Abstract
Assertive Community Treatment (ACT) is an outreach-based case management model that assists people with severe mental illness through an intensive and integrated approach. In this program, a multidisciplinary team provides medical and psychosocial services. The purpose of this study was to examine the effectiveness of the following two ACT intervention strategies: “replacement” (supporting the clients) versus “backup” (supporting family members who provide care to clients). Admission days, psychiatric symptoms, quality of life, self-efficacy, and service satisfaction ware evaluated as outcome variables. To identify effective methods of supporting family members, clients living with family were divided into two groups based on the amount and types of services received—the backup group and the replacement group. ANCOVA was used to compare the outcomes between the two groups. The replacement group displayed significantly better psychiatric symptoms, social functioning, self-efficacy, and service satisfaction scores. No differences in admission days or quality of life were found. Clients provided more support directly to clients themselves than to family members was found to have better client outcomes in improving psychiatric symptoms, social functioning, and self-efficacy, resulting in higher levels of service satisfaction. This indicates that society should reduce the responsibility of the family and share responsibility for the care of people with mental illness to effectively improve outcomes for people with mental illnesses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Japan has the highest ratio of beds devoted to psychiatric patients in the world (2.8 beds per 1,000 persons in 2006) (OECD 2008). Effective methods of enriching community care for persons with mental illnesses have been explored. In May 2003, the first experimental adoption of Assertive Community Treatment (ACT) was initiated at the National Center of Neurology and Psychiatry in Chiba, Japan (Horiuchi et al. 2006; Ito et al. 2009, 2011).
The ACT model is an outreach-based psychosocial case management model that has been implemented in the United States for the past 30 years. ACT has been shown to effectively increase social functioning and decrease the length of hospital stays for persons with severe mental illnesses (Marshall and Lockwood 2000; Stein and Test 1980; Test and Stein 1980; Weisbrod et al. 1980).
The consideration of Japanese cultural concepts is important in disseminating ACT in a social context that differs from Western countries. One of the essential components of ACT that reflects Japanese culture is family support. Historically, family members have played an important role in the community care of people with severe mental illnesses in Japan (Oshima and Ito 2003).
In Japan, family members of ACT clients have expressed anxiety about the future. They fear that they may not be able to provide care for the mentally ill family member and hope that ACT will provide care similar to what is currently being provided by the family. When family members are able to provide care for clients, they often do not require ACT services, especially components such as assistance with daily living tasks, financial management, and housing services (Sono et al. 2007b, 2008).
Services provided through ACT have been associated with a decrease in family members’ burden of care and self-esteem regarding their care-giving abilities. Therefore, past research has suggested that ACT practitioners must pay increased attention to the autonomy and empowerment of the clients’ family members (Sono et al. 2007a).
Few studies have focused on the support that ACT provides families or the effects of family support on client outcomes. In order to resolve these issues, the current study addresses two questions. First, what type and how much service does ACT provide to the clients? Second, what type of family support is more effective in producing positive client outcomes?
Methods
Settings
The ACT program is operated jointly by the National Institute of Mental Health and Kohnodai Hospital, which is an acute-care hospital located in a suburban area near Tokyo. The National Center of Neurology and Psychiatry of Japan is located in this facility. The program’s catchment areas are the three adjacent cities, which represent a total population of approximately 1,500,000. When the program began, the multi-disciplinary team was composed of 12 case managers, including nurses, psychiatric social workers, psychologists, and a full-time psychiatrist.
This ACT program’s fidelity to the original ACT model was measured using the Dartmouth Assertive Community Treatment Scale (DACTS) (Bond and Salyers 2004; McGrew et al. 1994; Salyers et al. 2003; Teague et al. 1998). DACTS items are divided into the following three subscales: Human Resources, Organizational Boundaries, and Nature of Services. Scores range from 1 = not implemented to 5 = fully implemented. The average score of the research period for this ACT was 3.8 (i.e., 76% Implementation). When excluding three items related to dual diagnosis (which is uncommon in Japan), there was a consistently low item rating of 1, with an average score of 4.3 (i.e., 86% Implementation). Thus, this ACT program appears to be well-implemented and in line with international standards.
