Abstract
Panic disorder (PD) can result in significant functional impairment. Studies of cognitive behavioral therapy (CBT) for PD have demonstrated response rates ranging between 38 and 65%. d-cycloserine (DCS), a partial NMDA agonist, may enhance the effects of exposure-based therapy for PD in adults; however, no studies have examined its effect in adolescents with PD. This study examined the feasibility and acceptability of the use of DCS to augment intensive CBT for PD in adolescents. Twenty-four adolescents (ages 12–17) participated in this randomized, double-blinded, placebo-controlled trial, to compare CBT + DCS to CBT + placebo. The results demonstrated the feasibility and acceptability of the treatment to participants. No significant differences were found between the two groups, but both groups showed significant improvement. This is the first investigation of DCS in the treatment of PD in adolescents and it provides initial support for a more extensive study of DCS augmentation of CBT among adolescents with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Panic disorder (PD) is a distressing and debilitating set of symptoms that can result in significant functional impairment over time. Evidence demonstrates that the initial peak age for onset of PD is adolescence (e.g., Ref. [1]), with lifetime prevalence rates ranging from 1 to 5% in community samples (e.g., Ref. [2]) and as high as 28% in emergency room settings [3]. PD in adolescents is associated with increased economic costs for both adults and adolescents [4] as well as multiple additional behavioral and emotional problems such as depression and substance use problems [5, 6]. The symptoms of PD in adolescence typically lead to severe impairment in functioning, mostly by means of avoidance of developmentally important activities in school or with peers, and interference with relationships with friends and family members. If left untreated, these symptoms may take a chronic course throughout adulthood [7, 8].
Evidence suggests that cognitive behavioral therapy (CBT) for PD is associated with significant reductions in symptoms among adults [9,10,11] and adolescents [12]. Studies evaluating CBT for specific treatment of PD have demonstrated response rates ranging between 38 and 65% [13,14,15]. A recent development in CBT for PD in adolescents has been the development of an intensive treatment that is delivered to youth over the course of 8 days (see [16] for the description of the protocol). This intensive treatment program involves teaching youth core CBT skills, including psychoeducation about anxiety, cognitive restructuring, interoceptive exposure to frightening physical sensations of panic, and massed situational exposures with therapist coaching. A recently completed study compared youth who were randomly assigned to one of three different study conditions: (1) a waitlist condition, (2) intensive panic treatment with a parent component and (3) intensive panic treatment without a parent component. Results of this trial are described in detail elsewhere [16,17,18,19,20]; youth in both of the treatment conditions evidenced significant improvement in symptoms of panic over the 8 day period, with approximately 72% of youth displaying non-clinical levels of panic at the 3 month follow up assessment. Youth in the waitlist condition did not show any significant change from pre-treatment to post-treatment. This trial was the first randomized trial of intensive treatment for panic disorder in adolescents and indicated that this treatment has the potential to help youth return to healthier functioning after a course of brief CBT. However, further work is necessary to understand how to bolster treatment for non-responders and ensure maintenance of gains over time. Finding ways to maximize the effectiveness of exposures and potentially increase the rate of change through treatment are also important. With this in mind, examination of efficacious agents that may augment the effectiveness of existing treatments is warranted.
One such agent that has shown promise in potential augmentation of treatments for anxiety disorders is d-Cycloserine (DCS), a partial N-methyl-d-aspartate-agonist (NMDA) [21]. The NMDA receptor is involved in fear extinction, e.g., Ref. [22], and DCS aids the extinction of learned fear. Extinction of fear is one of the main objectives of CBT for anxiety disorders, which is accomplished through exposure to the feared object, situation, thought, or physical symptom. To date, DCS has been used in a number of clinical trials of treatment of anxiety disorders in adults, demonstrating small to moderate treatment effects [22, 23].
Two studies to date have examined the effects of DCS for enhancing CBT for panic disorder (PD) in adults [24, 25]. Otto et al. [24] demonstrated that DCS enhances the response to treatment initially. Siegmund et al. [25] reported that while DCS does not enhance the effects of CBT, it accelerates the response to treatment. While the exact mechanism of action of DCS is unclear, some evidence suggests that it facilitates learning-related synaptic plasticity (e.g., Ref. [26]), enhancing both amygdala- and hippocampus-dependent learning. DCS can potentially increase the speed of learning from exposures and subsequently decrease the duration of treatment. Decreased duration in turn may decrease the treatment dropout rates.
Despite its potential benefits, only a handful of studies have examined DCS augmentation of CBT in children and adolescents, producing mixed findings. Storch et al. [27] examined the effects of DCS in the treatment of obsessive compulsive disorder in 30 youth 8–18 years of age, reporting no difference between placebo and DCS. In a pilot study of 17 youth with difficult-to-treat OCD, Farrell et al. [28] found the DCS group demonstrated greater gains at 1 month follow-up than the placebo group. Scheeringa and Weems [29] randomized 57 youth with posttraumatic stress disorder ages 8–17 to CBT + DCS or CBT + placebo, finding evidence for increased speed of recovery in the DCS group. Byrne et al. [30] conducted a randomized controlled trial among 35 children ages 6–14 with dog or spider phobia, randomly assigned to DC or placebo condition, demonstrating improved extinction learning and increased generalization of the fear extinction to other contexts. Additional research is needed to examine the utility of DCS to augment treatment of pediatric anxiety disorders.
