Abstract
Osteosarcoma is major cause of cancer-related death in the pediatric age group, and this is due to the development of pulmonary metastases that fail to be eradicated with current treatment regimes. Although there have been significant improvements in the long-term survival of such patients, 25–50% with initially non-metastatic disease, subsequently develop metastases and this remains the major cause of death for these patients. In this study, we report the multimodal activity of pigment epithelium-derived factor (PEDF) in inhibiting osteosarcoma growth, angiogenesis and metastasis. In vitro, we found that administration of recombinant PEDF (rPEDF) on two osteosarcoma cell lines (rat UMR 106-01 and human SaOS-2) significantly reduced tumor cell proliferation and increased apoptosis, as well as decreased cell invasion, angiogenesis, and increased adhesion to collagen type-1. Administration of rPEDF upregulated the mRNA expression of phenotypic osteoblast differentiation markers (ALP, pro-α1 collagen and osteocalcin) in a pre-osteoblastic cell line, UMR 201, and also increased mineralized nodule formation in both UMR 106-01 and SaOS-2. In vivo, rPEDF dramatically suppressed primary osteosarcoma growth and the development of macroscopic pulmonary metastases in an orthotopic model of human osteosarcoma (SaOS-2). Interestingly, no activity was seen in tumors grown subcutaneously, suggesting a paracrine interaction between PEDF and the bone microenvironment. Preliminary pharmacoevaluation studies demonstrated rPEDF stability within media containing serum and osteosarcoma cells, and no gross systemic toxicity was observed in vivo with rPEDF administration. These results suggest that PEDF is emerging as an attractive and clinically appealing drug candidate for the treatment of osteosarcoma
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumorigenesis entails the sequential acquisition of numerous genetic defects that renders neoplastic cells capable of growing, invading and eventually metastasising [1]. With significant advances in medical research, various tumor-specific targets have been identified, such as angiogenesis, aberrant cell-signaling pathways and disrupted cell-matrix interactions. It has been these targets that have been the center of much research, and currently several clinical trials are underway to evaluate the efficacy of such treatments against these targets in specific cancer types. However, despite the ability to affect key aspects of tumorigenesis, it is clear that the biological diversity of cancer mandates a multitargeted approach to therapy.
One tumor type that underscores the need for multimodal treatment is osteosarcoma. Osteosarcoma is the most common primary tumor of bone and the second highest cause of cancer-related death in young people. Although the current treatment of this aggressive tumor, which comprises of resection with pre- and post-operative multiagent chemotherapy, has resulted in substantial improvements in minimizing local recurrence and prolonging survival, one in three patients still develop pulmonary metastases, and this remains the major cause of death from this condition [2–4]. Therefore, it is the systemic spread of this tumor that has invariably occurred by the time of presentation that fails to be adequately eradicated with current treatment regimes. Furthermore, from clinical studies, dose intensification of chemotherapeutic agents, to the point of requiring hematopoietic stem cell reconstitution, has failed to consistently offer any added survival benefit to these patients [4]. One alternative source of potential osteosarcoma therapeutics is endogenous biologicals, which should preclude the problems faced with current cytotoxic agents such as drug resistance and toxicity. From our previous study of the progression of osteosarcoma adjacent to the growth plate cartilage in bones, we reported that this relatively avascular structure acts as a natural barrier to the progression of this tumor, and this is attributable to the expression of potent antiangiogenic factors such as pigment epithelium-derived factor (PEDF) that is expressed in the growth plate cartilage [5].
Pigment epithelium-derived factor is a widely expressed 50-kDa secreted glycoprotein that has been identified as more potent than any other known endogenous inhibitors of angiogenesis, being twice as potent as angiostatin and seven times as potent as endostatin [6]. It induces endothelial cell apoptosis through the Fas/FasL death pathway, as well as decreasing the expression of important pro-angiogenic factors such as vascular endothelial growth factor (VEGF) [6–8]. PEDF has shown the ability to suppress endothelial cell migration even in the presence of pro-angiogenic factors such as VEGF, FGF-1, FGF-2, and interleukin-8. In addition, PEDF [also known as early population doubling level cDNA-1 (EPC-1)] also plays a role in influencing cell proliferation by regulating the cell cycle [9] and inducing apoptosis [10] as well as inducing tumor cell differentiation toward a more mature phenotype [11, 12]. Furthermore, several clinical studies have shown that decreased levels of intratumoral PEDF have been correlated with higher microvessel density and a more metastatic phenotype and a poorer outcome in numerous malignancies, highlighting the key role PEDF plays in tumor progression [13]. Together, these findings suggest that the mechanisms by which PEDF exhibits multitargeted anticancer activity, is directly tumor cell proliferation, metastasis, and cell differentiation, as well as indirectly through tumor angiogenesis.
Therefore, in light of its potential endogenous antitumor activity, to date, few studies have tested the therapeutic potential of PEDF against a number of tumor models, both in vitro and in vivo, and have demonstrated inhibition of growth and the suppression of metastasis in cancers such as pancreatic carcinoma [14], prostate carcinoma [15], melanoma [10], neuroblastoma [11], and ovarian cancer [16]. In these studies, however, all have used models that have developed following ectopic implantation of cancer cell lines, most commonly subcutaneously. Hence, no paper has reported the role and antitumor effect of PEDF in an orthotopic model of cancer (that is, a tumor grown within its organ of origin).
In this study, we demonstrate for the first time, the therapeutic potential of PEDF against osteosarcoma and demonstrate its multitargeted antitumor activity using two clinically relevant orthotopic models of osteosarcoma [17, 18] and a panel of cell-based assays relevant to osteosarcoma proliferation, apoptosis, differentiation, angiogenesis, and metastasis. We also test the feasibility of recombinant PEDF (rPEDF) as a potential biological drug candidate in terms of protein stability and toxicity.