The present study was approved by the Research Ethics Board of the University of Tokyo Graduate School of Medicine and the Faculty of Medicine as well as by the Research Ethics Board of the National Center of Neurology and Psychiatry.
Procedures
The schedule of data collection was as follows:
-
T0: Date of discharge of the index admission, or the day when informed consent was obtained (if informed consent was obtained after discharge of the index admission). The clients completed self-report questionnaires and, interviews conducted by research staff
-
T1: Twelve months after T0, the survey used at T0 was re-administered.
A daily service log and socio-demographic data from T0 to T1 were obtained on a continuous basis.
Subjects
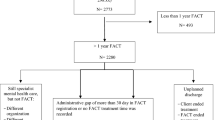
Of the 2,860 patients that were newly admitted to the psychiatric wards at Kohnodai Hospital between May 1, 2003 and October 31, 2007, 257 met the entry criteria for the program (see below). Of these eligible patients, 161 provided written informed consent to the research contents and ethical considerations, including their privacy rights. From May 1, 2003 to April 30, 2004, a pilot study of 43 clients was conducted. On May 1, 2004, a randomized controlled trial was initiated. In total, 118 clients were randomized; 59 clients were assigned to the intervention group and 59 clients were assigned to the control group. The control group received hospital-based psychiatric and psychosocial rehabilitation services and was excluded from the current analysis. The ACT team provided services to 102 clients. In other words, those who participated during the pilot study and those who were assigned to the intervention group of the randomized controlled trial received ACT services. The data presented here are from 99 clients (3 clients were excluded because they had not been discharged, or 1 year had not passed since discharge). The data used for the main analysis of this study are from 76 clients who live with their families. All of the 76 clients completed the T0 survey, and 36 declined the follow-up interview. Therefore, the response rate for T1 was 56.8% in the replacement group and 46.9% in the backup group. The flow chart is presented in Fig. 1.
The entry criteria were as follows:
-
1.
Aged 18–59 years;
-
2.
Resident of one of the three cities in the ACT program’s catchment area;
-
3.
Primary diagnosis of either schizophrenia (F2x), mood disorder (F3x), or neurotic disorder (F4x), defined by ICD-10 (WHO 1992), excluding those who had a primary diagnosis of mental retardation, dementia, substance/alcohol abuse, or personality disorders;
-
4.
Frequent psychiatric service utilization (2 or more hospitalizations, 100 or more inpatient days, or 3 or more psychiatric emergency room visits) or refusal of psychiatric service utilization (3 months or more no-show to outpatient clinics) in the last 2 years;
-
5.
Low level of social functioning in the previous year (at best, a GAF score of less than 50).
Clients with schizophrenia or mood disorders had to meet either criteria 4 or 5; clients with other disorders had to meet both criteria 4 and 5.
Table 1 shows the basic client characteristics. The average age was 39.4 years old, and the average age of onset of mental illness was 24.0 years old. Of the clients, 76.8% were living with their families. The majority of clients (73.7%) were diagnosed with schizophrenia or related disorders.
Variables
Processes
Daily service log: ACT staff used a computerized daily service log system to record and share clinical service information. The log data contained the date, time, duration, place, client, staff, and service codes of each contact. Service codes included 14 codes such as “Medical support for psychiatric symptoms”, “Social life support”, and “Family support”, which were chosen based on expert opinions, literature on ACT, and existing scales (see Table 2). All service codes were listed in the database, and ACT staff members were asked to mark all that apply for each client on a daily basis. Data on services provided between T0 and T1 were used for each case. Only data on direct (face-to-face) contact were used; contacts through telephone, fax, or email were excluded.
Outcome Assessment Scales
The Brief Psychiatric Rating Scale (BPRS) (Kolakowska 1976; Overall and Gorham 1962): The BPRS is an 18-item scale with subscales for positive symptoms, negative symptoms, depression, mania, and hypochondria. The BPRS was administered by a trained rater, and each item was scored on a seven-point severity scale (the higher the number, the more severe the symptom), with a total score ranging from 18 to 126. A Japanese translation of the BPRS was provided and validated by Kitamura et al. (1990).
