Abstract
Metastasis to the regional lymph node is the most important prognostic indicator for the outcomes of patients with sold cancer. In general, it is well recognized that cancer development is genetically determined with progression from the microenvironment of the primary tumor site, oftentimes via the SLN gateway, to the distant sites. In about 20 % of the time, the cancer cells may spread directly through the blood vascular system to the distant sites. Thus, in general, cancer progression is consistent with Hellman’s spectrum theory in that development of nodal and systemic metastasis from a localized cancer growth is a progressive process. Cancer proliferation within the tumor microenvironment may give rise to increased tumor heterogeneity, which is further complicated by its continuous change through its evolution within the host in a Darwinian sense. It is crucial to understand the molecular process of lymphangiogenesis and hemangiogenesis in the tumor microenvironment with respect to the initial steps of cancer cells entering into the lymphatic and vascular systems so that rational therapy can be developed to curb the process of specific routes of metastasis. This chapter elucidates the role of lymphatics, nodal metastasis and antitumor immunity. We present novel immune targets in nodal metastases, the importance of the lymph node as a pre-metastatic niche, and immune-related proteins as biomarkers of metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Squamous cell carcinoma of the head and neck (SCCHN) frequently metastasizes to the regional lymph nodes and this is the strongest predictor of disease prognosis and outcome [1, 2]. Whereas accurate staging of lymph nodes in the neck is essential for optimal patient management, current preoperative clinical methods, including newer radiographic techniques, are suboptimal and misdiagnose the presence or absence of cervical nodal metastasis in many patients [3–5]. Therefore, due to the low sensitivity of detecting nodal metastasis and the poor prognosis when these metastases are missed, the current management of the clinically node negative (cN0) neck commonly includes routine elective neck dissection (END) with pathologic examination of the removed lymph nodes.
END, or cervical lymphadenectomy done at the time of primary surgery for SCCHN for a cN0 neck, is associated with a significantly improved regional recurrence-free survival and lower incidence of distant metastases. Furthermore, when END is not done, patients often present later with bulky neck metastases and unresectable disease [2]. END not only provides more accurate staging, it also provides objective criteria to decide when to give adjuvant therapies, such as number/levels of cervical lymph nodes involved and the presence of extracapsular spread (ECS) of tumor. However, upon END and pathologic analysis of neck dissections, only 25–30 % of clinically negative necks are found to harbor pathologic evidence of disease, and 15 % of clinically positive necks are in fact tumor negative. Consequently, lymphadenectomy may represent overtreatment of almost 50 % of patients. Even with END, 7–15 % of patients with no pathologic evidence of cervical lymph node metastases (pN0) will nonetheless suffer disease recurrence in the neck, indicating the limitation of routine pathology for identifying micrometastasis [4, 6–13].
Because of the need to accurately stage the neck and to treat only those most likely to benefit from therapy, much interest has arisen recently to validate the technique of sentinel lymph node (SLN) mapping for SCCHN. This technique has the potential to define those cN0 patients in whom neck dissection is most appropriate (i.e., those who are pathologically node positive), thereby obviating END and its associated morbidities in node-negative patients [5, 14]. Numerous single-institution studies have suggested that SLN mapping in SCCHN accurately predicts the status of the neck [13], and this finding is currently being evaluated in a large multicenter validation trial sponsored by the American College of Surgeons Oncology Group (ACOSOG Z0360 trial). When combined with intraoperative analysis of the SLN(s), this approach could allow for definitive staging and surgical treatment in a single procedure. For this goal to be fully realized, however, intraoperative SLN analysis must be both rapid and accurate.
Unfortunately, although final pathology on fixed tissues (with immunostaining if necessary in the case of SLNs) is highly accurate, intraoperative frozen section examination is notoriously insensitive. In breast cancer, reports on intraoperative SLN sensitivity range from 47 to 74 % [3] whereas in melanoma the sensitivity is even worse, with reports from 38 to 47 %. Consequently, many patients have to undergo a second surgical procedure to complete lymph node dissection after definitive pathologic assessment identifies microscopic metastatic disease not evident on intraoperative analysis. Our own work, and that reported by others, suggests that low sensitivity may also be an issue for intraoperative SLN analysis in SCCHN [15, 16]. Performing a second surgery on the neck is an undesirable scenario because this would likely increase complications and morbidity and could delay the use of adjuvant therapy. This is in addition to the extra cost, discomfort, and psychological toll on the patient. Such issues may negatively affect the widespread acceptance of SLN biopsy in SCCHN.
