Abstract
Drought is a devastating natural hazard that significantly affects human health and social and economic activities. This study aims to explore the short-term association between drought and outpatient visits for respiratory diseases (RDs) in four northwest cities, China. In this study, we obtained daily outpatient visits for RDs, meteorological factors, and air pollutant data in four cities (Lanzhou from 2014 to 2016, Wuwei from 2016 to 2018, Tianshui and Zhangye from 2015 to 2018) of northwest China. We used the daily Standardized Precipitation Index (SPI) as an indicator of drought and estimated the effects of drought on outpatient visits with RDs by using a generalized additive model (GAM) in each city, controlling for daily temperature, time trends, and other confounding factors. The city-specific estimates were pooled by random-effects meta-analysis. There were 1,134,577 RDs cases in the hospitals across the four cities. We found that a 1-unit decrease in daily exposure to SPI-1 was positively associated with daily outpatient visits for RDs, with estimated RR of 1.0230 (95% CIs: 1.0096, 1.0366). Compared to non-drought periods, the RR of daily outpatient visits for RDs for exposure to all drought conditions was 1.0431 (95% CIs: 1.0309, 1.0555). In subgroup analysis, the estimated effects of drought on outpatient visits for RDs appeared larger for males than females though not statistically different, and the estimated effects in children and adolescents were the greatest among different age groups. Drought likely increases the risk of respiratory diseases, particularly among children and adolescents. We highlight that public health adaptations to drought such as drought monitoring, mitigation measures, and adaptation strategies are necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
A changing climate has been considered one of the major health threats globally in the twenty-first century (Watts et al. 2018a; 2018b), including more frequently occurring heat waves, hurricanes, and droughts (Franchini and Mannucci 2015; Schwalm et al. 2017). The 2020 report of the Lancet Countdown showed that the global land surface area affected by excess drought was more than twice that of a historical baseline, and drought poses multiple risks for health (Watts et al. 2020). Droughts were reported to have killed more lives than all the other natural hazards combined over the past century (Maskey and Trambauer 2015). Long-term drought would lead to the deterioration of the ecological environment (Allen et al. 2010; Wu et al. 2018) and cause many other tangible and intangible damages. A study in China suggested that the annual economic losses caused by droughts may reach several tens of billions of US dollars in China with increasing drought intensity and areal coverage across China (Su et al. 2018). Schwalm et al. (2017) reported that global droughts would occur more frequently in the future, and researchers predicted that the ecosystems in some places would encounter another drought before they recover from one, which may cause permanent ecological damage. According to Zhang et al. (2019), since the year 2000, at least 79 global big cities have already suffered from urban drought disaster more than once. They found that urban drought occurred not only in arid or semi-arid regions but also in semi-humid and even in humid regions. So droughts may become a new normal in the twenty-first century.
Therefore, it is critical to explore the effects of droughts on human health at this urgent moment because droughts will become a common challenge in many populations. However, until now, few studies have reported the effects of drought on health (Berman et al. 2017; Ebi and Bowen 2016; Salvador et al. 2019). Drought may damage ecosystems, thereby reducing the food supplies, and then reduce quantity and/or quality of nutrient intake, which leads to greater vulnerability to illness and increases mortality risk (Ebi and Bowen 2016; Stanke et al. 2013). Drought can cause a shortage of drinking water and/or a decline in drinking water quality, exposing many people to potentially contaminated water, and promote the risk of waterborne diseases Yusa and Berry (2015). For example, there was an epidemic of cholera in northern Kenya following a severe drought (Shuman 2010). Some studies have shown that economic stress caused by droughts may harm mental health (Barreau et al. 2017; Lv et al. 2014; Stain et al. 1982).
In addition, dusty and wildfires that often accompany drought could harm health (Franchini and Mannucci 2015), particularly by increasing the concentrations of particulate matter in the air (Yusa and Berry 2015). Exposure to these elements was responsible for large respiratory morbidity (Barnes 2018; Reid et al. 2016). Machado-Silva et al. (2020) found that drought exacerbated the incidence of respiratory diseases (RDs) in the Amazon. Berman et al. (2017) estimated the risk of drought on daily hospital admissions for cardiovascular and respiratory and daily deaths among adults 65 years or older in the western USA. A recent study from Spain showed a statistically significant relationship between daily natural-cause mortality, daily respiratory-cause mortality, and drought (Salvador et al. 2020). However, no study has reported the effects of drought on respiratory diseases in China.
In this study, we proposed to evaluate the short-term association between drought and outpatient visits for respiratory diseases in an arid area of China-Gansu province (Wang et al. 2015). To define the level of drought, the Standardized Precipitation Index (SPI) was applied; the index has been used to estimate the effects of drought on daily mortality (Salvador et al. 2019; 2020). We conducted a time-series study to evaluate the effects of droughts on daily outpatient visits for respiratory diseases with SPI.
2 Material and methods
2.1 Study area and data collection
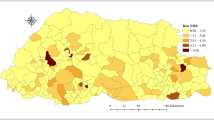
We conducted a retrospective ecological study of daily time series to evaluate the short-term impact of droughts on daily outpatient visits for respiratory diseases in four northwest cities of China (Fig. S1), which included Tianshui, Lanzhou, Wuwei, and Zhangye. These cities mostly covered by semi-arid to arid land, alternatively influenced by subtropical monsoon climate and temperate continental climate (Wang et al. 2015), and the mean annual precipitation was less than 400 mm (Xu et al. 2015). According to the provincial population data reported by the Gansu Provincial Bureau of Statistics in 2016 (http://tjj.gansu.gov.cn/), the populations of Tianshui, Lanzhou, Wuwei, and Zhangye were over 3.32 million, 3.70 million, 1.81 million, and 1.22 million, respectively.
