 2005). Therefore, in order to estimate the actual cost of GAD, indirect costs must also be considered in addition to direct costs.
The objective of the present study is to assess or estimate the cost and the burden of GAD in Spain. A comparison of a sample of patients with GAD enrolled at PHC centers versus a control group formed the basis. The study analyzed the determining factors and possible explanatory variables of the cost and the burden of disease. This article focuses on assessment of the annual cost attributable to GAD in Spain in 2006.
Methods
Study Design and Participating Centers
This is a multicenter, longitudinal, observational, and retrospective study. Data was collected by the doctors from a representative sample of PHC centers in Spain. The proportion of the regional population served/covered by these centers acted as a weight. The Scientific Research Ethics Committee approved the protocol of the study. The participating researchers were randomly selected from a database of qualified researchers. All had previous experience in studies on mental health and were familiar with the administration of basic mental health scales. Based on the estimates of the required sample size of GAD cases and controls (see more below), the study anticipated participation by approximately 174 primary healthcare doctors. Each doctor was asked to recruit the first three patients diagnosed with GAD and one control who came to his/her office and met the specified study criteria. The doctors were asked to select one patient with GAD from each of the following three age brackets: 18–34 years, 35–64 years, and 65 years and above. The control group was to be recruited from individuals who came to the PHC center for administrative purposes, such as to get a medical prescription or to accompany a patient, etc., and/or due to a minor illness (e.g., common cold, skin infection, or diarrhea). Controls were also required to belong to one of the three age brackets in order to maintain uniformity.
Exclusion and Inclusion Criteria for Recruiting Participants
The inclusion and the exclusion criteria of the study were as follows: Inclusion criteria: Outpatients, both male and female, over 18 years of age with a diagnosis of generalized anxiety disorder (ICD-9 code: 300.02 and ICD-10 code: F41.1) (World Health Organization 1992). To be included in the GAD group, it was important that the clinical history of the patient be available for a minimum of 12 months. Other mandatory requirements for inclusion were written consent by the patient and ability to read, to understand, and complete health status questionnaires in Spanish. Exclusion criteria: The exclusion criteria included non-availability of clinical history or medical records for the past 12 months, inability to read or understand health questionnaires in Spanish, and presence of another serious illness that interfered with the patient’s capacity to fill in the questionnaires. For example, mental retardation or insufficiency can hinder a patient’s ability to recall previous utilization of health services and health-related expenditures, and to complete health questionnaires.
Calculation of Sample Size
Owing to the absence of studies estimating the cost of GAD in a primary healthcare setting in Spain, this study had to define its own criteria for arriving at an appropriate sample size. The sample size was determined on the basis of two criteria: (a) a sample should be representative. This required a sample composed of 100–150 individuals (adjusted for loss of 10 % of participants) in each of the 3 age brackets; (b) The sample size had to be large enough to capture a minimum average cost differential of 450€ with a standard deviation of 675€ between the cost of treating a patient with moderate/severe GAD (a score >15 on the Hamilton Anxiety Rating Scale, HAM-A) and a patient with mild GAD (HAM-A score of 6–14), and between GAD and control group. The figure of 450€ was selected as a benchmark because it was assumed that a new treatment that provided cost savings of at least 450€ would be considered to have a financially significant impact and might qualify for reimbursement. The study design required recruitment of a total of 696 participants, 522 (75 %) with GAD in the treatment group and 174 (25 %) in the control group. This sample would make it possible to test the study hypothesis with an α error <0.016 (including the Bonferroni correction for multiple comparisons), and a power of 80 % (β error <0.2) using a two-tailed test.
Data Collection
The data was collected on a questionnaire. The questionnaire comprised seven forms, of which Forms 1 and 2 were meant to be completed by the investigator and Forms 3–7 by the participants themselves. The questionnaires were specifically designed for this study and were modified on the basis of a pilot study with 19 participants. In the part of the questionnaire meant to be filled by the investigator, Form 1 contained questions on socio-demographic information (personal information such as age, gender, etc.), co-morbidity, absenteeism from work, course of the illness, medication for GAD and other causes, and the physician’s perception of the patient’s state of health and Form 2 contained the Spanish version of the HAM-A (Hamilton 1959; Lobo et al. 2002). Forms 3–7, meant to be completed by the patients themselves, contained personal information, information on the use of caregivers, course of the illness, medication, etc.