Materials and methods
Cell lines, culture conditions, reagents, and mice
Osteosarcoma cell lines, rat UMR 106-01 (from St. Vincent’s Institute of Medical Research) and human SaOS-2 (American Tissue Culture Collection, Manassas, VA, USA), were cultured in α-MEM (Invitrogen, Carlsbad, CA, USA) supplemented with 10% fetal calf serum (FCS, giving complete medium, CM). Rat pre-osteoblastic UMR 201 cells (kindly provided by A/Prof. K. W. Ng, St. Vincent’s Institute of Medical Research, Australia) were grown in α-MEM containing 2% vitamin A-deficient FCS. Culture conditions comprised of 37°C in a humidified 5% CO2 atmosphere. Commercially available human recombinant rPEDF was purchased from Upstate (NY, USA). Polyclonal antibodies to PEDF and VEGF were obtained from Upstate (NY, USA) and Santa Cruz Biotechnology, Santa Cruz, CA, USA, respectively. Secondary antibodies were purchased from Dako, Carpinteria, CA, USA. All animal experimentation was approved by the St. Vincent’s Health AEC. Five-week-old Balb/c nude mice were purchased from the Animal Resource Centre, Australia, and maintained under specific pathogen-free conditions.
Proliferation assay
UMR 106-01 and SaOS-2 osteosarcoma cells were treated with or without various concentrations of rPEDF. Cells were seeded at a density of 5 × 104 cells per well into 6-well plates and cultured in α-MEM media containing 10% FBS at 37°C/5% CO2 in triplicate. Cells were trypsinized and viable cells were quantified using trypan blue exclusion and a hemacytometer at days 1, 2, and 5 post-seeding.
Apoptosis assay
Osteosarcoma cells were seeded at a density of 1 × 104 into 96-well plates with varying concentrations of rPEDF in the presence or absence of 10 μg/ml of PEDF-antibody (Upstate, NY, USA) for 48 h in triplicates. Apoptotic cells were enumerated using the terminal dUTP nick end labeling (TUNEL) assay (Roche, Dee Why, NSW, Australia) according to manufacturer guidelines.
Invasion assay
Tumor cell invasiveness was examined using chamber inserts with 8 μm filter membranes (BD Biosciences, Palo Alto, CA, USA) coated with Matrigel (1:4 dilution; BD Biosciences). Each insert was filled with 5 × 104 cells suspended in 200 μl of ∝-MEM (serum-free) and placed into wells filled with 800 μl of ∝-MEM + 10% FCS, and incubated for 48 (UMR 106-01) and 72 h (SaOS-2) at 37°C in a 5% CO2 incubator. Cells that had invaded through the Matrigel-coated pores were quantitated after Quick-Dip (Froline, Australia) staining.
Collagen adhesion
About 24-well plates were coated with 0.2% collagen I (BD Biosciences) at 37°C for 60 min. Cells (1 × 105) were seeded and incubated at 37°C for 1 h. Wells were washed twice in 1 × PBS to remove non-adherent cells, and the remaining cells were enumerated at 200× magnification under three random fields using a Nikon Eclipse TE2000-U microscope (Nikon, Lidcombe, NSW, Australia) and photographed with SPOT Advanced software (SciTech, Aurora, IL, USA).
RT-PCR evaluation of osteoblastic differentiation markers
UMR 201 cells were grown in 175 cm2 culture flasks (Sigma Aldrich, Castle Hill, NSW, Australia) to ∼90% confluency and were then trypsinized and washed in 1 × PBS. The total cell number was split in a ratio of 1:20 and cells were resuspended in CM containing various concentrations of rPEDF and seeded into 75 cm2 culture flasks in duplicates. At intervals of 2, 4, 24, and 72 h, cells were trypsinized and placed into Trizol reagent (Invitrogen) for total RNA extraction according to manufacturer’s guidelines. The Expand Reverse Transcriptase-PCR and PCR Master (Roche) kits were utilized in accordance to guidelines. A negative control (no cDNA template) was always included in each series of PCRs. About 35 cycles were used at the respective or relatively close theoretical T ann, T ext = 72°C, T den = 94°C and PCR products electrophoresed on a 1% agarose gel. (For primers, refer to Table 1.)
Mineralized nodule formation
For mineralized nodule formation, 4,000 cells/well with various treatments were seeded in 24-well plates in CM supplemented with 1.4 mM CaCl2, 10 nM dexamethasone, and 50 μg/mL ascorbic acid. On day 3, 10 mM β-glycerophosphate was added, and on day 7, nodules were quantitated as previously described [19]. All chemicals were from Sigma-Aldrich and experiments were performed in triplicates.
Western blot analysis
Briefly, cells were grown to 90–95% confluency in the presence of various concentrations of rPEDF, harvested and total cellular proteins extracted using modified RIPA buffer (150 nM NaCL, 50 mM Tris pH 8.0, 1 mM EDTA, 0.1% SDS, and 1% Triton X-100) with PMSF (1 mM), leupeptin (2 μg/ml), aprotinin (2 μg/ml), and pepstatin (2 μg/ml). Approximately 15 μg of protein was electrophoresed through a 4–20% SDS-PAGE gel (Invitrogen) and electrotransferred onto a polyvinylidene difluoride membrane (PVDF; Invitrogen). Antibodies were visualized using the ECL-Plus chemiluminescence system (Amersham Biosciences, Buckinghamshire, UK). After initial blotting with VEGF antibody, the PVDF membrane was stripped with 325 mM Tris–HCl pH 6.7/10% SDS at 70°C and probed with PEDF antibody, then probed with GAPDH antibody (Santa Cruz, CA, USA). Semi-quantitative assessment of band intensities were made by Image Pro Plus (Media Cybernetics, Silver Spring, MD, USA) after normalization with GAPDH.
Protein stability
Protein stability was assessed by Western blot analysis of PEDF levels within ∝-MEM + 10% FCS with 0.5 or 5 nM concentrations of rPEDF in the presence of SaOS-2 cells. Protein levels were measured at days 0, 2, and 5 in duplicates.
In vivo studies in mice
Subcutaneous xenograft model
About 5 × 104 cells (>95% viability) suspended in 100 μl of 50% matrigel (BD Biosciences), ±rPEDF (25 nM) ± PEDF-antibody (4 μg, Upstate, NY, USA), were injected into the dorsum of 5-week-old female Balb/c (Animal Resource Centre, Australia) nude mice. Tumor volumes were calculated as π/6(length × width2) and were measured at twice weekly intervals, and mice were sacrificed at week 3 [20].