No studies to date have examined the effects of DCS augmentation on CBT for PD in youth. However, adolescence is a population of increased interest for several reasons. First of all, as previously mentioned, the peak age of onset of PD is adolescence, and if left untreated, PD may take a chronic course throughout adulthood. Second, adolescence is a period of increased neuroplasticity, as during this time the neuronal circuitry of the brain continues to develop, making the brain more susceptible to change from experiential learning [31]. This suggests that if fear-related learning is targeted in this age group, it may lead to greater and more enduring improvement. For adolescents with PD, the novel strategy of combining intensive exposure-based CBT and DCS provides for a promising treatment, which may potentially lead to faster recovery.
This is the first study to investigate the use of DCS in a brief, intensive intervention for adolescents with PD in an effort to capitalize on increased neuroplasticity during this developmental period. The main goal of this pilot study was to evaluate the feasibility and acceptability of using DCS in youth in conjunction with intensive CBT for PD, including feasibility of recruitment, randomization, blinded assessment and assignment to DCS versus placebo condition, as well as acceptability of the treatment, including parent’s perception of acceptability of the DCS component of the treatment.
Methods
Participants
The sample included 24 adolescents, ranging in age from 12 to 17 years (M = 14.5; SD = 1.77) and their parents. Given the pilot nature of this study, it was determined that 24 participants and their parents would afford sufficient evaluation of protocol feasibility and acceptability, setting the stage for a subsequent large-scale RCT to evaluate efficacy. Participants were excluded if they: (a) had a diagnosis of schizophrenia, pervasive developmental disorder, bipolar I or II disorder, organic brain syndrome, and conduct disorder, or current suicidal ideation; or (b) had a change in their psychiatric medication regimen within 4 weeks of the start of the treatment.
The majority of the sample was identified as Non-Hispanic White (95.8%), and the remainder was identified as African American. In the sample, 41.7% were males, and 58.3% were females. Ten out of 24 participants (41.2%) were on a stable dose of serotonin reuptake inhibitors. Three (12.5%) out of 24 participants reported an income level of below $44,000, i.e., 200% above the established federal poverty guidelines for a household of four people.
All participants had a principal diagnosis of DSM-IV Panic Disorder with Agoraphobia (PDA) with a clinical severity rating (CSR) of four or above (M = 5.38; SD = 0.71) as established based on the report from both parents and adolescents. The most common comorbid diagnosis in the sample was specific phobia (N = 9; 37.5%), and 6 out of 9 had a specific phobia of vomiting. Additionally, 16.7% met the criteria for generalized anxiety disorder, 12.5% met the criteria for separation anxiety disorder, 8.3% met the criteria for social anxiety disorder, 8.3% for major depressive disorder, 4.2% for depressive disorder, not otherwise specified and 4.2% for oppositional-defiant disorder.
Procedures
The study procedures were reviewed and approved by the Institutional Review Board of the university where the study was conducted. The majority of the families were recruited from the wait list at a university based specialty clinic in New England. Additional families learned about the study from an advertisement on the clinic website. Following the initial contact, the families underwent a preliminary phone screen. If they met the inclusion/exclusion criteria on the screen, they were invited for an in-person diagnostic assessment with trained clinicians (for out-of-state families, the assessment was conducted over the telephone). Prior to the assessment, the families signed parental consent and child assent. The assessment included the Anxiety Disorders Interview Schedule for the DSM-IV-Child version, Child and Parent report forms (ADIS-IV-C/P) as well as additional study questionnaires. Additionally, the medical history was collected and reviewed by a study physician to screen for medical conditions that would be counter-indicative to the use of DCS. The assessments were conducted at baseline, posttreatment, and at 3-month follow-up by trained independent evaluators, who were doctoral students in clinical psychology at the university where the study was conducted. These evaluators were also trained to reliability in administration of the ADIS-IV-C/P. Participants were offered monetary compensation for the posttreatment and the follow-up assessments.
All adolescents who met the inclusion criteria were randomized into either the DCS or placebo group. The treatment consisted of six 2–6 h long sessions and 2 days of independent practice. The participants received 50 mg of DCS or 50 mg of placebo pill identical in appearance on all 3 days of their exposure-based therapy sessions (days 3–5), 1 h prior to the start of the exposure. All treatment was conducted by the principal investigator of the study, a licensed psychologist with extensive experience with the treatment protocol. Both the evaluators and the study therapist were blind to the treatment condition.
Treatment Program
The intensive treatment protocol for PD in adolescents described earlier [16] was used in the study. The treatment entailed 8 days of CBT (2–6 h of treatment each day) and included the following skills: psychoeducation, cognitive restructuring, interoceptive exposures, in-vivo exposures (with the therapist on days 4 and 5 and independently on days 6 and 7), and relapse prevention. Each session also included a 30-min-long parent component at the end, where the therapist introduced the parents to the skills learned in session and to parenting techniques intended to help manage their child’s anxiety.
Measures
Measures used in this study were a combination of clinician-rated, parent-report, and self-report. The most psychometrically sound measures for each construct were carefully selected. Table 1 presents the Cronbach’s Alpha values for the self-report measures. Following guidelines by George and Mallery [32], internal consistency values were considered acceptable if Cronbach’s alpha was ≥ 0.70.
