Abstract
The guanine nucleotide exchange factor Tiam1 regulates numerous biologic properties including migration and invasion. We demonstrated previously that colon tumor cells biologically selected for increased migration were increased in Tiam1 expression. Cells selected for increased Tiam1 expression or that ectopically overexpress Tiam1 were increased in metastatic potential. Here, we demonstrate that Tiam1 regulates additional functions associated with metastasis, including reduced cellular adhesion and resistance to anoikis. Tiam1 effects on cellular migration are mediated through its downstream substrate, Rac. Increased Tiam1 expression also leads to anoikis-resistance, whereas decreasing Tiam1 expression by siRNA sensitizes cells to this form of apoptosis; however, Tiam1’s regulation of anoikis is Rac-independent. Staurosporine sensitivity is also Rac-independent, suggesting Tiam1’s effects on apoptosis require other effectors. As many of the observed phenotypes are characteristic of a transition of transformed epithelial cells to a mesenchymal-like phenotype, we also examined biochemical properties associated with an EMT. We demonstrate an increase in vimentin expression in cell lines that overexpress Tiam1 and have a more metastatic phenotype. Concomitant with this increase, we observe a decrease in E-cadherin expression in these cells. Lastly, we stained a panel of human colorectal specimens and adjacent normal tissue, and demonstrate that Tiam1 is overexpressed in a subset of human colorectal tumors. In summary, in colon tumor cells, Tiam1 affects multiple properties associated with acquisition of the metastatic phenotype, and may represent a marker of colon tumor progression and metastasis in a subset of tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal carcinoma ranks third in incidence and cancer deaths for both men and women in the United States, and will account for approximately 10% of all cancer deaths in this country in 2006 [1]. When colorectal cancer is discovered at an early stage, prognosis is very good, with an 85–95% 5-year survival rate for patients in stage I, and 60–80% for patients in stage II. However, prognosis drops precipitously for later stages, to 30–60% 5-year survival for patients in Stage III, and to less than 5% for Stage IV [2]. While adjuvant chemotherapies and newer targeted therapies such as bevacizumab (Avastin) [3], are having some impact on survival, colorectal carcinoma patients still succumb to metastatic disease. Therefore, an enhanced understanding of colorectal carcinoma metastasis is critical to extending the lives of patients. We reported previously that increased expression of the guanine nucleotide exchange factor (GEF) Tiam1 in cells biologically selected for increased migratory potential, or by ectopic overexpression, leads to increased cellular migration and confers growth of colon cancer cells at metastatic sites in an orthotopic nude mouse model [4]. Thus, further study of Tiam1 functions and signaling may be important in a more complete understanding of colorectal carcinoma metastasis.
Tiam1’s best-characterized function in cells is as a guanine nucleotide exchange factor. In vitro, Tiam1 has been shown to act primarily as an exchange factor for Rac1 and Cdc42, and to a lesser extent, for RhoA [5] and for Rac alone [6]. In vivo, Tiam1 also acts as an exchange factor for Rac1 [5], and we have demonstrated an increase in GTP-bound Rho and Rac when Tiam1 is overexpressed [4]. It is a member of the Dbl gene family of GEFs, as it contains an 150 amino acid region termed the Dbl homology (DH) domain, which is the catalytic region for nucleotide exchange [7]. In addition Tiam1 contains two PH domains, one at the C-terminal (PHc) and one at the N-terminal (PHn) [7], two N-terminal PEST domains, associated with protein stability [8], a discs-large homology region (DHR), or PDZ domain, located between the N-terminal PH domain and the DH domain, and a Ras binding domain (RBD) [9, 10]. Two additional regions in the Tiam1 protein, a coiled coil (CC) domain, and another region, termed Ex, are immediately adjacent to the PHn domain [11]. Finally, a glycine at position two in Tiam1 is a potential myristoylation site, though myristoylation is not sufficient for membrane localization [12].
Tiam1 is conserved amongst vertebrates, implying a critical importance to cellular function. In addition, Tiam1 is expressed in almost all adult tissues, with especially high expression in the brain and testis. The conservation and broad expression pattern of Tiam1 across many tissue types indicates that Tiam1 may have crucial roles in cellular function [13]. Thus, Tiam1 has been implicated in numerous cellular processes, including cellular migration and adhesion. However, whether Tiam1 acts positively or negatively on these functions remains controversial, as previous studies on these roles of Tiam1 differ on the basis of cell type, substrate, and experimental design, suggesting that Tiam1 regulation may be cell-type dependent.
A number of recent reports suggest that alterations in Tiam1 expression/function might contribute to tumorigenesis and carcinoma progression. Tiam1 was first identified by proviral tagging in combination with in vitro selection for invasiveness from murine leukemia cells [7], and the human homolog is highly conserved [13]. A study in renal cell carcinoma (RCC) cell lines found that Tiam1 expression was generally inversely correlated with invasive potential, but that downregulation of Tiam1 alone was not sufficient to confer an invasive phenotype. A distinct mutation in Tiam1 in the RCC cell lines was sufficient to transform NIH 3T3 cells and may therefore play a major role in RCC progression [14]. Tiam1 expression has also been examined in two human giant-cell lung carcinoma cell lines of differing metastatic capacities. Hou, et al. found that the highly metastatic cells express more Tiam1 protein than do the low metastatic cells [15]. In addition, the authors concluded that an antisense Tiam1 expression vector transfected into the high metastatic lung carcinoma cell line results in a reduction in the in vitro invasiveness of these cells. Insights into the potential role of Tiam1 in tumorigenesis and progression have also been obtained by the generation of a strain of Tiam1−/− mice [16]. These mice are resistant to the development of Ras-induced skin tumors, and the tumors that do develop are small and slow growing. Moreover, the putative tumor metastasis suppressor nm23H1 has been shown to interact with Tiam1 at the N-terminus, and negatively regulates its activity [17], further suggesting that Tiam1 has pro-tumorigenic and/or pro-metastatic properties.
Recent studies demonstrate that in breast and colon carcinomas, overexpression of Tiam1 is associated with a more malignant potential; in human breast carcinomas, a close correlation was observed between increased Tiam1 expression and increased tumor grade [18], and increased Tiam1 expression is associated with increased metastatic potential in colon cancer cell lines [4]. We have also shown that in a panel of 11 breast carcinoma cells lines of varying migratory and metastatic potential, the more migratory or more metastatic lines express more Tiam1 protein than do the less migratory or metastatic lines [19].