Orthotopic model
About 2 × 105 cells were injected into the proximal tibia of nude mice as previously described [17, 18]. Tumors were measured in the anteroposterior (AP) and lateral (L) planes) twice weekly using digital callipers and the volume was calculated using 4/3π[1/4(AP + L)]2. Affected limbs were X-rayed at 35 kV for 30 s using a cabinet system (Faxitron Corp., Wheeling, IL, USA). At week 5, the mice were sacrificed and the lungs were harvested to determine the extent of pulmonary metastasis. Briefly, lungs were gently washed in 1 × PBS and laid flat on a Petri dish. Careful examination of the lungs was performed under a dissecting microscope and the number of macroscopic metastatic nodules was counted. Tumors and whole lungs were harvested and fixed in 4% paraformaldehyde. All tissues were embedded in paraffin for histological analysis. Lung metastases were analyzed using Q500MC Qwin software (Leica, St. Gallen, Switzerland) following haematoxylin and eosin staining on 4 μm sections.
In vivo wound healing
A 1.5 cm superficial incision was made on the dorsum of the mouse. The wounds were then injected locally with rPEDF ± PEDF antibody or matrigel vehicle alone. Wounds were loosely closed with interrupted sutures and overlayed with antiseptic solution. Mice were sacrificed after 1 week and the skin over the dorsum of the mouse was harvested and processed for histological analysis.
Statistical analysis
Results were analyzed using MedCalc for Windows Version 8.1 (Medcalc Software, Mariakerke, Belgium). In vitro and in vivo data were analyzed for statistical significance using the Students t-test (two-tailed). p ≤ 0.05 was considered significant.
Results
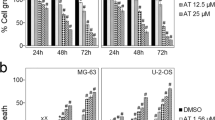
PEDF inhibits osteosarcoma cell proliferation and induces apoptosis in vitro
We firstly evaluated the antiproliferative effect of rPEDF treatment on two clonal osteosarcoma cell lines, rat UMR 106-01 and human SaOS-2. Both cell lines were treated with increasing concentrations of rPEDF (0, 0.5, 5, and 25 nM) over 1, 2, and 5 days. In both UMR 106-01 and SaOS-2 cells, a statistically significant dose-dependent reduction in cell proliferation was observed, which was most marked on day 5 (Fig. 1a). In UMR 106-01 cells, after 24 h, treatment with rPEDF resulted in a 51% (0.5 nM), 64% (5 nM), and 71% (25 nM) reduction in cell numbers compared to control (p < 0.003). Cell proliferation remained suppressed after 48 h, with rPEDF inhibiting cell proliferation by 42% (0.5 nM), 53% (5 nM), and 64% (25 nM) compared to controls (p < 0.0002). The most marked decrease in cell proliferation was seen at day 5, where there was a 56% (0.5 nM), 72% (5 nM), and 78% (25 nM) reduction in cell numbers compared to control (p < 0.0002). In SaOS-2 cells, a similar effect on cell proliferation was also seen with rPEDF (Fig. 1a). After 24 h, rPEDF resulted in a 60% (0.5 nM), 72% (5 nM), and 92% (25 nM) reduction in cell numbers compared to control (p < 0.007). By 48 h, cell proliferation was inhibited by 42% (0.5 nM), 53% (5 nM), and 64% (25 nM) compared to controls (p < 0.00003). The decrease in cell proliferation was most marked by day 5, where there was a 92% (0.5 nM), 80% (5 nM), and 81% (25 nM) reduction in cell numbers compared to control (p < 0.0005).
PEDF inhibits osteosarcoma cell proliferation in vitro. (a) Effect of rPEDF on cell proliferation measured at days 1, 2, and 5. (b) Effect of rPEDF on apoptosis. SaOS-2 cells were treated with increasing concentrations of rPEDF ± PEDF antibody and the degree of apoptosis was assessed by TUNEL assay (left) by comparing the number of apoptotic cells (red) to the total number of cells (blue) (right). Data shown are mean ± SD of triplicates or quadruplicates. *p < 0.05 versus rPEDF + PEDF-antibody control, **p < 0.01 versus rPEDF + PEDF-antibody control (Student’s t-test, two-tailed)
One of the mechanisms through which PEDF has been shown to inhibit tumor cell proliferation is via induction of cell apoptosis [10]. Therefore, to determine whether rPEDF induced apoptosis in osteosarcoma, SaOS-2 cells were treated with varying concentrations of rPEDF for 48 h and then analyzed by TUNEL assay to determine the percentage of cells undergoing apoptosis. As shown in Fig. 1b, rPEDF dose-dependently increased the rate of apoptosis, with 25 nM of rPEDF inducing a 20-fold increase compared to control (0 nM), and this was shown to be reversible with an antibody to PEDF (p < 0.01). These results are consistent with the 66% reduction in the number of SaOS-2 cells observed (relative to seeding number) after 24 h with 25 nM of rPEDF.
Effects of PEDF on osteosarcoma cell invasion and collagen adhesion in vitro
Previous studies have reported that decreased intratumoral levels of PEDF is associated with an increased incidence of metastatic spread and a poorer prognosis [21]. Given that metastasis to the lung remains the major cause of death from osteosarcoma, the role of PEDF in the inhibition of osteosarcoma metastasis was investigated by studying its effect on tumor cell invasion through Matrigel. We found that treatment with rPEDF resulted in a significant dose-dependent inhibition of cellular invasion, with 25 nM of rPEDF demonstrating a 99% (UMR 106-01) and 86% (SaOS-2) reduction (p < 0.001) (Fig. 2a).
PEDF reduces metastatic potential and changes cellular morphology in vitro. (a) Effect of rPEDF on cellular invasion through Matrigel-coated 8 μm pores. Representative slides are shown (below). (b Cellular adhesion to collagen type-1 coated plates with rPEDF. c Representative images demonstrating increased cell adhesion and a flattened cell morphology compared to control and the formation of cell clusters (arrows). Data shown are mean ± SD of triplicates or quadruplicates. *p < 0.05 versus control, **p < 0.01 versus control, ***p < 0.001 versus controls (Student’s t-test, two-tailed)
Biochemically, PEDF has been shown to have high affinity to collagen type-1, the most abundant extracellular matrix protein present within bone [22]. Furthermore, as cellular adhesion to the surrounding extracellular matrix is an important phenotype in cancer metastasis, the effects of rPEDF on cellular adhesion to collagen type-1 was studied. It was observed that rPEDF treatment significantly increased cellular adhesion to collagen type-1 in a dose-dependent manner (p < 0.01) (Fig. 2b). Interestingly, closer inspection of the adherent cells revealed that, in the presence of increased PEDF, the morphology of the osteosarcoma cells changed to appear flatter and there was a tendency to form clusters with neighboring cells (Fig. 2c). Together with the findings that PEDF decreases Matrigel invasion, these results suggest that PEDF may play an important role in regulating tumor cell invasion and attachment to the surrounding extracellular matrix, which are key aspects in determining a malignant cell’s metastatic potential.