Anxiety Disorders Interview Schedule for the DSM-IV-Child and Parent Versions (ADIS-IV-C/P [33])
The ADIS-C/P a structured interview designed to diagnose anxiety disorders of childhood and adolescence. It is based on DSM-IV criteria and is used both to determine the diagnosis and its severity. It allows for differential diagnoses among all the DSM-IV anxiety and related disorders and provides data regarding symptomatology of the disorder. In addition to anxiety disorders, the ADIS assesses for related conditions, including depressive disorders. For each diagnosis, a clinical severity rating (CSR) is assigned, ranging from 0 (none) to 8 (very severe), based on the degree of impairment and distress of the disorder. A CSR level of 4 or above is indicative of a clinical level of impairment.
Panic Disorder Severity Scale (PDSS [34, 35])
The PDSS is a seven-item self-report scale that assesses panic disorder symptomatology (panic frequency, distress, anticipatory anxiety, panic-related avoidance of situations and sensations), and impairment associated with the disorder. The reliability and validity of the PDSS have been established [35]. A parallel seven-item child version of the PDSS was used (PDSS-C) in which reference to work has been replaced by one to school. The PDSS-C has been shown to have strong psychometric properties [36]. In addition to pre-, post-, and 3-month evaluation, the PDSS-C was administered at each visit.
Panic and Phobia Questionnaire (PPQ [37])
The PPQ is a 27-item self-report scale consisting of three factor-analytically distinct subscales that assess fear and avoidance of agoraphobic situations, social situations, and situations and activities that produce bodily sensations commonly feared by individuals with panic disorder (interoceptive fear). The three subscales have good internal consistency, test–retest reliability, and construct validity. In addition to pre-, post-, and 3-month evaluation, the PPQ was administered at each visit.
Subjective Symptoms Scale (SSS-C)
The SSS-C is a modification of a self-report scale introduced by Hafner and Marks [38], consisting of ratings of the extent to which anxiety symptoms interfere with five areas of daily functioning. These areas have been modified slightly to be developmentally appropriate for adolescents. They are: school, home management, private leisure, social leisure, and family relationships. The SSS for Adults has been used in several large NIMH-funded studies, including several multicenter panic studies. The SSS was administered at pre-, post-, and 3-month evaluation.
Childhood Anxiety Sensitivity Index (CASI [39])
The CASI is an 18-item self-report scale modified from the Anxiety Sensitivity Index [40]. The CASI solicits ratings of how aversely youth view anxiety symptoms. The CASI has been reported to have good psychometric properties in both clinical and nonclinical samples [39, 41,42,43]. The CASI was administered at pre-, post-, and 3-month evaluation.
Clinical Global Impression-Improvement (CGI-Improvement [44])
The CGI is a one item measure of diagnostic improvement, which is rated by the clinician. The scale ranges from 1 (very much improved) to 7 (very much worse). It was rated at post-treatment and at 3-month follow-up.
Perceptions of Treatment Questionnaire-Adolescent Version (POTQ-A [45])
The POTQ-A is a self-report instrument that was developed for use in treatment studies at the university in which this study was conducted. It assesses the acceptability of treatment, its helpful and unhelpful aspects, as well as satisfaction with treatment on a 0–8 scale. It was administered at post-treatment as well as 3-month-follow up in order to assess whether the treatment was perceived differently between the DCS and the placebo group.
Statistical Approach
Data were entered in SPSS version 20. T tests and Chi square tests were utilized to examine the pre-treatment differences between the two groups. The treatment effects were examined using mixed-factor general linear models where time was entered as the repeated measure. Additionally, the differences in the rate of improvement between the two groups were compared using mixed linear modeling in R.
Results
Feasibility
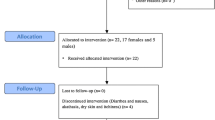
The recruitment flow chart is presented in Fig. 1. The recruitment efforts were carried out for approximately 21 months. Four potential participants were screened per month, out of which two were asked to complete the diagnostic assessment. Approximately two participants enrolled in the study each month. Out of the 24 participants enrolled, two did not complete the treatment, suggesting a retention rate of 91.6%. All the participants, who completed the treatment, completed their post-treatment and 3-month questionnaires. The participants and their families adhered to the treatment protocol, including taking a pregnancy test for females who have entered puberty prior to starting the DCS phase of the study and taking the DCS or placebo pill an hour prior to the start of exposures. No parent reported reservations about the DCS component of the study.
Power Analysis
Although this was a pilot study with a primary goal of establishing feasibility, a power analysis was conducted to determine the likelihood of showing meaningful differences by means of a mixed model repeated measures ANOVA with two conditions. The power analysis, assuming a medium effect size (alpha ≤ 0.05 and beta ≥ 0.8) found that a sample of 34 participants is sufficient to detect stable and reliable findings. Assuming a medium effect size, power for the current sample size is 0.69.
Adverse Effects
None of the participants reported adverse side effects following the administration of the medication.
Pre-treatment Differences
No pre-treatment differences were found between the DCS and placebo groups on the CSR of the PDA diagnosis, PDSS, PPQ, CASI, SSS, or the number of comorbid diagnosis (Table 2). No differences were found in gender and income distribution between the two groups. No difference was found in the number of the SSRI prescriptions between the two groups.
