Abstract
Systemic chemotherapy has limited success in treating liver metastasis of colorectal cancer. Alternative approaches such as hepatic arterial infusion or trans arterial chemoembolisation aim to deliver the chemotherapy locally to address the predominant liver disease. Chemoembolisation with drug eluting beads (DEB) designed to deliver drug at the target over a protracted period of time is a new strategy to reduce the tumor burden of liver metastases. To test this hypothesis, DEB possessing anionic groups capable of ionically complexing with cationic drugs were synthesised by a suspension polymerisation method and were fractionated to produce an average size of 75 μm. The DEB were loaded with the desired concentration of either doxorubicin hydrochloride or irinotecan hydrochloride prior to administration by immersion in the drug solution, yielding essentially 100% loading efficiency. To determine their effect in vivo, a transplantable orthotopic and isogenic rat liver metastasis model was used which is based on intraportal injection of 4 × 106 β-galactosidase transfected CC531 rat colorectal cancer cells into male WAG/Rij rats. By MTT assay, the cells were shown to be sensitive to both drugs in vitro with the IC50 being by two orders of magnitude lower for doxorubicin (110 nM after 72 h) compared to irinotecan (25 μM after 72 h). For the in vivo phase, a differential expression of the ERK MAP kinase between tumor cells cultured in vitro and those inoculated in vivo was noted using Western blotting techniques. This was considered to be indicative of passage-induced cell senescence that reduced the sensitivity of the tumor cells to DEB chemoembolisation. This notwithstanding, administration of DEB loaded with irinotecan or doxorubicin by single injection into the hepatic artery showed significant anticancer activity, as measured by a reduction in the tumor burden of the liver and a corresponding reduction in liver weight. Comparing the two agents, irinotecan appears more advantageous because of its significant activity and excellent tolerability following administration at two dosages of either 20 or 30 mg/kg. Doxorubicin showed a narrower window of activity, being effective at 4 mg/kg but ineffective at the lower dose of 2 mg/kg. We conclude that chemoembolisation with DEB with either agent may have potential for treating patients with colorectal liver metastasis, although irinotecan DEB appeared to have a more favourable safety profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the existence of excellent screening and preventive strategies, colorectal carcinoma (CRC) remains a major public health problem in western countries. The American Cancer Society estimates there will be 153,760 new cases diagnosed in 2007, and 52,180 people will die of the disease. In the UK, an estimated 36,000 new cases were diagnosed in 2002, and 17,190 people died of colorectal cancer. Colorectal carcinoma is the second leading cause of death from cancer in the US. It also is the third most common malignancy in both men (after prostate and lung cancers) and women (after breast and lung cancers).
Patients with early, localized disease have a 5-year survival rate of 90%, whereas the overall 5-year survival rate is 64%. By the time they are diagnosed, some 25% of colon cancers and 50–70% rectal cancers will have spread through the bowel wall and metastasized to lymph nodes in 50–60% of patients. The most common site of extra-lymphatic involvement is the liver, with the lungs the most frequently affected extra-abdominal organ. Liver metastases are present at initial diagnosis in 15–30% of colorectal cancer cases, and a similar number of patients will develop liver metastases within a period of 3 years [1]. Patients with metastatic colorectal tumors frequently die of hepatic failure due to liver metastases.
Treatment options for patients with metastatic CRC are limited and clinical outcome is generally poor. Only a small number of people with liver metastases from CRC are eligible for curative surgical resection. Surgical resection in selected patients can achieve 25–39% 5-year survival [2]. For patients with unresectable disease where 5-year survival is extremely rare, there is renewed interest in local delivery of chemotherapy to the liver in an attempt to increase the effectiveness of these drugs against liver metastases. Strategies such as hepatic arterial infusion (HAI) chemotherapy with floxuridine have produced higher overall response rates but no consistent improvement in survival when compared with systemic chemotherapy [3–7].
Drug eluting beads (DEB) are an alternative approach to loco-regional treatment of liver metastases that combine the drug with the embolisation device by using the embolic device to reduce blood flow to the tumor whilst at the same time eluting a chemotherapeutic into the tumor via its own vasculature [8, 9]. Therefore, beads with the capability to elute drug may offer the possibility of precisely controlling the release and dose of the chemotherapeutic agent into the tumor bed. The use of doxorubicin loaded DEB in the chemoembolisation of hepatocellular carcinoma has demonstrated significant clinical benefits with respect to significantly reduced systemic drug dose, 75% response rate and 1- and 2-year survival rates of 92.5 and 88.9%, respectively [10].
