Abstract
Trauma exposure can lead to poor psychological health not only for those directly affected, but also for their children. Additional research is needed to understand mechanisms in the intergenerational sequelae of traumatic stress. The current study examined parenting stress as a moderator of the association between parents’ lifetime trauma exposure and school-aged children’s internalizing symptoms (N = 139 dyads). Results of multiple regression analyses showed that the relationships between parental trauma exposure and child separation anxiety and harm avoidance were significant when parenting stress was moderate to high, but not when parenting stress was low. Parental trauma exposure was not significantly associated with child depressive symptoms. Clinical implications include the importance of screening and addressing parents’ trauma exposure and parenting stress in the context of child and family mental health services. Further research is needed to explicate the mechanisms linking parents’ trauma exposure with child anxiety symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Most adults in the United States have experienced at least one traumatic event. The results of a large-scale nationally representative study found that 89.7% of respondents had experienced at least one traumatic event meeting DSM-5 criteria, with many endorsing multiple event types [1]. Trauma exposure is associated with a number of deleterious health consequences, including both physical and mental health problems [2,3,4]. Given the widespread nature of trauma exposure, investigating the paths through which trauma exerts an impact on children is a public health priority [5].
Trauma exposure can have intergenerational consequences, affecting not only the exposed individuals but also their children. Not only is parental trauma exposure associated with an increased risk of trauma exposure for children [6], but it is also associated with child psychopathology even in the absence of child trauma exposure [7,8,9]. Results of a recent literature review indicate that young children of parents with PTSD symptoms tend to be more emotionally labile and have more negative affect, and that when these children are older, they tend to have more problems with psychosocial functioning [10]. According to the tripartite model, negative affect is a core feature of both depressive and anxiety disorders [11], suggesting that children of parents struggling with the effects of trauma exposure may be more prone to depressive and anxiety disorders compared to children of parents without trauma exposure.
Efforts to understand the intergenerational consequences of trauma exposure indicate that, among other factors (e.g., heightened stress reactivity, epigenetic factors), parents’ trauma exposure may affect children through problematic parent–child interactions. According to the theory of parent–child coregulation, the dynamic, moment-to-moment interactions between parents and children are fundamental to the development of children’s self-regulation [12, 13]. However, parents’ difficulty coping with traumatic experiences can derail the coregulation process [14]. Parents exposed to trauma may exhibit behaviors consistent with posttraumatic stress symptomatology, such as irritable behavior and angry outbursts, persistent negative emotional states, detachment from others, or dissociative symptoms which can be observed and reenacted by the child [15, 16] or can create a state of fear in the child [17, 18]. Additionally, parents may be unable to provide the support necessary to help children cope with distress if they are coping with their own posttraumatic stress symptoms [19].
Although parental trauma exposure can have negative effects on children’s mental health, many children whose parents have experienced trauma experience no disruption in the course of their development. This is consistent with the developmental psychopathology tenets of multifinality and equifinality—that is, the same risk factor may have different outcomes, and that different risk factors may have the same outcome, respectively [20]. Additional research needed to understand the factors associated with multifinality in this particular developmental pathway—that is, why some children with trauma-exposed parents develop psychopathology whereas others appear well-adjusted [10]. A recent meta-analysis found a moderate effect size for the link between parent PTSD and child psychopathology (PTSD, depression, anxiety, behavior problems), but identified significant variability across studies, suggesting that moderators may account for heterogeneity in this relation [8].
Parenting stress may be a potential moderator of the relationship between parent trauma and child outcomes. Parenting stress, or “aversive feelings associated with demands of parenting role”, is a normative experience of parenting [21]. However, when present at high levels, parenting stress can undermine effective parenting behaviors [22] and affect children’s well-being [23]. The day-to-day hassles associated with parenting may be particularly burdensome for parents exposed to trauma who are already struggling with more significant difficulties with emotion regulation. This theorizing is consistent with the diathesis stress model, which holds that individuals with certain vulnerability factors may be differentially susceptible to environmental stressors. Vulnerabilities include premorbid factors such as genetic makeup, temperament, biological characteristics, or preexisting conditions [24, 25].