Recent work [20] has also demonstrated that the metastatic potential of eight colon tumor cell lines positively correlates with Tiam1 gene expression. In agreement with that study, we demonstrated previously that overexpression of Tiam1 contributes directly to the metastatic phenotype of colon cancer cells, and that ectopic overexpression of Tiam1 is sufficient to increase cellular migration and metastatic potential of these cells [4]. As acquisition of a metastatic phenotype requires more than simply increased migration, this current study examines additional biologic properties induced by Tiam1. This work demonstrates that Tiam1 regulates cellular adhesion and sensitivity to anoikis by distinct signaling pathways. We suggest an underlying mechanism for Tiam1-induced phenotypic changes is its ability to promote a more mesenchymal-like phenotype.
Materials and methods
Cell lines
SW480 [21] human adenocarcinoma cells (ATCC, Rockville, MD) cells were cultured in 10 cm dishes in Dulbecco’s Modified Eagle Medium/ Ham’s F12 Nutrient Mixture (DMEM/F12) (GIBCO/BRL; Rockville, MD) supplemented with 10% fetal bovine serum (FBS) (Hyclone; Logan, UT) in the absence of antibiotics. Subclones of SW480 increased in migration have been described [4] and were grown under identical conditions to SW480. Briefly, these cells were selected for increased cellular migration by serial migration through Boyden chamber migration assays. SW480 clones transfected with Tiam1 C1199HA, and vector control clones have also been described [4] and were grown as detailed above, except that media was supplemented with 500 μg/ml G418 (Fisher Scientific; Houston, TX). For passage of all cell lines, both floating and attached cells were harvested.
Cell lysis and immunoblots
Confluent dishes of cells were washed twice with Ca2+, Mg2+-free ice cold phosphate-buffered saline (135 mM NaCl, 1.5 mM KH2PO4, 8.0 mM Na2HPO4, pH 7.4, 2.5 mM KCl) and lysed on ice in radioimmunoprecipitation assay A (RIPA A) lysis buffer (20 mM sodium phosphate buffer [19% v/v 1 M NaH2PO4-H2O, 81% v/v 1 M Na2HPO4], pH 7.4, 5 mM NaPPi, 5 mM EDTA, 150 mM NaCl, 0.5% sodium deoxycholate (Na DOC), 0.5% SDS, 1% Triton X-100, 1 mM Na2VO4) plus a Protease Inhibitor Cocktail tablet (Roche; Nutley, NJ) by passing the cells and buffer through a 25 gauge needle approximately 10 times. Lysates were cleared by centrifugation at 13,000 rpm at 4°C for fifteen minutes and protein in the lysate was quantitated with the Detergent-Compatible (DC) Protein Assay system (BioRad; Hercules, CA).
Proteins (30 μg of whole-cell lysate) were boiled for 5 min in Laemelli’s sample buffer and resolved by SDS-PAGE on an 8% or 12% polyacarylamide gel. Immunoblotting was performed as described previously [4, 22]. Blots were probed with anti-HA antisera, diluted 1:500 (Santa Cruz Biotechnology; Santa Cruz, CA); anti-Tiam1 antisera (C16), diluted 1:800 (Santa Cruz Biotechnology); anti-Rac antibody, diluted 1:1000 (Upstate Biotechnology, Inc; Charlottesville, VA); anti-E-cadherin antibody, diluted 1:1000 (BD Transduction Laboratories; San Jose, CA); anti-vimentin antibody, diluted 1:1000 (Chemicon International, Inc.; Temecula, CA); anti-β-actin antibody, diluted 1:10,000 (Upstate Biotechnology, Inc.); or anti-vinculin antibody, diluted 1:10,000 (Sigma-Aldrich, Inc.; St. Louis, MO). Horseradish peroxidase-conjugated secondary antisera, either goat anti-mouse IgG or goat anti-rabbit IgG (BioRad) diluted 1:3000 were used to detect the primary antisera.
Northern blots
Northern blotting was performed as described previously [4, 23]. Briefly, mRNA was extracted from cells at 90% confluency using the GenElute Direct mRNA Miniprep Kit (Sigma; St. Louis, MO) and quantitated on a spectrophotometer. Five micrograms of mRNA per sample was loaded on a 1% agarose gel containing 17% v/v formaldehyde and 5% v/v 0.4 M MOPS. The probe, either Tiam1 or GAPDH, was labeled with α-32P dCTP using the RediPrime II random labeling kit according to manufacturer’s instructions (Amersham).
Migration assays
Migration was assessed using a wound healing assay. Cells were plated in 6-well plates and allowed to grow for 4 days to confluency. At time 0, media was removed and cells were wounded with a p10 pipet tip. Cells were washed to remove debris, media was replaced, and plates were returned to a culture incubator. Photographs were taken at time points indicated in Results. If wound healing was done in conjunction with transfection with siRNA (see below), cells were transfected 24 h after plating and wounded 72 h after transfection. Each condition was photographed in three separate fields and the same field at each time point was used, allowing the percent of wound closed by infiltration of migratory cells to be quantitated from the photographs using Image J software (National Institutes of Health).
Cell detachment
Equal numbers of cells were plated. Thirty-eight hours later, media was removed; cells were washed in PBS, and fresh media was added. At time points indicated in the figure, media was collected, cells were washed, and the wash buffer was collected. The floating cells were pelleted, suspended in a known volume of media, and viable cells (by trypan blue exclusion) were counted in a hemacytometer.
Anoikis and apoptosis assays
Cells were grown in 10 cm dishes until approximately 80% confluency. Anoikis was assayed in one of two ways. Cells were either (1) placed in 15 ml conical tubes with filter caps at a concentration of 500,000 cells per ml in a total volume of 8 ml complete DMEM/F12 media, and tubes were placed on a continuous rotator in a cell culture incubator or (2) cells were plated in 6-well dishes covered with 4% agarose to prevent cell attachment. At time points indicated in the Results section, cells from one tube or well for each cell line were collected and cells were stained with propidium iodide (PI) (50 μg/ml PI, 0.1% sodium citrate, 0.1% triton X-100, in PBS) and incubated at room temperature for 30 min. Stained cells were analyzed by fluorescence-activated cell sorting (FACS) analysis (Beckman Coulter EPICS XL-MCL machine; Beckman Coulter; Miami, FL). In addition, cells were collected at time of counting and analyzed as above for control cell death. Death is presented as percent of cells in sub G0/G1.
To examine apoptosis induced by staurosporine (Sigma-Aldrich, Inc.), cells were plated in 6-well dishes. Cells were either mock or siRNA transfected. Forty-eight hours later, media was removed and fresh media containing staurosporine or vehicle alone was added to the cells. Cells were collected after 12 h and assayed for apoptosis as above.