The optimal surgical management of the clinically negative (cN0) neck in patients with head and neck squamous cell carcinoma (SCC) is still controversial. Current treatment options include wait-and-see policy with subsequent therapeutic neck dissection in case of clinical appearance of metastasis, elective neck dissection and more recently sentinel lymph node biopsy. Each approach is based on consideration of oncologic efficacy versus neck morbidity. In this manuscript we present our approach to surgically stage the cN0 neck, based on the application of sentinel node identification and intraoperative assessment with molecular technique of RT-PCR.
Radiographic staging of the clinically negative neck
Although modern imaging techniques become more accurate for the assessment of lymph node metastases in the neck as criteria and technology evolve, micrometastases remain occult with any technique. Of clinically negative necks with occult metastases, 25 % contain only micrometastases. Current preoperative staging modalities for N0 neck are therefore unable to exceed a sensitivity of 75 % without sacrificing specificity. Thus incidence of occult metastases remains a significant clinical problem, for which no radiographic modality has sufficient achieved a negative predictive value (NPV) to permit safe observation of the tumor negative neck.
Observation of the clinically negative neck
The wait-and-see policy is based on strict follow up and detection of cervical metastasis at an early stage, when are curable. Arguments against observation of the clinically negative neck for early oral cavity carcinoma include decreased locoregional control (due to later presentation of metastatic disease), poor rates or surgical salvage (patients lost to follow up), delayed recognition of advanced stage patients (reducing early application of adjuvant therapy), and more radial/debilitating surgical procedures necessary to eradicate larger or more extensive disease when clinically apparent. Molecular analysis of the primary tumor is also not yet sufficiently accurate to permit prediction of metastasis in the patients who harbor it.
Elective neck dissection as a staging procedure
ECS is an important prognostic indicator of regional and distant failure and survival [17–22]. The incidence of ECS correlates with nodal size, and occurs with 12 % of nodes <5 mm in diameter, 18 % of nodes 5–10 mm, 23 % of nodes <10 mm, 44 % of nodes 10–20 mm, 53 % of nodes 20–30 mm, and 74 % of nodes >30 mm [23, 24]. Small metastatic nodes without ECS, if left untreated, will increase in size and may subsequently manifest ECS. Elective neck dissection may prevent this progression to ECS.
Moreover, elective neck dissection should reduce the risk of distant metastasis by minimizing tumor burden, restricting the duration of metastasis, and reducing number of nodes, and has been shown to reduce the likelihood of involvement of the lower levels of the neck. Salvage surgical treatment in patients managed by wait-and-see policy that failed in the neck during follow up range only from 25 to 71 %. Because of high incidence of occult metastases, the absence of reliable methods of detecting occult metastases, effectiveness of salvage surgery elective neck dissection is considered as standard of care in many institutions.
Selective neck dissection in patients with SCC of the head and neck with clinically negative neck provides crucial staging information, reduces regional recurrences rates, and improves regional disease free survival [2, 25].
Although the survival benefit of elective neck dissection (END), as a opposed to watchful waiting for head and neck SSC has not been proven in a prospective randomized studies [26], reported a survival benefit for END in a non-randomized study of carcinoma of the oral tongue. They reviewed 156 patients with squamous cell carcinoma of the oral tongue staged T1/T2N0. The survival and local/regional control for group of 102 patients with intraoral glossectomy only was 33 and 50 %, respectively. The survival and local/regional control for group of 54 patients with intraoral glossectomy plus neck dissection was 55 and 91 %, respectively.
In another study [27], retrospectively compared the results of END (33 patients) versus observation (30 patients) in surgical treatment of T1/T2 oral tongue. The regional recurrence rate was 47 % in the observation group and 9 % in the END group. Elective neck dissection also increased 5-year disease-free actuarial survival rate to 86 % compared with 55 % for watchful waiting.
