Abstract
This paper aims to improve the accuracy of standard compartment models in modeling the dynamics of an influenza pandemic. Standard compartment models, which are commonly used in influenza simulations, make unrealistic assumptions about human behavioral responses during a pandemic outbreak. Existing simulation models with public avoidance also make a rigid assumption regarding the human behavioral response to influenza. This paper incorporates realistic assumptions regarding individuals’ avoidance behaviors in a standard compartment model. Both the standard and modified models are parameterized, implemented, and compared in the research context of the 2009 H1N1 influenza outbreak in Arizona. The modified model with heterogeneous coping behaviors forecasts influenza spread dynamics better than the standard model when evaluated against the empirical data, especially for the beginning of the 2009–2010 normal influenza season starting in October 2009 (i.e., the beginning of the second wave of 2009 H1N1). We end the paper with a discussion of the use of simulation models in efforts to help communities effectively prepare for and respond to influenza pandemics.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The 2009 H1N1 influenza outbreak was the most recent influenza pandemic, following previous outbreaks in 1968, 1957, and 1918 (the year of the Spanish Flu). The Obama Administration declared a public health emergency in response to the 2009 H1N1 outbreak in April 2009 and a national emergency in October 2009. This recent influenza pandemicFootnote 1 does not exclude the possibility of another novel virus-caused influenza outbreak. The former Centers for Disease Control and Prevention (CDC) Director, Julie Gerberding, said in April 2007: “We know that a pandemic will eventually occur. We always say it’s not a question of if; it’s a question of when” (Ulene 2007). To minimize the impact of pandemic influenza, both the CDC and Department of Health and Human Services have made pandemic preparedness and response efforts a priority for public managers at all levels (Das et al. 2008; Ferguson et al. 2005). One prerequisite for effective planning and intervention for influenza pandemic situations is to accurately forecast the epidemic’s spread dynamics. Although such foresight efforts are dependent upon many factors, the focus of this paper is on incorporating the public’s response to risk information in influenza pandemic simulations.
When health emergencies such as an H1N1 influenza outbreak occur, two crucial intervention strategies are: providing medical countermeasures such as vaccines, and non-medical countermeasures such as social distancing and improving people’s protective behavior through risk communication. Several previous influenza pandemic simulations have attempted to determine the effect of vaccination on changes in the dynamics of the epidemic process (Lee et al. 2010a; Patel et al. 2005; Cowling et al. 2009), but much less work has been focused on the behavioral response to pandemic situations. Behavioral intervention is particularly important during the early stages of novel pandemic influenza outbreaks because it may be the only intervention strategy available for emergency managers until antiviral measures are developed and distributed. Since the last major influenza pandemic in 1968, technological advances such as the use of the Internet and other communication channels have been used to inform the public of health risks. This increased access to health information may, in turn, reduce flu transmission after the public is informed of the risk and as a result engages in risk-avoiding behaviors. Such a public response can greatly reduce the impacts of a pandemic. Our study supports the argument that accounting for human response behavior in the context of influenza pandemic simulation is crucial because standard compartment models that do not consider such behavioral changes are likely to overestimate the impact of a pandemic. However, how this behavioral component is included in influenza pandemic simulations is also important.
This paper focuses on a system dynamics model to simulate the 2009 H1N1 influenza progression in Arizona during the 2009–2010 normal influenza season. The model is structured with public risk avoidance behaviors as mitigating factors in human-to-human disease transmission. We first review the development of compartment mathematical models to simulate the spread dynamics of pandemic influenza within a population. We then explain how we incorporate the specific local conditions present during the outbreak into the revised model, including the public’s protective actions. We further conduct sensitivity analyses of uncertain parameters that can influence the spread dynamics of influenza in the community (i.e., the percent of the immune population and the case detection rate). We end the paper with a discussion of how simulation models can be further expanded for emergency preparedness and response during the influenza pandemic.
2 Influenza pandemic simulations
2.1 Use of compartment models
Classical compartmental epidemiology models have been used for decades to conceptualize and forecast the spread dynamics of infectious diseases such as influenza (Kermack and McKendrick 1927, 1932, 1933). In the SIR model of Kermack and McKendrick (and some of its variations such as SEIR, SEI, and SIS), the total population is divided into several subdivisions, called compartments, depending on their disease status (e.g., susceptible, infected, and recovered). A system of coupled ordinary differential equations defines the transition rates of individuals moving from one compartment to the next, and the spread condition of infectious disease in the population is then dynamically simulated as the solution to this system.
The most widely debated and critical assumption in any epidemic simulation using compartment models is the definition of a single “transmission event,” where it is assumed that two individuals are within close enough proximity for an infected person to transmit the virus to a susceptible host. In reality, the “transmission event” can be quite varied. In the case of airborne pathogens such as influenza, viruses can be suspended in air, so infection can occur through direct physical contact such as a handshake or through close physical proximity, such as in the case of sneezing or coughing. It can also occur through other transmission mechanisms (such as touching doorknobs or handling money) that do not require two individuals to be in the same location at the same time. Therefore, while the compartment model has been frequently used to study influenza epidemics, it has also been criticized because it is too simple to provide insightful information on influenza pandemic, as it ignores human behavioral responses (i.e., avoiding public gatherings and washing hands more frequently) to the potential threat of the disease.
This critique is fair, but not necessarily attributable to the compartmental structure of the model. Rather, understanding and modeling human responses to the risk of influenza requires more accurate information about the extent to which individuals can avoid transmission events. For example, classical compartment models assume “standard incidence,” where individuals do not change their behavior during an epidemic but continue their regular activities as usual. However, empirical studies have reported that people do change their behavior, especially in pandemic situations (Ekberg et al. 2009; Lau et al. 2003, 2007). When confronted with the threat of an influenza pandemic, people undertake actions to protect themselves from infection, and those taking protective actions continue these coping behaviors during the epidemic (Leung et al. 2003; de Zwart et al. 2010).
The limitations of basic compartment models have led to the introduction of the concept of prevalence elastic behavior, which refers to the adaptive actions people take in response to an epidemic (Philipson 2000; Philipson and Posner 1993). More recent studies on pandemic-related estimation incorporate this notion into epidemic models by substituting the classic standard incidence assumption along with the “mass action incidence” assumption (Larson and Nigmatulina 2009). People are assumed to reduce their overall social activities due to a pandemic, and the reduction is based on the propagation condition of the disease. A response such as foregoing contact with other people is also called an “avoidance response” (Lau et al. 2010; Yoo et al. 2010). For example, instead of assuming a constant value for the contact rate (which is the same as that on normal days), Larson and Nigmatulina (2009) include this parameter as a variable in their model, where its value is less than the normal contact rate and is simultaneously dependent upon the size of the remaining non-infected population in circulation.