In this study we examined the effectiveness of local delivery by DEB of irinotecan and doxorubicin. Irinotecan, a topoisomerase inhibitor, was the first drug other than 5-FU to demonstrate significant activity in metastatic CRC when administered intravenously. Current first- and second-line regimens containing irinotecan have become standard therapy in the treatment of metastatic CRC. However the most common and severe side effect of irinotecan treatment is diarrhoea; which can be dose limiting and sometimes necessitates termination of chemotherapy. Local delivery to the site of the tumor in the liver may reduce the likelihood of such side effects by limiting intestinal exposure.
Doxorubicin is an anthracycline antibiotic that blocks DNA and RNA synthesis, and although it is not used in clinical practice for treating colorectal cancer itself, there are reports of its use in chemoembolisation of metastatic disease in the liver. A study on trans-arterial chemoembolisation (TACE) for metastatic colorectal cancer has reported a complete response in 17% and 1- and 2-year survival rates of 68 and 37%, respectively, using doxorubicin as a single agent with lipiodol [11]. Other drugs such as cisplatin, mitomycin C and 5-fluorouracil have all been used successfully in the treatment of colorectal metastases to the liver, but the chemistry of these drugs is such that they do not form an interaction between drug and beads and so were not an option for DEB treatment in this study.
The rat model was chosen as a suitable model for TACE using the DEB, as it was previously demonstrated using this model that there was significant activity of irinotecan in terms of complete remission in 44% of rats and reduction of the mean tumor cell load by 66% [12]. In this model CC53l-lacZ cells are transplanted by portal vein injection into male WAG/Rij rats and detection of tumor cells is accomplished by measuring their β-galactosidase activity. This allows the determination of the number of cells using a chemo-luminescence assay. Here we report on the comparison of the efficacy of doxorubicin DEB with irinotecan DEB in the chemoembolisation of rat colorectal liver metastases. In addition, Western blotting is used to illustrate the differential expression of phosphorylated ERK MAP kinase between tumors cultured in vitro and those inoculated in vivo, indicative of passage-induced senescence and providing an explanation for a lower than expected sensitivity of the tumor cells to the DEB chemoembolisation.
Materials and methods
Cell culture
The CC531 colon carcinoma cell line was derived from an adenocarcinoma, induced by 1,2-dimethylhydrazine in the colon of a WAG/Rij rat. The cells are weakly immunogenic and moderately differentiated. A Lac-Z gene was transfected into the CC531 cell line for easy detection with a chemo-luminescence assay [13]. The Lac-Z gene codes for the β-galactosidase enzyme. The cell line was cultured in RPMI 1640 medium with 10% foetal calf serum in an incubator with 5% CO2 at 37°C. Flasks were seeded with 1 × 106 cells at a density of 1 × 105 cells/ml and were kept in the logarithmic growth phase. Cells were passaged every 4–5 days.
Drug eluting beads
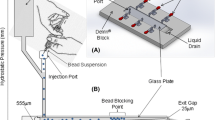
For this study, beads were made that could be loaded directly with either irinotecan or doxorubicin at the desired dosage a few hours prior to the chemoembolisation procedure. This is the concept of the DC Bead™ which is available commercially for the chemoembolisation of hypervascular tumors [8, 14]. The rat model requires a surgical procedure in order that the beads can be introduced directly into the hepatic artery. Owing to the size of the vessels in the animal, it was not possible to use any of the commercially available sizes of DC Beads for the study. A specific batch was therefore prepared in order to obtain sufficient beads for the entire study. The detailed process for the synthesis of the beads is described elsewhere [15] and so only a brief overview will be given here. The first step in the synthesis involved modification of polyvinyl alcohol (PVA) with N-acryloyl-aminoacetaldehyde dimethylacetal to form a reactive macromer. Beads were made by inverse suspension copolymerisation of this PVA macromer and 2-acrylamido-2-methylpropane-sulfonate sodium salt (AMPS) in butyl acetate and stabilised by cellulose acetate butyrate. The size of the beads could be controlled by a number of factors, including the stirrer speed and geometry. A size distribution of beads ranging from 30–1,200 μm were made, tinted with Reactive Blue 4 dye in order that they can be seen during handling and sieved into fractions. Beads with an average of 75 ± 25 μm in size were selected for this study (Fig. 1a). The beads were dispensed into vials (1 ml of beads and 5 ml of saline), steam sterilized and stored until required.
Drug was loaded by firstly removing the saline from the beads using a G22 filter needle and then by adding the appropriate dose of drug into the bead vial. Irinotecan hydrochoride (Campto®, Pfizer) at 20 mg/ml was used to achieve the desired dose of irinotecan/ml of hydrated beads and drug presence was indicated by a subtle change in color of the beads from blue to turquoise (Fig. 1b). In the case of doxorubicin hydrochloride, 50 mg vials of rapid dissolution powder were obtained (Adriamycin®, Pharmacia), stored at 4°C and prepared to the desired concentration prior to the procedure. Drug loading was indicated by a startling change in bead color from blue to intense red (Fig. 1c). Drug uptake in each case was essentially quantitative, as the ion-exchange process involves active uptake of the drug from solution [14, 16] and complete loading was achieved in less than 30 min. Drug release from the beads requires displacement by other ions and is a slow and controlled process for doxorubicin due to the strong interaction between drug and bead [9, 17]; release of irinotecan is quicker as the extent of interaction is less [14].