This study examines the relation between parental trauma exposure and child psychopathology through the diathesis stress model, considering prior trauma exposure as a diathesis that is activated by parenting stress. Despite trauma exposure, many parents may function well in their parent–child relationships, particularly given the prevalence of trauma exposure in the general population. However, significant stress in the parenting role may activate cognitive, behavioral, and affective processes related to their prior trauma exposure, resulting in trauma-related psychopathology. It is expected that functional impairments of psychopathology would include deficits in the parenting domain, increasing children’s risk for psychopathology. Late middle childhood (the period immediately preceding adolescence) presents unique developmental challenges for parents that may highlight the relationships among parental trauma exposure, parenting stress, and child psychopathology. During this developmental period, children become increasingly autonomous in their self-regulation [26]. With decreasing parental support, deficits in children’s emotion regulation may manifest and contribute to psychopathology. Further, as the developmental period immediately preceding adolescence, late middle childhood is an important time to examine elevated internalizing symptomatology as rates of depressive disorders and some types of anxiety disorders increase sharply thereafter [27, 28]. Prior literature on the effects of parents’ trauma exposure on their offspring has primarily focused on infants and young children, and additional research is needed to examine the effects of parental trauma exposure on child psychopathology among older children.
Thus, the current study sought to examine parenting stress as a moderator of the relation between parents’ cumulative trauma exposure and their school-aged children’s internalizing psychopathology. Depression and anxiety were selected as child outcomes of parental trauma exposure in the present study given prior research showing that emotional lability and negative affectivity are higher among children of trauma-exposed parents [10]. Child participants were recruited during late middle childhood to address the unique characteristics of this developmental period with regard to the study aim. We used linear regression analyses to test whether the interaction between parents’ trauma exposure and their parenting stress would significantly predict (a) children’s depressive symptoms, and (b) children’s anxiety symptoms. We hypothesized that parents’ trauma exposure would interact with their parenting stress to predict children’s internalizing symptoms. That is, we expected that the effect of parental trauma exposure on (a) children’s depressive symptoms and (b) children’s anxiety symptoms would be exacerbated by parenting stress.
Methods
Participants
Boys and girls (N = 139; 53% girls, Mage = 9.83, SDage = 1.49) between the ages of 8 and 12 and their primary caregivers (N = 139; 91% female, Mage = 37.91, SDage = 6.28) participated in this cross-sectional study. Missing data (see Measures for a description of percent missingness in each study variable) was handled using multiple imputation. Participants were recruited via internet postings and flyers. The data from this community sample were collected from a racially and ethnically diverse area within a southern California suburb of Los Angeles. The racial and ethnic breakdown of the sample matched the demographics of the area from which participants were recruited. The resulting sample was diverse in terms of race/ethnicity (39% Hispanic, 34% Caucasian, 18% African American, 5% Other, 3% Asian, and 1% Native American) and annual household income (49% reported annual income < $40,000, 22% $41,000–60,000, and 29% > $61,000). The Institutional Review Board approved this study prior to its inception.
Procedure
Upon arrival at the laboratory, research assistants explained the study protocol to dyads. During the session, children provided written assent and parents provided written informed consent. Parents reported on family demographics, parental stress, and trauma history. Child participants reported on their anxiety and depressive symptoms.
Measures
Parents’ Trauma History
The Traumatic Life Events Checklist (TLEC) [29] is a 23-item questionnaire assessing the number of times a person has experienced a wide range of traumatic events (e.g., assault, witnessing violence, natural disasters, sudden losses). This measure has strong psychometric properties and construct validity [29]. For each of the 23 experiences listed on this measure, participants indicated whether they had experienced the event (Yes) or not (No). In this study we computed the total number of traumatic events participants had experienced. Summing traumatic experiences is a common methodological approach to examine dosage of trauma exposure, such as in the Adverse Childhood Experiences literature [3]. The TLE total number of events variable had 12% missingness in this sample.
Parental Stress
The Parenting Stress Index, Short Form (PSI-SF) [30] is a brief self-report instrument designed to measure perceived stress associated with the demands of parenting children under 12 years old. Respondents indicate their level of agreement with 36 items on a 5-point Likert scale. The PSI-SF yields a Total Score and three subscales: Difficult Child, Dysfunctional Parent–Child Interactions, and Parental Distress. Analyses for the current study used only the Total Score. Internal consistency in this sample was good, αPSI-SF total score = 0.91. The PSI-SF total score had 9% missingness in the study sample.
Children’s Anxiety
The Multidimensional Anxiety Scale for Children (MASC) [31] is a 39-item questionnaire for use with youth between eight and 18 years of age. The questionnaire assesses four main aspects of anxiety: (1) physical symptoms (tense/restless and somatic/autonomic), (2) social anxiety (humiliation/rejection and public performance fears), (3) harm avoidance (anxious coping and perfectionism) and (4) separation anxiety. Children state the degree to which each item describes them (from 0 for “never true about me” to 3 for “often true about me”). The MASC total score and its subscales have demonstrated strong reliability and validity in clinical and community samples [31, 32]. In the current study we used the total and subscale scores from the MASC. In this sample, Cronbach’s alpha in this sample was acceptable for the MASC Total Score (α = 0.88), the Social Anxiety subscale (α = 0.85), the Physical Symptoms subscale (α = 0.82), the Separation Anxiety subscale (α = 0.68), and the Harm Avoidance subscale (α = 0.69). The MASC had less than 1% missingness in this sample.