Quality of Life Interview (QOLI) (Lehman 1988): QOLI is a comprehensive questionnaire developed by Lehman to objectively assess living situation and subjectively assess life satisfaction. The Japanese translated version of the QOLI was validated by Oka et al. (unpublished). The scale has eight subscales that are scored from 1 to 7 (housing, leisure activities, family relationships, social relationships, finances, safety, health, and global well-being), with higher scores indicating a higher Quality of Life (QOL).
Global Assessment of Functioning (GAF) (Phelan et al. 1994): The Global Assessment of Functioning (GAF) is a numeric scale (0 through 100; higher scores indicating higher functioning) used to rate the social, occupational, and psychological functioning of adults. The scale is presented and described in the DSM-IV-TR (American Psychiatric Association 2000). The GAF was translated into Japanese by Takahashi et al. (American Psychiatric Association translated by S Takanashi 2002).
Self-Efficacy for Community Living (SECL): The SECL is a self-report questionnaire designed to measure the self-efficacy of those with mental illnesses in the areas of daily life and function in the community. The scale has 18 items. Each item is rated on an 11-point scale, ranging from 0 (“I have no confidence at all”) to 10 (“I am absolutely confident”). The sum of these scores is defined as SECL. The reliability and validity of this scale were previously established by Okawa et al. (2001).
Client Satisfaction Questionnaire-8 (CSQ-8) (Larsen et al. 1979): The CSQ-8 is an 8-item scale that assesses client satisfaction with treatment, with scores ranging from 1 to 4. The CSQ-8 is scored by summing the individual item scores to produce a range of 8–32, with higher scores indicating greater satisfaction. The reliability and validity of the Japanese version of the CSQ-8 was previously established by Tachimori et al. (Tachimori and Ito 1999). In the present study, this scale was used only at T1.
Two Intervention Strategies
To identify effective methods of support given by family members, clients living with family were divided into two groups, the backup group and replacement group. In this study, “family support” includes the direct services ACT performed for family members, and the caregiver role was assumed by ACT. Therefore, “backup” refers to support given to family members who continued to care for clients, while “replacement” refers to direct support of the clients rather than support given to the family members. In general, services are provided to meet clients’ needs based on the assessment; therefore, the amount of services given depends on the clients’ needs. Because it is assumed that clients who were provided more backup services were also provided more replacement services and vice versa, the Z score of the amount of care was used to divide the clients into two groups. Using daily service log data, clients were divided into two groups as follows: the Z score of the amount of care typically provided by family (assistance with daily living tasks, finances, housing, communications, and coordination) was defined as Zreplacement, and the Z score of the amount of care ACT provided to the family was defined as Zbackup. If Zreplacement < Zbackup, clients were categorized as the backup group; if Zbackup < Zreplacement, they were categorized as the replacement group.
Analysis
To compare the outcomes at T1 between the replacement and backup groups, ANCOVA was used. Differences between the two groups were demonstrated by taking each outcome scale score at T0 and the GAF at T0 as the covariate. Statistical calculations were performed using SPSS version 11.5 J.
The authors declare that they have no known conflicts of interests.
Results
The most frequently provided service component was medical support for psychiatric symptoms (56.7 times, 53.2 h per year per client). Assistance with social life (28.8 times, 33.5 h) and family support (15.2 times, 19.5 h) were more frequently provided than the remaining services (see Table 2).
Table 3 shows differences between the replacement and backup groups with respect to the clients’ basic characteristics at T0, the services provided, and the outcome measures at T0. Only one significant difference was found between the two groups, with the replacement group displaying significantly higher GAF scores (t = 3.66, P < 0.01).