rPEDF upregulates expression of osteoblastic markers in pre-osteoblastic UMR 201 cells and enhances in vitro mineralized nodule formation in osteosarcoma cells
We have previously reported that, through in vivo studies, PEDF is likely to play an important regulatory role in osteoblastic differentiation, endochondral ossification, and bone remodeling [23]. Further studies have also shown that when rat-derived pre-osteoblastic cells, UMR 201, are exposed to a potent and well-known osteoblastic differentiator, retinoic acid (1 μM), a temporal increase in PEDF mRNA expression is observed, which is maximal at 4 h and tapers back to baseline (unpublished data). These results suggested that PEDF expression may be involved in the induction of osteoblastic differentiation. Hence, to further investigate this, the in vitro effects of rPEDF (0.5 and 5 nM) on UMR 201 cells was analyzed by determining the gene expression pattern of phenotypic osteoblastic markers after treatment with rPEDF. Using RT-PCR, the expression of pro-α1 collagen, alkaline phosphatase (ALP) and osteocalcin mRNA in vitro by UMR 201 cells, in response to rPEDF, was determined over time. Cells were exposed for 2, 4, 24, and 72 h. In keeping with a pre-osteoblastic phenotype, in UMR 201 cells, pro-α1 collagen mRNA (a marker of early osteoblastic differentiation) was constitutively expressed in UMR 201 cells, whereas ALP (a marker of differentiating osteoblasts) and osteocalcin (a marker of mature osteoblasts) mRNA was not detectable (Fig. 3a).
Effect of PEDF on the expression osteoblastic markers and on mineralized nodule formation. (a) Pre-osteoblastic UMR 201 cells were treated with rPEDF. RT-PCR results demonstrating the temporal expression of a panel of osteoblastic markers: Col-1 pro-α1 collagen, ALP alkaline phosphatase, OC osteocalcin, GAPDH glyceraldehyde-3-phosphate dehydrogenase. Semi-quantitative densitometry assessment of the degree of mineralized nodule formation was performed using GAPDH as a loading control. (b) The effect of rPEDF on mineralized nodule formation in UMR 106-01 (left) and SaOS-2 (right). Data shown are mean ± SD of triplicates or quadruplicates. *p < 0.05 versus control (Student’s t-test, two-tailed)
Pro-α1 collagen expression
With administration of 0.5 nM of rPEDF, semi-quantitative analysis of RT-PCR results showed that there was less than twofold upregulation of pro-α1 collagen mRNA expression, relative to constitutional levels, at 2 h (10% increase) and reached a maximum at 4 h (50% increase), and returned toward baseline by 72 h (10% increase). In comparison, 5 nM of rPEDF resulted in an increase in pro-α1 collagen mRNA levels by 20–30% over 24 h, and this return to base line at 72 h. This temporal increase in the mRNA expression over the first 24 h, may suggest that the cells have progressed toward a more mature phenotype.
Alkaline phosphatase (ALP)
Upon treatment with 0.5 nM of rPEDF, positive induction of ALP mRNA expression was observed only at 72 h (approximately ninefold increase). With 5 nM of rPEDF, ALP mRNA expression was seen at 2 h ( approximately sixfold increase), and remained elevated at 4 h (sevenfold increase), however this returned to baseline at 24 h. Interestingly, upregulation of ALP mRNA expression (approximately twofold increase) was detected after 72 h.
Osteocalcin
Osteocalcin is a marker of mature osteoblasts, and its expression in pre-osteoblastic UMR 201 cells, in response to any morphogen, has not been previously described [24]. In this study, the presence of both 0.5 and 5 nM of rPEDF resulted in positively induction of osteocalcin mRNA expression at 2 h, which remained elevated at 72 h (∼7–11-fold increase) when compared to steady state levels. Although this data is preliminary, these results suggest that treatment with rPEDF results in upregulation of specific osteoblastic markers, in particular osteocalcin, which are indicative of a more mature osteoblastic phenotype.
Mineralized nodule formation
Other than the expression of specific osteoblastic genes, one of the major characteristics of osteoblasts, as they differentiate in vitro, is the ability to form mineralized nodules which reflects bone forming ability [19]. Hence, in order to determine whether rPEDF stimulated differentiation in osteosarcoma cell lines in vitro, UMR 106-01, and SaOS-2 cells were treated with varying concentrations of rPEDF and a mineralized nodule formation assay was performed. The results of this assay showed that both cell lines exhibited dose-dependent increases in mineralized nodule formation, which was most marked with 25 nM of rPEDF (p < 0.01) (Fig. 3b). Together with the findings that PEDF upregulates the expression of osteoblastic markers in UMR 201 cells, this data suggests that PEDF is likely to be involved in promoting osteoblastic and osteosarcoma cell differentiation.
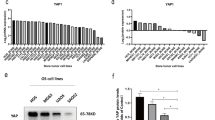
PEDF affects angiogenesis in osteosarcoma by inhibition of VEGF
PEDF has been shown to inhibit tumor neoangiogenesis by two main mechanisms; directly, through inducing endothelial cell apoptosis [7], and indirectly, by down-regulating the expression of potent pro-angiogenic factors such as VEGF [8]. Hence, to determine the antiangiogenic role of PEDF in osteosarcoma, its effect on VEGF protein synthesis within UMR 106-01 and SaOS-2 cells was evaluated by Western blot analysis of cellular lysates from cells treated with varying concentration of rPEDF over 48 h. As shown in Fig. 4, UMR 106-01 cells demonstrated a significant reduction in VEGF protein levels, with a greater than 45% inhibition seen with the various concentration of rPEDF tested (p < 0.05). Similar results were also observed in the SaOS-2 cells, with VEGF protein levels being less than 60% compared to control (p < 0.05). Interestingly, in both cell lines, 5 nM of rPEDF exhibited the greatest inhibition of VEGF compared to 0.5 and 25 nM, however this difference was not statistically significant.