Immunocytochemistry
Cells were grown on glass coverslips. Cells were fixed with 3.7% paraformaldehyde, permealized by cold acetone (or 0.25% Triton-X 100 for β-catenin), then blocked with 5% horse serum and 1% goat serum diluted in PBS, and incubated with antibody or anti-sera to vimentin, diluted 1:100, (Chemicon International, Inc.); E-cadherin, diluted 1:75 (Zymed; San Francisco, CA), or β-catenin, diluted 1:200 (Upstate Biotechnology). Fluorescent-conjugated secondary antisera diluted 1:400 (goat anti-mouse/Alexa-594 or anti-rabbit/Alexa-594) were used to detect the primary antisera. Primary and secondary antibodies were diluted in the blocking buffer. Primary antibodies were incubated at 4°C overnight, and secondary antibodies were incubated for 1–4 h at room temperature. Nuclei were stained with Hoescht (Molecular Probes). Immunoreactive proteins were visualized with a Zeiss Axioplan2 microscope (Carl Zeiss, Inc.; Thornwood, NY) equipped with a HBO 100 mercury lamp. Images were captured using a Hamamatsu ORCA-ER digital camera (Hamamatsu Corp; Bridgewater, NJ) and Image Pro Plus software (Media Cybernetics, Inc.; Silver Spring, MD).
Human tumor panel and staining
Surgically resected specimens of human colorectal tumors, frozen within 20 min of removal, were obtained at the University of Texas MD Anderson Cancer Center. Specimens were sectioned, blocked with 5% horse serum and 1% goat serum diluted in PBS, and stained with anti-Tiam1 antisera (C16), diluted 1:50 (Santa Cruz Biotechnology). Fluorescent-conjugated secondary antisera (goat anti-rabbit IgG/cy-5 diluted 1:600), was used to detect the primary antisera. Primary and secondary antibodies were diluted in the blocking buffer. Primary antibody was incubated at 4°C overnight, and secondary antibody was incubated for 1–4 h at room temperature. Immunoreactive proteins were visualized with the Zeiss Axioplan2 microscope system described above.
siRNA
siRNA oligonucleotides to Tiam1 and Rac1 were purchased from Ambion, Inc. (Austin, TX). Multiple oligonucleotides for each gene were tested, and only one was needed for each protein to achieve maximal downregulation. The Tiam1 oligonucleotide sense sequence was GGGAAUAUUUGAUGACAUUtt and antisense was AAUGUCAUCAAAUAUUCCCtc. Sense Rac1 sequence was GGAGAUUGGUGCUGUAAAAtt and antisense was UUUUACAGCACCAAUCUCCtt. Cells were transfected using TransFast Reagent (Promega Corp., Madison WI). Cells were plated in 6 well dishes, and 24 h later, when cells were approximately 40% confluent, transfection was performed.
Results
Tiam1 expression in a model system of colorectal carcinoma
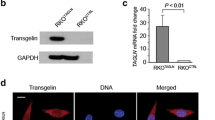
Previously, we demonstrated that stable sublines of SW480 cells biologically selected for increased migratory potential were increased in ability to grow at metastatic sites and were increased in Tiam1 expression relative to non-tumorigenic, poorly migratory parental cells [4]. The model system consists of the parental, low migratory, non-metastatic colorectal carcinoma cell line SW480, three biologically selected cell lines (SW480 mmig3 Clone1, SW480 mmig3 Clone6, and SW480 mmig3 Clone8), and three stable clones of SW480 that have been transfected with Tiam1 C1199 (2TClone42, 2TClone65, and 2TClone68). Isolation of these clones was described previously [4]. As shown in Fig. 1a, the biologically selected cell lines overexpress Tiam1 protein and mRNA. C1199 protein expression is demonstrated in Fig. 1b. To further examine biologic function of Tiam1, a single siRNA oligonucleotide was used to downregulate its expression, as described in Materials and methods section. Successful downregulation of both endogenous and ectopically expressed C1199HA Tiam1 is shown in Fig. 1c. Transfection with 300 nM of a single oligonucleotide decreased Tiam1 protein levels by an estimated 80%. Transfection of multiple oligonucleotides at same or lower concentrations (data not shown) did not result in the same protein reduction as with the single oligonucleotide, therefore, a single oligonucleotide was chosen for use in all experiments. Thus, the multiple approaches at affecting Tiam1 expression, including biologically selected cell lines, and cell lines specifically increased or decreased in Tiam1 expression, provide a unique model for studying Tiam1-regulated functions.
Tiam1 expression in a model system of colorectal carcinoma. (a) Immunoblotting and Northern blotting for Tiam1 were performed on SW480, SW480 mmig3 Clone1, SW480 mmig3 Clone6, and SW480 mmig3 Clone8. (b) Protein expression from the transfected C1199 construct. Lysates from 2TClone42, 2TClone65, and 2TClone68 were immunoprecipitated with HA, separated by SDS-PAGE, transferred to nitrocellulose, and then immunoblotted for Tiam1. The first two lanes contain whole-cell lysate. (c) Expression of Tiam1 after siRNA silencing. Twenty-four hours after plating, SW480, mmig3 Clone1, mmig3 Clone6, 2T42, and 2T68 were transfected with 300 nM siRNA (as described in Materials and methods). Control cells and cells mock-transfected with TransFast reagent alone were treated under identical conditions. Cells were lysed 72 h after transfection
Tiam1 requirement for cellular migration
To further characterize the role of Tiam1 in migration, we performed a wound healing assay, as described in Materials and methods. Briefly, 72 h after control or siRNA transfection, confluent monolayers of cells were wounded with a pipet tip (time 0), and photographed at designated intervals afterwards. Each condition was photographed in three separate fields, and one of three fields shown in Fig. 2a. The percent of wound closed by infiltration of migratory cells is shown in Fig. 2b. The control SW480 wounds are only 41% closed at 14 h, consistent with the low migratory potential of the parental cells. In contrast, the wounds for 2TClone68, which ectopically overexpresses Tiam1 (Fig. 1b) are 80% closed. The siRNA to Tiam1 reduced the migration of 2TClone68 to control SW480 levels (80% closed to 43% closed), demonstrating that expression of the Tiam1 construct in these cells was solely responsible for the altered migration ability. siRNA expression in parental SW480 cells had a modest effect on migration (34% of the wounds were closed compared to 41% for parental cells), further suggesting that Tiam1 expression regulates migration of colorectal carcinoma cells.