In this study, we chose the central urban districts of four cities as the study area (Fig. S2). The Tianshui city includes two central urban districts (Qinzhou and Maiji), Lanzhou city includes four central urban districts (Chengguan, Qilihe, Xigu, and Anning). The Wuwei city and Zhangye city include one central urban district; they are Liangzhou and Ganzhou, respectively. Daily data on outpatient visits for RDs between Jan 01, 2014, and Dec 31, 2016, were collected from 11 large general hospitals of Lanzhou. In Tianshui city, Wuwei city, and Zhangye city, the daily outpatient visit data of RDs were collected from their biggest hospitals, which were the First Hospital of Tianshui City, Tumor Hospital of Wuwei City, and People’s Hospital of Zhangye City, respectively. Due to the availability of outpatient visit data, the studying periods for the First Hospital of Tianshui City, Tumor Hospital of Wuwei City, and People’s Hospital of Zhangye City were Jan 01, 2015, to Dec 31, 2018, Jan 01, 2016, to Dec 31, 2018, and Jan 01, 2015, to Dec 31, 2018, respectively. Outpatient visit data were coded using the 10th Revision of the International Classification of Diseases (ICD-10) Code of respiratory diseases (J00-J99), which excluded the postprocedural respiratory disorders (J95). All data on outpatient visits for respiratory diseases were obtained from hospitals, which were confirmed and permitted by the hospitals and related health departments.
For each city, we chose the weather monitoring stations and air quality monitoring stations closest to the hospitals (Fig. S2). Meteorological factors (daily temperature and precipitation data) of Tianshui, Wuwei, and Zhangye were collected from the meteorological data web page of the National Greenhouse Data Sharing Platform (http://data.sheshiyuanyi.com/WeatherData/). As the data of the meteorological station in Lanzhou was not online for public access, we obtained the daily meteorological data of Lanzhou from the Shanghai Meteorological Bureau. Each city has a meteorological monitoring station. The daily mean air pollutant data were obtained from the Data Center for the Ministry of Ecology and Environment of the People’s Republic of China (http://datacenter.mee.gov.cn/), including particulate matter with aerodynamic diameter ≤2.5 μm (PM2.5), nitrogen dioxide (NO2), and ozone (O3). There were four air quality monitoring stations in Lanzhou, three in Tianshui, and two in both Wuwei and Zhangye. We used the average of all air quality monitoring points in each city to represent the average concentration of pollutants in each city. The locations of meteorological monitoring stations and air quality monitoring stations of four study cities are shown in Fig. S2.
2.2 Drought index
We used the Standardized Precipitation Index (SPI) to measure the drought conditions. The SPI was designed to quantify the precipitation deficit for multiple timescales. It could be calculated at various timescales (1, 3, 6, 9, 12, 36, and 48 months) that reflect the impact of drought on the availability of the different water resources. The different timescales correspond to different accumulation periods, which are associated with different drought types. For example, SPI obtained at 1 month of accumulation (SPI-1) for meteorological drought, 1 to 6 months for agricultural drought, and 6 up to 24 months or longer for hydrological drought (Salvador et al. 2019). The SPI of all timescales can be created in weekly or monthly time steps. In this study, we calculated the weekly SPI-1 to assess the short-term effects of droughts on outpatient visits for RDs. To obtain better control of acute daily confounding factors (including air pollution and weather), we assumed the same condition for each 7-day interval following the approach in Berman et al. (2017) and Salvador et al. (2019 and 2020). The SPI-1 was calculated by the latest SPI program (SPI Generator v 1.7.5), which can be downloaded for free (see http://drought.unl.edu/droughtmonitoring/SPI/SPIProgram.aspx for more details). The SPI calculated in this program is based on representing the historical precipitation record with a gamma distribution. The Standardized Precipitation Index User Guide introduced that the calculation of SPI requires at least 30 years of monthly/weekly precipitation data in order to have some confidence in the statistics (World Meteorological Organization, 2012). Therefore, we collected 30 years of continuous daily precipitation data to create weekly SPI-1 data. The missing values of daily precipitation data in all four cities were less than 10%, and there were more missing values in the first 15 years, which could be handled by the SPI program. According to the national standard of Grades of Meteorological Drought (GB/T 20481-2017) of the People’s Republic of China (National Standardization Management Committee of China, 2017) and previous study (Li et al. 2021), a drought event occurs when the SPI-1 is equal or below −0.5 and ends when the SPI-1 greater than −0.5. And the severity of drought periods can be classified into 4 grades by the SPI-1 value: (1) SPI-1 between −1.0 and −0.5 is considered “light drought”; (2) SPI-1 between −1.5 and −1.0 is considered “moderate drought”; (3) SPI-1 between −2.0 and −1.5 is considered “severe drought”; and (4) the SPI-1 lower than −2.0 is considered “very severe drought.”