Table 4 shows the ANCOVA results for the outcome scales at T1. For the BRPS, the total score (F (1, 38) = 10.67, P < 0.01), the positive symptom score (F (1, 38) = 6.64, P = 0.01), the depression score (F (1, 38) = 9.67, P < 0.01), and the hypochondria score (F (1, 38) = 4.85, P = 0.03) were significantly lower in the replacement group than the same scores in the backup group. On the other hand, the GAF (F (1, 39) = 7.68, P = 0.01) and self-efficacy for community living (F (1, 33) = 4.72, P = 0.04) scores were significantly higher in the replacement group than in the backup group. According to the results of the t test, the replacement group had a higher CSQ-8 score than the backup group (t = 2.45, P = 0.02).
Discussion
ACT provided a broad range of services, including medical support for psychiatric symptoms, assistance with daily living tasks, social life, finances, and family support. It is difficult to compare the quantity of the services provided through ACT programs in other countries due to the general lack of publication of daily service logs. However, there is research on the critical ingredients of ACT based on the perspectives of ACT clinicians (McGrew et al. 2003). All of the service components rated “beneficial” by ACT clinicians, such as medication management, provision of adequate housing, provision of social support, and money management, were provided in the current ACT program. While interactions with clients’ families were given relatively low priority in previous research, support for clients’ families was one of the most frequently provided services in the present ACT program. This suggests the importance of family support in Japan.
A comparison of client outcomes between the replacement and backup groups revealed that clients provided more support directly to clients themselves than to family members was found to have better outcomes in improving the psychiatric symptoms, social functioning, and self-efficacy of clients and resulted in a higher level of client and family satisfaction with the provided services.
Better outcomes were observed in the group in which clients directly received more services related to daily living tasks. Clients had a variety of experiences with the ACT staff in the world outside of the home or hospital, resulting in increased self-efficacy and social functioning. These experiences may have contributed to the reduction of psychiatric symptoms observed in this group.
In previous research on the families of people with mental illnesses, supportive behaviors provided by the families have been shown to intensify the burden on family members and increase the difficulty of family life. Supportive behaviors include various types of activities related to providing care and support for a family member with a chronic illness, such as monitoring medication, watching for signs of relapse, and providing ongoing physical support such as providing shelter and food. For each individual family members, these activity absorb the time for a life of their own, to cope with individual concerns, and to search for self-fulfillment (Oshima 1987). Difficulties related to family life increase the Expressed Emotion (EE) score, which is an important psychosocial factor that predicts the prognosis of clients with schizophrenia or other mental illness. Providing support to the families of people with mental illnesses not only reduces family life difficulty, but also improves client prognosis (Jackson et al. 1990; Vaughn and Leff 1976).
As mentioned above, the amount of family support provided was related to the needs of the clients and the family members. The “backup group” and “replacement group” could also be described as the “exhausted family group” and “not exhausted family group”, respectively. In other words, for clients whose family members were not excessively exhausted, there was less need for support, and the services provided by ACT were directed towards the clients. This aspect of non-exhaustion for family members could be related to the better outcomes observed in the replacement group. Therefore, an assessment of the need for family support and client support is critical. When family members are exhausted, there is a greater need to reduce the burden and responsibility of family caregiving. Shifting the responsibility of client care to resources in the community is vital. Furthermore, the relationship between clients and family members is interactive. Therefore, in addition to the adequate quantified assessment of the family’s and client’s needs using a more rigorous design, it is important to focus on the reciprocal and mutual relationship between the family and client in regards to both future research and clinical practice. Additionally, it is important to assess the family provision of care.
Subjects were not randomly assigned into the replacement and backup groups; therefore, a careful interpretation of the results is necessary. However, no significant differences in baseline measures, except GAF, were found between the two groups. The baseline GAF was statistically controlled, giving this discussion a certain level of validity.
Because subjects were limited to one ACT team, the generalizability of the current study’s findings is limited. However, ACT programs share a common structure of services regardless of country, region, or culture because they are based on internationally disseminated standards. Clients are chosen based on operational entry criteria, and ACT programs are monitored using a fidelity scale. Thus, it is possible to apply the findings of this study to other ACT programs in Japan and in communities worldwide where families play a large role as caregivers.