Tiam1 requirement for cellular migration. (a) A wound-healing migration assay on SW480 and 2TClone68. Seventy-two hours after control or Tiam1 siRNA transfection, confluent monolayers of cells were wounded with a pipet tip (time 0), and photographed at indicated times thereafter. Each condition was photographed in three separate fields (one of three fields shown in the figure), and the same field at each time point was used to quantitate percent of wound closed. (b) The percent of wound closed is plotted versus time after wounding as described in Materials and methods. Control conditions are represented by solid lines, and Tiam1 siRNA-treated cells are represented by dashed lines; error bars represent the standard error of the mean (SEM)
Cellular morphology, detachment, and viability
Tiam1-overexpressing clones produce more round cells that easily detach from the culture dishes, and, as determined by trypan blue staining, these floating cells are viable. These cells detach from the tissue culture plate and appear to reattach at a different location, and therefore were collected during passaging, as described in the Materials and methods. Photomicrographs were taken of SW480 and the Tiam1-transfected clones to illustrate cellular morphology. In Fig. 3a, light microscopic examination of the representative clone 2TClone68 illustrates the increase in round, floating cells with respect to SW480 cultures.
Effects of Tiam1 on cellular morphology, adhesion, and viability. (a) Photomicrographs under light microscopy at a power of 200× of SW480 and 2TClone68. (b) Viability of floating cells. Cultures were grown to approximately 80% confluency, media was changed, and number of viable floating cells was determined at indicated times thereafter, as described in Materials and methods. The number of viable floating cells per million attached at time 0 was plotted versus time after media change; error bars represent the standard deviation of the mean. The mean number of floating cells between the two cell lines were compared using a level of significance of α = 0.05 with a two-sided unpaired t-test. (c) Apoptosis in detached cells. SW480, 2TClone42, and 2TClone68 were placed in 15 ml conical tubes on a rotator in a cell culture incubator, as described in Materials and methods. Percent apoptosis, represented by the population of cells in the sub G0/G1 fraction, is plotted versus time; error bars represent the standard deviation of the mean. The mean death of two cell lines were compared using a level of significance of α = 0.05 with a two-sided unpaired t-test
To quantitate the floating cells in culture, an equivalent number of SW480 and 2TClone68 cells were plated in 6-well dishes. At indicated time points, media with floating cells were collected and the number of viable (by trypan blue exclusion) floating cells per million adherent cells at time 0 was calculated. Results are shown in Fig. 3b. The number of floating cells increased with time for all cell lines. However, detachment of viable cells is significantly (P < 0.05) increased in 2TClone68 cells relative to parental cells at both 48 h and 60 h after the media change (1 × 106 cells for 2TClone68 compared to 4.3 × 105 cells for SW480 after 60 h). Therefore, overexpression of Tiam1 decreases cell adhesion.
To determine the viability of cells after prolonged detachment, cells were placed in rotating conical tubes, and apoptosis was measured by staining the cells with propidium iodide and measuring the sub G0/G1 population with a flow cytometer at indicated times after detachment. As shown in Fig. 3c, the percentage of apoptotic cells increased over time in all cell lines examined, with 45% of the parental SW480 cells apoptotic at 120 h. In contrast, Tiam1-transfected cell cultures 2TClone42 and 2TClone68 contain significantly (P < 0.05) fewer apoptotic cells (25–29%) at 120 h. Thus, overexpression of Tiam1 confers anoikis-resistance in colon carcinoma cells.
Tiam1 protects cells from anoikis
To confirm the above results, the effects on anoikis of reducing Tiam1 expression were determined. Apoptosis was first measured in attached cells after transfection with siRNA. Cells were transfected with 300 nM of a single oligonucleotide of siRNA to Tiam1. Media and cells were collected 72 h later, and apoptosis was measured; the results are shown in Fig. 4a. Under control conditions, adherent 2TClone68 cells had a similar apoptotic population to that of parental SW480. Addition of the TransFast transfection reagent alone or in combination with the siRNA had little effect on cell death on adherent cells in all cell lines; apoptotic populations ranged from 4 to 6.5% for all cell lines and conditions. These results demonstrate that decreased Tiam1 expression does not affect apoptosis in attached cells.
Effect of Tiam1 expression on anoikis. (a) Apoptosis in attached cells. Cells were transfected with 300 nM of a siRNA oligonucleotide to Tiam1. Media and cells were collected 72 h later, and apoptosis was measured. Percent apoptosis, represented by the population of cells in the sub G0/G1 fraction, is shown for control, mock, and siRNA transfection for SW480 and 2T68; error bars represent the standard deviation of the mean. (b) Apoptosis in detached cells. SW480 and 2TClone68 were plated and transfected as described above. Twenty-four hours later, cells were trypsinized and plated in agarose-covered dishes, as described in Materials and methods. Percent apoptosis is represented by the population of cells in the sub G0/G1 fraction and is shown for 48 and 72 h of anoikis; error bars represent the standard deviation of the mean. The mean death of two cell lines were compared using a level of significance of α = 0.05 with a two-sided unpaired t-test. (c) Expression of Tiam1 after 72 h detachment. At the conclusion of the anoikis assay, cells were lysed and whole-cell lysate immunoblotted with Tiam1 and vinculin as a loading control
The effect of reduced Tiam1 expression was then determined on detached cells. For these experiments, cells were plated on tissue-culture dishes, and 24 h later, transfected with 300 nM siRNA to Tiam1. Twenty-four hours after transfection, cells were trypsinized and placed in 4% agarose-covered dishes to prevent attachment. Forty-eight or 72 h later (72 or 96 h post-transfection), cells were assayed for apoptosis. As shown in Fig. 4b, after 72 h, under control conditions, 27% of SW480 cells were apoptotic, while just 13% of 2TClone68 were apoptotic. These results are in accord with those obtained in rotating conical tubes (Fig. 3c). siRNA to Tiam1 increased anoikis in SW480 and 2TClone68 by a significant (P < 0.05) amount, compared to either control or mock transfection. Thirty-seven percent of SW480 cells treated with siRNA to Tiam1 were apoptotic after 72 h in suspension cultures, an increase from 27% under control conditions, and anoikis in 2TClone68 transfected with siRNA to Tiam1 increased from 13 to 26%. As shown in Fig. 4c, at the conclusion of the assay, Tiam1 protein continues to be downregulated with the siRNA, demonstrating the siRNA has maintained its effectiveness at the times studied. These results demonstrate that Tiam1 protects colon cancer cells from detachment-induced death.