The incorporation of public avoidance behavior has the potential to make these modified compartment models more accurate in anticipating pandemic influenza spread dynamics (Epstein et al. 2008). However, these models oversimplify human response, just as in the classical compartment model. While the basic model completely ignores the avoidance response, the modified model simply assumes that the total population reduces daily contact for self-protection, which the public risk communication literature has shown is far from reality. People who are the potential target of some risk are informed (through risk communication) of the risk and available protective actions. After receiving the information, they respond by taking a variety of actions, including continuing with normal activities as if no risk exists (Quarantelli 1983). Not all individuals respond by taking protective actions after knowing the existence of some risk. Therefore, the assumption that the total population may reduce daily contact for self-protection requires further scrutiny. Simulation models based on such an assumption may underestimate pandemic impacts.
In this paper, we suggest that one way to address the overestimation of the classical compartment model and the underestimation of the existing public avoidance model is to consider heterogeneity in people’s response to health risk information. This may provide a better understanding of the progress of an epidemic, especially during the period where antiviral measures are not readily available and risk communication strategies are actively used by emergency managers. Based on the previous literature, three behavioral assumptions during novel influenza outbreaks are made: even if risk information is available, not all individuals undertake risk avoidance behaviors (Bults et al. 2011; Jones and Salathe 2009); the proportion of individuals engaged in avoidance behaviors is influenced by a disease prevalence during the epidemic (Larson and Nigmatulina 2009); and once people undertake avoidance behaviors, they continue the coping behavior until the epidemic ends (Leung et al. 2003; de Zwart et al. 2010). In Sect. 2.2 we explain how a classical compartment model can be modified to incorporate these behavioral assumptions in pandemic simulations.
2.2 Modeling the dynamics of an influenza pandemic
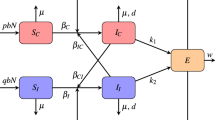
Figure 1(a) presents the standard Susceptible-Exposed-Infected-Removed (SEIR) model frequently used in epidemiologic modeling. SEIR is a refined model of Susceptible-Infected-Removed (SIR), and has been adopted in previous studies for the simulation of 2009 H1N1 influenza spread (Balcan et al. 2009; Halder et al. 2010). This model successfully captures the disease progression process of H1N1 influenza because it considers “exposed” status individuals (Li et al. 1999; Rost and Wu 2008).
In the SEIR model, the four compartments represent four health statuses relative to an epidemic. The first compartment is Susceptible (S), or those in the population who are healthy and can be infected by the disease. Exposed (E) includes those in the population who have been infected and may be infectious, but have not shown any disease symptom. Note that E′ is the population belonging to E who are infectious (e.g., in the case of 2009 H1N1, E′ are those who are on the last day of the latent period). The third group is Infected (I), or the population who are both infectious and symptomatic. Lastly, Removed (R) includes people who either recover from the disease (Re) or die when they are in infected status (D). Here we assume that the deaths only come from the infected compartment (Araz et al. 2011). Recovered individuals are usually assumed to acquire full immunity to subsequent infection, so these individuals never re-enter the susceptible population (Larson and Nigmatulina 2009; Yoo et al. 2010).
At each time step, individuals can move from one compartment to the next, as shown in Fig. 1(a). The transition rates of movement between two adjacent compartments are defined by the following set of ordinary differential equations:






The left part of the equal sign in each equation represents the change in the number of people in each compartment in a time step, while the right part shows how to calculate the change using other parameters. In Eq. (1), for example, the change in the susceptible population due to those who transit to the exposed status per time step is decided by the infection rate (α), the contact (mixing) rate β, the susceptible population size (S), and the fraction of infectious people among the total population ((E′+I)/N). The infection rate is the probability of a susceptible individual getting infected after having contact with an infectious individual. The contact rate is the average number of people each person contacts per day.
In Eq. (2), σ represents the progression rate from E to I, whose reciprocal (σ −1) is the latent period, or the time period between exposure to the disease and the time at which the disease becomes apparent through symptoms. The product of σ and E represents the number of exposed individuals who enter the infected compartment per time step. With the number of the susceptible who move to the exposed compartment (Eq. (1)), the product of σ and E determines the size change of the exposed population per time step. As mentioned above, some of the exposed are infectious and some are not. The number of the exposed and infectious population is based upon the exposed (E), the latent progression rate (σ), and a parameter ω (Eq. (3)). ω is part of the latent period, and represents the time period during which exposed individuals remain in a state of being infectious.
In Eq. (4), two groups of individuals move out of the infected compartment per time step. One group includes those who recover from the disease. The size of this group is equal to the product of the infected population size (I) and the recovery rate (γ), whose reciprocal is the infected period (γ −1) or the period between the moment an individual becomes symptomatic and the moment the individual recovers from the disease (Eq. (5)). The other group refers to those who died due to the disease. Its size equals the product of the infected population size (I) and the mortality rate (μ) (Eq. (6)). Therefore, the change in the size of the infected compartment per time step is calculated by subtracting the size of both groups from the number of exposed people who transit into infected status at this time step.
2.3 Structuring a population with heterogeneous coping behaviors
The SEIR model is modified in order to incorporate the response of humans to health risk information during the pandemic influenza outbreak. Figure 1(b) shows the schematic of the modified SEIR model. The total population is divided into two subpopulations: the population of individuals who engage in avoidance behaviors and the population of individuals who do not. The standard four-compartment model is then modified into an eight-compartment model, including the susceptible who engage (S a ) and do not engage (S na ) in avoidance behavior, the exposed who engage (E a ) and do not engage (E na ) in avoidance behavior, the infected who engage (I a ) and do not engage (I na ) in avoidance behavior, the recovered (Re), and those who died (D).
The decision to introduce heterogeneity in people’s response behaviors into the classical compartment model primarily influences the contact rate (β), a key parameter in the SEIR model. Avoidance behavior reduces the contact rate among people engaging in taking such actions, and the avoidance behavior effect (ϕ) is set to represent the reduction in the contact rate due to such behavior. Previous researchers estimate that the effective contact rate, which is the product of the infection rate (α) and the contact rate (β), could be reduced by 30–90 % through the early implementation of non-pharmaceutical pandemic mitigation measures such as social distancing (Jefferson et al. 2008; Larson and Nigmatulina 2009). We hypothesize that the infection rate in the SEIR model is a constant representing the biological features of the disease, so avoidance behavior could reduce the contact rate by 30–90 %. Avoidance behavior does not influence the values of other parameters such as the latent and infected periods of those already infected (i.e., the latent and infected periods remain the same regardless of whether exposed or infected people engage in avoidance behavior).