Children’s Depressive Symptoms
The Children’s Depression Inventory (CDI) [33], designed for use with children between 7 and 18 years, is a 27-item measure assessing the cognitive, emotional, behavioral and physiological symptoms of depression. Children choose one of three best-fitting statements to describe their symptoms over the past 2 weeks (e.g. “I am sad once in a while [0],” “I am sad many times [1]”, “I am sad all the time [2]”). The CDI yields a total score as well as four subscales: Negative Mood/Physical Symptoms, Negative Self-Esteem, Ineffectiveness, and Interpersonal Problems. The CDI is reliable and valid [33, 34]. In this sample, Cronbach’s alpha was acceptable for the CDI total score (α = 0.86), and the Ineffectiveness subscale (α = 0.69), but was below the level of acceptability for the Negative Mood/Physical Symptoms subscale (α = 0.44), the Negative Self-Esteem subscale (α = 0.49), and the Interpersonal Problems subscale (α = 0.46). There was no data missing from the CDI in this sample.
Data Analytic Plan
Data analysis for the study aim, to examine parenting stress as a moderator of the relation between parents’ cumulative trauma exposure and children’s internalizing symptoms (anxiety and depression), was conducted using hierarchical linear regression. Andrew Hayes’ PROCESS macro for SPSS was used [35]. Missing data was handled using multiple imputation. As Little’s MCAR test was nonsignificant (χ2(132) = 143.55, p = 0.23), the null hypothesis that data were missing completely at random was not rejected. Thus, multiple imputation was justified and performed using 10 iterations with the aid of the mice package in R [36]. The independent variable (mean of the traumatic events endorsed on the TLE), moderator variable (mean of all PSI-SF items), and outcome variables (mean of all CDI items, mean of CDI subscale items, and total and subscale scores on the MASC) were mean centered prior to analysis.
First, a linear regression model was examined to test the hypothesis that parenting stress moderates the relation between parent trauma and child depressive symptoms. Second, a linear regression model was examined to test the hypothesis that parenting stress moderates the relation between parent trauma and child anxiety symptoms. Linear regression models were examined for CDI and/or MASC subscale scores if the regression model with the total score was found to be significant.
Results
Table 1 presents the demographic characteristics of the sample and Table 2 presents intercorrelations among study variables and descriptive statistics. Results of two-sample t-tests indicated that CDI, MASC, and PSI-SF total scores did not differ by child gender. Correlations among study variables and demographic characteristics (parent and child age and gender, parent race/ethnicity, annual household income) were explored. Annual household income was negatively correlated with total number of parental traumas reported on the TLE (r = − 0.228, p = 0.01) such that as the number of parental traumas increased, family income decreased. In addition, child age was negatively correlated with the PSI-SF total score (r = − 0.212, p = 0.02). As such, annual household income and child age were included as covariates in subsequent analyses.
Moderation Analyses
Hayes’ PROCESS macro [35] was used to test the hypothesized linear regression moderation models—specifically, that the relations between TLE total score and CDI and MASC total and subscale scores would be moderated by PSI-SF total score. To avoid multicollinearity, TLE total score and PSI-SF total score were mean centered prior to analysis. The sample size for all analyses was 139. Aim 1 and 2 results are presented in Table 3.
Aim 1: Child Depressive Symptoms
The model with PSI-SF total score moderating the relation between TLE total score and CDI total score was not significant (R2 = 0.05, F(1,133) = 1.64, p = 0.15, n = 139). Thus, the hypothesis that PSI-SF total score would moderate the association between TLE total score and CDI total score was not supported. Given this finding, no further analyses were conducted with CDI subscales.
Aim 2: Child Anxiety Symptoms
The model with PSI-SF total score moderating the relation between TLE total score and MASC total score approached statistical significance (R2 = 0.07, F(1,133) = 2.13, p = 0.07). Although individual associations should be interpreted with caution given that the overall model p value was greater than 0.05, the interaction term was significant (Δ R2 = 0.03, F(1,133) = 4.79, p = 0.03), suggesting the possibility that moderation analyses with specific dimensions of childhood anxiety (i.e. MASC subscales) may be significant.