Use of Health Care and Non-healthcare Resources
The study classifies the resources in three categories: (a) Healthcare costs: costs of medical visits to primary care physicians and specialists, emergency room visits, diagnostic tests, routine and emergency hospitalizations, and medication, (b) Non-healthcare direct costs: expenses incurred for a caregiver, transportation, baby-sitting, and other out-of-pocket costs, and (c) Indirect costs: productivity loss due to employee absenteeism related to GAD.
The respondents were asked to list the general expenses incurred for healthcare in the past 3 months and expenses for emergency room visits and hospitalizations in the past year. The annual estimates were derived by linearly extrapolating the quarterly data by multiplying it by four. The questionnaire made a distinction between use of resources due to GAD and use related to other causes. The study assumes higher use of health care resources by patients with GAD in comparison with use by the general population. The people suffering from GAD may visit primary healthcare centers more frequently for apparently non-associated reasons, but the underlying cause may in fact be GAD. The costs associated with these visits can be therefore be classified as attributable to GAD. This study defined the cost attributable to GAD as the difference between the total average costs incurred by the GAD group and the control group.
Estimation of Costs
Table 1 lists the average unit costs of several healthcare services and resources. The majority of the information was taken from the SOIKOS healthcare costs database (SOIKOS 2005). The unit costs are presented in 2006 prices. The costs of consulting a psychiatrist and a psychologist were taken from the PSICOST study (Vazquez-Polo et al. 2005; Saldivia Borquez et al. 2005) describes the method of calculating these costs. The costs of medications were taken from Catalog of Pharmaceutical Specialties (Catálogo de especialidades Farmacéuticas 2006) of the General Council of Official Colleges of Pharmacists of Spain. Drug costs are presented as cost per milligram of active ingredient. For non-branded generics (drugs sold under their INN), the product with the lowest price was selected. For branded generics (non-INN), the brand with the lowest price was selected.
The average cost of absenteeism from work was calculated on a per-day basis from the information on labor costs provided by the National Institute of Statistics for the year 2006 (INE 2006). The average per-day cost of absenteeism was calculated by dividing the total average monthly cost per worker for a company (€2,197.39) by the average number of full working days in a month (according to the labor agreement, 156.8 h/8 h = 19.1 days). This ratio was then multiplied by the average daily wage (average monthly labor cost per worker divided by the working hours per month). The per-day cost of absenteeism was calculated to be €115.05 (2,197.39€/19.1 days).
Data Analysis Procedures
The descriptive analysis of the cost variables includes the mean, the standard deviation, and the minimum and maximum values. Since a Kolmogorov–Smirnov test confirmed that the continuous variables of the sample were not normally distributed, it was decided to use nonparametric tests for the comparative analysis. A Mann–Whitney test was used when only two groups were compared (e.g., patients with GAD vs. controls). A Kruskal–Wallis test was used when the comparisons involved three or more groups (e.g., comparison across the severity score intervals of the HAM-A). For the Kruskal–Wallis test, the Tukey–Kramer method was used to determine whether the difference in groups was statistically significant. If the p value was <0.05, the difference was considered statistically significant. Socio-demographic and habit data were compared using a χ 2 test or Fisher’s exact test.
Variables that Influence the Cost of the Illness
We seek to determine whether the variables age, sex, Hamilton scale values, index of quality of life, and CGI influence the annual cost of the illness (AnnCost). Costs can have a high degree of asymmetry. In this case is more realistic to assume that the costs follow a log-normal distribution (O’Hagan and Stevens 2001). Thus, the dependent variable, the annual cost of the illness, has lognormal distribution. The model shows the following functional form:
where
-
Sex = 1 if the person is female; otherwise, = 0.
-
Age in years
-
Hamtot measured from the Hamilton scale values
-
EQ index i The EQindex index value attached to an EQ-5D state according to Dolan (1996) particular set of weights.