Effect of PEDF on VEGF production in vitro. (a) Western blot analysis with VEGF antibody on cellular lysates of UMR 106-01 cells (above) and SaOS-2 cells (below) treated with rPEDF. (b) Semi-quantitative densitometry analyzes of VEGF level are demonstrated relative to control. GAPDH was used to normalize the levels of VEGF protein. Data shown are mean ± SD
PEDF inhibits osteosarcoma growth and metastasis in an orthotopic model
Having demonstrated the antitumor effects of rPEDF on osteosarcoma cells in vitro, attention was turned toward investigating the role and activity of PEDF on orthotopic growth and metastasis. Given that the SaOS-2 cell line is human-derived and thus clinically relevant, we used these cells and orthotopically implanted them into the proximal tibiae of nude mice co-administered with rPEDF (25 nM) ± PEDF antibody (Ab) at the time of inoculation. We found a significant reduction in primary tumor size and growth rates of ∼40% in tumors that were treated with rPEDF, compared to controls (p < 0.05). In addition, there was a greater than 70% reduction in the mean number of macroscopic pulmonary metastases seen in rPEDF-treated mice compared to controls (p < 0.002) (Fig. 5 ). Interestingly, although treatment with rPEDF at the time of tumor inoculation resulted in decreased tumor size and the number of macroscopic metastases, no significant difference was seen in the degree of MVD or VEGF expression compared to controls. Of note, the degree of PEDF immunostaining in the tumors did not appear greater than that of controls (data not shown).
PEDF inhibits osteosarcoma growth and metastasis in two orthotopic models. (a) Effect of rPEDF ± PEDF-antibody on SaOS-2 cells grown in vivo. Representative primary tumors of rPEDF treated and rPEDF + PEDF-antibody groups are shown (left). Radiographs demonstrate bony tumor involvement within the proximal tibia (inserts). Tumor volume (middle) and the development of macroscopic metastases (arrows; right) are displayed. (b) UMR 106-01 (left) and SaOS-2 (right) tumors treated with rPEDF were grown subcutaneously and were compared to control and rPEDF with PEDF-antibody groups. Data shown are mean ± SEM of at least five mice in each group. *p < 0.05 versus controls, **p < 0.002 versus controls (Student’s t-test, two-tailed)
To determine whether the bone microenvironment plays an important role in the antitumor activity of PEDF, ectopic tumors were grown subcutaneously by injecting UMR 106-01 and SaOS-2 cells, with or without rPEDF and with or without PEDF antibody, into the dorsum of nude mice. Concentrations of rPEDF used were identical to that used for orthotopic inoculations (25 nM). Cells were suspended within a 50% Matrigel bioscaffold to prevent dissipation within the subcutaneous layer. As shown in Fig. 5, no significant difference in tumor volumes was observed between the three groups in both cell lines. These results suggest that the inhibition of osteosarcoma progression by PEDF is largely dependent on an interaction with bone microenvironment.
Pharmacoevaluation of rPEDF
For effective drug development, there is a need to address potential side-effect issues as early as possible post-discovery. Since PEDF may theoretically disrupt the normal physiological process of angiogenesis and proliferation, we monitored potential local side-effects by administering rPEDF and comparing the rate of wound healing with control and rPEDF + PEDF antibody groups. After 1 week, there was no significant difference in the rate of wound closure and healing between the groups, both macroscopically and histologically (Fig. 6a, b). In addition, mice that were orthotopically or ectopically inoculated with tumors with rPEDF treatment did not lose weight (Fig. 6c), and there was no overt evidence of lethargy or soft stools. Another aspect of drug development examined was the stability of PEDF in serum together with SaOS-2 cells. By Western blot analysis we demonstrated no significant degradation of rPEDF at 37°C over 2 and 5 days at 0.5, 5, and 25 nM concentrations of rPEDF (Fig. 6d).
rPEDF stability and effect of rPEDF on in vivo wound healing. (a) Effect of rPEDF on physiological wound healing. Incisions were made on the dorsum of mice (∼1.5 cm) down to the deep fascia and rPEDF ± PEDF-antibody was infiltrated into the wound (left). Wounds (n = 4) were loosely closed with continuous sutures and overlayed with antiseptic solution (middle). Matrigel alone was used as a control. Results at 1 week show no difference in wound healing (right). (b) H&E section demonstrating epidermis (E) and underlying dermis (D). No obvious difference seen in wound healing (arrows) at 1 week. (c) Body weights of mice bearing orthotopic tumors. (d) Western blot analysis of stability of rPEDF in media containing fetal calf serum and in the presence of SaOS-2 cells over 5 days. Conditioned media from SaOS-2 cells was used as a control. Data shown are mean ± SD (n = 5 in each group for in vivo study)
Discussion
Although the long-term survival of patients diagnosed with osteosarcoma has considerably improved with the advent of effective chemotherapy, still a significant proportion of patients succumb to this condition, invariably from metastatic dissemination to the lungs [2]. The limitation of current chemotherapeutic regimes for osteosarcoma, like for most other tumors, is the inability to eradicate micrometastases at the time of presentation, whether this is due to the inability to achieve adequate therapeutic levels or the development of drug-resistant clones. Thus, there is a real need for new therapies to be developed with improved efficacy, especially against refractory tumors.
In the present study, the multitargeting role of PEDF against osteosarcoma growth and progression has been demonstrated. Through the use of the recombinant protein, we have shown that PEDF not only reduces osteosarcoma cell proliferation but also induces apoptosis. Previous studies have shown that PEDF activates apoptosis through the Fas/FasL death pathway [7], and this is supported by a recent study by Takenaka et al. who described the direct effect of PEDF on tumor cell proliferation in MG63 osteosarcoma cells in vitro [25]. In their paper, in vitro cell proliferation was significantly inhibited through a combination of apoptotic cell death and a decrease in DNA synthesis, which is consistent with that shown in other current published reports in the literature [10, 11, 26]. PEDF’s ability to directly suppress tumor growth has been shown to occur at two levels, through induction of cell apoptosis [10, 25], and also through regulation of the cell cycle leading to a decrease in the entry of cells into the DNA synthesis (S) phase [9, 25].