Post-treatment
Twenty-two of the 24 participants completed the treatment, and the post-treatment data were available for all the treatment completers. Treatment response was examined in several ways. When the CSR level of ADIS-C/P was used as the recovery criterion (CSR < 4), 66.7% (8 out of 12) of the DCS group and 90% (9 out of 10) of the placebo group no longer carried their diagnosis of PD at the end of the treatment. There was no significant difference between the two treatment groups in the recovery rate at post-treatment (Fisher exact test, p = 0.323).
Treatment response was also measured by evaluating CGI-I scores; responders were characterized as having been much improved (CGI-I score of “2”) or very much improved (CGI-I score of “1”). Response rates were similar to diagnosis-specific recovery rates described above; 75% of individuals (9 out of 12) in the DCS group were CGI-I responders whereas 90% of individuals (9 out of 10) in the placebo group were CGI-I responders. Only one person in each group was characterized as not improved (“no change or worsened”).
A mixed model repeated measures ANOVA with treatment condition (DCS and placebo) as a between-subject factor and time (pre- and post-treatment) as a within-subject factor was conducted to assess treatment outcome using the treatment outcome measures (CSR, PDSS, CASI, PPQ, SSS) as well as the total number of comorbid diagnoses. The descriptive statistics for outcome measures are presented in Table 2.
Significant effects were found for time on all the primary outcome measures: CSR [F (1, 20) = 63.99, p < 0.001]; PDSS [F (1, 20) = 19.08, p < 0.001], CASI [F (1, 20) = 13.51, p < 0.001], APPQ [F (1, 20) = 15.52, p = 0.001], SSS [F (1, 20) = 18.73, p < 0.001], and number of diagnoses [F (1, 20) = 43.04, p < 0.001]. The effect sizes were large, Cohen’s d ranging from 1.64 to 3.58. However, no significant effects were found for the interaction of time and treatment condition for any of these measures. Overall, the participants were satisfied with the treatment, as reported in POTQ-A. On a specific item asking how much the treatment helped them cope with anxiety on a scale ranging from 0 (not at all) to 8 (very much), 46% of the sample reported “8” and another 16% reported “7”. Independent t test was conducted to compare the POTQ-A scores at post-treatment between the two groups, not detecting any significant differences.
3-Month Follow Up
The data were collected from all 22 treatment completers. Using the CSR level of ADIS-C/P as the recovery criterion (CSR < 4), 10 out of 12 participants (83.3%) in the DCS group and 9 out of 10 participants (90%) in the placebo group no longer carried their diagnosis of PD at the 3-month follow up. There was no significant difference between the two groups in the recovery rate at 3-month follow up (Fisher exact test, p = 1.0). However, two additional participants in the DCS group demonstrated improvement after the completion of the treatment. The examination of the CGI scores demonstrated that 75% of individuals (9 out of 12) in the DCS group were CGI-I responders whereas 80% of individuals (8 out of 10) in the placebo group were CGI-I responders.
A mixed model repeated measures ANOVA with treatment condition (DCS and placebo) as a between-subject factor and time (pre- and 3-months follow up) as a within-subject factor was conducted to assess treatment outcome using the treatment outcome measures (CSR, PDSS, CASI, PPQ, SSS) as well as the total number of comorbid diagnoses. Significant effects were found for time on all the primary outcome measures: CSR [F (1, 20) = 86.92, p < 0.001]; PDSS [F (1, 20) = 36.06, p < 0.001], CASI [F (1, 20) = 31.42, p < 0.001], APPQ [F (1, 20) = 25.96, p < 0.001], SSS [F (1, 20) = 18.73, p < 0.001], and number of diagnoses [F (1, 20) = 44.48, p < 0.001]. The effect sizes were large, Cohen’s d ranging from 1.92 to 3. Additionally, a significant effect was found for the interaction of treatment condition and time for PDSS (F = 4.51, p = 0.046; Cohen’s d = 0.8), suggesting that the placebo group had more significant reduction at 3 months than the DCS group.
Overall, the participants continued to be satisfied with the treatment at the 3-month follow-up, as reported in POTQ-A. On a specific item asking how much the treatment helped them cope with anxiety on a scale ranging from 0 (not at all) to 8 (very much), 32% of the sample reported “8” and another 32% reported “7”. Independent t-test was conducted to compare the POTQ-A scores between the two groups, not detecting any significant differences.
Speed of Improvement
To investigate the speed of improvement, we fit a linear mixed effects model with random intercept and slopes. We created two categories for the time: sessions 1–2 (before the introduction of DCS/placebo) and sessions 3–6 (after the introduction of DCS/placebo). We fit a model that incorporated the treatment group as the class variable, subject level as the random intercept, and a random group-by-time interaction term to examine whether the difference in the slopes between the two treatment groups in the first part of treatment was significantly different from the difference in the slopes between the two treatment groups in the second part of treatment. These models were examined for two separate dependent variables: panic symptomatology as measured by PDSS (Fig. 2) and situational avoidance as measured by APPQ (Fig. 3), both collected daily throughout the treatment. No differences were found in the speed of improvement between the two groups on either measure.