Moreover, we analyze the influence of the above variables on the annual cost comparing controls with patients:
The multiplicative dummy variable CGI control is not included in Model 2 because all control subjects belong to the same category (Normal, not ill). And the multiplicative dummy variable EQindex control is not considered because 68 % control subjects belong to the same category (the “best” health state, representing to value 11,111). Otherwise, introducing this variable in the model would produce multicollinearity with the control variable. This was confirmed by collinearity tests.
The computations and simulations made for the models above were carried out by Bayesian statistics, using Gibbs sampling and Metropolis-Hasting algorithms, which constitute the two basic approaches used in the Markov Chain Monte Carlo methodology (Gilks et al. 1996). These algorithms were applied by means of WinBUGS 1.4 statistical software (Spiegelhalter et al. 2003). For the simulations, a total of 100,000 iterations were carried out, after a burn-in run of 10,000, with a few minutes being required for the simulation of each model.
The analysis revealed a wide dispersion in individual costs and the existence of outliers (extreme or atypical values) that could substantially influence the average values of some variables. Therefore, it was decided to conduct a cost analysis with and without outliers. The outliers were identified by graphical plotting of data. A threshold was set for each cost category. Since the statistical results for the analysis with and without outliers did not show any significant difference, the reported results are those from the analysis with outliers unless stated otherwise.
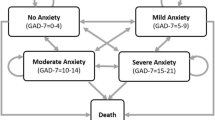
The results show the cost of treatment by age group (18–34, 35–64, and >65 years), gender, co-morbidity according to the Charlson Index (Quan et al. 2005:1130–1139; Charlson et al. 1987:373–383) grouped into three levels (index 0, 1, and 2 or more. 0: no or irrelevant co-morbidity; 1: low-level co-morbidity; 2 or more: advanced co-morbidity); and severity of anxiety symptoms according to the HAM-A scale, which groups patients into four categories [no anxiety (0–9 pts); mild anxiety (10–15 pts); moderate anxiety (16–24 pts); and serious anxiety (>24)].
Results
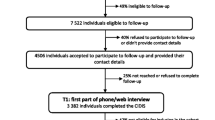
The data for the study were collected between February and June 2006. A total of 456 patients with GAD and 74 participants in the control group were enrolled by a randomly selected sample of 134 physicians from primary healthcare centers. The sample was representative of the whole of the country.
Sample Characteristics
The study was able to recruit 456 patients in the GAD group and 74 subjects in the control group as against the projection of 522 and 174 participants, respectively. Therefore, the study recruited 87 and 43 % of the expected participants in the treatment and control groups. Table 2 provides the main socio-demographic profile of the participants in the treatment and the control groups. Women constituted 77 % of the treatment group and 42 % of the control group (p < 0.001). In the GAD group, 45 % of the patients were between 35 and 64 years of age, 67 % were either married or living with a partner, 35 % were full-time employees, 27 % had house work as a main occupation, 46 % had a primary level education, 35 % a secondary education, and 19 % held a university degree. Table 3 shows the distribution of the sample according to severity of anxiety on the HAM-A scale and perception of illness by the investigator on the clinical global impression (CGI) scale. According to this scale, 83 % of the patients were ill (between borderline and extremely ill). 34 % of the patients with GAD were given a severity score >24 pts on the HAM-A scale.
Annual Per-patient Cost of GAD
Table 4 presents the itemized estimates of the annual cost of generalized anxiety disorder with their corresponding levels of significance. This includes direct costs of healthcare and indirect costs imposed by GAD. The table also presents the costs attributable to GAD, defined as the difference between the average cost in the GAD group and the control group. The mean of the annual total costs of GAD was found to be €7,541 as compared to €2,351 for the control group. According to the estimates, the total cost attributable to GAD was €5,189. Of this amount, direct costs accounted for €1,424, and €3,765 could be classified as indirect costs imposed by productivity loss. Non-GAD-related direct healthcare costs were marginally higher for the control group (€681) than for the GAD group (€623). However, this difference was not statistically significant (p = 0.409).