Requirement for Rac in migration
We showed previously that GTP-bound Rac and Rho are increased in the biologically selected and Tiam1-transfected cells [4]. To determine the contribution of Rac to cellular migration in our model system, we downregulated Rac1 protein expression with siRNA. As shown in Fig. 5a, 300 nM of one siRNA oligonucleotide decreases Rac expression in SW480 and 2TClone68 greater than 90%. Transfection with multiple oligonucleotides was not superior to transfection with a single oligonucleotide (data not shown), therefore, we used a single oligonucleotide for these experiments. Migration was assessed by the wound healing assay. The photographs of the wounds (one of the three observations) are shown in Fig. 5b and quantitated in Fig. 5c. Under control conditions, the wounds for SW480 are 46% closed after 14 h, while the wounds for 2TClone68 are 87% closed. When the cells were treated with siRNA to Rac1, the migratory ability of SW480 is largely unaffected. However, migration of 2TClone68 returns to SW480 control levels with siRNA to Rac1, from 87% of the wounds closed to only 43% closed. These results demonstrate that downregulation of Rac1 is equivalent to downregulation of Tiam1 in affecting migration, strongly suggesting that Tiam1 exerts its effects on migration through Rac1.
Requirement for Rac in Tiam1-mediated phenotypes. (a) Rac expression after downregulation with an siRNA oligonucleotide. SW480 and 2TClone68 were treated with transfection reagent alone (mock) or 300 nM of an oligonucleotide siRNA to Rac1. Whole-cell lysate was immunoblotted with Rac1 and vinculin as a loading control. (b) Effects of Rac downregulation on migration. A wound-healing migration assay was performed for the cell lines SW480 and 2TClone68 with and without Rac downregulation. Wound healing assays were performed as described in Fig. 2. (c) Plot of wound healing. Control conditions are illustrated with solid lines, and Rac1 siRNA-treated cells are illustrated with dashed lines; error bars represent the SEM. (d) Effect of Rac downregulation on anoikis. SW480 and 2TClone68 were treated with transfection reagent alone (mock) or 300 nM siRNA to Rac1. Anoikis assays were performed as described in Fig. 3. The mean death of two cell lines were compared using a level of significance of α = 0.05 with a two-sided unpaired t-test. (e) At the conclusion of the anoikis assay, cells were lysed and whole-cell lysate immunoblotted with Rac and vinculin as a loading control. (f) Effect of Rac on staurosporine-induced death. SW480 and 2TClone68 cells were treated with staurosporine in the presence or absence of siRNA to Rac. Error bars represent the standard deviation of the mean
Tiam1-regulated sensitivity to anoikis is Rac-Independent
We next determined Rac1’s requirement for the migratory cells’ resistance to anoikis. For these experiments, Rac expression was reduced with siRNA as described above. As with the experiments with siRNA to Tiam1, apoptosis was first measured in attached cells after transfection with siRNA. No differences in the number of apoptotic cells were observed between control cells and cells in which Rac was downregulated (data not shown). The effect of reduced Rac1 expression was then determined on cells under detached conditions (agarose-covered dishes), as described above for siRNA to Tiam1. Cells were assayed for apoptosis after 96 h of detachment. As shown in Fig. 5d, decreasing Rac protein expression significantly (P < 0.05) decreases death due to detachment in SW480 (30% anoikis to 19%), but has no effect on anoikis in 2TClone68. These results, in combination with the results from decreasing Tiam1 protein expression, demonstrate that the effects of Tiam1 on anoikis are Rac-independent. At the conclusion of the assay, Rac1 protein continues to be downregulated with the siRNA (Fig. 5e), demonstrating that the results are not due to re-expression of the protein over the time period assayed. Lastly, the function of Rac in apoptosis induced by another agent was tested. SW480 parental cells and Tiam1-transfected clone 2TClone68 were exposed to varying concentrations of staurosporine, with or without siRNA to Rac. As shown in Fig. 5f, apoptosis in the control cell line SW480 and 2TClone68 increases with increasing dose of staurosporine, and the Tiam1-transfected cells are less sensitive to staurosporine-induced death when compared to SW480 cells. Downregulating Rac protein with siRNA to Rac had little effect on cell death in Tiam1-transfected cells, indicating that cell death in response to staurosporine is Rac-independent in these cells. At the conclusion of the assay, Rac1 protein continues to be downregulated with the siRNA (data not shown), demonstrating that the results are not due to re-expression of the protein over the time period assayed. Thus, Tiam1 functions in a Rac-independent manner in affecting apoptosis.
Increased Tiam1 promotes an EMT-like phenotype
We have demonstrated thus far that multiple characteristics of increased cellular migration, increased metastatic growth, decreased adhesion, and increased resistance to anoikis are associated with increased Tiam1 protein expression. Many of the above-described morphologic properties are characteristic of a transition of transformed epithelial cells to a mesenchymal-like phenotype. Biochemical properties associated with an epithelial mesenchymal-like transition (EMT) include, among others, increased expression of the mesenchymal marker vimentin and decreased expression of the epithelial protein E-cadherin. EMT occurs at critical phases of embryonic development, and increasing evidence suggests that EMT-like transitions occur during tumor progression (reviewed in [24–26]). Therefore, we examined biochemical properties of EMT in parental SW480 cells, mmig3 Clone1 (which was biologically selected for increased migration and overexpresses endogenous Tiam1), and 2TClone68 (which ectopically overexpresses Tiam1). As shown in Fig. 6a, by immunoblotting, vimentin is increased in all cells overexpressing Tiam1 relative to SW480 parental cells, whereas a marked decreased expression of E-cadherin protein is observed. Localization of vimentin and E-cadherin was determined by immunofluorescence. As shown in Fig. 6b, vimentin is expressed in the cytoplasm and nucleus of all three cell lines, with the most prominent localization in the perinuclear area of the cell. In accord with results from immunoblotting (Fig. 6a), vimentin expression is increased in the Tiam1-overexpressing cells. As shown in Fig. 6c, E-cadherin protein is expressed at cellular junctions in the cell line SW480, and the expression at the cellular junctions and in the cytoplasm is decreased in the more migratory, more metastatic cell lines that also overexpress Tiam1. Lastly, cells were stained for β-catenin, as translocation of β-catenin from the cytoplasm and cell membrane to the nucleus is associated with EMT [27, 28]. As shown in Fig. 6d, β-catenin protein exhibits decreased expression at the cell periphery and cytoplasm in the cells that overexpress Tiam1.