In 2004 [2] in their study analyzed, whether elective neck dissection improves regional control and survival in patients with SCC of the oral cavity and oropharynx presenting with T1/T2 node-negative disease. Of the 359 patients included for analyses, 179 patients had excision of the primary tumor and neck observation and 180 patients underwent elective neck dissection with primary tumor excision and observation of the neck. Elective neck dissection improved the regional control rate, disease-free survival, and regional recurrence-free survival. The rate of regional failure in observation group was 27 %, compared with 9 % in the END group.
It is recommended, that when the probability of occult cervical metastasis is greater than 20 %, treatment of the neck is warranted [28]. The incidence of occult metastases in patients with head and neck squamous cell carcinoma is ~30 %. However, 70–80 % of these patients have no benefit from the elective neck dissection, and undergo unnecessary morbidity. Recently, selective neck dissection is indicated for elective surgical treatment of the neck, and its morbidity is less than modified radical neck dissection.
Shortcomings of elective neck dissection
Despite preservation of non-lymphatic structures, morbidity of elective SND still exist, including neck pain, shoulder dysfunction, lower lip paresis.
Although routine histopathological examination of elective neck dissection specimen is considered as the gold standard in occult metastases diagnosis, even this gold standard (hematoxylin–eosin staining) underestimate incidence of occult metastases. Regional recurrence rate for pathologically node negative (pN0) patients vary from 3 to 5 %. Consequently, END is not a 100 % reliable staging tool in the N0 neck with conventional pathologic evaluation (although regional control is effective). Many authors demonstrated upstaging of patients with pN0 neck after routine hematoxylin–eosin evaluation based on serial or semiserial sectioning, immunohistochemistry, and molecular analysis. Depending on method, which is used for detection, the incidence of occult subpathologic metastases vary from 5 to 40 %. These additional pathologic techniques for evaluation every lymph node within a neck dissection specimen are very time consuming and expensive [29].
SLNB—progress, staging, second surgery
Sentinel lymph node biopsy (SLNB) may obviate this problem with overtreatment, morbidity, and accurate regional staging. This technique has been proposed as minimally invasive, low morbidity modality able to select patients with occult metastases who will be benefit from neck dissection, and to minimize the morbidity and cost of neck treatment in patients with clinically negative neck. SLNB allows use additional pathologic techniques to accurate stage the neck with minimal node sampling.
The sentinel node concept states that tumor will spread from the primary site to a single node or group nodes, termed sentinel nodes then allows accurate prediction of the disease of the rest of the basin. Sentinel lymph node (SLN) is defined as the first lymph node to receive lymphatic drainage from a primary tumor. There might be more than one SLN for a specific tumor. If lymphatic spread occurs, the sentinel lymph node is the first node involved. Other nodes should be involved only subsequently.
Results from the First international conference on SLNB in mucosal head and neck cancer reported Ross et al. in 2002 [29]. Three hundred sixteen clinically N0 necks from 22 centers were included. Sentinel nodes were identified in 301 necks (95 %). The overall sensitivity of the procedure was 90 %. Centers who had performed less than 10 cases had a lower sensitivity (57 %), in comparison with centers that had performed more than 10 cases (94 % sensitivity). The cumulative results of 22 centers that contributed to first international conference confirm that there is a role for SNB in staging the clinically N0 neck and that technique has a similar sensitivity to that of a staging neck dissection.
The first multicenter prospective trial to determine whether SNB may be used to stage the clinically N0 neck in early T1/T2 SCC of the oral cavity and oropharynx were conducted in six European centers. Two hundred twenty-seven patients underwent SNB alone or in combination with END at six centers. One hundred thirty-four patients were considered suitable for the study. Seventy-nine patients had SNB alone, and 55 patients had SNB-assisted END. SNB was successful in identifying a sentinel nodes in 125/134 patients (93 %). The identification rate for floor of mouth (FOM) tumors was 37/43 (86 %), compared with 88/91 (97 %) for other tumors groups. Upstaging of disease occurred in 42/125 cases (34 %), with hematoxylin–eosin in 32/125 (26 %) and with additional pathological staging in 10/93 (11 %). The overall sensitivity of the technique with a mean follow up of 24 months was 42/45 (93 %). The sensitivity for FOM tumors was 12/15 (80 %), compared with 30/30 (100 %) for other tumor groups. SNB alone has similar identifications rate and sensitivities in comparison with SNB-assisted END.