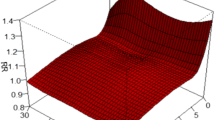
2.3 Statistical methods
We conducted a two-stage analysis to estimate the effects of drought on daily outpatient visits for RDs. In the first stage, we fitted a generalized additive model (GAM) with quasi-Poisson regression to estimate the short-term associations between drought and the outpatient visits with RDs in each city. The quasi-Poisson distribution was applied to overcome the overdispersion of outpatient visit data of RDs. Based on the previous study (Berman et al. 2017), the natural cubic spline smooth function was used to adjust for long-term time trends and meteorological factors. Although air pollutants may increase the risk of RDs, the air pollution was not adjusted in the model due to the strong correlation between air pollutants and temperature (Table S1-S4), so as to assess the total effects of drought. But in the sensitivity analysis, we provided the results after adjusting the PM2.5, O3, and NO2, respectively. The GAM equation is as follows:
where t is the day of the observation, E(Yt) is the expected number of daily outpatient visits for RDs on day t, α is the intercept, β and λ are the regression coefficients, time is the days of calendar time on day t, SPI-1t is the daily SPI-1 on day t, and ns() denotes the natural cubic spline smooth function. Based on previous studies (Berman et al. 2017; Wang et al. 2018a), the 7 degrees of freedom (df) per year is used to adjust for time trends and 6 df for 3-day moving average ambient temperature (AT) to control potential nonlinear effects of temperature. Dow is a categorical variable for day of week to account for possible variations of morbidity in a week, and holiday is a binary variable (0 indicates no holiday and 1 indicates a holiday) for national holidays in China.
After the establishment of the above model, we divided SPI-1 into a binary variable by the Grades of Meteorological Drought (GB/T 20481-2017) (0 for the non-drought periods and 1 for the drought periods) to estimate the effects of all drought conditions on the outpatient visits with RDs compared with the non-drought period. Moreover, we considered drought severity when assessing health risks (Berman et al. 2017). We further separated SPI-1 into five categorical variables (0 for the non-drought periods, 1 for the light drought periods, 2 for the moderate drought periods, 3 for the severe drought periods, and 4 for very severe drought periods) to estimate the effects of light, moderate, severe, and very severe drought periods compared to non-drought periods.
In the second stage, the random-effects meta-analysis was used to pool the city-specific effects.
2.4 Subgroup and sensitivity analysis
The subgroup analyses were defined by gender (male and female) and age (children and adolescents, 0~18 years old; adults, 19~64 years old; and elders, ≥65 years old) only in Tianshui, due to unavailability of age and gender data in Lanzhou, Wuwei, and Zhangye. We used Z-test to test the statistical significance of the differences between subgroups following the formula  , where β1 and β2 are the effect estimates for the subgroups and SE1 and SE2 are their respective standard errors (Altman and Bland 2003).
, where β1 and β2 are the effect estimates for the subgroups and SE1 and SE2 are their respective standard errors (Altman and Bland 2003).
We conducted a sensitivity analysis by changing the threshold of drought defined by SPI-1: (1) the onset of drought is defined when the SPI-1 value falls below 0 (Salvador et al. 2019; Salvador et al. 2020). (2) A drought event is defined when the SPI-1 falls below −1.0 (World Meteorological Organization, 2012). Considering acute and delayed effects of air pollutants on outpatient visits for RDs (Shahi et al. 2014; Wang et al. 2018b), we used 2-day moving average of current-day and previous-day concentrations of PM2.5, NO2, and O3 (lag 01) separately controlled in the models. Besides, we also changed the df from 6 to 9 per year for calendar time and from 3 to 7 for temperature and changed the moving average days of temperature (lag 07, lag 014, lag 021) in models.
All analyses were conducted using R software (version 4.0.3) with the GAM fitted by the “mgcv” package (version 1.8-33). And the meta-analysis was based on the “meta” package (version 4.15-1). All statistical tests were two-sided, and P-values less than 0.05 were considered statistically significant. The effects of SPI-1 were denoted as the relative risks (RR) and their 95% confidence intervals (CIs) in daily outpatient visits for RDs associated with per 1-unit (1 unit is equal to 1) decrease in SPI-1. And the effects of all drought conditions, light, moderate, severe, and very severe drought periods were denoted as RR and their 95% CIs of daily outpatient visits for RDs compared to the non-drought periods
3 Results
3.1 Description of the general situation
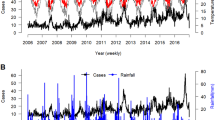
There were 647,855 RDs outpatient visits during Jan 1, 2014, through Dec 31, 2016, in 11 major hospitals of Lanzhou, 17,089 RDs outpatient visits during Jan 1, 2016, through Dec 31, 2018, in one hospital of Wuwei, 235,604 outpatient visits with RDs during Jan 1, 2015, to Dec 31, 2018, in one large hospital of Zhangye, and 234,029 outpatient visits with RDs during Jan 1, 2015, through Dec 31, 2018, in one large hospital of Tianshui. Among the hospital of Tianshui, there were 127,118 males (54.32%), 106,911 females (45.68%), 155,887 children and adolescents (66.61%), 64,238 adults (27.45%), and 13,904 elders (5.94%). During the study period, drought occurred on approximately 25.94% of the days in Tianshui, 17.42% in Lanzhou, 33.48% in Wuwei, and 27.52% in Zhangye (Fig. 1). In four cities, the daily average temperature of Tianshui was the highest (12.47°C), and Zhangye had the lowest minimum temperature (−22.40°C) (Table 1). Among these four cities, the daily average concentration of PM2.5 and NO2 in Lanzhou was the highest (were 54.16 μg/m3 and 50.87 μg/m3, respectively), but the highest daily average concentration of O3 was found in Zhangye (105.63 μg/m3) (Table S5).