The low response rate, especially at T1, is another important limitation of this work. Despite this limitation, the responders who were followed at T1 did not differ from the non-responders by age, sex, the total amount of provided services, or any outcome variables at T0. The low response rate is, therefore, unlikely to have affected the results.
In light of current trends in the deinstitutionalization of people with mental illnesses, the construction of a community support system is an urgent issue. The shape of the average family is rapidly changing (for example, a focus on the nuclear rather than the extended family) and the capacity of family members to care for persons with disabilities has been weakened. Inevitably, family caregivers will find it difficult to continue to play a large role in community care. To provide community-level support to people with mental illnesses, comprehensive and community-rooted outreach services will play increasingly crucial roles. In addition, effective family support during home visits is critical in Japan, as the majority of clients discharged from hospitals live with their families. The findings of the current research indicate that the ACT team must provide practical supports, such as psychoeducation and individual consultation, to family members, reduce the responsibility of the family, and take responsibility for the care of people with mental illness.
This is the first systematic evaluation study focusing on the family support activities of ACT. The results showed that families and the ACT team shared the responsibility of client care. Clients provided more support directly to clients themselves than to family members was found to produce better outcomes in improving psychiatric symptoms, social functioning, and self-efficacy, resulting in higher levels of service satisfaction. The findings of the present study indicate that society should reduce the responsibility of the family and take responsibility for the care of people with mental illness to effectively improve outcomes for people with mental illnesses.
References
American Psychiatric Association. (2002). Diagnostic and statistical manual of mental disorders: DSM-IV-TR (translated by S. Takanashi, Y. O., T. Someya). Tokyo: Igaku Syoin.
American Psychiatric Association (APA), American Psychiatric Association Task Force on DSM-IV. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Association.
Bond, G. R., & Salyers, M. P. (2004). Prediction of outcome from the Dartmouth assertive community treatment fidelity scale. CNS Spectrums, 9(12), 937–942.
Horiuchi, K., Nisihio, M., Oshima, I., Ito, J., Matsuoka, H., & Tsukada, K. (2006). The quality of life among persons with severe mental illness enrolled in an assertive community treatment program in Japan: 1-year follow-up and analyses. Clinical Practice and Epidemiology in Mental Health, 2, 18.
Ito, J., Oshima, I., Nishio, M., & Kuno, E. (2009). Initiative to build a community-based mental health system including assertive community treatment for people with severe mental illness in Japan. American Journal of Psychiatric Rehabilitation, 12(3), 247–260.
Ito, J., Oshima, I., Nishio, M., Sono, T., Suzuki, Y., Horiuchi, K., et al. (2011). The effect of assertive community treatment in Japan. Acta Psychiatrica Scandinavica, 123(5), 398–401.
Jackson, H. J., Smith, N., & McGorry, P. (1990). Relationship between expressed emotion and family burden in psychotic disorders: An exploratory study. Acta Psychiatrica Scandinavica, 82, 243–249.
Kitamura, T., Yuzuriha, T., Morita, M., Ito, J., Suga, R., & Nakagawa, Y. (1990). Oxford version of BPRS: Development and validation of subscales. Archives of Psychiatric Diagnostics and Clinical Evaluation, 1(1), 101–107.
Kolakowska, T. (1976). Brief psychiatric rating scale. Glossaries and rating instructions. Oxford: Oxford University.
Larsen, D. L., Attkisson, C. C., Hargreaves, W. A., & Nguyen, T. D. (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2(3), 197–207.
Lehman, A. (1988). A quality of life interview for the chronically mentally ill. Evaluation and Program Planning, 11(1), 51–62.
Marshall, M., & Lockwood, A. (2000). Assertive community treatment for people with severe mental disorders. Cochrane Database of Systematic Reviews, 2000(2), CD001089.
McGrew, J. H., Bond, G. R., Dietzen, L., & Salyers, M. (1994). Measuring the fidelity of implementation of a mental health program model. Journal of Consulting and Clinical Psychology, 62(4), 670–678.