Currently, there are three accepted indications for SLNB in early oral/oropharyngeal SCC. 1. staging of the ipsilateral neck in unilateral cT1/T2 cN0 tumors, 2. staging of the ipsilateral and contralateral neck in midline tumors or tumors crossing the midline (cT1/T2 cN0), 3. staging of the contralateral neck in midline tumors or tumors crossing the midline (cT1/T2 cN + ipsilateral).
Paleri et al. [30] performed a systemic review and a diagnostic meta-analysis of all published literature regarding sentinel node biopsies in head and neck cancer until December 2003. A total of 301 patients with oral cavity and 46 patients with oropharyngeal carcinomas were included for the meta-analysis. The identification rate for SLN was 97.7 %. Overall sensitivity results using the random effects model was 0.926 (95 % confidence interval, 0.852–0.964).
The American College of Surgeons Oncology Group (ACOSOG) conducted a prospective multi-institutional trial involved 25 institutions over a 3 year period. They validated sentinel node biopsy (SLNB) pathologically when compared to completion selective neck dissection for patients with T1 or T2, clinically N0 SSC of the oral cavity. Twenty five institutions registered 161 patients. One hundred and forty patients were eligible and evaluated, including 95 cancers of the tongue, 26 of the floor of mouth, and 19 other oral cancers. In the 106 SLNB which were found to be pathologically and clinically node negative by routine hematoxylin–eosin staining, 100 patients were found to have no other pathologically positive nodes, corresponding to a NPV of 94 %. With additional sectioning and immunohistochemistry, NPV was improved to 96 %. For T1 lesions, metastases were correctly identified in 100 %. The NPV in surgeons who had experience in oral cancer was 100 % vs 95 % for inexperienced.
Results of clinical application of SNB study reported Stoeckli et al. in 2007 [31]. Their series of 51 patients with early stage T1/T2 N0 SCC of the oral cavity and oropharynx were evaluated in an observational trial. END was performed only in case of positive SNB. The sentinel node detection rate was 98 %. Two patients (6 %) with negative SNB experienced a neck recurrence during the mean time follow up of 19 months. The NPV for a negative SNB was therefore 94 %.
Once the procedure had been modified to a strictly intraoperative detection method, Werner et al. [32] recommend identifying one to three sentinel nodes (SN1–SN3). Histological results of SN1–SN3 reflected the correct stage of metastatic disease in 97 %. The evaluation of the three hottest SLNs to predict a lymph node status of the patients is supported by subsequent studies.
SLNB for early oral and oropharyngeal SCC has been demonstrated to be technically feasible and accurate with high rate of sentinel lymph node detection. The NPV of negative SLN proves high reliability of this technique. SNB considerably reduces the number of lymph nodes that must be investigated compared with END specimen. Thus, more detailed histopathologic evaluation, including step serial sectioning and immunohistochemistry, can be employed. Consequently, this technique allows more accurate pathological staging of the clinically N0 neck in comparison to the routine examination of many nodes from a neck dissection specimen and can select patients that benefit from END [31, 33, 34].
A major disadvantage of the SNB is undergoing second surgical procedure to complete lymph node dissection after definitive pathologic evaluation if the SLN is positive. Performing a second surgery on the neck would likely increase complications and morbidity and could delay to use of adjuvant therapy. One-stage procedure concept can reduce cost, discomfort and anxious apprehension for the patients. A rapid, accurate intraoperative test for the presence of metastatic disease in SLN may support widespread acceptance SLNB in SCC of the head and neck [15].
In conclusion, a large multi-institutional pathologic validation trial has supported previous single institution studies, establishing that the sentinel node concept applies to SCCHN, as well as to cutaneous melanoma and breast cancer. The recently published American College of Surgeons Oncology Group (ACOSOG) prospective multi-center trial of 168 patients demonstrated that the pathologic status of the SLN correlated highly with the results of subsequent, immediate formal lymphadenectomy, yielding a NPV of 96 % for accurately staging a pN0 neck using SNB [13]. Whereas the ACOSOG Z0360 trial is powered to validate the multiple single-institution studies that suggest the utility of SLN mapping for staging the cN0 neck in SCCHN, it is unlikely that SLN biopsy will be widely accepted without a rapid, accurate, and standardized method of staging the SLN(s). Our development of such an assay and identification of discriminatory marker genes provides the pilot data necessary for the incorporation of QRT-PCR into future clinical studies applying SLN mapping to clinical practice for patients with this disease.