Intriguingly, in this present study, rPEDF was only effective in inhibiting orthotopic, not ectopic (subcutaneous) tumor growth, implicating a possible interaction between the tumor cells and the bone microenvironment resulting in paracrine regulation of cell proliferation. This result is interesting in that in other subcutaneous xenograft tumor models, both PEDF-overexpression and rPEDF has resulted in suppression of primary tumor growth [26–28]. Therefore, it is unclear why in osteosarcoma, PEDF does not alter tumor growth when implanted subcutaneously. One possible explanation for this is that in vivo, PEDF antitumor activity against osteosarcoma grown orthotopically, is enhanced by the presence of collagen type-I, which is main extracellular matrix protein within bone [29]. In contrast, the predominant collagen within subcutaneous tissue is collagen type-VI [30]. A recent study by Hosomichi et al. reported that PEDF’s interaction with collagen type-I through its collagen-binding motif is essential for suppression of tumor progression and antiangiogenesis [31]. This is further supported by Meyer et al., who demonstrated that rPEDF forms complexes with collagen type-I from bovine cornea and vitreous, and proposed that this collagen-binding property may play a key role in modulating cell migration and adhesion as well as regulating angiogenesis in tissues such as the eye and bone, which are rich in collagen type-1 [22]. However, it is interesting that in vitro, PEDF exerts it antitumor activity against osteosarcoma without the presence of collagen type-1. Therefore, further research is indeed warranted to elucidate the reasons behind the disparity in antitumor activity of rPEDF in orthotopically and subcutaneous-grown osteosarcoma cells.
Physiologically, PEDF is widely expressed throughout foetal and adult tissues, including the adult brain, spinal cord, eye, liver, plasma, heart, lung, and bone [32–36]. However, relatively little is known to date of its true biological role within bone. We have previously reported that PEDF mRNA expression is upregulated in osteoblasts during endochondral ossification, osteoblastic differentiation and bone remodeling, indicating a regulatory role during skeletogenesis [23]. Our current finding that PEDF upregulates the expression of key osteoblastic differentiation markers in pre-osteoblastic UMR 201 cells and increases mineralized nodule formation in osteosarcoma cells lends further credence to this theory. Furthermore, as the degree of differentiation is often inversely related to the malignant potential of neoplastic cells, the ability of PEDF to steer osteosarcoma cells toward a more mature phenotype, may contribute to its overall capacity to slow growth kinetics, and decrease metastatic spread [37]. The ability of PEDF to induce differentiation has also been noted in neuroblastomas [11], retinoblastomas [38], and prostate cancer cells [12], however the mechanisms through which this occurs remains to be elucidated. In retinoblastoma (Y79 cells), PEDF has been shown to promote differentiation, which is manifested by the development of neurite-like extension, increased expression of neuronal differentiation markers and growth arrest [38]. Similarly, in neuroblastoma cell lines (SK-N-BE(2) and SH-SY5Y), rPEDF induced differentiation in vitro, evidenced by the formation of neurite outgrowths in a dose-dependent manner, and in vivo, by increased immunohistochemical staining for neurofilament, a marker for neuronal differentiation [11].
Angiogenesis, the formation of new blood vessels from pre-existing ones, is central to tumor growth, invasion and metastasis [39]. Our studies show that, not only does PEDF act directly on endothelial cells, but it also down-regulates the synthesis of VEGF in osteosarcoma cells, therefore abrogating a strong stimulus of angiogenesis. This is in keeping with the findings of Takenaka et al. who also showed similar down-regulation of VEGF in MG63 osteosarcoma cells [25]. However, recent studies have attempted to elucidate the molecular interaction between VEGF and PEDF, and it is becoming increasingly clear that there is a highly complex cross-talk between inducers and inhibitors of angiogenesis [7, 8, 27]. VEGF has been shown to upregulate c-FLIP through dephosphorylation of the transcription factor nuclear factor of activated T-cells (NFATc2), which inhibits caspase-8 dependent apoptosis in endothelial cells [40]. On the other hand, PEDF has been shown to oppose this, by triggering c-Jun NH2-terminal kinase (JNK)-mediated rephosphorylation of NFATc2, hence blocking c-FLIP synthesis. To add further complexity to this interplay between VEGF and PEDF, another mechanism reported by Cai et al., involves the activation of γ-secretase-dependent cleavage of the C terminus of VEGF-receptor 1 (VEGF-R1) [8]. Furthermore, PEDF interferes with the phosphorylation of VEGF-R1, and consequently, may modulate angiogenic signaling via VEGF-R2. Although several other investigators have shown similar direct inhibition of VEGF expression with PEDF, the mechanism through which this occurs is still unclear. Recently, Zhang et al. reported that PEDF inhibited hypoxia-induced increases in VEGF promoter activity, hypoxia inducible factor-1 (HIF-1) nuclear translocation and MAP kinase phosphorylation, hence inhibiting VEGF expression at a transcriptional level [41]. Needless to say, these data underscores the complexity of the interaction between these two molecules.
Pulmonary metastasis remains the major challenge for osteosarcoma management, as local recurrence rates after primary resections are relatively low [2, 3]. Although PEDF could conceivably inhibit metastases through antiangiogenesis, inhibition of tumor cell proliferation and increased apoptosis, and pro-differentiation, we have demonstrated the profound effects of PEDF on in vitro tumor cell invasion and adhesion and more impressively on the formation of metastasis. The significant reduction of metastases with PEDF treatment strongly indicates that it plays a key antimetastatic role, possibly through regulation of the microenvironment or direct changes in tumor cell phenotype [42]. In a study by Guan et al. [43], decreased Matrigel invasion of malignant U251 cells was also seen in cells overexpressing PEDF. They showed that this was associated with a significant down-regulation in matrix metalloproteinase-9 (MMP-9) activity, which plays an important role in extracellular matrix degradation. In osteosarcoma, overexpression of MMP-9 has been shown to strongly correlate with the acquisition of metastatic potential and the development of pulmonary metastases [44]. This concept of PEDF-induced inhibition of tumor invasion is further supported by our previous findings demonstrating the ability of the epiphyseal growth plate cartilage, which highly expresses PEDF, to act as a effective barrier to osteosarcoma progression and invasion [5]. Furthermore, similar results, in terms of PEDF’s antiinvasive activity, have also been reported in melanoma [27]. Interestingly, Notari et al. reported a negative regulatory loop, in which the activation of MMP-2 and MMP-9 by hypoxia or VEGF results in proteolytic inactivation of PEDF, hence abolishing its antitumor activity [45].