Treatment Responders
There were no significant differences between post-treatment treatment responders and non-responders when evaluating baseline symptom differences collapsed across treatment condition on the PDSS, t(20) = 0.093, p = 0.927; CASI, t(20) = 0.936, p = 0.360; SSS, t(20) = − 1.556, p = 0.135; and the APPQ, t(20) = 0.389, p = 0.701. When evaluating treatment response at 3-month follow-up, there were again no significant differences between treatment responders and non-responders when evaluating baseline symptom differences collapsed across treatment condition on the PDSS, t(20) = 0.637, p = 0.824; CASI, t(20) = 1.235, p = 0.231; SSS, t(20) = − 1.059, p = 0.302; and the APPQ, t(20) = 0.701, p = 0.492.
Discussion
This was the first study to examine the acceptability and feasibility of the use of DCS in conjunction with intensive CBT for PD in adolescents. The study explored the potential effects of DCS on the efficacy of the intensive treatment of PD in adolescents in comparison to placebo at post-treatment and 3 months after the completion of the treatment. The results demonstrate that the study of the effects of DCS on the intensive CBT treatment of PD in adolescents is feasible to conduct and DCS is acceptable to participants and families. The recruitment goals were met, and the study procedures were carried out as intended. No adverse effects were reported at the 50 mg dose, and no families reported unwillingness to participate in the treatment because of the administration of DCS. The attrition rates were 8.3%. The participants overall were satisfied with the treatment, reporting it to be helpful.
Both placebo and DCS groups benefited significantly from the treatment, demonstrating once again that the intensive treatment for PD in adolescents is potentially highly effective. Overall, 77% of all participants no longer had a PD diagnosis at post treatment and 86% did not have a PD diagnosis at 3-month follow-up. Three additional participants in the DCS group no longer met the criteria for PD at 3 months in comparison to post treatment. This number was unchanged for the placebo group. However, this difference was not significant. Both groups showed significant improvement from pre to post-treatment and from pretreatment to 3-month follow-up. Interestingly, there was a significant interaction effect of treatment condition and time found at follow-up for PDSS, showing a greater decrease in the scores of the placebo group. However, these findings are difficult to interpret due to the small sample size.
The recovery rates in this study were slightly higher than those reported in the intensive study of PDA in adolescents (Pincus et al. in preparation). This may be due to the presence of the pill and the potential placebo effect from it. In fact, several participants anecdotally attributed their success to the pill (e.g., “I must be in the medicine group.”).
The post-treatment and 3-month follow-ups revealed that in both groups the number of comorbid conditions significantly decreased as a result of the intensive CBT for panic disorder. This was consistent with the previous study of intensive CBT for panic in adolescents [46]. The speed of recovery did not differ significantly between the two groups. No significant difference was found between the groups in first versus second part of treatment.
The lack of effect of DCS is consistent with some of the DCS studies with other psychiatric disorders (e.g., Ref. [27]), and there are several reasons that may explain it. First, it is possible that the lack of effect of DCS is due to the high degree of efficacy of CBT itself, which then results in ceiling effect for further enhancement [27]. Another reason for the lack of the effect of DCS may be that not only does DCS enhance fear extinction, but it also may enhance the fear-related memories (e.g., Ref. [47]). For example, Smits et al. [48] found that low subjective ratings of fear at the end of the exposure led to greater improvements in patients with acrophobia who were given DCS versus placebo. Similar findings were reported by Smits et al. [49] for individuals with social anxiety disorder. If this is the case, perhaps DCS should be administered following successful exposures only, in order to consolidate the learning that takes place following that exposure (e.g., Ref. [50]).
Some studies have considered the potential interaction of SSRIs with the NMDA receptor complex. In animal studies, Paul et al. [51] found that long-term exposure to all classes of antidepressant medication (including SSRIs) in mice leads to neurochemical changes in the NMDA receptor complex, which in turn will reduce the effects of DCS. On the contrary, in a meta-analysis of DCS studies, McGuire et al. [52] found that in anxiety disorder trials, a larger DCS effect was associated with a higher number of participants taking SSRIs. Mataix-Col et al. [53] reported no effects for SSRIs. In the present study, 42% of the participants were on a stable dose of an SSRI, but the small n did not allow for the investigation of the potential SSRI effects.
Conclusions
The present investigation demonstrates that the use of DCS in youth with PD is feasible and acceptable by the families and youth. It further confirms that intensive treatment for PD is highly effective, as demonstrated by the recovery rates for both DCS and placebo groups. Moreover, while PD was the focus of the treatment, the number of comorbid diagnoses not specifically addressed in the treatment decreased significantly at post treatment and at the 3-month follow-up for both groups, suggesting that the intensive treatment is potentially effective for a range of anxiety disorders.
Limitations
The study has certain limitations. While the small sample size was determined by the pilot nature of the study, it limited statistical power and thereby the opportunity to draw meaningful conclusions about the effects of DCS on treatment. Moreover, the sample size did not allow us to statistically examine the differences between treatment responders and non-responders as well as the response to DCS between the participants who were on a stable dose of SSRIs and the ones who were not. Additionally, because multiple exposures were conducted per day, we did not have a meaningful way of distinguishing successful and unsuccessful exposures in order to examine the differential effects of DCS. Finally, all the treatments were conducted by the same therapist (the PI of the study), which ensures treatment adherence, but at the same time it is not clear whether these results would generalize to other therapists.