Neither the MASC Physical Symptoms subscale (R2 = 0.07, F(1,133) = 1.59, p = 0.17) nor the MASC Social Anxiety subscale (R2 = 0.05, F(1,133) = 1.48, p = 0.20) was significantly predicted by the interaction between TLE total score and PSI-SF total score. The model predicting the MASC Separation Anxiety subscale from the interaction between the TLE total score and the PSI-SF total score was significant (R2 = 0.29, F(1,133) = 2.51, p = 0.03) as was the interaction term (ΔR2 = 0.04, b = 0.04, t = 2.54, F(1,133) = 2.58, p = 0.01). The model predicting the MASC Harm Avoidance subscale from the interaction between the TLE total score and the PSI-SF total score was also significant (R2 = 0.32, F(1,133) = 3.00, p = 0.01) as was the interaction term (ΔR2 = 0.04, b = 0.04, t = 2.54, F(1,133) = 2.52, p = 0.01).
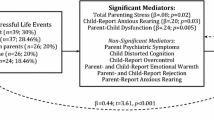
Post-hoc probing indicated that there was no significant relation between TLE total score and MASC Separation Anxiety or Harm Avoidance at low levels of parenting stress (PSI-SF 16th percentile). However, as parenting stress increases, a positive association between parental trauma and child psychopathology emerged. For MASC Separation Anxiety, the interaction between TLE and PSI-SF was not significant at moderate levels of parenting stress (PSI-SF 50th percentile) but was significant at high levels (84th percentile; b = 0.04, t = 2.38, p < 0.05; see Fig. 1). For MASC Harm Avoidance, the interaction between TLE and PSI-SF was significant at both moderate (b = 0.04, t = 2.70, p < 0.01) and high (b = 0.05, t = 3.2, p < 0.01) levels of parenting stress (see Fig. 2).
Interaction between parenting stress and parental trauma in relation to child separation anxiety. Results of multiple regression showed that parenting stress moderated the association between number of lifetime traumatic incidents reported by parents on the Traumatic Life Events (TLE) and children’s self-reported separation anxiety on the Multidimensional Anxiety Scale for Children (MASC). The association between TLE and MASC Separation Anxiety was not significant when parenting stress was low (16th percentile or below) but was significant when parenting stress was moderate (50th percentile) or high (84th percentile)
Interaction between parenting stress and parental trauma in relation to child harm avoidance. Results of multiple regression showed that parenting stress moderated the association between number of lifetime traumatic incidents reported by parents on the Traumatic Life Events (TLE) and children’s self-reported harm avoidance on the Multidimensional Anxiety Scale for Children (MASC). The association between TLE and MASC Harm Avoidance was not significant when parenting stress was low (16th percentile or below) but was significant when parenting stress was moderate (50th percentile) or high (84th percentile)
Discussion
Findings from the current study demonstrate significant associations between parental trauma exposure and child anxiety symptoms—specifically, separation anxiety and harm avoidance. As hypothesized, parental trauma exposure was positively associated with child anxiety symptoms and there were differences in the strength of this association depending on the level of parenting stress. For parents with low parenting stress, the relationship between parent trauma exposure and child anxiety was not significant. However, parent trauma exposure was positively associated with child anxiety among parents with moderate and high parenting stress. This is consistent with findings from other studies that demonstrate maternal trauma is associated with child behavior problems through parenting stress [37], and that parenting stress is associated with the relationship between maternal PTSD and child internalizing behaviors [15]. Taken together, these findings indicate that children of parents who are exposed to trauma are at increased risk for mental health concerns, but this risk is specific to the context of elevated levels of parenting stress. Results support application of the diathesis stress model to the intergenerational consequences of parents’ trauma exposure. That is, parents’ prior trauma exposure is a vulnerability factor that is activated when parenting stress reaches moderate levels.
Parents’ trauma exposure was associated with children’s separation anxiety and harm avoidance symptoms but not with social anxiety, physical symptoms, or total anxiety. Prior research has found that separation anxiety and avoidance are common outcomes among children exposed to traumatic events [38, 39]. However, this study is the first to demonstrate that separation anxiety and harm avoidance symptoms in children are also associated with parents’ trauma exposure. A possible explanation is that parents’ trauma history is associated with modeling and reinforcing anxiety and avoidance. For example, parents who have experienced trauma may be more likely to provide excessive reassurance, accommodate children’s anxiety, and provide direct messages about avoiding harm moreso than parents who do not have a traumatic learning history. Prior research has found that parental intrusiveness (e.g. taking over tasks that children could do independently) is associated with children’s separation anxiety, possibly because this type of parental behavior limits children’s mastery experiences and induces dependence on caregivers [40]. Some studies have found that parental intrusiveness is higher among parents reporting childhood maltreatment compared to those without childhood maltreatment, though this research is limited to parents of infants and young children [41, 42]. Thus, parental trauma exposure may be associated with separation anxiety through parental intrusiveness. Additional research is needed to explore these mechanisms of the link between parental trauma exposure and children’s anxiety.