New infections occur when susceptible individuals (S) are infected by an infectious individual who may not show disease symptoms (E′) or may show disease symptoms (I). Given the different contact rates resulting from individuals’ choices regarding avoidance behavior, four influenza virus transmission mechanisms can be structured, as presented in the following matrix β.
where β na,na represents influenza virus transmission between susceptible individuals who are not engaging in avoidance behavior and those who are infectious and also not engaging in avoidance behavior. The contact rate in a normal situation (β 0) is used to represent the contact rate between these two groups of people because neither is engaging in avoidance behavior. β a,na and β na,a capture (a) the interaction between susceptible people engaging in avoidance behavior and infectious people not engaging in such behavior, and (b) the interaction between susceptible people not engaging in avoidance behavior and infectious people engaging in such behavior, respectively. Assuming that only one side engages in avoidance actions, the contact rates are of the same value and assigned as ϕβ 0. Finally, β a,a represents virus transmission to susceptible individuals who are engaging in avoidance behaviors from infectious individuals who are also engaging in avoidance behaviors, and has the smallest magnitude of the contact rate (ϕ 2 β 0) because people in both interaction compartments reduce their contact rate.
Using this matrix, the rate equations that represent the population change in the susceptible and exposed compartments among the avoidance behavior takers and non-takers are specified as below. Other rate equations remain unchanged from the standard SEIR model.




In this modified model, the percent of the susceptible taking avoidance action at each time step is determined by the percent of susceptible population engaging in avoidance behavior at time 0 and disease prevalence in the system. Disease prevalence indicates the severity of the disease spread condition in the system. Adopting Larson and Nigmatulina’s (2009) measurement, disease prevalence at time t can be captured as
where N active represents the population of healthy individuals (susceptible or recovered) at a single time point. Here it is assumed that the percent of the susceptible population engaging in avoidance actions increases as the disease becomes more prevalent (Lau et al. 2007; Leung et al. 2003). The increase in the proportion of the susceptible taking avoidance actions due to disease prevalence influences the size of the S a and S na compartments over time, and as a result influences the number of people in the remaining compartments. Therefore, there is a feedback loop among the percent of the susceptible population engaging in avoidance actions, disease prevalence, and the population size in each compartment. Once individuals move to S a from S na , it is assumed that they continue their avoidance behaviors during the pandemic as found in de Zwart et al. (2010).
In Sect. 3, we implement the classical and modified models to simulate the epidemic process in the context of the second wave of the 2009 H1N1 flu outbreak in Arizona. We paid particular attention to the early dynamics of the epidemic before a vaccine was widely available because behavioral response can have a significant impact on the epidemic process (CDC 2010c).
3 2009 H1N1 influenza pandemic in Arizona
3.1 Research context
H1N1 influenza emerged as a new pandemic strain of influenza in April 2009. As the first global pandemic in over 40 years, it caused a substantial number of illnesses, hospitalizations, and deaths (CDC 2010a). The United States experienced its first wave of the 2009 H1N1 influenza outbreak in the spring and summer months of 2009. By June 19, all states in the United States had reported cases of 2009 H1N1 infection. The second wave occurred in the fall of 2009, with most of the nation experiencing the influenza outbreak from October to early December 2009 (Ross et al. 2010).
In Arizona, the first case of 2009 H1N1 infection was confirmed on April 29, 2009 (Shanks 2009). The second wave of the influenza outbreak began in early September 2009 and continued through the 2009–2010 normal influenza season. The Arizona Department of Health Services (ADHS) reported the number of newly infected and deceased cases each week starting on August 30, 2009. By early October 2009, a total of 2,243 people had been infected and 30 people had died from H1N1 in Arizona (ADHS 2009a).Footnote 2 Newly infected cases continued to emerge until May 2010. By the end of the 2009–2010 normal influenza season, 5,620 people in Arizona had been infected with H1N1, and the total number of deceased cases was 122. Figure 2 shows how the number of newly infected laboratory-confirmed cases in Arizona changed each week during the early stage of the 2009–2010 normal influenza season (from October 4, 2009 to January 31, 2010; and the second wave of 2009 H1N1 in Arizona; ADHS 2009b).
3.2 Data sources and simulation setup
Table 1 summarizes the parameters used in the simulation, their values, and the sources of these values. Parameters related to the epidemic characteristics of 2009 H1N1 influenza were collected from CDC reports and previous studies. According to the CDC, “the incubation period for influenza is estimated to range from 1 to 4 days with an average of 2 days” and “influenza virus shedding (the time during which a person might be infectious to another person) begins the day before illness onset and can persist for 5 to 7 days” (CDC 2009a). In the simulation model, we assume a latent period of 2 days and an infected period of 5 days. Another important implication from the CDC statement is that individuals in exposed status are not infectious at all times; they only begin to transmit the virus from the last day of their latent period (CDC 2009a). We assume a period of exposed and infectious (ω) of 1 day. The infection rate can be estimated based on previous findings on the basic reproduction number (R 0), which is the number of secondary infections caused by a single infectious case introduced into the susceptible population. Considering the assumption that people can only die when they are in the infected status, R 0 is equal to the product of the average contact rate, the infection rate, and the average infectious period (Keeling and Rohani 2008). The basic reproduction number of H1N1 has been estimated between 1.4 and 1.6 in Coburn et al. (2009) or between 1.3 and 1.7 in Yang et al. (2009). We use a value of 1.4 % for the infection rate, dividing 1.5 (the average estimated basic reproduction number in the studies) by the product of 21 for the average contact rate and 5 days for the average infectious period. The mortality rate for H1N1 influenza has been reported to be approximately 0.3 % (Donaldson et al. 2009; Tuite et al. 2010). Regarding the contact rate, studies on the number of interpersonal contacts have generally been based on convenience samples or data from European countries (Edmunds et al. 2006; Mossong et al. 2008), but few studies on the daily contact rate have used the US population (Destefano et al. 2010). We start the simulation using the assumption of Larson and Nigmatulina (2009) of an average daily contact rate in the United States of 21. Given previous research findings indicating an avoidance behavior effect of 30–90 % (Jefferson et al. 2008; Larson and Nigmatulina 2009), the avoidance behavior effect is assumed to be a stochastic variable that follows a truncated normal distribution, with a mean of 60 %, standard deviation of 15 %, minimum of 30 %, and maximum of 90 %.