Drought characterization for Tianshui (from 2015 to 2018), Lanzhou (from 2014 to 2016), Wuwei (from 2016 to 2018), and Zhangye (from 2015 to 2018) in the northwest of China. Blue lines represent days with no drought conditions, and red represents days with drought conditions. Moreover, the more negative the SPI-1 values, the greater the severity of the drought conditions. SPI-1 showed the weekly value.
3.2 The effects of droughts on respiratory diseases
Fig. 2 shows the associations of SPI-1 with daily outpatient visits for RDs. By conducting a meta-analysis, we found that each 1-unit decrease in the daily SPI-1 was positively and significantly associated with daily outpatient visits for RDs, the estimated RR was 1.0230 (95% CIs: 1.0096, 1.0366). For city-specific effects, the estimated effects of SPI-1 were positively linked to the daily outpatient visits for RDs in Tianshui, Lanzhou, Wuwei, and Zhangye, but Wuwei was not statistically significant (P>0.05). However, the strongest estimated RR in Lanzhou was 1.0374 (95% CIs: 1.0337, 1.0412).
Associations between drought and the daily outpatient visits for respiratory diseases in four northwest cities of China. The effect of SPI-1 is estimated as a relative risk (RR) and 95% confidence intervals (CI) to represent the risk of daily outpatient visits for respiratory diseases associated with a 1-unit decrease in exposure to SPI-1.
As shown in Fig. 3, there were significant positive associations between droughts and daily outpatient visits for RDs. Compared with the non-drought periods, the pooled RR of daily outpatient visits for RDs during all drought conditions was 1.0431 (95% CIs:1.0309, 1.0555). For city-specific effects, compared to the non-drought periods, the estimated effects of all drought conditions were positively linked to the daily outpatient visits for RDs in Tianshui, Lanzhou, Wuwei, and Zhangye, but Wuwei was not statistically significant (P>0.05). However, the strongest estimated RR in Tianshui was 1.0577 (95% CIs: 1.0459, 1.0696) (Fig. S3). In the analysis of drought severity, daily outpatient visits for RDs were positively related to light, moderate, severe, and very severe drought periods compared to non-drought periods, but only light drought was significant (P<0.05). Although the estimated RR of the moderate drought was larger than that of light drought, the difference was not significant (P >0.05). The city-specific results of drought severity are shown in Supplementary Material (Fig. S3).
The overall relative risks (RR) of daily outpatient visits for respiratory diseases associated with exposure to all drought conditions and exposure by the severity of drought from light to very severe in comparison to exposure to non-drought periods. The RRs and their 95% confidence intervals (CIs) are combined estimates pooled across four cities using meta-analysis.
3.3 The subgroup analysis
In gender-specific analyses, we observed positive and significant associations between drought and outpatient visits for RDs in both males and females (Fig. 4). Males showed a larger RR, while the difference was not significant (P>0.05). In age-specific analyses, the estimated effects of drought on outpatient visits for RDs were significant among children, adolescents (≤18 years), and adults (19~64 years). Positive but no significant association was found among the elderly (≥65 years) (Fig. 4). The estimated effects of SPI-1 on RDs were not significantly different across the three age groups, although the younger age groups tended to show larger estimates. The estimated effect of exposure to all drought conditions in comparison to exposure to non-drought periods was the highest in children and adolescent group, followed by adults and the elderly. There was evidence (P < 0.05) suggesting a difference between the children and adolescents (≤18 years) and the adults (19~64 years) (Fig. 4).
The effects of drought on the daily outpatient visits for respiratory diseases in Tianshui, stratified by gender and age. The effects of SPI-1 are estimated as relative risks (RR) and 95% confidence intervals (CIs) to represent the risk of daily outpatient visits for respiratory diseases associated with a 1-unit decrease in exposure to SPI-1. The effects of all drought conditions are estimated as RR and 95% CIs to represent the risk of daily outpatient visits for respiratory diseases associated with exposure to all drought conditions in comparison to the non-drought periods. *The difference between children and adolescents (≤18 years) and adults (19~64 years) was significant at α=0.05.
3.4 The sensitivity analysis
Fig. 5 shows the estimated effects of drought defined by the three thresholds on the daily outpatient visits for RDs. Except for Zhangye, the estimated results were similar in other regions. In Tianshui and Lanzhou, the estimated effects of drought defined by the three thresholds on respiratory diseases were positive and significant. However, the estimated effects of drought only defined by threshold 2 on the daily outpatient visits with RDs were significant in Zhangye. The estimated effects of drought defined by the three thresholds on respiratory diseases were not statistically significant in Wuwei (P>0.05). The biggest total effect was threshold 2.
The relative risks (RR) of daily outpatient visits for respiratory diseases during all drought conditions compared to non-drought periods by changing the threshold of drought defined by SPI-1. Threshold 1 indicates that drought is defined as SPI-1 value falls below 0. Threshold 2 indicates that drought is defined as SPI-1 value is less than −0.5. Threshold 3 indicates that drought is defined as SPI-1 value is less than −1.0.