Future Directions
There are several potential directions for future research stemming from this work. First, because we have found the use of DCS in intensive treatment of PD in adolescents feasible and acceptable, a larger scale RCT of cognitive enhancers for CBT in this population can be developed. A study with a larger sample would allow for detection of the effects of DCS not only on the treatment outcome but on the speed of recovery. A larger sample would also enable the investigators to look at the differences between responders and non-responders in order to tailor the treatment accordingly as well as to examine the role of SSRIs in moderating the effects of DCS. In such a study, a “no pill” group can be included to ensure that the improvement is not due to a placebo effect. Finally, a larger scale study would allow to examine the timing of the administration of DCS in order to maximize its effectiveness. One such study is under way now for adults with social anxiety disorder, with a goal of developing an optimal algorithm of DCS administration in CBT [54].
Another important direction for future research is the expansion of intensive CBT treatment for youth. In this study, all participants regardless of the treatment group demonstrated a significant decrease in the number of comorbid disorders (predominantly anxiety disorders) as the result of intensive CBT for panic disorder. This demonstrates the effectiveness of the intensive treatment model. It is imperative to develop an intensive CBT protocol for adolescents that will target all anxiety disorders in a developmentally appropriate manner. There are only a handful of intensive treatment protocols developed for youth (in addition to the one utilized in this study), including one for obsessive–compulsive disorder and one for specific phobia. No treatments have targeted the entire spectrum of often comorbid anxiety disorders in adolescents. The development of such protocols will likely increase patients’ access to treatment and provide more immediate relief for youth and their families.
Finally, while DCS has been the most empirically supported cognitive enhancer, there are several others that are being investigated with adults, including yohimbine, catecholamines, and methylene blue (see Ref. [54]). The research on these enhancers is in the beginning stages, but they may be worthy of exploration in adolescents as we strive to continue to improve the efficacy of CBT for anxiety disorders in youth.
Summary
Panic disorder is a distressing and debilitating set of symptoms that can result in significant functional impairment over time. The symptoms of PD in adolescence typically lead to severe impairment in functioning, mostly by means of avoidance of developmentally important activities in school or with peers, and interference with relationships with friends and family members. If left untreated, these symptoms may take a chronic course throughout adulthood.
Studies evaluating CBT for PD have demonstrated response rates ranging between 38 and 65%. Preliminary results have suggested that d-cycloserine (DCS), a partial NMDA agonist, may enhance the effects of exposure-based therapy for PD in adults; however, no studies have examined its effect in adolescents with PD.
The present study examined the feasibility and acceptability of the use of DCS in conjunction with intensive CBT for PD in adolescents. Twenty-four adolescents (ages 12–17) participated in this randomized, double-blinded, placebo-controlled trial, to compare CBT + DCS to CBT + placebo. Both groups received individual intensive CBT for PD, delivered over a course of 8 days, with DCS or placebo administered 1 h prior to the start of the exposures.
The results demonstrated that the study of the effects of DCS on the intensive CBT treatment of PD in adolescents is feasible to conduct and DCS is acceptable to participants and families. No adverse events were reported. The participants overall were satisfied with the treatment. No significant differences were found between the two groups on any of the outcome measures, but both groups showed significant improvement. This is the first investigation of DCS in the treatment of PD in adolescents and it provides initial support for a more extensive study of DCS augmentation of CBT among adolescents with PD.
References
Barlow DH (2001) Anxiety and its disorders: the nature and treatment of anxiety and panic. Guilford Press, New York
Merikangas KR, He J-P, Burstein M et al (2010) Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 49:980–989. https://doi.org/10.1016/j.jaac.2010.05.017
Lipsitz JD, Gur M, Sonnet FM et al (2010) Psychopathology and disability in children with unexplained chest pain presenting to the pediatric emergency department. Pediatr Emerg Care 26:830–836. https://doi.org/10.1097/PEC.0b013e3181fb0e23
Batelaan N, Smit F, Graaf R et al (2007) Economic costs of full-blown and subthreshold panic disorder. J Affect Disord 104:127–136. https://doi.org/10.1016/j.jad.2007.03.013
Ollendick T, Pincus D (2008) Panic disorder in adolescents. In: RG Steele, TD Elkin, M Roberts (eds) Handbook of evidence based therapies for children and adolescents. Springer, New York, pp 83–102