References
Argiris A, Karamouzis MV, Raben D, Ferris RL (2008) Head and neck cancer. Lancet 371:1695–1709
Duvvuri U, Simental AA Jr, D’Angelo G, Johnson JT, Ferris RL, Gooding W, Myers EN (2004) Elective neck dissection and survival in patients with squamous cell carcinoma of the oral cavity and oropharynx. Laryngoscope 114:2228–2234
Morton DL, Wen DR, Wong JH, Economou JS, Cagle LA, Storm FK, Foshag LJ, Cochran AJ (1992) Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 127:392–399
Alex JC, Sasaki CT, Krag DN, Wenig B, Pyle PB (2000) Sentinel lymph node radiolocalization in head and neck squamous cell carcinoma. Laryngoscope 110:198–203
Chepeha DB, Taylor RJ, Chepeha JC, Teknos TN, Bradford CR, Sharma PK, Terrell JE, Wolf GT (2002) Functional assessment using constant’s shoulder scale after modified radical and selective neck dissection. Head Neck 24:432–436
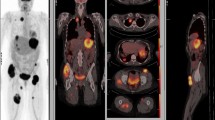
Civantos FJ, Gomez C, Duque C, Pedroso F, Goodwin WJ, Weed DT, Arnold D, Moffat F (2003) Sentinel node biopsy in oral cavity cancer: correlation with PET scan and immunohistochemistry. Head Neck 25:1–9
Civantos FJ, Stoeckli SJ, Takes RP, Woolgar JA, de Bree R, Paleri V, Devaney KO, Rinaldo A, Silver CE, Mondin V, Werner JA, Ferlito A (2010) What is the role of sentinel lymph node biopsy in the management of oral cancer in 2010? Eur Arch Otorhinolaryngol 267:839–844
Koch WM, Choti MA, Civelek AC, Eisele DW, Saunders JR (1998) Gamma probe-directed biopsy of the sentinel node in oral squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 124:455–459
Shoaib T, Soutar DS, MacDonald DG, Camilleri IG, Dunaway DJ, Gray HW, McCurrach GM, Bessent RG, MacLeod TI, Robertson AG (2001) The accuracy of head and neck carcinoma sentinel lymph node biopsy in the clinically N0 neck. Cancer 91:2077–2083
El-Sayed IH, Singer MI, Civantos F. Sentinel lymph node biopsy in head and neck cancer. Otolaryngol Clin North Am 2005;38:145–60, ix–x
Pitman KT, Ferlito A, Devaney KO, Shaha AR, Rinaldo A (2003) Sentinel lymph node biopsy in head and neck cancer. Oral Oncol 39:343–349
Taylor RJ, Wahl RL, Sharma PK, Bradford CR, Terrell JE, Teknos TN, Heard EM, Wolf GT, Chepeha DB (2001) Sentinel node localization in oral cavity and oropharynx squamous cell cancer. Arch Otolaryngol Head Neck Surg 127:970–974
Civantos FJ, Zitsch RP, Schuller DE, Agrawal A, Smith RB, Nason R, Petruzelli G, Gourin CG, Wong RJ, Ferris RL, El Naggar A, Ridge JA et al (2010) Sentinel lymph node biopsy accurately stages the regional lymph nodes for T1–T2 oral squamous cell carcinomas: results of a prospective multi-institutional trial. J Clin Oncol 28:1395–1400
Schiefke F, Akdemir M, Weber A, Akdemir D, Singer S, Frerich B (2009) Function, postoperative morbidity, and quality of life after cervical sentinel node biopsy and after selective neck dissection. Head Neck 31:503–512
Ferris RL, Xi L, Raja S, Hunt JL, Wang J, Gooding WE, Kelly L, Ching J, Luketich JD, Godfrey TE (2005) Molecular staging of cervical lymph nodes in squamous cell carcinoma of the head and neck. Cancer Res 65:2147–2156
Ferris RL, Xi L, Seethala RR, Chan J, Desai S, Hoch B, Gooding W, Godfrey TE (2011) Intraoperative qRT-PCR for detection of lymph node metastasis in head and neck cancer. Clin Cancer Res 17:1858–1866
Alvi A, Johnson JT (1996) Extracapsular spread in the clinically negative neck (N0): implications and outcome. Otolaryngol Head Neck Surg 114:65–70