Table 5 presents the total costs by age bracket, gender, Charlson Index, and severity of anxiety on the HAM-A scale. The average annual total costs of patients with GAD in the 18–34 year age group were €8,973, close to €8,913 for the 35–64 year age bracket. However, the cost of those aged 65 years and above was a lower €3,725. This can be attributed to lower productivity losses, because people in this age group are over the retirement age. Although the cost differences were not found to be statistically significant between age intervals, the average total costs per patient in the GAD group for each age group were significantly higher than those for the control group in the corresponding age group. The estimated costs attributable to GAD were €4,656, €6,911, and €2,405 for the 18–34, 35–64, and 65 and over age groups, respectively. The analysis revealed that the costs of GAD patients were significantly higher than those for the control group in general and also when segregated by gender. Across all categories, indirect costs constituted a larger component of the total costs. An analysis by level of co-morbidity revealed significantly higher total annual costs for the GAD group than the control group. However, there was no clear association between cost and level of co-morbidity (Table 5). The total costs per patient in each group were €7,591, €7,549, and €6,889 for Charlson Index categories 0, 1, and 2 or more, respectively. It can be seen in Table 5 that the annual average total costs of patients with severe anxiety (>24 pts on the HAM-A) are significantly higher than in the other sub-groups: €11.674 versus €6.390, €5.724, and €3.496 for progressively less severe anxiety (p < 0.01 for the all groups comparisons, and p < 0.05 between moderate anxiety and no anxiety).
Direct Healthcare Costs
Those components of healthcare costs in the GAD group and those in the control group that are mostly financed by the National Health System are presented in Table 6 and Fig. 1. These are itemized by treatment and control group, by gender, by age group, co-morbidity, and severity of anxiety. The highest proportion of costs in GAD patients is incurred for specialists, €473 (26 %), followed by medication, €381 (21 %), and primary healthcare, €366 (20 %). The analysis of costs by age groups reveals that the highest cost for specialists was in the 18-34 (€598) and 35–64 years (€464) age groups. In the >65 years age group, the highest cost was for medication, which was €478 per patient per year. Itemized by gender, the estimated per patient per year specialist cost (€505), medication costs (€402), and PHC costs (€361) were higher in women, whereas in male, the costs of the three categories were very similar (Table 6). In general, the different categories of healthcare costs tend to be higher for patients with a higher Charlson Index. The specialist costs in the group with a value of 1 on the Charlson Index and the hospital emergency room costs in patients with a Charlson Index of 2 or more are the only ones that deviate from this pattern. When analyzing the care costs according Hamilton Scale score the costs for each category of resource increase with the score. The increases are larger for scores greater than 15 pts for almost all the components of healthcare costs, with the exception of medication, which remain similar across the different sub-groups of anxiety severity. However, patients with mild anxiety (10–15 pts on the HAM-A) show costs, in almost all healthcare cost categories, lower than the corresponding costs in the group with a 0–9 score (Fig. 1).
Models 1 and 2 (Table 7) show the influence of different variables on the annual cost of GAD. Results of Model 1 show the relevance of the health variables HAM and CGI: increments in those variables produce increments in cost. For EQ-5D, improvements in the EQ index are associated to lower cost. To belong to the control group is associated to a lower cost. All variables in Model 1 have been different from zero with a probability of 95 %, as shown in the credible interval that excludes the value zero.
Model 2 adds the incremental influence on cost when the relations between controls and variables are considered. In the control group higher age contributes to a higher annual cost and the opposite occurs in the patients group. An increment in HAM in the control group is associated to a lower cost, and the opposite occurs in the patients group.
Discussion
There are few studies that allow us to put the results of the present study into a broader perspective. There is only one published study on the costs of the mental disorders in Spain (Lopez-Bastida et al. 2004). This study is restricted to the Canary Islands for the year 2002. It provides only aggregate estimates. The direct healthcare costs are €81.7 million. If we accept the estimation of the prevalence of mental disorders provided in the study (24.8 %) and apply it to the population of nearly 2 million in the Canary Islands, the average annual costs per mental health patient would be on the order of €165, a figure much lower than the estimates found by this study for healthcare costs attributable to GAD (€1,206).
Berndt et al. (2000) estimated the healthcare costs due to various forms of mental illnesses from a sample of 2,222 insured persons in the US using information from administrative databases. Their estimates are averages for the period 1993–1995. For GAD, the estimates are based on a small sample of 20 individuals. According to Berndt et al., the annual healthcare costs of treating GAD were US $6,747. Their estimates are considerably higher than those in this study. However, this difference can be possibly explained by differences in unit costs between Spain and the US.