Animals
WAG/Rij male rats, aged 6–7 weeks, weighing 130–160 g were supplied by Charles River (Sulzfeld, Germany). They were kept under specific pathogen-free conditions in a ventilated rack with Macrolon-III cages (Ventirack, UNO Roestvastsaal, Zevenaar, The Netherlands). Before starting experiments, rats were acclimatized for 7 days. A temperature of 22 ± 1°C and a humidity of 50 ± 10% were maintained. Animals were kept in a dark-light rhythm of 12 h. Water and standard laboratory diet were provided ad libitum. The experimental protocol was approved by the local Animal Research Committee, in accordance with the national guidelines for animal care and use of laboratory animals.
In vivo inoculation
Batches of 20 rats were inoculated with CC531-lacZ cells within 1 day and used as single experimental unit. Tumor cell preparation and transplantation were conducted as previously described [12, 18, 19]. Briefly, for in vivo injection, 4 × 106 tumor cells were suspended in 0.2 ml phosphate buffered saline (PBS) without calcium and magnesium ions. 0.2 ml of Matrigel (extract of Engelbreth-Holm-Swarm-mouse tumor, Biomatrix EHS solution, Serva, Heidelberg, Germany) was added to the cell suspension and kept on ice until required.
A median laparotomy was performed under anesthesia (isoflurane) prior to tumor cell injection. The caecum was exteriorized from the abdominal cavity and a mesocolic vein was prepared for injection. Tumor cells were injected slowly under microscopic control using a 28-gauge needle. Cells were injected for at least 60 s, and then the puncture site was compressed between two cotton swabs for at least 1 min to prevent bleeding. The caecum was then returned to the abdomen, and the musculature closed with a running suture (4-0 vicryl, Ethicon, Norderstedt, Germany), and the skin closed with metal clips. Successfully inoculated rats were randomly assigned to treatment and control groups.
Embolisation procedure
Under isoflurane anesthesia, a high median laparotomy was performed and the liver inspected 7 days after the tumor cells were transplanted. Animals were included in the study when the presence of liver metastases was confirmed visually. The duodenum was encircled with two ligatures proximal and distal to the common bile duct to achieve as much caudad traction as possible by the length of the duodenum’s mesentery for inspecting the liver hilum. The gastrointestinal artery was prepared and ligated distally, close to the bifurcation into the upper pancreaticoduodenal arteries. The common and the proper hepatic artery were encircled and the blood flow was temporarily occluded by using two microvascular clamps. An arteriotomy of the gastroduodenal artery was performed, and a PVC catheter with an outer diameter of 0.61 mm was inserted and fixed by ligature.
The required volume of beads for a specific drug dose (based on mg/kg) was administered slowly after removing the temporary clamp from the proper hepatic artery. After injection, the catheter was removed and the artery ligated proximal to the arteriotomy to maintain the normal blood flow into the liver after removing the second temporary clamp. Finally, the gut was repositioned into the abdomen and the abdominal cavity closed.
The embolisation procedure was not without its complications. The DEB synthesised specifically for this study were fractionated into a size range that could be administered into the vessels of a rat. Loading of drug causes a further decrease in the diameter of the beads; coupled with the compressible nature of the DEB, it was found that if excessive force was used during delivery, non-target embolisation could occur which then resulted in exclusion of the animal from the study. Refinement of the delivery technique and modification of the viscosity of the DEB solution using various injection volumes was required in order to optimise a procedure that could be used reproducibly and reduce the occurrence of non-target embolisation. Successfully treated batches of rats were combined for evaluation only when gathered in a cohesive time period.
Rat liver preparation
Four weeks after tumor transplantation, the animals were euthanized. To reduce the blood content of the liver, the hepatic veins were perfused with about 10 ml 0.9% NaCl. The wet liver was weighed and kept at −80°C until further processing.
Quantification of tumor cells in liver
Frozen livers were homogenized mechanically in a lysis buffer solution (G2, Quiagen, Hilden, Germany) at a concentration of 500 mg of liver tissue per ml of lysis solution. Homogenates were then dissolved in the lysis solution at a ratio of 1:10 resulting in a final concentration of 50 mg liver tissue/ml solution. The mixture was centrifuged at 15,000 rpm, and the supernatant recovered.