McGrew, J. H., Pescosolido, B., & Wright, E. (2003). Case managers’ perspectives on critical ingredients of assertive community treatment and on its implementation. Psychiatric Services, 54(3), 370–376.
Okawa, N., Oshima, I., Cho, N., Makino, H., Oka, I., Ikebuchi, E., et al. (2001). Development of ‘self-efficacy for community life scale’ for people with Schizophrenia: Its reliability and validity. Seishin Igaku, 43(7), 727–735.
Organization for Economic Co-operation and Development (OECD), Institute for Research and Information in Health Economics. (2008). OECD health data 2008. Paris: Organization for Economic Co-operation and Development.
Oshima, I. (1987). A study on the family support system for the mentally disabled from the perspective of its function and resources. The Japanese Journal of Psychiatry and Neurology, 89, 204–241.
Oshima, I., & Ito, J. (2003). Care management for people with schizophrenia: Focusing on ACT. Japanese Journal of Biological Psychiatry, 14, 29–34.
Overall, J. E., & Gorham, D. R. (1962). The brief psychiatric rating scale. Psychological Reports, 10, 790–812.
Phelan, M., Wykes, T., & Goldman, H. (1994). Global function scales. Social Psychiatry and Psychiatric Epidemiology, 29(5), 205–211.
Salyers, M. P., Bond, G. R., Teague, G. B., Cox, J. F., Smith, M. E., Hicks, M. L., et al. (2003). Is it ACT yet? Real-world examples of evaluating the degree of implementation for assertive community treatment. The Journal of Behavioral Health Services & Research, 30(3), 304–320.
Sono, T., Nishio, M., Suzuki, Y., Oshima, I., Fukaya, H., Horiuchi, K., et al. (2007a). Effects of assertive community treatment on families of people with severe mental illness in Japan—An analysis of self-report questionnaire using a quasi-experimental method. Australian and New Zealand Journal of Psychiatry, 41(S2), A359–A432.
Sono, T., Oshima, I., & Ito, J. (2007b). Needs for assertive community treatment of families of people with severe mental illness and their structure. Japanese Bulletin of Social Psychiatry, 16, 29–37.
Sono, T., Oshima, I., & Ito, J. (2008). Family needs and related factors in caring for a family member with mental illness: Adopting assertive community treatment in Japan where family caregivers play a large role in community care [regular article]. Psychiatry and Clinical Neurosciences, 62, 584–590.
Stein, L. I., & Test, M. A. (1980). Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Archives of General Psychiatry, 37(4), 392–397.
Tachimori, H., & Ito, H. (1999). Reliability and validity of Japanese version of client satisfaction questionnaire-8. Seishin Igaku, 41(7), 711–717.
Teague, G. B., Bond, G. R., & Drake, R. E. (1998). Program fidelity in assertive community treatment: Development and use of a measure. The American Journal of Orthopsychiatry, 68(2), 216–232.
Test, M. A., & Stein, L. I. (1980). Alternative to mental hospital treatment. III. Social cost. Archives of General Psychiatry, 37(4), 409–412.
Vaughn, C. E., & Leff, J. P. (1976). The influence of family and social factors on the course of psychiatric illness. British Journal of Psychiatry, 129, 125–137.
Weisbrod, B. A., Test, M. A., & Stein, L. I. (1980). Alternative to mental hospital treatment. II. Economic benefit-cost analysis. Archives of General Psychiatry, 37(4), 400–405.
WHO. (1992). The international classification of diseases and health related problems tenth revision. Geneva: World Health Organization.
Acknowledgments
This research was part of a project supported by grant H14-Kokoro-009 and H17-Kokoro-006 from the Ministry of Health, Labor, and Welfare of Japan. I am grateful to the members of the ACT clinical team, research team, and the clients who made the evaluation possible. I would also like to thank Norito Kawakami and Wakate Kai, who were important advisors during the work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sono, T., Oshima, I., Ito, J. et al. Family Support in Assertive Community Treatment: An Analysis of Client Outcomes. Community Ment Health J 48, 463–470 (2012). https://doi.org/10.1007/s10597-011-9444-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-011-9444-3