Although parental trauma was associated with child anxiety, it was not associated with child depression. This surprising finding supports distinguishing among types of child psychopathology when trying to understand intergenerational consequences of trauma exposure. Although there has been a recent push towards transdiagnostic approaches to the study of psychopathology [43, 44]—including the tripartite model which identifies depression and anxiety as sharing the core feature of negative affectivity—it is noteworthy that parents’ trauma exposure was uniquely associated with risk for anxiety. Anxiety tends to have an earlier age of onset compared to depression [45], so it is possible that the children identified in the current study as having anxiety may be at risk for depressive disorders at a later stage in their development. Another explanation for the association between parents’ trauma and children’s anxiety, but not children’s depression, may be the role that behavioral modeling plays in the intergenerational transmission of traumatic stress. According to social learning theory, children learn new behaviors observationally through modeling; this includes parents modeling behavior consistent with psychopathology [46]. Parents’ posttraumatic stress symptoms such as hypervigilance, avoidance of trauma reminders, and verbalizations of worry may model anxiety and avoidance behaviors more than depressive behavior.
Trauma exposure was highly prevalent among parents in this sample, with parents endorsing an average of over six traumatic life events. Given that parental trauma exposure was positively associated with mental health symptoms for children, the results of this study highlight the importance of assessing parent trauma history and current functioning through family-focused assessment and intervention in the content of mental health interventions for children and families. Although an increasing number of investigations demonstrate associations between parent trauma exposure and child mental health outcomes [10, 15, 37], routine comprehensive and sensitive assessment along with coordinated parent–child services continues to be limited.
The predominance of research examining parenting stress has focused on the experiences of parents of young children. Thus, the current study constitutes a contribution to the literature by providing an assessment of parenting stress among parents of older children. As with studies using the Parenting Stress Index—Short Form with parents of infants and toddlers [47], the current study found that parents of older children also report experiencing moderate stress levels. Although we did not directly measure the sources of parenting stress, we anticipate that they differ from the sources of stress for parents of younger children—that they may derive from age-appropriate causes, such as the need to support children’s academics, peer relationships, identity development, activities, as well as other more universal sources of parenting stress (e.g., finances, discipline, decision-making, managing difficult emotions in one’s child) and for parents of older children, stress levels is meaningfully related to constructs of interest.
Future Research Directions
This study provides novel information about the moderating role of parenting stress on the association between parental trauma exposure and children’s psychopathology. Additional research is needed to explicate the mechanisms of the intergenerational transmission of parents’ traumatic stress. As mentioned earlier, one potential mechanism could be modeling of anxious and avoidant behaviors. Future studies may use behavior observational techniques and longitudinal study design to assess whether parents’ posttraumatic stress symptoms exhibited during interactions with their children mediate the link between parents’ trauma exposure and child psychopathology. Another potential mechanism may be parental responsiveness. Characterized by the expression of warmth, acceptance, and attention to their child’s physical and emotional needs, parental responsiveness is a key factor to promote positive emotional and behavioral outcomes for children [48]. Parents who are struggling with psychological outcomes of trauma exposure may spend less time or be less attuned to their children (i.e. less responsive), which may in turn increase children’s risk for anxiety symptoms. Directly assessing these potential mediators deserves attention in future studies.
Limitations
The findings of this study should be interpreted in light of its limitations. The study is cross-sectional in nature, which limits causal inferences about the nature of the association between parents’ trauma exposure and children’s anxiety. The fact that parents retrospectively reported on their lifetime trauma exposure makes it likely that their trauma exposure occurred prior to the onset of their children’s anxiety symptoms, but the study design precludes definite conclusions regarding causality. Data regarding characteristics of parent trauma experiences (age at exposure, chronicity, perpetrator, etc.) or specific mental health diagnoses were not available, and thus it was not possible to explore differences in the association between parental trauma exposure and child psychopathology based on these important characteristics. The trauma data was self-reported and retrospective, which carries with it some limitations in that parents’ memories may be biased. Further, the use of parental self-report to gather data on parental trauma exposure and parenting stress carries the risk of common method variance.
Nonetheless, results of this study underscore the importance of considering parent trauma history and parenting stress in the assessment and treatment of children and directly addressing the multigenerational transmission of the impact of trauma exposure on child mental health outcomes. Finally, while we consider it a strength that our sample included some fathers, the ultimate number of fathers who participated in the study was too low to enable us to conduct any meaningful cross-gender comparisons between mothers and fathers. Thus, in future studies it will be important to collect data from larger and more gender-balanced samples of parents to address these research questions.