The activity of β-galactosidase was determined as a measure of cell number using the Galacto-light-plus β-galactosidase Reporter Gene Assay kit (Tropix, Weiterstadt, Germany). 2 μl of supernatant was incubated in 200 μl of Galacton-plus assay buffer. 300 μl of accelerator II was added and immediately luminescence was measured for 30 min in a luminometer (Auto Lumat LB 953, EG&G Bertold, Wildbad, Germany). A standard curve was established by measuring healthy liver and tumor cells alone at concentrations from ∼1 × 105 to 1 × 108 cells/g liver tissue.
MTT assay
Logarithmically growing CC531-LacZ cells were trypsinised and 100 μl cell suspensions containing 3,000 cells were seeded in 96-well plates. After 1 day, cells were exposed to different concentrations of irinotecan or doxorubicin in 100 μl medium. Irinotecan was added to the CC531-LacZ cells at the following concentrations: 60, 30, 12, 6, 1.2 and 0.6 mg/l. Doxorubicin was added to the cells at: 60, 20, 6.7, 2.2, 0.74, 0.247, 0.082, 0.027, and 0.009 mg/l.
The effect on cell growth was measured at 48 and 72 h after addition of drug using the MTT assay. With this test, viable cells were detected by incubation with 3-(4,5-dimethylthiazol-2-yl)5-diphenyltetrazolium bromide (MTT), with formazan crystals forming in tumor cells that had survived. 10 μl of MTT was added to the cells and incubated for 3 h at 37°C; the medium containing drug and MTT was then discarded. Cells were lysed and formazan crystals dissolved by the addition of acidified 2-propanol (0.04 N HCl). Absorption was measured at 540 nm with reference filter of 690 nm in an automated microtiter plate spectrophotometer. The absorption was expressed as a percentage of untreated control cells.
Western blotting
To generate cell lysates of liver tissue, a sample of 20–40 mg tissue was mechanically homogenized in an equal amount of suspension and lysis buffer containing protease inhibitors. Samples were heated at 99°C for 10 min and centrifuged at 13,000 rpm at 4°C for 30 min. After protein determination of the supernatant using the BCA protein assay (Pierce), a determined amount of supernatant was mixed with 6× loading dye (Invitrogen) and dithiothreitol (DTT, final concentration 200 mM). Before loading, samples were denatured at 99°C for 10 min. Proteins (10–40 μg) were separated on 4–12% Bis-Tris gels (Invitrogen, NuPAGE) in SDS running buffer (Invitrogen) by electrophoresis (X-cell Sure Lock system, Invitrogen) at 200 V for 1 h. The full range Rainbow™ Markers (Amersham Biosciences) was used as a reference.
Following electrophoresis, the separated proteins were transferred onto a PVDF membrane (Hybond, Amersham Biosciences) in a blotting system filled with transfer buffer (Invitrogen) containing 20% methanol. After blocking the membrane with 5% dry milk and 0.1% Tween20 in Tris-buffered saline (TBS-T) for 1 h, the membrane was incubated with the first antibody in TBS-T with 1% dry milk at 4°C overnight (Table 1). Before incubation with the second antibody in TBS-T with 1% dry milk at room temperature for 1 h (all antibodies form Santa Cruz, Cell Signalling or Amersham Biosciences), the membrane was washed four times for 10 min with TBS-T. Antibody incubation was followed by washing again 4 times for 10 min and development of the membrane with electrochemiluminescence (ECL, Amersham Biosciences).
Statistics
Descriptive data are presented as the mean ± standard error (in case of summing up means) or standard deviation, as appropriate. Drug efficacy is expressed as percentage of treated versus control animals (T/C %). The non-parametric Wilcoxon Rank Sum test was used to compare tumor cell numbers and liver weights of treated animals with controls, a P value <0.05 was considered significant.
Results
MTT-assay
The kill-curves for irinotecan or doxorubicin administration to CC531-lac Z cells are shown in Fig. 2. After exposure to irinotecan, an IC50 of 50 μM was attained at 48 h and 25 μM after 72 h, comparing well with previous studies with irinotecan in this model [12]. On a mole for mole basis, doxorubicin was by more than two orders of magnitude more effective at killing tumor cells with an IC50 that was at 257 nM after 48 h and 110 nM after 72 h, but the slope of the cell kill curve was less steep than that of irinotecan. Just 18% (48 h) and 12% (72 h) of tumor cells survived at a 2 μM concentration, compared to 113% (48 h) and 93% (72 h) for irinotecan at the same concentration. These results demonstrate that the CC531-lac Z cells are sensitive to both irinotecan and doxorubicin in vitro and support the in vivo evaluation of both variants of DEB.