The purpose of using the model was to simulate the 2009–2010 normal flu season (starting from October 2009), so the model was initialized with 3,280 exposed, 3,280 infected, 465,415 recovered, and 30 deceased individuals based on lab-confirmed cases at the beginning of October (ADHS 2009a) and an assumed case detection rate of 10 % (an der Heiden et al. 2009). No data are available for the estimation of the number of exposed cases, so we assumed at least the same number as the infected cases when initializing the simulation. The recovered population initially consists of two groups: some portion of the elderly population (equal to or more than 65 years old) who may have pre-existing immunity to the 2009 H1N1 influenza virus (CDC 2009b), and those who had recovered from the disease by October 3, 2009 (ADHS 2009a). Here we made a moderate assumption, initializing the simulation with 7 % of the population having pre-existing immunity (14 % of the Arizona population is elderly (ACS 2009)).
The modified SEIR model assumes that the susceptible population is categorized as those who engage in risk avoidance actions and those who do not. To initialize the model with the starting percent of people who belong to each group, we used information gathered from the Arizona population. This survey was conducted using a random-digit telephone survey of representative households in Arizona during the month of October 2009Footnote 3 (see Jehn et al. 2011). The survey contained 53 main questions and related sub-questions on respondents’ demographics, knowledge of 2009 H1N1 influenza, methods of receiving public health information, perceived risk, and whether they were engaging in protective behavior to reduce their risk of H1N1 influenza infection. Regarding the last survey item, respondents were asked to identify which precautionary measures they were taking for self-protection against 2009 H1N1 flu. Because the percentage of people who engage in avoidance behaviors is related to the contact rate in the modified model, four questions involved physical contact with others: staying away from places where large groups of people gather, stopping shaking hands, stopping hugging or kissing, and staying away from people with flu-like symptoms. It is uncertain which measure best reflects the reality of risk avoidance behavior in this population, so rather than using the percent of respondents selecting each type of avoidance behavior, we identified the percent of respondents who reported taking one or more avoidance actions (87.3 %), two or more actions (48.9 %), three or more actions (22.5 %), or all four avoidance actions (7.8 %), and used this information to initialize the model for the second wave of 2009 H1N1 influenza in Arizona. While the simulation is running, the percent of the susceptible who engage in avoidance behavior changes dynamically at each step, influenced by the disease prevalence in the system.
The simulation output is measured using two indicators: (1) the number of people in infected status on each day (morbidity), and (2) the number of people who were ever infected each day since the beginning of the second wave of 2009 H1N1 (cumulative morbidity). The first step of the simulation represents October 4, 2009, and one day is used as one time step in the simulation. Experiments run 364 time steps to cover the whole 2009–2010 normal influenza season while our main interest is the beginning of the season.Footnote 4
4 Results
The simulation results are first evaluated against empirical data from October and November 2009 (the first six weeks of the normal influenza season: October 4, 2009 to November 14, 2009). Arizona requested its first batch of 2009 H1N1 vaccines from the CDC on September 30, 2009 (ADHS 2009c) and received it on October 6, 2009 (Holland 2009). More vaccines were continuously received each week following the initial shipment, and by the end of October 2009 the vaccine was widely available in the state for high-risk priority groups (ADHS 2009d, 2009e). Considering previous findings that 2009 H1N1 vaccination confers immunity two weeks after administration (Lee et al. 2010b), the simulated and empirical data are most comparable from the beginning of the normal influenza season to November 14, 2009, as the introduction of vaccination can greatly change the spread dynamics (CDC 2010c). As shown in Fig. 3, the simulation results from the eight compartment models are relatively close to the estimated actual number of cases in Arizona with a 10 % case detection rate, while the standard SEIR model produced a much higher number of cases and the model assuming that 100 % of the susceptible were engaged in avoidance actions produced a lower number of cases.
Simulated and empirical cumulative morbidity by week. Note: The percent as showed in the legends shows the percent of the susceptible taking avoidance behavior when the simulation is initialized for the 2009–2010 normal influenza season, starting from October 2009 (also the second wave of 2009 H1N1). After simulation begins, this percent changes over time, depending upon the disease prevalence and feedback to disease prevalence and rest compartment
Simulated morbidity during the 2009–2010 normal influenza season. Note: The percent as showed in the legends shows the percent of the susceptible taking avoidance behavior when the simulation is initialized for the 2009–2010 normal influenza season, starting from October 2009 (also the second wave of 2009 H1N1). After simulation begins, this percent changes over time, depending upon the disease prevalence and feedback to disease prevalence and rest compartment
Table 2 summarizes the simulation results regarding morbidity and cumulative morbidity in the standard and modified SEIR models. Figures 4 and 5 show how morbidity and cumulative morbidity change over time in each model. In the standard SEIR model (where there is no public avoidance action), the morbidity peaks on December 9, 2009 (67th time step), and 416,860 people are in the infected status group on that day. Although the morbidity continues decreasing after that day, the disease continues to spread until June 20, 2010 (260th time step). By the end of the normal influenza season, the total number of people infected is 3,905,743, which is 61.3 % of the total Arizona population.
Simulated cumulative morbidity during the 2009–2010 normal influenza season. Note: The percent as showed in the legends shows the percent of the susceptible taking avoidance behavior when the simulation is initialized for the 2009–2010 normal influenza season, starting from October 2009 (also the second wave of 2009 H1N1). After simulation begins, this percent changes over time, depending upon the disease prevalence and feedback to disease prevalence and rest compartment
When considering individuals’ protective behavior in the eight compartment model, the impacts of the pandemic are mitigated and the spread of the disease slows. For example, when the simulation was initialized with 7.8 % of the susceptible taking protective behavior at the beginning of the second wave of 2009 H1N1, the peak morbidity is reduced to 330,511 people on December 18, 2009 (76th time step), with morbidity reaching zero on September 10, 2010 (342nd time step). The cumulative morbidity reaches approximately 3.7 million. With the assumption of 22.5 % of the population taking avoidance behavior when the model is initialized, the peak morbidity is reduced to 160,076 on January 17, 2010 (106th time step). The cumulative morbidity is a little less than 3 million.
An important characteristic of the pandemic spread found in this condition is that the disease continues spreading during the entire season, and the morbidity and cumulative morbidity continue to increase at the end of the normal influenza season. However, this buys more time for public health professionals to prepare for the arrival of the peak and to develop countermeasures. Once the model is initialized with greater than 22.5 % of the susceptible engaging in risk avoidance behaviors, we no longer see multiple waves. Morbidity quickly reaches its peak, and continues to the end of the season or no longer appears. Figure 4 shows the simulation of morbidity during the 2009–2010 normal influenza season based on different assumptions regarding the percent of the susceptible taking avoidance actions at the beginning of the normal flu season. Figure 5 presents the simulated cumulative morbidity for the same period.