Clinical Implications
The current study’s findings have clinical implications. First, results support the argument that parental trauma exposure is a risk factor for the development of child anxiety symptoms, except when parenting stress is low. This indicates the importance of screening parents’ trauma history in child mental health prevention and treatment services. Identifying parental trauma exposure can guide providing additional resources to help parents manage their stress symptoms and support to reduce risk for child psychopathology. Further, study findings provide additional support for growing calls to target parenting stress in interventions with children exposed to trauma [15]. The daily demands of parenting are numerous. Even parents who possess effective parenting knowledge may find themselves unable to behave skillfully in the context of stress due to decreased emotion regulation capacity [49, 50]. Effectively managing parenting stress may reduce mental health problems, particularly anxiety, for children whose parents have experienced several traumatic life events. Further, parental trauma has been identified as a barrier to successful parenting intervention completion [51, 52]. When providing treatment to families in which a parent has experienced trauma, it may be important to consider modifications to help parents identify sources of stress and build effective coping mechanisms.
Summary
Trauma exposure can lead to poor psychological health not only for those directly affected, but also for their children. Variability in the degree of association between parents’ trauma exposure and children’s psychopathology suggest that additional research is needed to understand the intergenerational transmission of traumatic stress. The current study examined parenting stress as a moderator the association between the number of parents’ lifetime traumatic events and school-aged children’s internalizing symptoms (depression and anxiety) among a sample of 139 parent–child dyads. Results of multiple regression analyses showed that parenting stress moderated the association between parents’ trauma exposure and children’s separation anxiety and harm avoidance symptoms, but not between parents’ trauma exposure and children’s depressive symptoms. The relationships between parent trauma exposure and child anxiety were significant among dyads including parents with moderate and high parenting stress, but not among those with low parenting stress. Findings support application of the diathesis stress model to the intergenerational consequences of parental trauma exposure—that is, that trauma exposure is a vulnerability factor for parents which is activated by moderate to high parenting stress. Clinical implications include the importance of screening and addressing parents’ trauma exposure and parenting stress in the context of child and family mental health services. Further research is needed to explicate the mechanisms linking parents’ trauma exposure with child anxiety symptoms.
References
Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ (2013) National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria: DSM-5 PTSD prevalence. J Trauma Stress 26:537–547. https://doi.org/10.1002/jts.21848
Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH (2006) The enduring effects of abuse and related adverse experiences in childhood: a convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci 256:174–186. https://doi.org/10.1007/s00406-005-0624-4
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am J Prev Med 14:245–258. https://doi.org/10.1016/S0749-3797(98)00017-8
McLaughlin KA (2016) Future directions in childhood adversity and youth psychopathology. J Clin Child Adolesc Psychol 45:361–382. https://doi.org/10.1080/15374416.2015.1110823
Magruder KM, Laughlin KA, Elmore Borbon DL (2017) Trauma is a public health issue. Eur J Psychotraumatol 8:1375338. https://doi.org/10.1080/20008198.2017.1375338
Randell KA, O’Malley D, Dowd MD (2015) Association of parental adverse childhood experiences and current child adversity. JAMA Pediatr 169:786–787. https://doi.org/10.1001/jamapediatrics.2015.0269
Dekel R, Goldblatt H (2008) Is there intergenerational transmission of trauma? The case of combat veterans’ children. Am J Orthopsychiatry 78:281–289. https://doi.org/10.1037/a0013955
Lambert JE, Holzer J, Hasbun A (2014) Association between parents’ PTSD severity and children’s psychological distress: a meta-analysis. J Trauma Stress 27:9–17. https://doi.org/10.1002/jts.21891
Yehuda R, Halligan SL, Grossman R (2001) Childhood trauma and risk for PTSD: relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Dev Psychopathol 13:733–753. https://doi.org/10.1017/S0954579401003170
van Ee E, Kleber RJ, Jongmans MJ, Mooren TTM, Out D (2016) Parental PTSD, adverse parenting and child attachment in a refugee sample. Attach Hum Dev 18:273–291. https://doi.org/10.1080/14616734.2016.1148748