Marciniak et al. (2004) conducted a study on the costs of anxiety using an approach similar to this study. Like this study, they also compared a cohort of patients with a diagnosis of anxiety with a control group, in their case of the same size. There were 1,917 individuals in each group. Differences in the costs to treat different levels of anxiety also formed part of their study design. As in the study by Berndt et al. (2000), they used information from an administrative database. Marciniak et al. (2004) estimated the direct healthcare costs for treating anxiety to be US $1,555 for the year 2000. Their estimates are in keeping with this study. The comparability of the US estimates can be questioned on the basis of the higher per-unit healthcare costs in the US. However, a high proportion of patients with greater severity of GAD in the sample of this study can be viewed as compensating for the higher costs in the US.
The results of this study are likely to overestimate the average cost of GAD in Spain, because of the high proportion of the patients (one-third) in the study sample who had a severe anxiety. Generally, the proportion of the patients with severe anxiety is assumed to be lower. The rationale behind the methodology employed to determine the costs attributable to GAD and its limitations are worth discussing. The costs attributable to GAD have been presented as an estimated difference between all the GAD-related costs (incurred in GAD group) and non-GAD-related costs (incurred in control group). The approach is based on the assumption that patients with GAD may incur healthcare costs that may not be explicitly attributable to the illness but may be spurred by it. Therefore, it is important to compare the total non-GAD-related costs incurred in a (relatively) healthy control group versus those incurred in patients with GAD. The control group was selected from the population of individuals who attended the same healthcare centers as those diagnosed with GAD, but for administrative purposes or for minor illnesses. The underlying assumption of this selection process was that it would yield an appropriate control group with the same socio-economic characteristics as the GAD group. The fact that the costs not associated with GAD were higher for the control group than the GAD group suggests that the participants in the control group may be suffering from severe illnesses that involve substantial healthcare costs. This would imply an underestimation of the cost attributable to GAD. These unexpected results may also partly be due to the small size of the control group. It is important to emphasize that only 74 researchers (55.2 %) complied with the criteria for selecting subjects for the control group. This led to a substantially lower number of individuals recruited to the control group than was originally envisaged. This had repercussions for drawing valid and meaningful comparisons between the two groups, especially when the comparisons involved smaller subgroups.
Co-morbidity might be a confounding factor in assessing the cost and health effects of a disease, especially when diagnostic criteria are not well defined, because it might be arbitrary to attribute the costs to any of the concomitant diagnoses. 64.0 % of the patients with GAD had some type of physical co-morbidity, a similar figure to the control group (64.9 %). Twenty-one (4.6 %) patients with GAD had an additional diagnosis of a psychiatric disorder, which was depression in 18 cases, while no individuals in the control group reported a psychiatric diagnosis. The average annual cost of GAD patients with no co-morbidities is €6,152; for patients with physical co-morbidities, the cost rises to €7,809 and for those with psychiatric co-morbidity, to €14,334. Although this figure doubles the cost for the entire GAD sample, €7,541, the impact on the average is not too large due to the relatively small number of GAD patients with psychiatric co-morbidities. If these patients were removed from the sample, the average annual cost would only fall by 4.3 % to €7,210.
It is worth mentioning that the lack of standardization and, consequently, of comparability of the studies on the cost of illness done by different authors limits the usefulness of the studies of the cost of individual illnesses. This limitation might not apply directly to this study because there is a practical absence of studies on the cost of mental disorders in Spain. The results of the study indicate a strong association between the severity of anxiety symptoms and the cost of illness. Particularly, beyond a score of 15 points on the HAM-A scale, there is a considerable increase in cost of all components, particularly for the category of indirect costs, which according to this study represents around 70 % of the cost of this illness. In addition, from a pure healthcare perspective, it is interesting to see that the cost of medication for GAD does not substantially change with the level of severity of the symptoms. However, the costs of medical visits (be they PHC, specialist, or emergency room visits), tests and hospitalizations change substantially with the severity of symptoms. It should be noted that although only 16 % of patients were perceived by the physician as being moderately or seriously ill, around 1/3 of the recruited patients showed serious symptoms of anxiety. This could explain the relatively small impact of GAD in terms of the cost of health resources and the greater impact in terms of absenteeism.