We made a few assumptions regarding important model parameters with uncertain values, including the percent of the population with natural immunity in the community and the case detection rate. Both parameters are known to be crucial elements in determining the outcome of epidemic modeling (Jenvald et al. 2007). In the following section, a sensitivity analysis is performed on each of these parameters in order to better understand the impact of variability in key parameters on pandemic-related estimations of morbidity. For the following sensitivity analysis, the percent of the susceptible engaging in avoidance behavior at the beginning of the normal flu season is set to 22.5 %.
4.1 The percent of the naturally immune population
In the modified SEIR model, 7 % of the total Arizona population is assumed to have natural immunity against 2009 H1N1. The elderly population (who may have higher levels of natural immunity based on exposure to previous pandemics) accounts for 14 % of the total population in Arizona, so a sensitivity analysis is first conducted to explore whether, and how, changing the proportion of the natural immune population influences the influenza spread dynamics.
With all other variables fixed at the values shown in Table 1, three values for the percent of naturally immune people among the total population were experimented with: 0 %, 7 %, and 14 %. The experimental results are presented in Table 3. When no natural immunity against influenza exists in the community, the peak morbidity is 269,772, which occurs on January 2, 2010 (91st time step). As the proportion of people with natural immunity increases in the population, the epi curves flatten out (i.e., the peak morbidity decreases and the duration of the epidemic increases), as shown in Fig. 6. For example, increasing the percent of the naturally immune population from 0 to 7 % can reduce the peak morbidity by 37.3 percentage points, delaying the peak morbidity by 15 days. When the naturally immune proportion of the population reaches 14 %, the impacts of influenza on the community become limited. The morbidity increases slowly over time, and the peak morbidity is delayed to February 8, 2010 (128th time step).
4.2 The case detection rate
In our initial model run, we used an der Heiden et al.’s assumption (2009) that the detection rate of 2009 H1N1 influenza cases is 10 % (see Table 1), meaning that lab-confirmed cases reflect only 10 % of actual (clinical and subclinical) 2009 H1N1 cases in Arizona. Here we examine the sensitivity of the experimental results to changes in the case detection rate. The value for this parameter is changed to 30 % and 50 %, and the simulation results are summarized in Table 3 and Fig. 7.
When the case detection rate reaches 30 %, the peak morbidity occurs much later (March 18, 2010 or 166th time step) with a much lower number for morbidity at the peak as compared with the base assumption of 10 %. Increasing the case detection rate from 30 % to 50 % can still bring considerable reduction in morbidity or delay the occurrence of peak morbidity, although the extent of reduction or delay is not as large as that when the detection rate is increased from 10 % to 30 %.
5 Discussion
In this paper, we underline the importance of a realistic representation of social and human factors in determining epidemic dynamics, especially in regards to early stages of the epidemic where antiviral measures are not readily available. Social and behavioral responses to the disease as well as risk information need to be seriously considered in epidemic simulations if emergency managers want to properly anticipate the dynamics of emergencies and prepare for them. This requires careful consideration of the assumptions made regarding social and human behaviors in traditional epidemiologic simulation models. Classical compartment models without social and human responses may overestimate the impact of a pandemic, whereas existing modified models incorporating the assumption that all people take avoidance actions may underestimate the impact. The model presented here aimed to address such a limitation in influenza pandemic simulations through the modification of compartment models.
This approach may be particularly relevant and useful in simulating the dynamics of a pandemic influenza when antiviral measures such as a vaccine are not available. Vaccination can greatly change the spread process of an epidemic. Researchers and practitioners often consider vaccination to be the best measure for preventing and controlling an influenza outbreak (Longini et al. 2004). However, with the outbreak of a novel pandemic strain of influenza, the time and production capacities are usually insufficient to produce and distribute enough effective vaccines to protect the general public (Mniszewski et al. 2008; Monto 2006). Other measures, such as non-pharmaceutical measures through public risk communication, delay the disease spread process until vaccines become widely available. We paid attention to the period in which public risk communication might be an important intervention strategy and incorporating human behavioral response is thus particularly critical.
One potential extension of the current study is to link public risk communication characteristics with the public’s protective behavior. For example, during decades of research, useful knowledge has been accumulated regarding the relationship between risk information, risk perception, and responsive behavior. When emergency managers aim to encourage individuals’ protective behaviors by influencing their risk perceptions, they could consider the following key attributes of risk information: the information source and frequency, message content, message style, and transmission channel. For instance, individuals are more likely to personally perceive the existing danger when the information source is official and familiar as well as when the risk message is repeated in an expected way (Donner 2006; Mileti and Fitzpatrick 1992; Perry 1979). It is also important to encompass in the risk message the answers to key questions such as what the risk is and when it will likely occur, what geographical area is threatened, how people can protect themselves, who is the source of the warning, and whether the information includes graphical information in addition to verbal messages (Mileti 1995; Mileti and Darlington 1997; Pfister 2002). The message style is also critical. People are more likely to perceive the risk and take appropriate protective actions when the message is consistent, continuous, certain, urgent, sufficient, clear, and accurate (Donner et al. 2007; Mileti and Sorensen 1990; Perry et al. 1980). Finally, most individuals receive risk messages through various impersonal transmission channels, such as television, newspapers, or social media, which are convenient tools that can be easily utilized by public managers. Systematic research related to the influence of risk communication characteristics on individual responsive behaviors and the contribution of such behavioral changes to influenza spread dynamics can help public managers develop effective risk communication strategies during a pandemic influenza outbreak situation.
There are several limitations to the present study. Although we used the best available data (based on our knowledge) to parameterize the model and conducted a sensitivity analysis on key parameters, questions still remain for parameters whose values were derived from other types of secondary data. The values of some parameters in the model cannot be easily determined empirically (e.g., contact rates), or they exist only as certain range values (e.g., the case detection rate and proportion of the population with pre-existing immunity). We hope that the sensitivity analyses we performed provide perspectives on the variability of morbidity and mortality estimates from a pandemic given uncertainty in the model parameters.
Exposed and infected individuals can, in reality, be medically treated to shorten their latent and infectious periods, which is not taken into account in the present model. However, we believe that the influence of those medical treatments on the simulation results is minor because we used the average length of the latent and infectious periods found in the empirical data (which already includes the effect of medical treatments). The influence of vaccination and other types of public intervention can be further included and tested by extending the current simulation model.
The simulation model is also constrained by limitations inherent in the SEIR compartment model, such as the homogeneous population assumption. Standard compartment models assume a group of identical people in terms of contact patterns and the impact of an epidemic. We attempted to introduce some heterogeneity into the model by splitting the population into eight compartments based on behavioral response. However, such a change introduces only a limited degree of heterogeneity into people’s contact patterns, and the biological characteristics of the disease are the same for all individuals. Social networks and geographical topology in the epidemic process have not been considered and cannot be easily introduced in the compartment models.