Effects of Tiam1 on promotion of an EMT-like phenotype. (a) Expression of vimentin and E-cadherin. Immunoblotting was performed on SW480, SW480 mmig3 Clone1, SW480 mmig3 Clone6, 2TClone42 and 2TClone68, with vinculin or actin as a loading control. Protein localization for the EMT markers (b) E-cadherin, (c) vimentin, and (d) β-catenin is illustrated. Cells were grown on glass coverslips and immunofluorescence was performed as described in Materials and methods
Tiam1 expression in human tumors
The above results demonstrate that Tiam1 overexpression contributes to distinct properties of colon carcinoma progression and metastasis in cultured tumor cells. To determine Tiam1 expression in tissue from primary human colorectal carcinoma, eleven human colorectal carcinoma specimens ranging in location of origin within the colon and rectum, along with patient-matched normal colorectal tissue, were stained for Tiam1 protein. Table 1 illustrates patient and tumor characteristics at the time of specimen collection, though a direct correlation between tumor stage and fluorescence was not observed. Immunoreactive proteins were visualized by fluorescent-tagged secondary antibodies, and fluorescence was quantitated utilizing Image Pro Plus software. As shown in the representative images in Fig. 7, 64% of the tumor samples are increased in Tiam1 expression in the tumor tissue compared to patient-matched normal tissue. These findings agree with the very recent results of others [29] that have demonstrated that Tiam1 mRNA was overexpressed in the peripheral blood of 80% of colorectal carcinoma patients. Our results, along with those from others, show that in a subset of human colorectal carcinoma, Tiam1 is overexpressed.
Tiam1 Expression in Human Tumors. Primary antibody was visualized by incubation with a cy5-conjugated secondary antisera, and hematoxylin and eosin (H and E) staining is also shown for each section. Tiam1 is colored green, and the nuclei are colored blue. Five pairs of tumor and pathologically normal adjacent tissue are represented in the figure
Discussion
Isogenic cell lines have proven excellent model systems to examine specific molecular events mediating biologic processes. For example, the human colon cancer cell line HCT116 [30] with and without activated Ras has proven a valuable tool in dissecting Ras-mediated signaling functions relevant to colon tumorigenesis and progression. The model derived for the work in this study involved selecting cells with increased migratory potential and then examining the effects on properties of the metastatic process. This model led to the demonstration that the guanine nucleotide exchange factor Tiam1 contributes to colorectal carcinoma cell migration and metastasis [4]. In agreement with this study, Liu et al. [20] demonstrated that in eight colorectal carcinoma cell lines, the level of Tiam1 expression correlated with metastatic potential. Included in their study were the cell lines SW480 and SW620, a lymph node metastasis derived from the same patient as was the cell line SW480 [21]. They demonstrate that SW620 has increased Tiam1 expression relative to SW480 [20]. We have also demonstrated (unpublished results) that a second, well-established model for colorectal carcinoma metastasis, the KM12 series, shows higher Tiam1 expression in two cell lines (KM12SM and KM12L4) that are more migratory and more metastatic than the parental KM12C cell line. Both KM12SM and KM12L4 are increased in cellular migration relative to their parental line, but were selected for, and are increased in, in vivo metastasis [31], and have increased Tiam1 protein and mRNA expression when compared to their parental line, KM12C. These results further suggest that Tiam1 contributes to increased migration in other colon tumor cell lines, and tumor progression and metastasis. Further, in the current study, specimens of human tissue were examined for Tiam1 expression, and we demonstrated that Tiam1 is overexpressed in a subset of human colorectal tumors. These results indicate that Tiam1 may play a role in human colorectal carcinoma progression. Others [32] have demonstrated that APC mutant multiple intestinal neoplasia (Min) mice lacking Tiam1 have reduced incidence and growth of colon polyps. Very recently, Yeh et al. [33] have reported that Tiam1 is part of a 6-member panel of mRNA markers in peripheral blood that can be utilized to successfully detect stage 1 and stage 2 colorectal carcinomas. The authors found that Tiam1 mRNA was overexpressed in the peripheral blood of 80% of colorectal carcinoma patients. Collectively, our results in combination with those of others suggest strongly that overexpression of Tiam1 may be one of the multiple mechanisms that contribute to colon tumor progression/metastasis.
The primary goal of the current study was to characterize Tiam1-mediated functions that contribute to its ability to increase metastatic potential. We previously described the role of Tiam1 in increasing migration. However, overexpression of Tiam1 (by biologic selection or stable transfection) substantially increases the number of viable, floating cells, demonstrating that Tiam1 also affects cellular adhesion. As cellular migration and cellular adhesion are intimately related, changes in one may be expected to result in changes in the other.
Markedly, the floating cells were of high viability, and their resistance was regulated by Tiam1 expression, as siRNA reduction of Tiam1 increased anoikis, indicating that Tiam1 protects colorectal carcinoma cells from detachment-induced death. In contrast to migration, the effects of Tiam1 on anoikis were not reversed by decreasing Rac expression by siRNA, suggesting that promotion of anoikis-resistance by Tiam1 is Rac-independent. These results demonstrate that Tiam1 affects biologic properties through mechanisms not related to its GEF activity, perhaps through association with additional signaling proteins as predicted by its many protein interaction domains. Despite the reduced Rac expression in Rac siRNA-treated cells, all cell lines were able to adhere to tissue culture plates, as well as migrate. Possibly, the marginal Rac protein remaining was sufficient for these properties to occur. In addition, SW480 cells contain an activating K-Ras mutation, suggesting that downstream targets may be compensating for the reduced Rac.
Finally, in an effort to determine a unifying characteristic of Tiam1 overexpression in colon tumor cells, we noted that many of the phenotypes associated with Tiam1 overexpression are characteristic of transition to a more mesenchymal-like phenotype. We demonstrate that increased Tiam1 expression leads to biologic phenotypes of mesenchymal cells, including increased vimentin expression, decreased E-cadherin expression at the cell periphery but increased nuclear expression of this protein, and relocalization of β-catenin. One of the mechanisms by which inactivation of cadherin-mediated cell–cell adhesion occurs is through the small G proteins in the Rho family. Rac and Rho have been shown to have opposite roles in epithelial cells, with Rac promoting the inactivation of Rho and cellular adhesion [34]. Our results suggest another possibility, that Rac and Rho are both modestly activated simultaneously, which may explain the small increase in activity in both [4], and that Rac is promoting migration, and Rho is promoting loss of adhesion, as Rho is involved in cell contraction.
Recently, Robson, et al. [35] showed that in three mammary epithelial cell lines, EMT confers resistance to apoptosis. As resistance to apoptosis is key in tumor development and progression, these observations support our model that Tiam1-induced phenotypes are a result of its ability to promote a more mesenchymal-like phenotype. Further, increasing evidence supports a role for EMT in colon cancer progression (reviewed in 36).