Despite its limitations, the study provides the first estimates of the costs of GAD in Spain. It is among the few international studies evaluating the economic impact of GAD. The strength of the study lies in the primary data (individual data) and the micro-costing technique (calculation of resource utilization by each enrolled patient). The techniques used by the study provide a useful reference for management decisions and for future economic evaluations. The study has adopted a novel definition of the costs attributable to GAD: the difference between the costs incurred by a cohort of patients with a given disease and those incurred by a control group.
In sum, the study shows that the GAD imposes a substantial cost in terms of healthcare resource utilization and absenteeism from work. This entails substantial costs for the National Health System and for society as a whole. The severity of illness is the most influencial variable on the cost of the illness.
References
Alonso, J., Angermeyer, M. C., Bernert, S., et al. (2004). Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica Supplementum, 420, 21–27.
Andlin-Sobocki, P., & Wittchen, H. U. (2005). Cost of affective disorders in Europe. European Journal of Neurology, 12(Suppl 1), 34–38.
Berndt, E. R., Bailit, H. L., Keller, M. B., Verner, J. C., & Finkelstein, S. N. (2000). Health care use and at-work productivity among employees with mental disorders. Health Affaires (Millwood), 19, 244–256.
Boada, M., Pena-Casanova, J., Bermejo, F., et al. (1999). Costs of health care resources of ambulatory-care patients diagnosed with Alzheimer’s disease in Spain. Medicina Clinica (Barc), 113, 690–695.
Candilis, P. J., & Pollack, M. H. (1997). The hidden costs of untreated anxiety disorders. Harvard Review of Psychiatry, 5, 40–42.
Catálogo de Especialidades Farmacéuticas de. (2006). Consejo General de Colegios Oficiales de Farmacéuticos de España. Madrid 2006.
Charlson, M. E., Pompei, P., Ales, K. L., & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40, 373–383.
Chocron Bentata, L., Vilalta Franch, J., Legazpi Rodriguez, I., Auquer, K., & Franch, L. (1995). Prevalence of psychopathology at a primary care center. Atencion Primaria, 16, 586–590.
Dolan, P. (1996). Modelling valuation for health states: The effect of duration. Health Policy, 38, 189–203.
Fricchione, G. (2004). Clinical practice. Generalized anxiety disorder. New England Journal of Medicine, 351, 675–682.
Gilks, W. R., Richardson, S., & y Spiegelhalter, D. J. (1996). Markov chain Monte Carlo in practice. London: Chapman and Hall.
Goldberg, D., & Lecrubier, Y. (1995). Form and frequency of mental disorders across centres. In T. Üstün & N. Sartorius (Eds.), Mental illness in general health care: An international study (pp. 323–334). New York: Wiley.
Hamilton, M. (1959). The assessment of anxiety states by rating. British Journal of Medical Psychology, 32, 50–55.
Haro, J. M., Salvador-Carulla, L., Cabases, J., Madoz, V., & Vazquez-Barquero, J. L. (1998). Utilisation of mental health services and costs of patients with schizophrenia in three areas of Spain. British Journal of Psychiatry, 173, 334–340.
INE. (2006). Encuesta trimestral de coste laboral. Notas de Prensa. September 20, 2006. Available from: http://www.ine.es/daco/daco42/etcl/etcl0206.pdf. Accessed 28 January 2007.
Lieb, R., Becker, E., & Altamura, C. (2005). The epidemiology of generalized anxiety disorder in Europe. European Neuropsychopharmacology, 15, 445–452.
Lobo, A., & Campos, R. (1997). Los trastornos de ansiedad en atención primaria. Madrid: EMISA.
Lobo, A., Chamorro, L., Luque, A., et al. (2002). Validation of the Spanish versions of the Montgomery-Asberg depression and Hamilton anxiety rating scales. Medicina Clinica (Barc), 118, 493–499.