Another possible mechanism through which PEDF inhibits tumor migration and invasion could be mediated through its interaction with collagen type-I. Kozaki et al. found that PEDF secreted by colon cancer cells bound with high affinity to collagens type-I and -III, and its expression levels inversely correlated with the tumors cell’s metastatic capacity [46]. Similarly, Meyer et al. postulated that the collagen binding property of PEDF regulates cellular interactions and functions as a cell adhesion molecule and/or a substrate adhesion molecule. This is evidenced by the fact that, at a molecular level, PEDF has binding sites for collagens and glycosaminoglycans, which are characteristic features of cell adhesion molecules [22]. This is consistent with the findings of this present study, where rPEDF in vitro resulted in increased cellular adhesion to collagen type-I. Therefore, together with reduced invasive capacity, this data indicates that in osteosarcoma, PEDF may be central to regulating tumor cell invasion through the surrounding extracellular matrix and also the establishment of metastasis at distant sites.
Although rPEDF treatment at the time of tumor inoculation resulted in suppression of in vivo tumor growth, no significant difference, at the time of animal sacrifice (∼5 weeks), was observed in the degree of angiogenesis (MVD and VEGF immunostaining) and PEDF levels in the rPEDF-treated tumors compared controls. This is likely to be the result of rPEDF being proteolytically degraded over time. However, as PEDF has high affinity for collagen type-1, which is the principle protein in bone, it is probable that the presence of rPEDF within the intramedullary space would be prolonged, hence exerting sustained bioactivity. Furthermore, this would have been facilitated by the co-administration of Matrigel, with which the SaOS-2 tumors were suspended, thus providing a potential scaffold for rPEDF to act on the osteosarcoma cells, and limiting dissipation. One can speculate that the initial high levels of rPEDF caused a decrease in tumor cell burden and also influenced other aspects of osteosarcoma tumourigenicity, which have been demonstrated in vitro, such as invasion, differentiation, and angiogenesis resulting in reduced primary tumor growth and metastasis.
Significant stumbling blocks to clinical application of therapeutic biomolecules are associated toxic side-effects and lack of stability. Our studies demonstrate that rPEDF did not perturb physiological proliferation and angiogenesis during the process of wound healing. Furthermore, the recombinant protein was stable in serum and when exposed to osteosarcoma cells in culture. Hence, in summary our work provides strong evidence of the multifunctional activity of PEDF in inhibiting osteosarcoma primary tumor growth and preventing metastasis, therefore making it an appealing and clinically promising agent for targeted molecular anticancer therapeutics.
References
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100:57–70
Ferrari S, Smeland S, Mercuri M et al (2005) Neoadjuvant chemotherapy with high-dose Ifosfamide, high-dose methotrexate, cisplatin, and doxorubicin for patients with localized osteosarcoma of the extremity: a joint study by the Italian and Scandinavian Sarcoma groups. J Clin Oncol 23:8845–8852
Petrilli AS, de Camargo B, Filho VO et al (2006) Results of the Brazilian Osteosarcoma treatment group studies III and IV: prognostic factors and impact on survival. J Clin Oncol 24:1161–1168
Ek ET, Choong PF (2006) The role of high-dose therapy and autologous stem cell transplantation for pediatric bone and soft tissue sarcomas. Expert Rev Anticancer Ther 6:225–237
Quan GM, Ojaimi J, Nadesapillai AP et al (2002) Resistance of epiphyseal cartilage to invasion by osteosarcoma is likely to be due to expression of antiangiogenic factors. Pathobiology 70:361–367
Dawson DW, Volpert OV, Gillis P et al (1999) Pigment epithelium-derived factor: a potent inhibitor of angiogenesis. Science 285:245–248
Volpert OV, Zaichuk T, Zhou W et al (2002) Inducer-stimulated Fas targets activated endothelium for destruction by anti-angiogenic thrombospondin-1 and pigment epithelium-derived factor. Nat Med 8:349–357
Cai J, Jiang WG, Grant MB et al (2006) Pigment epithelium-derived factor inhibits angiogenesis via regulated intracellular proteolysis of vascular endothelial growth factor receptor 1. J Biol Chem 281:3604–3613
Pignolo RJ, Francis MK, Rotenberg MO et al (2003) Putative role for EPC-1/PEDF in the G0 growth arrest of human diploid fibroblasts. J Cell Physiol 195:12–20
Abe R, Shimizu T, Yamagishi S et al (2004) Overexpression of pigment epithelium-derived factor decreases angiogenesis and inhibits the growth of human malignant melanoma cells in vivo. Am J Pathol 164:1225–1232
Crawford SE, Stellmach V, Ranalli M et al (2001) Pigment epithelium-derived factor (PEDF) in neuroblastoma: a multifunctional mediator of Schwann cell antitumor activity. J Cell Sci 114:4421–4428
Filleur S, Volz K, Nelius T et al (2005) Two functional epitopes of pigment epithelial-derived factor block angiogenesis and induce differentiation in prostate cancer. Cancer Res 65:5144–5152
Ek ET, Dass CR, Choong PF (2006) Pigment epithelium-derived factor: a multimodal tumor inhibitor. Mol Cancer Ther 5:1641–1646
Hase R, Miyamoto M, Uehara H et al (2005) Pigment epithelium-derived factor gene therapy inhibits human pancreatic cancer in mice. Clin Cancer Res 11:8737–8744
Doll JA, Stellmach VM, Bouck NP et al (2003) Pigment epithelium-derived factor regulates the vasculature and mass of the prostate and pancreas. Nat Med 9:774–780
Cheung LW, Au SC, Cheung AN et al (2006) Pigment epithelium-derived factor is estrogen sensitive and inhibits the growth of human ovarian cancer and ovarian surface epithelial cells. Endocrinology 147:4179–4191
Fisher JL, Mackie PS, Howard ML et al (2001) The expression of the urokinase plasminogen activator system in metastatic murine osteosarcoma: an in vivo mouse model. Clin Cancer Res 7:1654–1660