Many additional approaches have been developed to model the spread of an epidemic: agent-based models, multi-scale models, and network models that rely on computational advance and more sophisticated data structures (Barrat et al. 2008). For instance, agent-based models have shown some promise in terms of including important types of heterogeneity in epidemic simulations (Bobashev et al. 2007; Mniszewski et al. 2008; Rahmandad and Sterman 2008). Agent-based models recreate the movements and interactions of individuals in space and time on a very detailed level. The model also shows how social contact networks and local interactions shape the spread of an epidemic in a community (Zhong 2012). Such a model would take a significant amount of time and resources to build, but can certainly provide useful insights on the epidemic process, addressing inevitable limitations of compartment models.
5.1 Conclusion
This paper focuses on an isolated public health emergency in the United States. In reality, many systems and processes (e.g., disease processes or emergency communication systems) are coupled with each other. Thus, it may be unrealistic to conceptualize emergencies and disasters with a focus on only one dimension of such a system. For example, disease propagation may be closely coupled with social and human behaviors influenced by an emergency controlling system, which follows up on the spread of the disease in society and communicates risk information. Therefore, ongoing feedback loops exist between different types of systems during emergencies and disasters.
Despite such limitations, the current study addresses critical challenges in forecasting epidemic spread dynamics in general and studying emerging respiratory infectious diseases in particular. The complexity of the context does not easily lend itself to a simple methodological approach or simple solutions. The flexibility of the approach presented can be used to conduct further experiments and test social interventions in specific contexts without suffering from the issues involved in real experiments or observational studies. This approach can provide a useful decision support tool to help inform decision-makers’ judgments during an emergency, such as a novel influenza outbreak.
Notes
An influenza pandemic is “a global outbreak of disease that occurs when a new influenza virus appears or “emerges” in the human population, causes serious illness, and then spreads easily from person to person worldwide” (CDC 2012). It is different from pandemic influenza, which refers to the influenza that causes a global outbreak of the disease.
Note that these are the laboratory confirmed cases. On August 30, 2009, the CDC stopped reporting laboratory-confirmed 2009 H1N1 influenza cases because such data tends to underestimate the true number of cases (CDC 2010b), whereas ADHS continued to report weekly laboratory-confirmed cases in Arizona. Given the difficulty in determining the true number of infected cases or the true case detection rate, a previous study (an der Heiden et al. 2009) used the number of laboratory-confirmed cases and an assumed case detection rate to estimate the actual number of cases. In this paper, the actual number of infected cases is calculated based on the number of laboratory-confirmed cases in Arizona reported by ADHS and a 10 % detection rate of 2009 H1N1 influenza cases as in the study by an der Heiden et al. (2009).
Previous researchers have found that self-protective action is a family-level decision, and the whole household usually acts as one respondent (Ekberg et al. 2009; Vaughan and Tinker 2009). Here we assumed that the proportion of households in Arizona taking avoidance actions might be equivalent to the proportion of (susceptible) people taking avoidance actions.
The modified model has one stochastic variable, the avoidance behavior effect. We run the model 20 and 100 times separately for each scenario shown in Figs. 3, 4 and 5. The results for 100 runs are very similar to those from 20 runs. In each scenario shown in Fig. 3, for example, the results from 20 and 100 runs are not much different, and the curve of cumulative morbidity (Fig. 4) produced from 100 runs is almost identical to that from 20 runs. In this paper we report the simulation results from 20 runs.
References
ACS (2009) American Community Survey. American Community Survey (ACS). http://factfinder.census.gov/servlet/DatasetMainPageServlet?_program=ACS&_submenuId=datasets_2&_lang=en&_ts=. Accessed 3 Feb 2011
ADHS (2009a) Arizona supplemental influenza summary: MMWR week 39. Arizona Department of Health Services (ADHS). http://www.azdhs.gov/phs/oids/epi/flu/pdf/az_flureport_supp_39_0809.pdf. Accessed 3 Feb 2011
ADHS (2009b) Arizona weekly influenza summary: MMWR week 40. Arizona Department of Health Services (ADHS). http://www.azdhs.gov/phs/oids/epi/flu/pdf/h1n1_report_october14.pdf. Accessed 3 Feb 2011
ADHS (2009c) Arizona orders 2009 H1N1 vaccine for state; Counties plan distribution of vaccine. Arizona Department of Health Services (ADHS). http://www.azdhs.gov/diro/pio/news/2009/VaccineRequest-093009.htm. Accessed 1 July 2012
ADHS (2009d) H1N1 vaccine information. Arizona Department of Health Services (ADHS). http://www.hr.az.gov/State_Employee/PDF/News_Vaccine.pdf. Accessed 1 July 2012
ADHS (2009e) Report to the governor on H1N1 influenza preparedness and response activities. Arizona Department of Health Services (ADHS). http://www.azdhs.gov/pandemicflu/pdf/governors%20report%20h1n1.pdf. Accessed 1 July 2012
an der Heiden M, Buchholz U, Krause G, Kirchner G, Claus H, Ha WH (2009) Breaking the waves: modelling the potential impact of public health measures to defer the epidemic peak of novel influenza A/H1N1. PLoS ONE. doi:10.1371/journal.pone.0008356
Araz OM, Lant T, Fowler JW, Jehn M (2011) A simulation model for policy decision analysis: a case of pandemic influenza on a university campus. J Simul 5:89–100
Balcan D, Colizza V, Singer AC, Chouaid C, Hu H, Gonçalves B, Bajardi P, Poletto C, Ramasco JJ, Perra N, Tizzoni M, Paolotti D, Broeck WVd, Valleron A, Vespignani A (2009) Modeling the critical care demand and antibiotics resources needed during the fall 2009 wave of influenza A (H1N1) pandemic. PLoS Curr. doi:10.1371/currents.RRN1133