Dose-ranging experiments
Using a limited number of animals, dose-ranging experiments were performed in order to identify effective doses of each drug that would not induce undue toxicity (Table 2). In a previous study using the same orthotopic model and irinotecan, doses of up to 90 mg/kg were shown to be well-tolerated with minimal impact on body weight. Although not statistically significant, the dose-ranging suggested a dose around 30 mg/kg of irinotecan DEB would be effective in reducing tumor burden. Interestingly, one animal treated at 30 mg/kg irinotecan DEB produced a T/C of 0%; gross pathological analysis of the liver of this animal showed it to be virtually normal in appearance and weight, a particularly impressive outcome compared to the untreated control in the same experimental group (Fig. 3). Therefore, 20 and 30 mg/kg irinotecan DEB were selected for evaluation in the main study.
The procedure for introducing the DEB into the liver via the hepatic artery is crucial to the outcome; consequently, if the dose cannot be administered evenly into all segments of the liver, only partial chemoembolisation will occur and hence inefficient reduction of tumor cell number. This is clearly illustrated in Fig. 3 with the 60 mg/kg dose of irinotecan DEB, where almost half of the liver remains untreated with significant tumor visible beneath the liver capsule.
Doses of doxorubicin DEB in the range 15–60 mg/kg were efficacious in reducing the tumor burden in the liver but induced significant hepatotoxicity, often leading to death of the animal (Fig. 3, note the distinct yellow colouration in the liver treated with 30 mg/kg doxorubicin DEB). It was therefore decided to significantly reduce the doses to 2 and 4 mg/kg doxorubicin DEB for evaluation in the main study.
Chemoembolisation with doxorubicin and irinotecan DEB
Administration of beads alone (containing no drug) failed to yield any reduction in tumor cell burden (Fig. 4) and a non-significant decrease in liver weight (T/C 82%) was observed. Similarly, 2 mg/kg doxorubicin DEB had no effect on overall tumor burden reduction, however, it was observed to have a significant effect on liver weight reduction (T/C 79%). An increase in dose to 4 mg/kg doxorubicin DEB had a highly significant effect on both reduction of tumor cell number (T/C 28%) and liver weight (T/C 64%). Chemoembolisation using irinotecan DEB at both 20 and 30 mg/kg was effective at treating CC531-lac Z cells, both in terms of reduction of tumor burden (T/C 42 and 47%, respectively) and liver weight (T/C 62 and 54%). Overall, treatment with DEB chemoembolisation regardless of the drug type, resulted in reduction of the mean tumor cell number in the range 1.2–2.79 × 109 and the mean liver weight in the range of 7.6–13.1 g (Table 3).
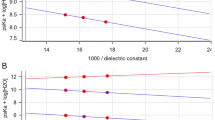
Evaluation of p-38 and ERK expression
The expression of p38 at 38 kDa was evaluated using Western blotting techniques in control liver (without tumor cells), liver with tumor and in normal tissue within a tumor-bearing liver. The p38 status was simultaneously determined in CC531 cells in vitro (Fig. 5). No difference in p38 status was found between all four samples. Therefore, the activated form of p38, phosphorylated-p38 (p-p38), was evaluated in tissue and cell samples. Activated p-p38 was detected after development with a super enhancer, indicating that p-p38 expression was very low. The in vitro CC531 cells showed the highest expression of p-p38. In tumor and control liver the presence of p-p38 was at similar levels, but in the normal appearing tissue of a metastasised liver p-p38 was less abundant.
The expression of the non-activated ERK1 was similar in tumor tissue and in vitro CC531 cells. When the activated form of ERK was evaluated, phosphorylated ERK (pERK), the CC531 cells in vitro showed a very high signal. In the other tissue samples pERK could not be detected, even not in tumor tissue. Actin levels, used to evaluate loading conditions, were comparable in tissue samples of the tumor liver and the in vitro CC531 cells, but were slightly lower in the control liver (data not shown).
Discussion
The use of CC531 colon carcinoma cells in tumor metastasis models has been evaluated in several studies [19–24]. It has been shown that CC531 cells injected into the vena mesocolica are a reliable tumor metastasis model. Additionally, the quantitative detection of CC531 cells by introduction of the LacZ gene is of great advantage. The sensitivity of this enzymatic tumor cell load detection is superior to histology, detecting 1 in 2,500 surrounding cells [13].
Rats transplanted with CC531-lac Z cells experienced an increase in tumor cell load. At 8 days post transplant, microscopic analysis of the liver surface revealed discrete tumor nodules fed by a significant network of neovascularisation. This demonstrates that the tumor cells have induced a rich blood supply via which intra-arterial treatment can be administered. Nevertheless, some variation in tumor burden has been observed. Although each animal was injected with the same number of tumor cells, differences in tumor cell growth were detected between animals [13]. Different cell batches used for implantation and the immune system of the rats may have played a role in extent of tumor cell outgrowth. Some variation in the original cell number due to differences in cell suspension preparation was unavoidable but was minimized by standardising inoculation of control and treated animals with the same tumor suspension, on the same day with identical operational procedures.