Mattis SG, Pincus DB (2003) Treatment of SAD and panic disorder in children and adolescents. In: PM Barrett, TH Ollendick (eds) Handbook of interventions that work with children and adolescents: prevention and treatment. Wiley, West Sussex, pp 145–169
Woodward LJ, Fergusson DM (2001) Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry 40:1086–1093. https://doi.org/10.1097/00004583-200109000-00018
Bittner A, Egger HL, Erkanli A et al (2007) What do childhood anxiety disorders predict? J Child Psychol Psychiatry Allied Discip 48:1174–1183. https://doi.org/10.1111/j.1469-7610.2007.01812.x
Gloster AT, Hauke C, Höfler M et al (2013) Long-term stability of cognitive behavioral therapy effects for panic disorder with agoraphobia: a two-year follow-up study. Behav Res Ther 51:830–839. https://doi.org/10.1016/j.brat.2013.09.009
Hendriks G-J, Kampman M, Keijsers GPJ et al (2014) Cognitive-behavioral therapy for panic disorder with agoraphobia in older people: a comparison with younger patients. Depress Anxiety 31:669–677
Roshanaei-Moghaddam B, Pauly MC, Atkins DC et al (2011) Relative effects of CBT and pharmacotherapy in depression versus anxiety: is medication somewhat better for depression, and CBT somewhat better for anxiety?. Depress Anxiety 28:560–567
Pincus DB, May JE, Whitton SW et al (2010) Cognitive-behavioral treatment of panic disorder in adolescence. J Clin Child Adolesc Psychol 39:638–649. https://doi.org/10.1080/15374416.2010.501288
Barlow DH, Gorman JM, Shear MK, Woods SW (2000) Cognitive-behavioral therapy, imipramine, or their combination for panic disorder. JAMA 283:2529. https://doi.org/10.1001/jama.283.19.2529
Craske MG, Maidenberg E, Bystritsky A (1995) Brief cognitive-behavioral versus nondirective therapy for panic disorder. J Behav Ther Exp Psychiatry 26:113–120. https://doi.org/10.1016/0005-7916(95)00003-I
Milrod B, Chambless DL, Gallop R et al (2016) Psychotherapies for panic disorder: a tale of two sites. J Clin Psychiatry 77:927–935. https://doi.org/10.4088/JCP.14m09507
Angelosante AG, Pincus DB, Whitton SW et al (2009) Implementation of an intensive treatment protocol for adolescents with panic disorder and agoraphobia. Cogn Behav Pract 16:345–357. https://doi.org/10.1016/j.cbpra.2009.03.002
Elkins RM, Gallo KP, Pincus DB, Comer JS (2016) Moderators of intensive CBT for adolescent panic disorder: the role of fear and avoidance. Child Adolesc Ment Health 21:30–36. https://doi.org/10.1111/camh.12122
Gallo KP, Cooper-Vince CE, Hardway CL et al (2014) Trajectories of change across outcomes in intensive treatment for adolescent panic disorder and agoraphobia. J Clin Child Adolesc Psychol 43:742–750. https://doi.org/10.1080/15374416.2013.794701
Hardway CL, Pincus DB, Gallo KP, Comer JS (2015) Parental involvement in intensive treatment for adolescent panic disorder and its impact on depression. J Child Fam Stud 24:3306–3317. https://doi.org/10.1007/s10826-015-0133-7
Pincus DB, Elkins RM, Hardway C (2014) Intensive treatments for adolescent panic disorder and agoraphobia: helping youth move beyond avoidance. Psychopathol Rev 1:189–194
Hofmann SG, Otto MW, Pollack MH, Smits JA (2012) D-Cycloserine as an augmentation strategy for cognitive behavioral therapy for anxiety disorders: an update. Curr Psychiatry Rep 18:5659–5662. https://doi.org/10.2174/138161212803530916
Norberg MM, Krystal JH, Tolin DF (2008) A meta-analysis of D-cycloserine and the facilitation of fear extinction and exposure therapy. Biol Psychiatry 63:1118–1126
Rodrigues H, Figueira I, Lopes A et al (2014) Does d-cycloserine enhance exposure therapy for anxiety disorders in humans? A meta-analysis. PLoS ONE 9:e93519
Otto MW, Tolin DF, Simon NM et al (2010) Efficacy of D-cycloserine for enhancing response to cognitive-behavior therapy for panic disorder. Biol Psychiatry 67:365–370. https://doi.org/10.1016/j.biopsych.2009.07.036
Siegmund A, Golfels F, Finck C et al (2011) D-Cycloserine does not improve but might slightly speed up the outcome of in-vivo exposure therapy in patients with severe agoraphobia and panic disorder in a randomized double blind clinical trial. J Psychiatr Res 45:1042–1047. https://doi.org/10.1016/j.jpsychires.2011.01.020
Onur OA, Schlaepfer TE, Kukolja J et al (2010) The N-methyl-D-aspartate receptor co-agonist D-cycloserine facilitates declarative learning and hippocampal activity in humans. Biol Psychiatry 67:1205–1211. https://doi.org/10.1016/j.biopsych.2010.01.022
Storch EA, Murphy TK, Goodman WK et al (2010) A preliminary study of D-cycloserine augmentation of cognitive-behavioral therapy in pediatric obsessive-compulsive disorder. Biol Psychiatry 68:1073–1076. https://doi.org/10.1016/j.biopsych.2010.07.015
Farrell LJ, Waters AM, Boschen MJ et al (2013) Difficult-to-treat pediatric obsessive-compulsive disorder: feasibility and preliminary results of a randomized pilot trial of d-cycloserine-augmented behavior therapy. Depress Anxiety 30:723–731. https://doi.org/10.1002/da.22132
Scheeringa MS, Weems CF (2014) Randomized placebo-controlled D-cycloserine with cognitive behavior therapy for pediatric posttraumatic stress. J Child Adolesc Psychopharmacol 24:69–77. https://doi.org/10.1089/cap.2013.0106