Barrat A, Barthelemy M, Vespignani A (2008) Dynamical processes on complex networks. Cambridge University Press, Cambridge
Bobashev GV, Goedecke DM, Yu F, Epstein J (2007) A hybrid epidemic model: combining the advantages of agent-based and equation-based approaches. In: Henderson SG, Hsieh MH, Shortle J, Tew JD, Barton RR (eds) Proceedings of the 2007 winter simulation conference. Society for Computer Simulation International, Washington, pp 1532–1537
Bults M, Beaujean DJ, de Zwart O, Kok G, van Empelen P, van Steenbergen JE, Richardus JH, Voeten HA (2011) Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the influenza A (H1N1) pandemic in the Netherlands: results of three consecutive online surveys. BMC Public Health. doi:10.1186/1471-2458-11-2
CDC (2009a) H1N1 early outbreak and disease characteristics. Center for Disease Control and Prevention (CDC). http://www.cdc.gov/h1n1flu/surveillanceqa.htm. Accessed 3 Feb 2011
CDC (2009b) Updated interim recommendations for the use of antiviral medications in the treatment and prevention of influenza for the 2009–2010 season. Centers for Disease Control and Prevention (CDC). http://www.cdc.gov/h1n1flu/recommendations.htm. Accessed 3 Feb 2011
CDC (2010a) H1N1 flu. Center for Disease Control and Prevention (CDC). http://www.cdc.gov/h1n1flu/. Accessed 3 Feb 2011
CDC (2010b) Monitoring influenza activity, including 2009 H1N1. Centers for Disease Control and Prevention (CDC). http://www.cdc.gov/h1n1flu/reportingqa.htm. Accessed 1 July 2012
CDC (2010c) Key facts about 2009 H1N1 flu vaccine. Center for Disease Control and Prevention (CDC). http://www.cdc.gov/h1n1flu/vaccination/vaccine_keyfacts.htm. Accessed 3 Feb 2011
CDC (2012) Questions and answers on the executive order adding potentially pandemic influenza viruses to the list of quarantinable diseases. http://www.cdc.gov/quarantine/qa-executiveorder-pandemic-list-quarantinable-diseases.html. Retrieved 21 Nov 2012
Coburn BJ, Wagner BG, Blower S (2009) Modeling influenza epidemics and pandemics: insights into the future of swine flu (H1N1). BMC Med. doi:10.1186/1741-7015-7-30
Cowling BJ, Ng S, Ma ESK, Cheng CKY, Wai W, Fang VJ, Chan K-H, Ip DKM, Chiu SS, Peiris JSM, Leung GM (2009) Protective efficacy of seasonal influenza vaccination against seasonal and pandemic influenza virus infection during 2009 in Hong Kong. Clin Infect Dis 51(12):1370–1379
Das T, Savachkin A, Zhu Y (2008) A large scale simulation model of pandemic influenza outbreaks for development of dynamic mitigation strategies. IIE Trans 40(9):893–905
de Zwart O, Veldhuijzen IK, Richardus JH, Brug J (2010) Monitoring of risk perceptions and correlates of precautionary behaviour related to human avian influenza during 2006–2007 in the Netherlands: results of seven consecutive surveys. BMC Infect Dis. doi:10.1186/1471-2334-10-114
Destefano F, Haber M, Currivan D, Farris T, Burrus B, Stone-Wiggins B, McCalla A, Guled H, Shih H, Edelson P, Wetterhall S (2010) Factors associated with social contacts in four communities during the 2007–2008 influenza season. Epidemiol Infect. doi:10.1017/S095026881000230X
Donaldson LJ, Rutter PD, Ellis BM, Greaves FEC, Mytton OT, Pebody RG, Yardley IE (2009) Mortality from pandemic A/H1N1 2009 influenza in England: public health survelliance study. BMJ. doi:10.1136/bmj.b5213
Donner B (2006) Public warning response to hurricane Katrina: a preliminary analysis. Disaster Research Center, University of Delaware, Newark, DE
Donner WR, Rodriguez H, Diaz W (2007) Public warning response following tornadoes in New Orleans, LA, and Springfield, MO: a sociological analysis. Paper presented at the 87th annual meeting of the American meteorological society, San Antonio, Texas, 15–18 Jan 2007
Edmunds WJ, Kafatos G, Wallinga J, Mossong JR (2006) Mixing patterns and the spread of close-contact infectious diseases. Emerg Themes Epidemiol. doi:10.1186/1742-7622-3-10
Ekberg J, Eriksson H, Morin M, Holm E, Strömgren M, Timpka T (2009) Impact of precautionary behaviors during outbreaks of pandemic influenza: modeling of regional differences. AMIA Annu Symp Proc 2009:163–167
Epstein JM, Parker J, Cummings D, Hammond RA (2008) Coupled contagion dynamics of fear and disease: mathematical and computational explorations. PLoS ONE. doi:10.1371/journal.pone.0003955
Ferguson NM, Cummings DAT, Cauchemez S, Fraser C, Riley S, Meeyai A, Iamsirithaworn S, Burke DS (2005) Strategies for containing an emerging influenza pandemic in southeast Asia. Nature 437(8):209–214
Halder N, Kelso JK, Milne GJ (2010) Analysis of the effectiveness of interventions used during the 2009 A/H1N1 influenza pandemic. BMC Public Health. doi:10.1186/1471-2458-10-168
Holland C (2009) H1N1 vaccine to arrive in Arizona today. http://www.azfamily.com/news/health/H1N1-vaccine-to-arrive-in-Arizona-today-63593292.html. Accessed 1 July 2012
Jefferson T, Foxlee R, Mar CD, Dooley L, Ferroni E, Hewak B, Prabhala A, Nair S, Rivetti A (2008) Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. doi:10.1136/bmj.39393.510347.BE
Jehn M, Kim Y, Bradley B, Lant T (2011) Community knowledge, risk perception and preparedness for the 2009 influenza A (H1N1) pandemic. J Public Health Manag Pract 17(5):431–438
Jenvald J, Morin M, Timpka T, Eriksson H (2007) Simulation as decision support in pandemic influenza preparedness and response. In: Van de Walle B, Burghardt P, Nieuwenhuis C (eds) Proceedings of the 4th international conference on information systems for crisis response and management. Vub Brussels University Press, Brussels, pp 295–304
Jones JH, Salathe M (2009) Early assessment of anxiety and behavioral response to novel swine-origin influenza A (H1N1). PLoS ONE. doi:10.1371/journal.pone.0008032
Keeling MJ, Rohani P (2008) Modeling infectious disease in humans and animals. Princeton University Press, Princeton
Kermack WO, McKendrick AG (1927) A contribution to the mathematical theory of epidemics. Proc R Soc Lond A 115(772):700–721
Kermack WO, McKendrick AG (1932) A contribution to the mathematical theory of epidemics: the problem of endemicity. Proc R Soc Lond A 138(834):55–83
Kermack WO, McKendrick AG (1933) A contribution to the mathematical theory epidemics: further studies of the problem of endemicity. Proc R Soc Lond A 141(843):94–122