In this study, a single intra-arterial injection of DEB containing either irinotecan or doxorubicin at certain doses, was shown to be effective at reducing tumor burden in this orthotopic rat model. Irinotecan is indicated for treatment of colorectal metastases to the liver and is an important drug used in combination or as a monotherapy in first and second-line patients. It is not without significant side effects however, and local delivery from DEB could provide an option for reducing systemic levels and potentially toxicity. Doxorubicin has been used in TACE of hepatic metastases [11]. Despite such reports, systemic administration of doxorubicin is not listed under those drugs which are considered effective against colorectal cancer [25]. This may be because it has a low hepatic extraction compared to say, floxuridine (95–99% for floxuridine compared to 20–30% for doxorubicin [26]). Despite this, in vitro evaluation of doxorubicin on human colorectal cells shows that the drug is effective at levels 1,000 fold lower than those of 5-FU, which suggests it is presumably the fact that the drug is not reaching the tumor in vivo and/or the high systemic toxicity related to a narrow therapeutic window which is the issue with its effectiveness. Here, the MTT assay clearly demonstrated doxorubicin was potent against rat CC531 colon cancer cells. Hence, sustained delivery post-embolisation from drug-loaded beads appears to provide a method of delivering an effective dose of the drug local to the tumor.
Although useful in demonstrating efficacy of the DEB in this study, the use of such small animal models in embolisation studies is fraught with difficulty. First, the non target emobolisation was an issue that resulted probably as a consequence of the smallest beads passing through the capillary network and into the venous side where they could potentially locate in the lungs and the brain. This effect reduced the number of effective rats in the treated groups to a level that in view of the considerable treatment efficacy still allowed meaningful evaluation, but which could have obscured lower treatment effects. Then, the model does not lend itself to repeat embolisation procedures because of the surgical requirements. It is anticipated however, that for clinical use, local treatment with DEB could be repeated regularly, as has been the case for their use in the treatment of HCC [10]. Larger animals would have allowed the use of commercial products that represent the size of the devices used in humans; without some of the complications experienced here with non-target embolisation.
Moreover, there were biological issues with the model. Although the results demonstrate that chemoembolisation with DEB significantly reduces tumor burden in a rat model of colorectal metastases, a former study using the same model evaluated the combination of irinotecan with degradable starch microspheres yielded an 80% reduction in tumor cell load with 64% of cases resulting in complete remission [12]. To determine whether the model was performing as previously reported, the starch microsphere plus irinotecan experiment was repeated in a small number of rats (n = 4). Surprisingly, no effect on tumor burden was observed (data not shown), which prompted the question as to whether there had been a change in the behaviour of the CC531 cells used in the experiments.
Complexities of the rat orthotopic model
It was known that a different cell batch of CC531 had been used than in earlier experiments. These cells originated from an animal passage of CC531 cells, in an attempt to obtain new CC531 cells for in vivo inoculation. Passaging tumor cells in vivo can increase the aggressiveness of these cells, but repeat of the MTT assay with irinotecan produced kill curves with an IC50 very similar to that previously reported by Saenger et al. [12] thus proving that the cells were still sensitive to irinotecan whilst in culture. When in vivo however, there was an indication that their growth characteristics may have changed, as there was a distinct trend whereby tumor cell numbers within the liver were significantly higher in the earlier experiments compared to those conducted almost 1 year later in elapsed time (from 1.1 × 1010 cells at the beginning of the study to 2.15 × 108 cells 15 months later). Cells may alter their expression profile in vivo, for example, to survive the inflammatory system or the effects of chemotherapeutic intervention. For example, Matrigel used in this experiment increased the outgrowth possibility of tumor cells in vivo in relation to tumor cells inoculated without Matrigel [13]. This indicates that cells change their expression profile in response to the environmental matrix.
The reduced growth rate observed in vivo may therefore be indicative of cellular processes which may influence the degree to which the tumor model will respond to chemoembolisation with DEB. A known mechanism for insensitivity of tumor cells to chemotherapeutic agents is senescence [27]. Cellular senescence is the phenomenon of cells losing the ability to divide. In response to DNA-damage, e.g. caused by chemotherapeutics, cells either undergo senescence or self-destruct by apoptosis. Several stress mechanisms, including oncogenic stress and treatment with chemotherapeutic agents, may activate the mitogen-activated protein kinase (MAPK) p38. The p38 pathway has a central role in many cell signaling processes. Activation of p38 results in regulation of transcription factors and protein synthesis and also plays a role in apoptosis. The p38 tumor suppressor is associated with inhibition of cell cycle progression at the G1/S transition and G2/M checkpoints and negatively regulates cell growth.
