Abstract
Studies have shown a high prevalence of autistic spectrum traits in both children and adults with psychiatric disorders; however the prevalence rate has not yet been investigated in young children with OCD. The aim of the current study was to (1) determine whether ASD traits indicated by the Social Communication Questionnaire (SCQ) and the Social Responsiveness Scale (SRS) were elevated in young children with OCD who do not have a specific ASD diagnosis and (2) determine if ASD traits were associated with OCD severity. Participants (N = 127) were children ages 5–8 years enrolled in the pediatric obsessive–compulsive disorder treatment study for young children (POTS Jr.). Results indicated that the SRS showed elevated autistic traits in the sample and was associated with OCD severity whereas the SCQ did not indicate heightened ASD symptoms. Implications of these results are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obsessive–Compulsive Disorder (OCD) and autism spectrum disorders (ASD) share similar clinical characteristics, most notably symptoms of repetitive or stereotyped behaviors. The Diagnostic and Statistical Manual [DSM-5; 1] describes the core features of ASD as persistent deficits in social communication and social interaction across multiple contexts and restricted, repetitive patterns of behavior, interests, or activities. ASD also includes specific deficiencies in social-emotional reciprocity, nonverbal communicative behaviors, and the ability to cultivate and maintain meaningful interpersonal relationships. Individuals with ASD may exhibit stereotyped or repetitive motor movements or language usage, the need for sameness, inflexibility, intensely fixated interests, and/or hyper- or hypo-reactivity to sensory input. The DSM-5 core features of OCD include the presence of obsessions, compulsions, or both. Similar to fixed interests in ASD, obsessions are defined as thoughts, urges, or impulses that are recurrent and persistent. However, the distinction between a circumscribed interest and an obsession is that obsessions are intrusive and distressing. Individuals with OCD attempt to neutralize their obsessions with a compulsive, repetitive thought or action. Other topographically similar behaviors shared by OCD and ASD include inflexibility, the need for sameness, and the repetitive nature of characteristic behaviors (compulsions, stereotypies).
Previous research has shown a high prevalence of autistic spectrum traits in both children and adults with OCD [2, 3]. Ivarsson and Melin [2] found that higher ASD traits in children and adolescents with a primary OCD diagnosis were also associated with co-morbid diagnoses, such as tic disorders and attention deficit hyperactivity disorder (ADHD). ASD traits were assessed using the Autism Spectrum Screener Questionnaire [ASSQ; 4], a 27-item parent-report measure. The ASSQ was revised to exclude questions that may overlap with symptoms of OCD and tics. Even with those questions excluded, ASD traits were common amongst their sample and the researchers propose that a diagnosis of OCD itself may be associated with some lower level of ASD traits. Consistent with Ivarsson and Melin’s findings, Bejerot, Nylander, and Lindstrom [3] found that 20 % of their adult subjects with OCD were identified as also having autistic traits. The researchers relied on a clinical interview using the High-Functioning Autism/Asperger Syndrome Global Scale [HAGS; 3] and the Asperger Syndrome Diagnostic Interview [ASDI; 5] to assess autistic features. ASD was not a specific exclusion criterion for either of these studies, making it unclear if co-morbid ASD contributed to these findings. Although an ASD/OCD overlap has been demonstrated in multiple samples, this finding has not yet been investigated in young children (before 10 years old), who after a clinical interview were determined to not have an ASD diagnosis. It would be useful for clinicians to be more adept at this particular differential diagnosis as previous research has emphasized the importance of early treatment especially in ASD [6]. Furthermore, young children may not be adequate reporters of symptoms, which makes assessing for differential diagnoses and establishing consequent treatment paths especially challenging.