Greenberg JS, Fowler R, Gomez J, Mo V, Roberts D, El Naggar AK, Myers JN (2003) Extent of extracapsular spread: a critical prognosticator in oral tongue cancer. Cancer 97:1464–1470
Myers JN, Greenberg JS, Mo V, Roberts D (2001) Extracapsular spread. A significant predictor of treatment failure in patients with squamous cell carcinoma of the tongue. Cancer 92:3030–3036
Alvi A, Johnson JT (1997) Development of distant metastasis after treatment of advanced-stage head and neck cancer. Head Neck 19:500–505
Genden EM, Ferlito A, Bradley PJ, Rinaldo A, Scully C (2003) Neck disease and distant metastases. Oral Oncol 39:207–212
Ferlito A, Rinaldo A, Devaney KO, MacLennan K, Myers JN, Petruzzelli GJ, Shaha AR, Genden EM, Johnson JT, de Carvalho MB, Myers EN (2002) Prognostic significance of microscopic and macroscopic extracapsular spread from metastatic tumor in the cervical lymph nodes. Oral Oncol 38:747–751
Som PM (1987) Lymph nodes of the neck. Radiology 165:593–600
Don DM, Anzai Y, Lufkin RB, Fu YS, Calcaterra TC (1995) Evaluation of cervical lymph node metastases in squamous cell carcinoma of the head and neck. Laryngoscope 105:669–674
Myers JN (1999) Value of neck dissection in the treatment of patients with intermediate-thickness cutaneous malignant melanoma of the head and neck. Arch Otolaryngol Head Neck Surg 125:110–115
Lydiatt DD, Karrer FW, Lydiatt WM, Johnson PJ (1994) The evaluation, indications, and contraindications of selective neck dissections. Nebr Med J 79:140–144
Yuen AP, Wei WI, Wong YM, Tang KC (1997) Elective neck dissection versus observation in the treatment of early oral tongue carcinoma. Head Neck 19:583–588
Weiss MH, Harrison LB, Isaacs RS (1994) Use of decision analysis in planning a management strategy for the stage N0 neck. Arch Otolaryngol Head Neck Surg 120:699–702
Ross G, Shoaib T, Soutar DS, Camilleri IG, Gray HW, Bessent RG, Robertson AG, MacDonald DG (2002) The use of sentinel node biopsy to upstage the clinically N0 neck in head and neck cancer. Arch Otolaryngol Head Neck Surg 128:1287–1291
Paleri V, Rees G, Arullendran P, Shoaib T, Krishman S (2005) Sentinel node biopsy in squamous cell cancer of the oral cavity and oral pharynx: a diagnostic meta-analysis. Head Neck 27:739–747
Stoeckli SJ (2007) Sentinel node biopsy for oral and oropharyngeal squamous cell carcinoma of the head and neck. Laryngoscope 117:1539–1551
Werner JA, Dunne AA, Ramaswamy A, Dalchow C, Behr T, Moll R, Folz BJ, Davis RK (2004) The sentinel node concept in head and neck cancer: solution for the controversies in the N0 neck? Head Neck 26:603–611
Stoeckli SJ, Alkureishi LW, Ross GL (2009) Sentinel node biopsy for early oral and oropharyngeal squamous cell carcinoma. Eur Arch Otorhinolaryngol 266:787–793
Ross GL, Soutar DS, MacDonald DG, Shoaib T, Camilleri IG, Robertson AG (2004) Improved staging of cervical metastases in clinically node-negative patients with head and neck squamous cell carcinoma. Ann Surg Oncol 11:213–218
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferris, R.L., Kraus, D.H. Sentinel lymph node biopsy versus selective neck dissection for detection of metastatic oral squamous cell carcinoma. Clin Exp Metastasis 29, 693–698 (2012). https://doi.org/10.1007/s10585-012-9492-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-012-9492-2