Lopez-Bastida, J., Serrano-Aguilar, P., & Duque-Gonzalez, B. (2004). Socio-economic costs of mental health in the Canary Islands, Spain, in 2002. Atencion Primaria, 34, 32–37.
Marciniak, M., Lage, M. J., Landbloom, R. P., Dunayevich, E., & Bowman, L. (2004). Medical and productivity costs of anxiety disorders: Case control study. Depress Anxiety, 19, 112–120.
NIMH. (2005). Generalized anxiety disorder (GAD). http://www.nimh.nih.gov/health/topics/generalized-anxiety-disorder-gad/index.shtml. Updated 2005. Accessed 21 Nov 2005.
O’Hagan, A., & Stevens, J. W. (2001). A framework for cost-effectiveness analysis from clinical trial data. Health Economics, 10, 303–315.
Peiro, S., Gomez, G., Navarro, M., Guadarrama, I., & Rejas, J. (2004). Psychosp Group. Length of stay and antipsychotic treatment costs of patients with acute psychosis admitted to hospital in Spain. Description and associated factors. The Psychosp study. Social Psychiatry and Psychiatric Epidemiology, 39, 507–513.
Quan, H., Sundararajan, V., Halfon, P., et al. (2005). Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care, 43, 1130–1139.
Saldivia Borquez, S., Torres Gonzalez, F., Cabases Hita, J. M., & PSICOST Group. (2005). Estimation of mental health care cost units for patients with schizophrenia. Actas Españolas de Psiquiatría, 33, 280–285.
Salvador-Carulla, L., Haro, J. M., Cabases, J., Madoz, V., Sacristan, J. A., Vazquez-Barquero, J. L., et al. (1999). Service utilization and costs of first-onset schizophrenia in two widely differing health service areas in north-east Spain. Acta Psychiatrica Scandinavica, 100, 335–343.
Salvador-Carulla, L., Segui, J., Fernandez-Cano, P., & Canet, J. (1995). Costs and offset effect in panic disorders. British Journal of Psychiatry Supplement, 27, 23–28.
Sicras, A., Rejas, J., Arco, S., et al. (2005). Prevalence, resource utilization and costs of vascular dementia compared to Alzheimer’s dementia in a population setting. Dementia and Geriatric Cognitive Disorders, 19, 305–315.
SOIKOS Database. (2005). SOIKOS, Centro de Estudios en Economía de la Salud y Política Social. Base de datos de costes sanitarios. Versión 2.2. Barcelona 2005. http://www.soikos.com.
Souetre, E., Lozet, H., Cimarosti, I., et al. (1994). Cost of anxiety disorders: Impact of comorbidity. Journal of Psychosomatic Research, 38(Suppl 1), 151–160.
Spiegelhalter, D. J., Thomas, A., Best, N., & y Lunn, D. (2003). “WinBUGS user manual”, Biostatistic Unit, Cambrige, UK. http://www.mrc-bsu.cam.ac.uk/bugs.
Vazquez-Polo, F. J., Negrin, M., Cabases, J. M., Sanchez, E., Haro, J. M., & Salvador-Carulla, L. (2005). An analysis of the costs of treating schizophrenia in Spain: A hierarchical bayesian approach. Journal of Mental Health Policy and Economics, 8, 153–165.
Wittchen, H. U. (2002). Generalized anxiety disorder: Prevalence, burden, and cost to society. Depress Anxiety, 16, 162–171.
Wittchen, H. U., Zhao, S., Kessler, R. C., & Eaton, W. W. (1994). DSM-III-R generalized anxiety disorder in the national comorbidity survey. Archives of General Psychiatry, 51, 355–364.
World Health Organization. (1992). ICD-10: The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines, Geneva.
Acknowledgments
This study was funded by Pfizer Spain.
Conflict of interest
One of the authors, J. Rejas, is employed by Pfizer Spain. The other authors have no conflict of interests nor have they received fees or honoraria as a consequence of the study or manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rovira, J., Albarracin, G., Salvador, L. et al. The Cost of Generalized Anxiety Disorder in Primary Care Settings: Results of the ANCORA Study. Community Ment Health J 48, 372–383 (2012). https://doi.org/10.1007/s10597-012-9503-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-012-9503-4