The associations between drought and hospital outpatient visits for respiratory diseases were robust when adjusting for air pollution (PM2.5, NO2, and O3), changing the moving average days of temperature (lag 07, lag 014, and lag 021) and changing the df from 3 to 7 for temperature and from 6 to 9 per year for calendar time (Table S6-S10).
4 Discussion
This study reported the short-term association between drought exposure and the daily risk of outpatient visits for respiratory disease in China. The results of the present study are based on the four cities (including 1,134,577 RDs cases from 14 hospitals) in the arid area of China to assess the impact of drought on daily outpatient visits for RDs. With these data and analysis, we suggest that drought exposure may be also an important risk factor for RDs.
According to the Grades of Meteorological Drought (GB/T 20481-2017) of China (National Standardization Management Committee of China, 2017) and previous study (Li et al. 2021), SPI-1 values below −0.5 described drought conditions, and the more negative the SPI-1 values, the greater the severity of the drought conditions. In the estimated effects of SPI-1, negative coefficients of estimates obtained in the quasi-Poisson models indicated the higher risk for respiratory disease linked to severe drought events (Table S7 and Table S9). This is consistent with the study carried out by Salvador et al. (2019) in Spain and Berman et al. (2017) in the western USA. In the analysis by drought severity, daily outpatient visits for RDs were positively related to light, moderate, severe, and very severe drought periods compared to non-drought periods, but only light drought was significant (P<0.05). This may be related to the low frequency of moderate, severe, and very severe droughts (small sample size) (Fig.S3). Compared to SPI, the Standardized Precipitation-Evapotranspiration Index (SPEI) takes into account both precipitation and potential evapotranspiration (Vicente-Serrano et al. 2010). However, SPI allows for comparisons across different locations in different climates. A study by Salvador et al. (2020) that compared the performance of the SPI and SPEI to estimate the risks of droughts on daily respiratory mortality suggests that SPI may be a more sensitive drought indicator for assessing respiratory health risk. Also, we found that there were different estimated effects on the respiratory disease by changing the threshold of drought defined by SPI-1, indicating that different regions may have different thresholds for the association between drought and respiratory disease.
Although very few studies have discussed the effects of drought on respiratory health, our results are consistent with Smith et al. (2014) and Machado-Silva et al. (2020) who reported that drought events could increase the risks of respiratory diseases. In subgroup analysis, we found that males appeared to be more affected by drought than females, which might be attributed to their different physiologic characteristics and working environment. In particular, males may have more chances of outdoor exposure to drought than females due to their social role. In age-specific analyses, the estimated effects of drought on RDs in children and adolescents were greater than in adults and the elderly. It is generally recognized that this high vulnerability among the 0~18 age group can be attributed to their immature lungs and the underdeveloped immune function, which may add together to make children and adolescents more susceptible to droughts (Ma et al. 2020). Besides, our results showed a positive but non-significant association between drought exposure and outpatient visits for RDs among the elderly (≥65 years). This may be due to the small sample size of the elderly leading to the larger confidence intervals (CIs). However, Berman et al. (2017) described a decrease in respiratory hospital admissions during periods of drought among adults 65 years or older in the USA. This may be explained by the higher level of health care system for the elderly in the USA. Other explanations could be (1) different indices to measure drought; (2) different public health policies to deal with drought in each place; and (3) differences in securing livelihoods and maintaining well-being caused by different economic, educational, and cultural levels.
Although the mechanisms involved in the effects of drought on respiratory diseases are unclear, there are some potential and possible hypotheses. The drought may increase the number of particulates suspended in the air, such as pollen and smoke (Yusa and Berry 2015). These substances irritate the bronchi and lungs, worsening chronic respiratory disease and increasing the risk of acute respiratory infections (Barnes, 2018). And climate change in drought increases fungal infections by increasing the inhalational exposure of soil (Mirsaeidi et al. 2016). The toxins originating from cyanobacteria can become airborne in droughts (Richer et al. 2015). These toxins are related to lung stimulation. Also, the drought may promote the deterioration of the ecological environment, which in turn causes short-term or long-term mental health of human beings (Barreau et al. 2017; Lv et al. 2014; Stain et al. 1982). These mental stresses will influence the behavioral and physiological responses, including inflammatory, endocrine, and immunological dysfunction, which may increase the risk of respiratory diseases (Cohen et al. 2012; Pedersen et al. 2010). Another explanation could also come from the environmental changes in temperature, precipitation, and relative humidity which led to the drought, which may influence viral activity and transmission (Mirsaeidi et al. 2016; Yang and Marr 2012). These alterations may directly or indirectly affect the incidence and severity of respiratory infections by affecting the vectors and the host immune responses.
Although we found that there was a significant association between drought and RDs visits; some limitations of this study should not be ignored. Firstly, measure misclassification is a limitation in our study, but it may not cause substantial bias (Zeger et al. 2000). The individual-level confounders could not be controlled, such as indoor air pollution, second-hand smoke exposure, and personal social information. Secondly, droughts include meteorological droughts, hydrological droughts, agricultural droughts, and economic droughts (Vicente-Serrano et al. 2012). Different types of droughts have different health effects. We only estimated the effects of meteorological drought on the respiratory system. However, meteorological drought is the main cause of other droughts, and the evaluation results can be used as a basis for exploring the effects of other droughts on health. Thirdly, we use weekly SPI-1 to assume the same condition for each 7-day interval, which may lead to daily potential exposure misspecification. Finally, due to the limitation of access to respiratory disease data, Tianshui, Zhangye, and Wuwei contain only one hospital, and the sample size in Wuwei is relatively small and may not be enough to represent Wuwei. And our study covers only four regions in northwest China; thus, the generalizability should be considered when interpreting our results for other areas.