In contrast, the activation of the extra cellular signal-regulated kinase (ERK) pathway is associated with cell proliferation, especially with transition from the G0-G1 phase to the S-phase. Thus, a high ERK level and low p38 contributes to tumor cell growth and a low ERK and high p38 level to senescence and insensitivity to chemotherapy [28–32]. Therefore, the ERK and p38 status of the CC531 cells in vitro and in vivo may give an indication of changes in tumor cell growth patterns and sensitivity to chemotherapy and is why they were evaluated in this study. The Western blotting data demonstrate the lower expression of p-ERK in tumor cells in vivo, compared to the cell stock in vitro, and consequently therefore, may indeed be indicative of cell senescence resulting in reduced sensitivity to chemotherapy.
Conclusion
DEB loaded with irinotecan or doxorubicin were evaluated in the orthotopic rat model of metastatic colorectal cancer. In relation to untreated animals, both tumor cell number and the liver weights of rats treated with irinotecan DEB at 20 and 30 mg/kg were significantly reduced. The narrow therapeutic window for doxorubicin DEB, with marginal activity at 2 mg/kg, significant activity at 4 mg/kg and substantial toxicity above this dose, renders it a less attractive option than irinotecan as a candidate for clinical investigation in patients with colorectal metastases to the liver.
It was anticipated that the effectiveness of DEB chemoembolisation would be superior to the previously reported starch microsphere chemoembolisation using irinotecan, as for DEB the drug is eluted over an extended period of time and the embolisation of tumor feeding vessels is permanent. Surprisingly, this was not the case and thus prompted a direct comparison in a small study population. In this sub-study, starch microspheres in combination with irinotecan 30 mg/kg failed to reduce the tumor cell load. This led to the assumption that the CC531 cells had become less sensitive. Differences in the tumor cell expression profile of ERK in vivo compared to in vitro support the hypothesis that some cells transformed into a senescent state as a result of cell passaging, rendering them less sensitive to chemotherapeutic action.
Regardless of this reduced sensitivity, DEB chemoembolisation was able to reduce tumor burden at statistically significant levels.
References
Adam R, Lucidi V, Bismuth H (2004) Hepatic colorectal metastases: methods of improving resectability. Surg Clin North Am 84:659–671
Fusai G, Davidson BR (2003) Management of colorectal liver metastases. Colorectal Dis 5:2–23
Kemeny N, Daly J, Reichman B, Geller N, Botet J, Oderman P (1987) Intrahepatic or systemic infusion of fluorodeoxyuridine in patients with liver metastases from colorectal carcinoma. A randomized trial. Ann Intern Med 107:459–465
Chang AE, Schneider PD, Sugarbaker PH, Simpson C, Culnane M, Steinberg SM (1987) A prospective randomized trial of regional versus systemic continuous 5-fluorodeoxyuridine chemotherapy in the treatment of colorectal liver metastases. Ann Surg 206:685–693
Wagman LD, Kemeny MM, Leong L et al (1990) A prospective, randomized evaluation of the treatment of colorectal cancer metastatic to the liver. J Clin Oncol 8:1885–1893
Rougier P, Laplanche A, Huguier M et al (1992) Hepatic arterial infusion of floxuridine in patients with liver metastases from colorectal carcinoma: long-term results of a prospective randomized trial. J Clin Oncol 10:1112–1118
Kemeny N, Cohen A, Seiter K et al (1993) Randomized trial of hepatic arterial floxuridine, mitomycin, and carmustine versus floxuridine alone in previously treated patients with liver metastases from colorectal cancer. J Clin Oncol 11:330–335
Lewis AL, Gonzalez MV, Lloyd AW et al (2006) DC Bead™: in-vitro characterisation of a drug delivery device for transarterial chemoembolization. JVIR 17:335–342
Lewis AL, Taylor RR, Hall B, Gonzalez MV, Willis SL, Stratford PW (2006) Pharmacokinetic and safety study of doxorubicin-eluting beads in a porcine model of hepatic arterial embolization. JVIR 17:1335–1343
Varela M, Real MI, Burrel M et al (2007) Chemoembolization of hepatocellular carcinoma with drug eluting beads: efficacy and doxorubicin pharmacokinetics. J Hepatology 46:474–481
Lang EK, Brown C Jr (1993) Colorectal metastases to the liver: selective chemoembolization. Radiology 189:417–422