The roles of Tiam1 in normal cellular function differ depending on the model systems examined. Studies from several laboratories have examined the role of Tiam1 in cellular migration. These studies have led to different conclusions based upon the types of cells analyzed and the substrate on which migration is examined. For example, several studies have demonstrated that Tiam1 promotes cellular adhesion or decreased migration [14, 37–40]. In contrast, other studies have demonstrated that overexpression of Tiam1 increases migration in several cell types [41–46]. Recent work [47] in keratinocytes has demonstrated that Tiam1 plays a primary role in α3β1-mediated activation of Rac, which is then required for the manufacture and secretion of laminin 5, essential for the spreading and migration of these cells. Additional recent work [9, 48] has demonstrated additional functions for Tiam1, and that Tiam1 can complement activation of other proto-oncogenes during tumor progression. Because Tiam1 localizes to adherens junctions, it may interact with multiple proteins that affect cellular migration [49]. Thus, considerable recent data have demonstrated that Tiam1 is important in properties associated with metastasis, in some tumor types. Specifically, our work and that of others in colon [4, 20, 32] and breast [18, 19] demonstrate a role for Tiam1 in tumor progression of distinct epithelial tumors. Work in this manuscript expands biologic roles for Tiam1, demonstrating that this GEF can have Rac-dependent and—independent functions. As with other alterations (for example, K-Ras in colon tumors), only a subpopulation of tumors overexpresses Tiam1. Whether this population represents more invasive cells requires further investigation. Nevertheless, Tiam1 may represent a novel marker of tumor progression and metastasis in a specific subset of human colorectal carcinomas.
References
Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, Thun MJ (2006) Cancer statistics, 2006. CA Cancer J Clin 56:106–130
Zaniboni A, Labianca R (2004) Adjuvant therapy for stage II colon cancer: an elephant in the living room? Ann Oncol 15:1310–1318
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335–2342
Minard ME, Herynk MH, Collard JG, Gallick GE (2005) The guanine nucleotide exchange factor Tiam1 increases colon carcinoma growth at metastatic sites in an orthotopic nude mouse model. Oncogene 24:2568–2573
Michiels F, Habets GG, Stam JC, van der Kammen RA, Collard JG (1995) A role for Rac in Tiam1-induced membrane ruffling and invasion. Nature 375:338–340
Haeusler LC, Blumenstein L, Stege P, Dvorsky R, Ahmadian MR (2003) Comparative functional analysis of the Rac GTPases. FEBS Lett 555:556–560
Habets GG, Scholtes EH, Zuydgeest D, van der Kammen RA, Stam JC, Berns A, Collard JG (1994) Identification of an invasion-inducing gene, Tiam-1, that encodes a protein with homology to GDP-GTP exchangers for Rho-like proteins. Cell 77:537–549
Rogers S, Wells R, Rechsteiner M (1986) Amino acid sequences common to rapidly degraded proteins: the PEST hypothesis. Science 234:364–368
Lambert JM, Lambert QT, Reuther GW, Malliri A, Siderovski DP, Sondek J, Collard JG, Der CJ (2002) Tiam1 mediates Ras activation of Rac by a PI(3)K-independent mechanism. Nat Cell Biol 4:621–625
van Leeuwen FN, van der Kammen RA, Habets GG, Collard JG (1995) Oncogenic activity of Tiam1 and Rac1 in NIH3T3 cells. Oncogene 11:2215–2221
Stam JC, Sander EE, Michiels F, van Leeuwen FN, Kain HE, van der Kammen RA, Collard JG (1997) Targeting of Tiam1 to the plasma membrane requires the cooperative function of the N-terminal pleckstrin homology domain and an adjacent protein interaction domain. J Biol Chem 272:28447–28454
Michiels F, Stam JC, Hordijk PL, van der Kammen RA, Ruuls-Van Stalle L, Feltkamp CA, Collard JG (1997) Regulated membrane localization of Tiam1, mediated by the NH2-terminal pleckstrin homology domain, is required for Rac-dependent membrane ruffling and C-Jun NH2-terminal kinase activation. J Cell Biol 137:387–398
Habets GG, van der Kammen RA, Stam JC, Michiels F, Collard JG (1995) Sequence of the human invasion-inducing TIAM1 gene, its conservation in evolution and its expression in tumor cell lines of different tissue origin. Oncogene 10:1371–1376
Engers R, Zwaka TP, Gohr L, Weber A, Gerharz CD, Gabbert HE (2000) Tiam1 mutations in human renal-cell carcinomas. Int J Cancer 88:369–376
Hou M, Tan L, Wang X, Zhu YS (2004) Antisense Tiam1 down-regulates the invasiveness of 95D cells in vitro. Acta Biochim Biophys Sin (Shanghai) 36:537–540
Malliri A, van der Kammen RA, Clark K, Van Der Valk M, Michiels F, Collard JG (2002) Mice deficient in the Rac activator Tiam1 are resistant to Ras-induced skin tumours. Nature 417:867–871
Otsuki Y, Tanaka M, Yoshii S, Kawazoe N, Nakaya K, Sugimura H (2001) Tumor metastasis suppressor nm23H1 regulates Rac1 GTPase by interaction with Tiam1. Proc Natl Acad Sci U S A 98:4385–4390
Adam L, Vadlamudi RK, McCrea P, Kumar R (2001) Tiam1 overexpression potentiates heregulin-induced lymphoid enhancer factor-1/beta -catenin nuclear signaling in breast cancer cells by modulating the intercellular stability. J Biol Chem 276:28443–28450
Minard ME, Kim LS, Price JE, Gallick GE (2004) The role of the guanine nucleotide exchange factor Tiam1 in cellular migration, invasion, adhesion and tumor progression. Breast Cancer Res Treat 84:21–32
Liu L, Wu DH, Ding YQ (2005) Tiam1 gene expression and its significance in colorectal carcinoma. World J Gastroenterol 11:705–707
Leibovitz A, Stinson JC, McCombs WB III, McCoy CE, Mazur KC, Mabry ND (1976) Classification of human colorectal adenocarcinoma cell lines. Cancer Res 36:4562–4569
Windham TC, Parikh NU, Siwak DR, Summy JM, McConkey DJ, Kraker AJ, Gallick GE (2002) Src activation regulates anoikis in human colon tumor cell lines. Oncogene 21:7797–7807