Larson RC, Nigmatulina KR (2009) Engineering responses to pandemics. Inf Knowl Syst Manag 8(1–4):311–339
Lau JT, Yang X, Tsui H, Kim JH (2003) Monitoring community psychological responses to the SARS epidemic in Hong Kong: from day 10 to day 62. J Epidemiol Community Health 57(11):864–870
Lau JT, Kim JH, Tsui H, Griffiths S (2007) Anticipated and current preventative behaviours in response to an anticipated human-to-human H5N1 epidemic in Hong Kong Chinese general population. BMC Infect Dis. doi:10.1186/1471-2334-7-18
Lau JT, Griffiths S, Choi KC, Tsui HY (2010) Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect Dis. doi:10.1186/1471-2334-10-139
Lee BY, Brown ST, Korch GW, Cooley PC, Zimmerman RK, Wheaton WD, Zimmer SM, Grefenstette JJ, Bailey RR, Assi TM, Burke DS (2010a) A computer simulation of vaccine prioritization, allocation, and rationing during the 2009 H1N1 influenza pandemic. Vaccine 28(31):4875–4879
Lee BY, Tai JHY, Bailey RR, Smith KJ, Nowalk AJ (2010b) Economics of influenza vaccine administration timing for children. Am J Manag Care 16(3):e75–e85
Leung GM, Lam T-H, Ho L-M, Ho S-Y, Chan BHY, Wong IOL, Hedley AJ (2003) The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health 57(11):857–863
Li MY, Graef JR, Wang L, Karsai J (1999) Global dynamics of a SEIR model with varying total population size. Math Biosci 160(2):191–213
Longini IM, Halloran ME, Nizam A, Yang Y (2004) Containing pandemic influenza with antiviral agents. Am J Epidemiol 159(7):623–633
Mileti DS (1995) Factors related to flood warning response. Paper presented at the US–Italy Research Workshop on the Hydrometeorology, Impacts, and Management of Extreme Floods, Perugia, Italy, 13–17 Nov 1995
Mileti D, Sorensen JH (1990) Communication of emergency public warnings. Oak Ridge National Laboratory, Oak Ridge, TN
Mileti DS, Fitzpatrick C (1992) The causal sequence of risk communication in the parkfield earthquake prediction experiment. Risk Anal 12(3):393–400
Mileti DS, Darlington JD (1997) The role of searching behavior in response to earthquake risk information. Soc Probl 44(1):89–103
Mniszewski SM, Valle SYD, Stroud PD, Riese JM, Sydoriak SJ (2008) Pandemic simulation of antivirals+school closures: buying time until strain-specific vaccine is available. Comput Math Organ Theory 14(3):209–221
Monto AS (2006) Vaccines and antiviral drugs in pandemic preparedness. Emerg Infect Dis 12(1):55–60
Mossong J, Hens N, Jit M, Beutels P, Auranen K, Mikolajczyk R, Massari M, Salmaso S, Tomba GS, Wallinga J, Heijne J, Todys MS, Rosinska M, Edmunds WJ (2008) Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. doi:10.1371/journal.pmed.0050074
Patel R, Longini IM, Halloran ME (2005) Finding optimal vaccination strategies for pandemic influenza using genetic algorithms. J Theor Biol 234(2):201–212
Perry RW (1979) Incentives for evacuation in natural disaster: research based community emergency planning. J Am Plan Assoc 45(4):440–447
Perry RW, Lindell MK, Greence MR (1980) Enhancing evacuation warning compliance: suggestions for emergency planning. Disasters 4(4):443–449
Pfister N (2002) Community response to flood warnings: the case of an evacuation from Grafton, March 2001. Aust J Emerg Manag 17(2):19–29
Philipson TJ (2000) Economic epidemiology and infectious disease. In: Cuyler AJ, Newhouse JP (eds) Handbook of health economics, vol 1. North-Holland, Amsterdam, pp 1761–1799
Philipson TJ, Posner RA (1993) Private choices and public health: the AIDS epidemic in an economic perspective. Harvard University Press, Cambridge
Quarantelli EL (1983) People’s reactions to emergency warnings. Disaster Research Center, University of Delaware, Newark, DE
Rahmandad H, Sterman J (2008) Heterogeneity and network structure in the dynamics of diffusion: comparing agent-based and differential equation models. Manag Sci 54(5):998–1014
Ross T, Zimmer S, Burke D, Crevar C, Carter D, Stark J, Giles B, Zimmerman R, Ostroff S, Lee B (2010) Seroprevalence following the second wave of pandemic 2009 H1N1 influenza. PLoS Curr. doi:10.1371/currents.RRN1148
Rost G, Wu J (2008) SEIR epidemiological model with varying infectivity and infinite delay. Math Biosci Eng 5(2):389–402
Shanks J (2009) Arizona swine flu: Maricopa County gets first case. National Ledger. http://www.nationalledger.com/cgi-bin/artman/exec/view.cgi?archive=36&num=25842. Accessed 3 Feb 2011
Tuite AR, Greer AL, Whelan M, Winter A-L, Lee B, Yan P, Wu J, Moghadas S, Buckeridge D, Pourbohloul B, Fisman DN (2010) Estimated epidemiologic parameters and morbidity associated with pandemic H1N1 influenza. CMAJ 182(2):131–136
Ulene V (2007) Bracing for a flu pandemic. Los Angeles Times. http://www.latimes.com/features/health/la-he-themd4jun04,1,3259716.column. Accessed 4 June 2007
Vaughan E, Tinker T (2009) Effective health risk communication about pandemic influenza for vulnerable populations. Am J Publ Health 99(s2):S324–S332
Yang Y, Sugimoto JD, Halloran ME, Basta NE, Chao DL, Matrajt L, Potter G, Kenah E, Longini IM (2009) The transmissibility and control of pandemic influenza A (H1N1) virus. Science 326(5953):729–733
Yoo B-K, Kasajima M, Bhattacharya J (2010) Public avoidance and the epidemiology of novel H1N1 influenza A. National Bureau of Economic Research, Cambridge
Zhong W (2012) Communicative competence: computational simulation approach to public emergency management. Dissertation, Arizona State University
Acknowledgements
This study was funded by the Arizona Department of Health Services (ADHS) through a Health and Human Services (HHS) preparedness grant, Arizona State University College of Public Program’s research seed grant, and the National Research Foundation of Korea Grant (NRF-2010-330-B00262). The authors thank Diane Reed and Andrew Lawless at ADHS, and Ken Anderson at Maricopa County Research & Reporting. We also thank Deborah Schumacher, Tanida Rojchanakasetchai, Barrie Bradley and Tim Lant, who helped conduct this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhong, W., Kim, Y. & Jehn, M. Modeling dynamics of an influenza pandemic with heterogeneous coping behaviors: case study of a 2009 H1N1 outbreak in Arizona. Comput Math Organ Theory 19, 622–645 (2013). https://doi.org/10.1007/s10588-012-9146-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10588-012-9146-6