Dass CR, Ek ET, Contreras KG et al (2006) A novel orthotopic murine model provides insights into cellular and molecular characteristics contributing to human osteosarcoma. Clin Exp Metastasis 23:367–380
Nadiminty N, Lou W, Lee SO et al (2006) Prostate-specific antigen modulates genes involved in bone remodeling and induces osteoblast differentiation of human osteosarcoma cell line SaOS-2. Clin Cancer Res 12:1420–1430
Fahmy RG, Dass CR, Sun LQ et al (2003) Transcription factor Egr-1 supports FGF-dependent angiogenesis during neovascularization and tumor growth. Nat Med 9:1026–1032
Ek ET, Dass CR, Choong PF (2006) PEDF: a potential molecular therapeutic target with multiple anti-cancer activities. Trends Mol Med 12:497–502
Meyer C, Notari L, Becerra SP (2002) Mapping the type I collagen-binding site on pigment epithelium-derived factor. Implications for its antiangiogenic activity. J Biol Chem 277:45400–45407
Quan GM, Ojaimi J, Li Y et al (2005) Localization of pigment epithelium-derived factor in growing mouse bone. Calcif Tissue Int 76:146–153
Choong PF, Martin TJ, Ng KW (1993) Effects of ascorbic acid, calcitriol, and retinoic acid on the differentiation of preosteoblasts. J Orthop Res 11:638–647
Takenaka K, Yamagishi S, Jinnouchi Y et al (2005) Pigment epithelium-derived factor (PEDF)-induced apoptosis and inhibition of vascular endothelial growth factor (VEGF) expression in MG63 human osteosarcoma cells. Life Sci 77:3231–3241
Streck CJ, Zhang Y, Zhou J et al (2005) Adeno-associated virus vector-mediated delivery of pigment epithelium-derived factor restricts neuroblastoma angiogenesis and growth. J Pediatr Surg 40:236–243
Garcia M, Fernandez-Garcia NI, Rivas V et al (2004) Inhibition of xenografted human melanoma growth and prevention of metastasis development by dual antiangiogenic/antitumor activities of pigment epithelium-derived factor. Cancer Res 64:5632–5642
Browne M, Stellmach V, Cornwell M et al (2006) Gene transfer of pigment epithelium-derived factor suppresses tumor growth and angiogenesis in a hepatoblastoma xenograft model. Pediatr Res 60:282–287
Viguet-Carrin S, Garnero P, Delmas PD (2006) The role of collagen in bone strength. Osteoporos Int 17:319–336
Takasaki S, Fujiwara S, Shinkai H et al (1995) Human type VI collagen: purification from human subcutaneous fat tissue and an immunohistochemical study of morphea and systemic sclerosis. J Dermatol 22:480–485
Hosomichi J, Yasui N, Koide T et al (2005) Involvement of the collagen I-binding motif in the anti-angiogenic activity of pigment epithelium-derived factor. Biochem Biophys Res Commun 335:756–761
Bilak MM, Corse AM, Bilak SR et al (1999) Pigment epithelium-derived factor (PEDF) protects motor neurons from chronic glutamate-mediated neurodegeneration. J Neuropathol Exp Neurol 58:719–728
Tombran-Tink J, Mazuruk K, Rodriguez IR et al (1996) Organization, evolutionary conservation, expression and unusual Alu density of the human gene for pigment epithelium-derived factor, a unique neurotrophic serpin. Mol Vis 2:11
Kuncl RW, Bilak MM, Bilak SR et al (2002) Pigment epithelium-derived factor is elevated in CSF of patients with amyotrophic lateral sclerosis. J Neurochem 81:178–184
Sawant S, Aparicio S, Tink AR et al (2004) Regulation of factors controlling angiogenesis in liver development: a role for PEDF in the formation and maintenance of normal vasculature. Biochem Biophys Res Commun 325:408–413
Uehara H, Miyamoto M, Kato K et al (2004) Expression of pigment epithelium-derived factor decreases liver metastasis and correlates with favorable prognosis for patients with ductal pancreatic adenocarcinoma. Cancer Res 64:3533–3537
Thomas DM, Johnson SA, Sims NA et al (2004) Terminal osteoblast differentiation, mediated by runx2 and p27KIP1, is disrupted in osteosarcoma. J Cell Biol 167:925–934
Tombran-Tink J, Chader GG, Johnson LV (1991) PEDF: a pigment epithelium-derived factor with potent neuronal differentiative activity. Exp Eye Res 53:411–414
Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285:1182–1186
Zaichuk TA, Shroff EH, Emmanuel R et al (2004) Nuclear factor of activated T cells balances angiogenesis activation and inhibition. J Exp Med 199:1513–1522
Zhang SX, Wang JJ, Gao G et al (2006) Pigment epithelium-derived factor downregulates vascular endothelial growth factor (VEGF) expression and inhibits VEGF-VEGF receptor 2 binding in diabetic retinopathy. J Mol Endocrinol 37:1–12
Fidler IJ (2003) The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev Cancer 3:453–458
Guan M, Pang CP, Yam HF et al (2004) Inhibition of glioma invasion by overexpression of pigment epithelium-derived factor. Cancer Gene Ther 11:325–332
Kido A, Tsutsumi M, Iki K et al (1999) Overexpression of matrix metalloproteinase (MMP)-9 correlates with metastatic potency of spontaneous and 4-hydroxyaminoquinoline 1-oxide (4-HAQO)-induced transplantable osteosarcomas in rats. Cancer Lett 137:209–216
Notari L, Miller A, Martinez A et al (2005) Pigment epithelium-derived factor is a substrate for matrix metalloproteinase type 2 and type 9: implications for downregulation in hypoxia. Invest Ophthalmol Vis Sci 46:2736–2747
Kozaki K, Miyaishi O, Koiwai O et al (1998) Isolation, purification, and characterization of a collagen-associated serpin, caspin, produced by murine colon adenocarcinoma cells. J Biol Chem 273:15125–15130
Acknowledgments
E.T.H.E is supported by scholarships awarded by the University of Melbourne, the Royal Australasian College of Surgeons, and the National Health and Medical Research Council of Australia (NH&MRC). This study was generously supported by grants from the Australian Orthopaedic Association, the Victorian Orthopaedic Research Trust Grant, and the Cancer Council of Victoria.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors declare that they have no competing financial interests.
Rights and permissions
About this article
Cite this article
Ek, E.T.H., Dass, C.R., Contreras, K.G. et al. Inhibition of orthotopic osteosarcoma growth and metastasis by multitargeted antitumor activities of pigment epithelium-derived factor. Clin Exp Metastasis 24, 93–106 (2007). https://doi.org/10.1007/s10585-007-9062-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-007-9062-1