Laurent J, Ettelson R (2001) An examination of the tripartite model of anxiety and depression and its application to youth. Clin Child Fam Psychol Rev 4:209–230. https://doi.org/10.1023/a:1017547014504
Lunkenheimer ES, Olson SL, Hollenstein T, Sameroff AJ, Winter C (2011) Dyadic flexibility and positive affect in parent–child coregulation and the development of child behavior problems. Dev Psychopathol 23:577–591. https://doi.org/10.1017/S095457941100006X
Fonagy P, Gergely G, Jurist E, Target M (2002) Affect regulation, mentalization, and the development of the self, Other Press
Chemtob CM, Nomura Y, Rajendran K, Yehuda R, Schwartz D, Abramovitz R (2010) Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children’s behavior: impact of PTSD and depression. Child Dev 81:1129–1141. https://doi.org/10.1111/j.1467-8624.2010.01458.x
Samuelson KW, Wilson CK, Padrón E, Lee S, Gavron L (2017) Maternal PTSD and children’s adjustment: parenting stress and emotional availability as proposed mediators: maternal PTSD and children’s adjustment. J Clin Psychol 73:693–706. https://doi.org/10.1002/jclp.22369
van Veen T, Wardenaar KJ, Carlier IVE, Spinhoven P, Penninx BWJH, Zitman FG (2013) Are childhood and adult life adversities differentially associated with specific symptom dimensions of depression and anxiety? Testing the tripartite model. J Affect Disord 146:238–245. https://doi.org/10.1016/j.jad.2012.09.011
Jacobvitz D, Leon K, Hazen N (2006) Does expectant mothers’ unresolved trauma predict frightened/frightening maternal behavior? Risk and protective factors. Dev Psychopathol. https://doi.org/10.1017/S0954579406060196
Hesse E, Main M (2000) Disorganized infant, child, and adult attachment: collapse in behavioral and attentional strategies. J Am Psychoanal Assoc 48:1097–1127. https://doi.org/10.1177/00030651000480041101
Schwerdtfeger KL, Goff BSN (2007) Intergenerational transmission of trauma: exploring mother–infant prenatal attachment. J Trauma Stress 20:39–51. https://doi.org/10.1002/jts.20179
Cicchetti D, Rogosch FA (1996) Equifinality and multifinality in developmental psychopathology. Dev Psychopathol 8:597–600. https://doi.org/10.1017/S0954579400007318
Deater-Deckard K (1998) Parenting stress and child adjustment: some old hypotheses and new questions. Clin Psychol Sci Pract 5:314–332. https://doi.org/10.1111/j.1468-2850.1998.tb00152.x
Ritchie KL, Holden GW (1998) Parenting stress in low income battered and community women: effects on parenting behavior. Early Educ Dev 9:97–112. https://doi.org/10.1207/s15566935eed0901_5
Qi CH, Kaiser AP (2003) Behavior problems of preschool children from low-income families: review of the literature. Topics Early Child Spec Educ 23:188–216. https://doi.org/10.1177/02711214030230040201
McKeever VM, Huff ME (2003) A diathesis-stress model of posttraumatic stress disorder: ecological, biological, and residual stress pathways. Rev General Psychol 7:237–250. https://doi.org/10.1037/1089-2680.7.3.237
Zuckerman M (1999) Vulnerability to psychopathology: a biosocial model. Am Psychol Assoc, Wash. https://doi.org/10.1037/10316-000
Raffaelli M, Crockett LJ, Shen Y-L (2005) Developmental stability and change in self-regulation from childhood to adolescence. J Genetic Psychol 166:54–76. https://doi.org/10.3200/GNTP.166.1.54-76
Costello EJ, Copeland W, Angold A (2011) Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Trends in psychopathology across the adolescent years. J Child Psychol Psychiatry 52:1015–1025. https://doi.org/10.1111/j.1469-7610.2011.02446.x
Hankin BL, Young JF, Abela JRZ, Smolen A, Jenness JL, Gulley LD, Technow JR, Gottlieb AB, Cohen JR, Oppenheimer CW (2015) Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. J Abnorm Psychol 124:803–816. https://doi.org/10.1037/abn0000089
Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, Burns K (2000) Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess 12:210–224. https://doi.org/10.1037/1040-3590.12.2.210
Abidin RR (1995) Parenting stress index, third edition: professional manual. Psychological Assessment Resources Inc, Odessa
March JS, Parker JDA, Sullivan K, Stallings P, Conners CK (1997) The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 36:554–565. https://doi.org/10.1097/00004583-199704000-00019
Baldwin JS, Dadds MR (2007) Reliability and validity of parent and child versions of the multidimensional anxiety scale for children in community samples. J Am Acad Child Adolesc Psychiatry 46:252–260. https://doi.org/10.1097/01.chi.0000246065.93200.a1
Kovacs M (1992) The Children’s Depression Inventory (CDI) manual. Multi-Health Systems, New York
Saylor CF, Finch AJ, Spirito A, Bennett B (1984) The Children’s Depression Inventory: a systematic evaluation of psychometric properties. J Consult Clin Psychol 52:955–967. https://doi.org/10.1037/0022-006X.52.6.955
Hayes AF (2009) Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr 76:408–420. https://doi.org/10.1080/03637750903310360
von Hippel PT, Bartlett JW (2019) Maximum likelihood multiple imputation: faster imputations and consistent standard errors without posterior draws. Statist Sci 38.