5 Conclusion
In summary, our results indicate that drought exposure is associated with an increased risk of respiratory diseases, particularly among children, adolescents, and potentially males. As droughts would become more severe and occur more frequently in the future under climate change, we should pay more attention to its potential health effects. In addition, it is significantly essential for the government to establish drought monitoring, mitigation measures, and adaptation strategies to address this global public health challenge.
Data availability
The meteorological datasets and air pollutant datasets used and/or analyzed during the current study are available from the open-access websites. The meteorological datasets of Lanzhou were from the Shanghai Meteorological Bureau. All data on outpatient visits for respiratory diseases were obtained from hospitals, which were confirmed and permitted by hospitals and related health departments.
References
Allen CD, Macalady AK, Chenchouni H, Bachelet D, McDowell N, Vennetier M, Kitzberger T, Rigling A, Breshears DD, Hogg EH, Gonzalez P, Fensham R, Zhang Z, Castro J, Demidova N, Lim J-H, Allard G, Running SW, Semerci A, Cobb N (2010) A global overview of drought and heat-induced tree mortality reveals emerging climate change risks for forests. For Ecol Manag 259(4):660–684. https://doi.org/10.1016/j.foreco.2009.09.001
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. BMJ 326(7382):219. https://doi.org/10.1136/bmj.326.7382.219
Barnes CS (2018) Impact of climate change on pollen and respiratory disease. Curr Allergy Asthma Rep 18(11):59. https://doi.org/10.1007/s11882-018-0813-7
Barreau T, Conway D, Haught K, Jackson R, Kreutzer R, Lockman A, Minnick S, Roisman R, Rozell D, Smorodinsky S, Tafoya D, Wilken JA (2017) Physical, mental, and financial impacts from drought in two California counties, 2015. Am J Public Health 107(5):783–790. https://doi.org/10.2105/AJPH.2017.303695
Berman JD, Ebisu K, Peng RD, Dominici F, Bell ML (2017) Drought and the risk of hospital admissions and mortality in older adults in western USA from 2000 to 2013: a retrospective study. Lancet Planet Health 1(1):e17–e25. https://doi.org/10.1016/S2542-5196(17)30002-5
Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, Turner RB (2012) Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci U S A 109(16):5995–5999. https://doi.org/10.1073/pnas.1118355109
Ebi KL, Bowen K (2016) Extreme events as sources of health vulnerability: drought as an example. Weather and Climate Extremes 11:95–102. https://doi.org/10.1016/j.wace.2015.10.001
Franchini M, Mannucci PM (2015) Impact on human health of climate changes. European J Int Med 26(1):1–5. https://doi.org/10.1016/j.ejim.2014.12.008
Li W, Duan L, Wang W, Wu Y, Liu T, Quan Q, Chen X, Yin H, Zhou Q (2021) Spatiotemporal characteristics of drought in a semi-arid grassland over the past 56 years based on the Standardized Precipitation Index. Meteorog Atmos Phys 133(1):41–54. https://doi.org/10.1007/s00703-020-00727-4
Lv OB, Berry HL, Coleman C, Hanigan IC (2014) Drought as a mental health exposure. Environ Res 131:181–187. https://doi.org/10.1016/j.envres.2014.03.014
Ma Y, Yue L, Liu J, He X, Li L, Niu J, Luo B (2020) Association of air pollution with outpatient visits for respiratory diseases of children in an ex-heavily polluted Northwestern city, China. BMC Public Health 20(1):816. https://doi.org/10.1186/s12889-020-08933-w
Machado-Silva F, Libonati R, Melo de Lima TF, Bittencourt Peixoto R, de Almeida França JR, De Avelar Figueiredo Mafra Magalhães M, Lemos Maia Santos F, Abrantes Rodrigues J, CC DC (2020) Drought and fires influence the respiratory diseases hospitalizations in the Amazon. Ecol Indic 109:105817. https://doi.org/10.1016/j.ecolind.2019.105817
Maskey S, Trambauer P (2015) Chapter 10 - Hydrological modeling for drought assessment. In: Shroder JF, Paron P, Baldassarre GD (eds) Hydro-meteorological hazards, risks and disasters. Elsevier, Boston, pp 263–282. https://doi.org/10.1016/B978-0-12-394846-5.00010-2
Mirsaeidi M, Motahari H, Taghizadeh Khamesi M, Sharifi A, Campos M, Schraufnagel DE (2016) Climate change and respiratory infections. Annals Am Thorac Soc 13:1223–1230. https://doi.org/10.1513/AnnalsATS.201511-729PS
National Standardization Management Committee of China(2017) Grades of Meteorological Drought (GB/T20481-2017). http://c.gb688.cn/bzgk/gb/showGb?type=online&hcno=D2281945A96E8185F67EDC9E7A698049. Accessed 10 Mar 2021.