Saenger J, Leible M, Seelig MH, Berger MR (2004) Chemoembolization of rat liver metastases with irinotecan and quantification of tumor cell reduction. J Cancer Res Clin Oncol 130:203–210
Wittmer A, Khazaie K, Berger MR (1999) Quantitative detection of lac-Z-transfected CC531 colon carcinoma cells in an orthotopic rat liver metastasis model. Clin Exp Metastasis 17:369–376
Taylor RR, Tang Y, Gonzalez MV, Stratford PW, Lewis AL (2007) Irinotecan drug eluting beads for use in chemoembolization: in vitro and in vivo evaluation of drug release properties. Eur J Pharm Sci 30:7–14
Goupil DW, Hassan H, Holland T Embolic compositions comprising polymers with a diol structure unit. WO 2001068720
Lewis AL, Gonzalez MV, Leppard SW, Brown JE, Stratford PW, Phillips GJ, Lloyd AW (2007) Doxorubicin eluting beads −1: effects of drug loading on bead char-acteristics and drug distribution. J Mater Sci Mater Med 18:1691–1699
Gonzalez MV, Tang Y, Phillips GJ, Lloyd AW, Hall B, Stratford PW, Lewis AL (2007) Doxorubicin eluting beads −2: methods for evaluating drug elution and in vitro: in vivo correlation. J Mater Sci Mater Med (in press)
Seelig MH, Leible M, Sanger J, Berger MR (2004) Chemoembolization of rat liver metastasis with microspheres and gemcitabine followed by evaluation of tumor cell load by chemiluminescence. Oncol Rep 11:1107–1113
Rodenbach M, Eyol E, Seelig MH, Berger MR (2005) Combination treatment of CC531-lac-Z rat liver metastases by chemoembolization with pemetrexed disodium and gemcitabine. J Cancer Res Clin Oncol 131:289–299
Li X, Mikkelsen IM, Mortensen B, Winberg JO, Huseby NE (2004) Butyrate reduces liver metastasis of rat colon carcinoma cells in vivo and resistance to oxidative stress in vitro. Clin Exp Metastasis 21:331–338
Nestler G, Schulz HU, Schubert D, Kruger S, Lippert H, Pross M (2005) Impact of taurolidine on the growth of CC531 coloncarcinoma cells in vitro and in a laparoscopic animal model in rats. Surg Endosc 19:280–284
Oosterling SJ, van der Bij GJ, Meijer GA et al (2005) Macrophages direct tumor histology and clinical outcome in a colon cancer model. J Pathol 207:147–155
van Duijnhoven FH, Aalbers RI, Rovers JP, Terpstra OT, Kuppen PJ (2003) Immunological aspects of photodynamic therapy of liver tumors in a rat model for colorectal cancer. Photochem Photobiol 78:235–240
van Duijnhoven FH, Tollenaar RA, Terpstra OT, Kuppen PJ (2005) Locoregional therapies of liver metastases in a rat CC531 coloncarcinoma model results in increased resistance to tumor rechallenge. Clin Exp Metastasis 22:247–253
DeVita VT Jr, Hellman S, Rosenberg SA (eds) (2004) Cancer principles and practice of oncology, 7th edn. Williams and Wilkins, Lippincott
Bast EC, Kufe D, Pollock RE, Weichselbaum RR, Holland JF, Frei E (eds) (2000) Cancer medicine, 5th edn. Hamilton, pp 1436–1464
Katakura Y (2006) Molecular basis for the cellular senescence program and its application to anticancer therapy. Biosci Biotechnol Biochem 70:1076–1081
Aguirre-Ghiso JA, Liu D, Mignatti A, Kovalski K, Ossowski L (2001) Urokinase receptor and fibronectin regulate the ERK(MAPK) to p38(MAPK) activity ratios that determine carcinoma cell proliferation or dormancy in vivo. Mol Biol Cell 12:863–879
Aguirre-Ghiso JA, Estrada Y, Liu D, Ossowski L (2003) ERK(MAPK) activity as a determinant of tumor growth and dormancy; regulation by p38(SAPK). Cancer Res 63:1684–1695
Aguirre-Ghiso JA, Ossowski L, Rosenbaum SK (2004) Green fluorescent protein tagging of extracellular signal-regulated kinase and p38 pathways reveals novel dynamics of pathway activation during primary and metastatic growth. Cancer Res 64:7336–7345
Bulavin DV, Fornace AJ Jr (2004) p38 MAP kinase’s emerging role as a tumor suppressor. Adv Cancer Res 92:95–118
Ranganathan AC, Zhang L, Adam AP, Aguirre-Ghiso JA (2006) Functional coupling of p38-induced up-regulation of BiP and activation of RNA-dependent protein kinase-like endoplasmic reticulum kinase to drug resistance of dormant carcinoma cells. Cancer Res 66:1702–1711
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eyol, E., Boleij, A., Taylor, R.R. et al. Chemoembolisation of rat colorectal liver metastases with drug eluting beads loaded with irinotecan or doxorubicin. Clin Exp Metastasis 25, 273–282 (2008). https://doi.org/10.1007/s10585-008-9142-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-008-9142-x