Ellis LM, Staley CA, Liu W, Fleming RY, Parikh NU, Bucana CD, Gallick GE (1998) Down-regulation of vascular endothelial growth factor in a human colon carcinoma cell line transfected with an antisense expression vector specific for c-src. J Biol Chem 273:1052–1057
Savagner P (2001) Leaving the neighborhood: molecular mechanisms involved during epithelial-mesenchymal transition. Bioessays 23:912–923
Thiery JP (2002) Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer 2:442–454
Thiery JP (2003) Epithelial-mesenchymal transitions in development and pathologies. Curr Opin Cell Biol 15:740–746
Brembeck FH, Schwarz-Romond T, Bakkers J, Wilhelm S, Hammerschmidt M, Birchmeier W (2004) Essential role of BCL9–2 in the switch between beta-catenin’s adhesive and transcriptional functions. Genes Dev 18:2225–2230
Morali OG, Delmas V, Moore R, Jeanney C, Thiery JP, Larue L (2001) IGF-II induces rapid beta-catenin relocation to the nucleus during epithelium to mesenchyme transition. Oncogene 20:4942–4950
Yeh CS, Wang JY, Wu CH, Chong IW, Chung FY, Wang YH, Yu YP, Lin SR (2006) Molecular detection of circulating cancer cells in the peripheral blood of patients with colorectal cancer by using membrane array with a multiple mRNA marker panel. Int J Oncol 28:411–420
Shirasawa S, Furuse M, Yokoyama N, Sasazuki T (1993) Altered growth of human colon cancer cell lines disrupted at activated Ki-ras. Science 260:85–88
Morikawa K, Walker SM, Nakajima M, Pathak S, Jessup JM, Fidler IJ (1988) Influence of organ environment on the growth, selection, and metastasis of human colon carcinoma cells in nude mice. Cancer Res 48:6863–6871
Malliri A, Rygiel TP, van der Kammen RA, Song JY, Engers R, Hurlstone AF, Clevers H, Collard JG (2005) The RAC activator Tiam1 is a Wnt-responsive gene that modifies intestinal tumour development. J Biol Chem, epub Oct 05, Printed 2006, 281: 543–548
Yeh CS, Wang JY, Wu CH, Chong IW, Chung FY, Wang YH, Yu YP, Lin SR (2006) Molecular detection of circulating cancer cells in the peripheral blood of patients with colorectal cancer by using membrane array with a multiple mRNA marker panel. Int J Oncol 28:411–420
Evers EE, Zondag GC, Malliri A, Price LS, ten Klooster JP, van der Kammen RA, Collard JG (2000) Rho family proteins in cell adhesion and cell migration. Eur J Cancer 36:1269–1274
Robson EJ, Khaled WT, Abell K, Watson CJ (2006) Epithelial-to-mesenchymal transition confers resistance to apoptosis in three murine mammary epithelial cell lines. Differentiation 74:254–264
Bates RC, Mercurio AM (2005) The epithelial-mesenchymal transition (EMT) and colorectal cancer progression. Cancer Biol Ther 4:365–370
Engers R, Springer E, Michiels F, Collard JG, Gabbert HE (2001) Rac affects invasion of human renal cell carcinomas by upregulating TIMP-1 and TIMP-2 expression. J Biol Chem 276:41889–41897
Hordijk PL, ten Klooster JP, van der Kammen RA, Michiels F, Oomen LC, Collard JG (1997) Inhibition of invasion of epithelial cells by Tiam1-Rac signaling. Science 278:1464–1466
Sander EE, ten Klooster JP, van Delft S, van der Kammen RA, Collard JG (1999) Rac downregulates Rho activity: reciprocal balance between both GTPases determines cellular morphology and migratory behavior. J Cell Biol 147:1009–1022
Uhlenbrock K, Eberth A, Herbrand U, Daryab N, Stege P, Meier F, Friedl P, Collard JG, Ahmadian MR (2004) The RacGEF Tiam1 inhibits migration and invasion of metastatic melanoma via a novel adhesive mechanism. J Cell Sci 117:4863–4871
Bourguignon LY, Zhu H, Shao L, Chen YW (2000) CD44 interaction with tiam1 promotes Rac1 signaling and hyaluronic acid-mediated breast tumor cell migration. J Biol Chem 275:1829–1838
Bourguignon LY, Zhu H, Shao L, Chen YW (2000) Ankyrin-Tiam1 interaction promotes Rac1 signaling and metastatic breast tumor cell invasion and migration. J Cell Biol 150:177–191
Ehler E, van Leeuwen F, Collard JG, Salinas PC (1997) Expression of Tiam-1 in the developing brain suggests a role for the Tiam-1-Rac signaling pathway in cell migration and neurite outgrowth. Mol Cell Neurosci 9:1–12
Fleming IN, Gray A, Downes CP (2000) Regulation of the Rac1-specific exchange factor Tiam1 involves both phosphoinositide 3-kinase-dependent and -independent components. Biochem J 351:173–182
van Leeuwen FN, Kain HE, Kammen RA, Michiels F, Kranenburg OW, Collard JG (1997) The guanine nucleotide exchange factor Tiam1 affects neuronal morphology; opposing roles for the small GTPases Rac and Rho. J Cell Biol 139:797–807
Supriatno, Harada K, Kawaguchi S, Yoshida H, Sato M (2003) Effect of p27Kip1 on the ability of invasion and metastasis of an oral cancer cell line. Oncol Rep 10:527–532
Hamelers IH, Olivo C, Mertens AE, Pegtel DM, van der Kammen RA, Sonnenberg A, Collard JG (2005) The Rac activator Tiam1 is required for (alpha)3(beta)1-mediated laminin-5 deposition, cell spreading, and cell migration. J Cell Biol 171:871–881
Servitja JM, Marinissen MJ, Sodhi A, Bustelo XR, Gutkind JS (2003) Rac1 function is required for Src-induced transformation: evidence of a role for Tiam1 and Vav2 in Rac activation by Src. J Biol Chem 278:34339–34346
Strumane K, Rygiel TP, Collard JG (2005) The rac activator tiam1 and ras-induced oncogenesis. Methods Enzymol 407:269–281
Acknowledgements
We thank Nila U. Parikh for excellent technical assistance. This work was supported by the Rosalie B. Hite Fellowship and the Andrew Sowell-Wade Huggins Scholarship to MEM. MEM was the T.C. Hsu Memorial Scholar in Cell Biology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Minard, M.E., Ellis, L.M. & Gallick, G.E. Tiam1 regulates cell adhesion, migration and apoptosis in colon tumor cells. Clin Exp Metastasis 23, 301–313 (2006). https://doi.org/10.1007/s10585-006-9040-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-006-9040-z