Pedersen A, Zachariae R, Bovbjerg DH (2010) Influence of psychological stress on upper respiratory infection--a meta-analysis of prospective studies. Psychosom Med 72(8):823–832. https://doi.org/10.1097/PSY.0b013e3181f1d003
Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT (2016) Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect 124(9):1334–1343. https://doi.org/10.1289/ehp.1409277
Richer R, Banack SA, Metcalf JS, Cox PA (2015) The persistence of cyanobacterial toxins in desert soils. J Arid Environ 112:134–139. https://doi.org/10.1016/j.jaridenv.2014.01.023
Salvador C, Nieto R, Linares C, Diaz J, Gimeno L (2019) Effects on daily mortality of droughts in Galicia (NW Spain) from 1983 to 2013. Sci Total Environ 662:121–133. https://doi.org/10.1016/j.scitotenv.2019.01.217
Salvador C, Nieto R, Linares C, Díaz J, Gimeno L (2020) Short-term effects of drought on daily mortality in Spain from 2000 to 2009. Environ Res 183:109200. https://doi.org/10.1016/j.envres.2020.109200
Schwalm CR, Anderegg WRL, Michalak AM, Fisher JB, Biondi F, Koch G, Litvak M, Ogle K, Shaw JD, Wolf A, Huntzinger DN, Schaefer K, Cook R, Wei Y, Fang Y, Hayes D, Huang M, Jain A, Tian H (2017) Global patterns of drought recovery. Nature 548(7666):202–205. https://doi.org/10.1038/nature23021
Shahi AM, Omraninava A, Goli M, Soheilarezoomand HR, Mirzaei N (2014) the effects of air pollution on cardiovascular and respiratory causes of emergency admission. Emerg 2(3):107–114
Shuman EK (2010) Global climate change and infectious diseases. N Engl J Med 362(12):1061–1063. https://doi.org/10.1056/NEJMp0912931
Smith LT, Aragão LE, Sabel CE, Nakaya T (2014) Drought impacts on children’s respiratory health in the Brazilian Amazon. Sci Rep 4:3726. https://doi.org/10.1038/srep03726
Stain HJ, Kelly B, Carr VJ, Lewin TJ, Fitzgerald M (1982) Fragar L (2011) The psychological impact of chronic environmental adversity: responding to prolonged drought. Soc Sci Med 73(11):1593–1599. https://doi.org/10.1016/j.socscimed.2011.09.016
Stanke C, Kerac M, Prudhomme C, Medlock J, Murray V (2013) Health effects of drought: a systematic review of the evidence. PLoS currents 5. https://doi.org/10.1371/currents.dis.7a2cee9e980f91ad7697b570bcc4b004
Su B, Huang J, Fischer T, Wang Y, Kundzewicz ZW, Zhai J, Sun H, Wang A, Zeng X, Wang G, Tao H, Gemmer M, Li X, Jiang T (2018) Drought losses in China might double between the 1.5 °C and 2.0 °C warming. Proceedings of the National Academy of Sciences 115(42):10600. https://doi.org/10.1073/pnas.1802129115
Vicente-Serrano SM, Beguería S, López-Moreno JI (2010) A multiscalar drought index sensitive to global warming: the standardized precipitation evapotranspiration index. J Clim 23:1696–1718. https://doi.org/10.1175/2009JCLI2909.1
Vicente-Serrano SM, Beguería S, Lorenzo-Lacruz J, Camarero JJ, López-Moreno JI, Azorin-Molina C, Revuelto J, Morán-Tejeda E, Sanchez-Lorenzo A (2012) Performance of drought indices for ecological, agricultural, and hydrological applications. Earth Interact 16(10):1–27. https://doi.org/10.1175/2012EI000434.1
Wang Z, Deng X, Li X, Zhou Q, Yan H (2015) Impact analysis of government investment on water projects in the arid Gansu Province of China. Phys Chem Earth 79-82:54–66. https://doi.org/10.1016/j.pce.2015.03.006
Wang L, Liu C, Meng X, Niu Y, Lin Z, Liu Y, Liu J, Qi J, You J, Tse LA, Chen J, Zhou M, Chen R, Yin P, Kan H (2018a) Associations between short-term exposure to ambient sulfur dioxide and increased cause-specific mortality in 272 Chinese cities. Environ Int 117:33–39. https://doi.org/10.1016/j.envint.2018.04.019
Wang S, Li Y, Niu A, Liu Y, Su L, Song W, Liu J, Liu Y, Li H (2018b) The impact of outdoor air pollutants on outpatient visits for respiratory diseases during 2012-2016 in Jinan, China. Respir Res 19(1):246. https://doi.org/10.1186/s12931-018-0958-x
Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Berry H, Bouley T, Boykoff M, Byass P, Cai W, Campbell-Lendrum D, Chambers J, Daly M, Dasandi N, Davies M, Depoux A, Dominguez-Salas P, Drummond P, Ebi KL, Ekins P, Montoya LF, Fischer H, Georgeson L, Grace D, Graham H, Hamilton I, Hartinger S, Hess J, Kelman I, Kiesewetter G, Kjellstrom T, Kniveton D, Lemke B, Liang L, Lott M, Lowe R, Sewe MO, Martinez-Urtaza J, Maslin M, McAllister L, Mikhaylov SJ, Milner J, Moradi-Lakeh M, Morrissey K, Murray K, Nilsson M, Neville T, Oreszczyn T, Owfi F, Pearman O, Pencheon D, Pye S, Rabbaniha M, Robinson E, Rocklöv J, Saxer O, Schütte S, Semenza JC, Shumake-Guillemot J, Steinbach R, Tabatabaei M, Tomei J, Trinanes J, Wheeler N, Wilkinson P, Gong P, Montgomery H, Costello A (2018a) The 2018 report of the Lancet Countdown on health and climate change: shaping the health of nations for centuries to come. Lancet 392(10163):2479–2514. https://doi.org/10.1016/s0140-6736(18)32594-7
Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, Boykoff M, Byass P, Cai W, Campbell-Lendrum D, Chambers J, Cox PM, Daly M, Dasandi N, Davies M, Depledge M, Depoux A, Dominguez-Salas P, Drummond P, Ekins P, Flahault A, Frumkin H, Georgeson L, Ghanei M, Grace D, Graham H, Grojsman R, Haines A, Hamilton I, Hartinger S, Johnson A, Kelman I, Kiesewetter G, Kniveton D, Liang L, Lott M, Lowe R, Mace G, Odhiambo Sewe M, Maslin M, Mikhaylov S, Milner J, Latifi AM, Moradi-Lakeh M, Morrissey K, Murray K, Neville T, Nilsson M, Oreszczyn T, Owfi F, Pencheon D, Pye S, Rabbaniha M, Robinson E, Rocklöv J, Schütte S, Shumake-Guillemot J, Steinbach R, Tabatabaei M, Wheeler N, Wilkinson P, Gong P, Montgomery H, Costello A (2018b) The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet 391(10120):581–630. https://doi.org/10.1016/s0140-6736(17)32464-9
Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, Boykoff M, Byass P, Cai W, Campbell-Lendrum D, Capstick S, Chambers J, Coleman S, Dalin C, Daly M, Dasandi N, Dasgupta S, Davies M, Di Napoli C, Dominguez-Salas P, Drummond P, Dubrow R, Ebi KL, Eckelman M, Ekins P, Escobar LE, Georgeson L, Golder S, Grace D, Graham H, Haggar P, Hamilton I, Hartinger S, Hess J, Hsu S-C, Hughes N, Jankin Mikhaylov S, Jimenez MP, Kelman I, Kennard H, Kiesewetter G, Kinney PL, Kjellstrom T, Kniveton D, Lampard P, Lemke B, Liu Y, Liu Z, Lott M, Lowe R, Martinez-Urtaza J, Maslin M, McAllister L, McGushin A, McMichael C, Milner J, Moradi-Lakeh M, Morrissey K, Munzert S, Murray KA, Neville T, Nilsson M, Sewe MO, Oreszczyn T, Otto M, Owfi F, Pearman O, Pencheon D, Quinn R, Rabbaniha M, Robinson E, Rocklöv J, Romanello M, Semenza JC, Sherman J, Shi L, Springmann M, Tabatabaei M, Taylor J, Triñanes J, Shumake-Guillemot J, Vu B, Wilkinson P, Winning M, Gong P, Montgomery H, Costello A (2020) The 2020 report of the Lancet Countdown on health and climate change: responding to converging crises. Lancet. https://doi.org/10.1016/S0140-6736(20)32290-X
World Meteor Org (2012) Standardized precipitation index user guide (M.Svoboda,M.HayesandD.Wood).(WMO-No.1090), Geneva. https://public.wmo.int/en/resources/library/standardized-precipitation-index-user-guide. Accessed 13 Mar 2021.
Wu X, Liu H, Li X, Ciais P, Babst F, Guo W, Zhang C, Magliulo V, Pavelka M, Liu S, Huang Y, Wang P, Shi C, Ma Y (2018) Differentiating drought legacy effects on vegetation growth over the temperate Northern Hemisphere. Glob Chang Biol 24(1):504–516. https://doi.org/10.1111/gcb.13920
Xu M, Kang S, Li J (2015) Evaluation of water storage change of inland cryosphere in northwestern China. Adv Meteorol 2015:681634. https://doi.org/10.1155/2015/681634
Yang W, Marr LC (2012) Mechanisms by which ambient humidity may affect viruses in aerosols. Appl Environ Microbiol 78(19):6781. https://doi.org/10.1128/AEM.01658-12
Yusa A, Berry P, JC J, Ogden N, Bonsal B, Stewart R, Waldick R (2015) Climate change, drought and human health in Canada. Int J Environ Res Public Health 12(7):8359–8412. https://doi.org/10.3390/ijerph120708359
Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, Cohen A (2000) Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect 108(5):419–426. https://doi.org/10.1289/ehp.00108419
Zhang X, Chen N, Sheng H, Ip C, Yang L, Chen Y, Sang Z, Tadesse T, Lim TPY, Rajabifard A, Bueti C, Zeng L, Wardlow B, Wang S, Tang S, Xiong Z, Li D, Niyogi D (2019) Urban drought challenge to 2030 sustainable development goals. Sci Total Environ 693:133536. https://doi.org/10.1016/j.scitotenv.2019.07.342
Funding
This work was supported by the Fundamental Research Funds for the Central Universities, Lanzhou University, China (lzujbky-Stain et al., 1982-ey07), National Natural Science Foundation of China (4187050043), and Soft Science Special Project of Gansu Province (20CX4ZA028).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOC 1044 kb)
Rights and permissions
About this article
Cite this article
Wang, B., Wang, S., Li, L. et al. The association between drought and outpatient visits for respiratory diseases in four northwest cities of China. Climatic Change 167, 2 (2021). https://doi.org/10.1007/s10584-021-03152-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10584-021-03152-7