Byrne SP, Rapee RM, Richardson R et al (2015) D-cycloserine enhances generalization of fear extinction in children. Depress Anxiety 32:408–414. https://doi.org/10.1002/da.22356
Carpenter-Hyland EP, Chandler LJ (2007) Adaptive plasticity of NMDA receptors and dendritic spines: implications for enhanced vulnerability of the adolescent brain to alcohol addiction. Pharmacol Biochem Behav 86:200–208
George D, Mallery P, George D, Mallery P (2003) SPSS for Windows step by step: a simple guide and reference. 11.0 update, 4th edn. Allyn & Bacon, Boston
Silverman W, Albano AM (1996) Anxiety disorders interveiw schedule for DSM-IV. Graywind, New York
Katherine Shear M, Brown TA, Barlow DH et al (1997) Multicenter collaborative panic disorder severity scale. Am J Psychiatry 154:1571–1575. https://doi.org/10.1176/ajp.154.11.1571
Shear MK, Rucci P, Williams J et al (2001) Reliability and validity of the Panic Disorder Severity Scale: replication and extension. J Psychiatr Res 35:293–296. https://doi.org/10.1016/S0022-3956(01)00028-0
Elkins RM, Pincus DB, Comer JS (2014) A psychometric evaluation of the panic disorder severity scale for children and adolescents. Psychol Assess 26:609–618. https://doi.org/10.1037/a0035283
Rapee RM, Craske MG, Brown TA, Barlow DH (1996) Measurement of perceived control over anxiety-related events. Behav Ther 27:279–293. https://doi.org/10.1016/S0005-7894(96)80018-9
Hafner RJ, Marks IM (1976) Exposure in vivo of agoraphobics: contributions of diazepam, group exposure, and anxiety evocation. Psychol Med 6:71–88
Silverman WK, Fleisig W, Rabian B, Peterson RA (1991) Childhood Anxiety Sensitivity Index. J Clin Child Psychol 20:162–168. https://doi.org/10.1207/s15374424jccp2002
Peterson RA, Heilbronner RL (1987) The anxiety sensitivity index: construct validity and factor analytic structure. J Anxiety Disord 1:117–121. https://doi.org/10.1016/0887-6185(87)90002-8
Silverman WK, Ginsburg GS, Goedhart AW (1999) Factor structure of the childhood anxiety sensitivity index. Behav Res Ther 37:903–917. https://doi.org/10.1016/S0005-7967(98)00189-2
Chorpita BF, Albano AM, Barlow DH (1996) Child Anxiety Sensitivity Index: considerations for children with anxiety disorders. J Clin Child Psychol 25:77–82. https://doi.org/10.1207/s15374424jccp2501_9
Chorpita BF, Daleiden EL (2000) Properties of the Childhood Anxiety Sensitivity Index in children with anxiety disorders: autonomic and nonautonomic factors. Behav Ther Ther 31:327–349. https://doi.org/10.1016/S0005-7894(00)80018-0
Guy W (1976) The Clinical Global Impression Scale. In: ECDEU Assessment Manual for Psychopharmacology-Revised. US Dept. of Health, Education & Welfare, ADAMHA, NIMH Psychopharmacology Research Branch, Rockville, MD, pp 218–222
Mattis SG, Ollendick TH (1997) Panic in children and adolescents: a developmental analysis. Adv Clin Child Psychol 19:74
Gallo KP, Chan PT, Buzzella BA et al (2012) The impact of an 8-day intensive treatment for adolescent panic disorder and agoraphobia on comorbid diagnoses. Behav Ther 43:153–159. https://doi.org/10.1016/j.beth.2011.05.002
Davis ML, Witcraft SM, Smits JAJ et al (2016) d-cycloserine augmentation of exposure therapy: review and new directions. Qual Prim Care 24 PS:30–32
Smits JAJ, Rosenfield D, Otto MW et al (2013) D-cycloserine enhancement of fear extinction is specific to successful exposure sessions: evidence from the treatment of height phobia. Biol Psychiatry. https://doi.org/10.1016/j.biopsych.2012.12.009
Smits JAJ, Rosenfield D, Otto MW et al (2013) D-cycloserine enhancement of exposure therapy for social anxiety disorder depends on the success of exposure sessions. J Psychiatr Res. https://doi.org/10.1016/j.jpsychires.2013.06.020
Hofmann SG (2014) D-cycloserine for treating anxiety disorders: making good exposures better and bad exposures worse. Depress Anxiety 31:175–177
Paul I, Nowak G, Layer RT et al (1994) Adaptation of the N-methyl-D-aspartate receptor complex following chronic antidepressant treatments. J Pharmacol Exp Ther 269:95–102
McGuire JF, Wu MS, Piacentini J et al (2017) A meta-analysis of D-cycloserine in exposure-based treatment: moderators of treatment efficacy, response, and diagnostic remission. J Clin Psychiatry 78:196–206. https://doi.org/10.4088/JCP.15r10334
Mataix-Cols D, Fernández de la Cruz L, Monzani B et al (2017) D-cycloserine augmentation of exposure-based cognitive behavior therapy for anxiety, obsessive-compulsive, and posttraumatic stress disorders. JAMA Psychiatry 74:501. https://doi.org/10.1001/jamapsychiatry.2016.3955
Hofmann SG, Mundy EA, Curtiss J (2015) Neuroenhancement of exposure therapy in anxiety disorders. AIMS Neurosci. https://doi.org/10.3934/Neuroscience.2015.3.123
Funding
This study was funded by the Brain and Behavior Research Foundation Grant No. 19050 to Ovsanna Leyfer, Ph.D.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leyfer, O., Carpenter, A. & Pincus, D. N-methyl-d-aspartate Partial Agonist Enhanced Intensive Cognitive-Behavioral Therapy of Panic Disorder in Adolescents. Child Psychiatry Hum Dev 50, 268–277 (2019). https://doi.org/10.1007/s10578-018-0837-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-018-0837-1