Molina AP, Negriff S, Monro W, Mennen FE (2018) Exploring the relationships between maternal mental health symptoms and young children’s functioning in a low-income, Minority Sample. J Child Fam Stud 27:3975–3985. https://doi.org/10.1007/s10826-018-1225-y
Hoven CW, Duarte CS, Lucas CP, Wu P, Mandell DJ, Goodwin RD, Cohen M, Balaban V, Woodruff BA, Bin F, Musa GJ, Mei L, Cantor PA, Aber JL, Cohen P, Susser E (2005) Psychopathology among New York City Public school children 6 months after September 11. Arch Gen Psychiatry 62:545. https://doi.org/10.1001/archpsyc.62.5.545
Kim HK, Pears KC, Capaldi DM, Owen LD (2009) Emotion dysregulation in the intergenerational transmission of romantic relationship conflict. J Fam Psychol 23:585–595. https://doi.org/10.1037/a0015935
Wood JJ (2006) Parental intrusiveness and children’s separation anxiety in a clinical sample. Child Psychiatry Hum Dev 37:73–87. https://doi.org/10.1007/s10578-006-0021-x
Lyons-Ruth K, Block D (1996) The disturbed caregiving system: relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Ment Health J 17:257–275. https://doi.org/10.1002/(SICI)1097-0355(199623)17:3%3c257::AID-IMHJ5%3e3.0.CO;2-L
Moehler E, Biringen Z, Poustka L (2007) Emotional availability in a sample of mothers with a history of abuse. Am J Orthopsychiatry 77:624–628. https://doi.org/10.1037/0002-9432.77.4.624
Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, Bentley KH, Thompson-Hollands J, Conklin LR, Boswell JF, Ametaj A, Carl JR, Boettcher HT, Cassiello-Robbins C (2017) The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: a randomized clinical trial. JAMA Psychiatry 74:875. https://doi.org/10.1001/jamapsychiatry.2017.2164
Caspi A, Moffitt TE (2018) All for one and one for all: mental disorders in one dimension. Am J Psychiatry 175:831–844. https://doi.org/10.1176/appi.ajp.2018.17121383
Cole DA, Peeke LG, Martin JM, Truglio R, Seroczynski AD (1998) A longitudinal look at the relation between depression and anxiety in children and adolescents. J Consult Clin Psychol 66:451–460. https://doi.org/10.1037/0022-006X.66.3.451
Thompson RA (2001) Childhood anxiety disorders from the perspective of emotion regulation and attachment. In: Vasey MW, Dadds MR (eds) The developmental psychopathology of anxiety. Oxford University Press, Oxford, pp 160–182. https://doi.org/10.1093/med:psych/9780195123630.003.0008
Reitman D, Currier RO, Stickle TR (2002) A critical evaluation of the Parenting Stress Index-Short Form (PSI-SF) in a Head Start Population. J Clin Child Adolesc Psychol 31:384–392. https://doi.org/10.1207/153744202760082649
Morris AS, Robinson LR, Hays-Grudo J, Claussen AH, Hartwig SA, Treat AE (2017) Targeting parenting in early childhood: a public health approach to improve outcomes for children living in poverty. Child Dev 88:388–397. https://doi.org/10.1111/cdev.12743
Lupien SJ, McEwen BS, Gunnar MR, Heim C (2009) Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci 10:434–445. https://doi.org/10.1038/nrn2639
Wahler RG, Dumas JE (1989) Attentional problems in dysfunctional mother-child interactions: an interbehavioral model. Psychol Bull 105:116–130. https://doi.org/10.1037/0033-2909.105.1.116
Ammerman RT, Putnam FW, Chard KM, Stevens J, Van Ginkel JB (2012) PTSD in depressed mothers in home visitation. Psychol Trauma Theory Res Prac Policy 4:186–195. https://doi.org/10.1037/a0023062
Gardner F, Hutchings J, Bywater T, Whitaker C (2010) Who benefits and how does it work? Moderators and mediators of outcome in an effectiveness trial of a parenting intervention. J Clin Child Adolesc Psychol 39:568–580. https://doi.org/10.1080/15374416.2010.486315
Acknowledgements
The researchers would like to acknowledge the families who participated in this investigation as well as the research team from the Pomona CARE Lab who carried out the project.
Funding
This research was supported by a start-up grant awarded to the last author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cho, B., Woods-Jaeger, B. & Borelli, J.L. Parenting Stress Moderates the Relation between Parental Trauma Exposure and Child Anxiety Symptoms. Child Psychiatry Hum Dev 52, 1050–1059 (2021). https://doi.org/10.1007/s10578-020-01087-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-020-01087-1