Multiple standardized measures, such as the Social Communication Questionnaire [SCQ; 7] and the Social Responsiveness Scale [SRS; 8], have been developed to screen for different symptoms of ASDs in youth. The SCQ is a parent-reported ASD symptom screener. It includes 40 “yes–no” questions derived from the Autism Diagnostic Interview-Revised [ADI-R; 9]. The questions assess the child’s functioning over the past 3 months, as well as the child’s functioning at 4–5 years old. Subscales of the SCQ include: Reciprocal social interaction, communication, and restricted, repetitive, and stereotyped patterns of behavior. The SRS was designed to measure autistic traits and is also a parent-report measure. It includes 65 items rated from 0 to 3, “not true” to “always true.” Subscales of the SRS consist of: Social Awareness, measuring the capability to pick up on social cues; Social Cognition, measuring the interpretation of social cues; Social Communication, measuring expressiveness; Social Motivation, measuring the motivation to engage in social interactions and possible factors, such as, social anxiety, inhibition, and empathic orientation; and Autistic Mannerisms, measuring restricted interests and stereotyped behaviors. Higher scores on either the SRS or the SCQ indicate higher levels of social functioning impairment. Community-based studies find continuous distributions throughout the population on both the SCQ and SRS [10, 11]. Profiles of ASD traits, established through using ASD screening measures like the SCQ and SRS, can be used as a platform to help inform an OCD differential diagnosis; however clinicians should be cautious as these measures assess topography, not function. Higher ASD scores can be used to prompt the clinician to perform further functional assessment (i.e. why is the child doing this behavior?). For example, the clinician could ask: is the child repeating a behavior because he/she derives pleasure from it or is the child repeating because he/she is trying to reduce distress? Topographically the behavior of ASD-driven repeating versus OCD-repeating looks the same but functionally the behaviors serve a different purpose.
Symptom scales, such as the SCQ and SRS, are used frequently to assess for ASD; however, high scores on ASD symptom scales are not always equivalent to an ASD diagnosis [12–14]. The degree to which the SCQ and SRS measure distinct constructs and central features of ASD is questionable in different populations [12–14]. Studies have demonstrated high ratings on the SRS and SCQ for youth with mood and anxiety disorders who did not have an ASD diagnosis [15, 16]. Youth with disruptive behavior disorders or ADHD also may score higher on other ASD scales [17, 18]. Impaired social reciprocity, language deficits, and behavioral rigidity/stereotypy are shared characteristics of ASD and other psychiatric disorders (e.g. mood disorders, anxiety disorders, ADHD) [1]. Higher ASD screener scores in other psychiatric populations may be consistent with the conceptualization that symptoms of ASD are on a continuum. As more clinicians view ASD in this manner, the prevalence of ASDs have increased and less impairing, milder ASD is being diagnosed [10, 19].
The shared clinical characteristics of ASD and OCD are reflected on the SRS and SCQ. Many question-level items on the SRS and SCQ illustrate symptoms that are not solely associated with ASD [20]. For instance, questions on the SRS include: “anxious in social interaction”, “strange bizarre behaviors” and “confident when engaging with others” and questions on the SCQ include: “say the same thing over and over in almost exactly the same way”, “insist that you say the same thing over and over again”, and “have to do things in a particular way or order.” Clinicians should be mindful of the possible diagnostic overlaps when administering the SRS and/or the SCQ. Symptoms of ASD may appear topographically similar to that of other psychiatric disorders; therefore, it is important to assess for the function of the behavior in question. In regards to the ASD/OCD overlap, these measures do not differentiate between the behavioral function of soothing versus distracting or pleasure seeking versus reducing distress.
To date, the elevation of ASD measure scores and overlap of ASD symptoms with other psychiatric disorders have not been investigated in young children (under 10 years of age). This elevation and overlap is particularly difficult to assess in young children with OCD. Specific research is needed to identify profiles of ASD symptom scales in this population. The aims of the current study were to (1) examine scores on ASD symptom scales, using the SCQ and SRS, and determine whether the scores are elevated in young children with OCD who do not have a specific ASD diagnosis and (2) determine if ASD traits are associated with OCD severity. Given the past literature examining the elevation of ASD scores in psychiatric populations, the researchers hypothesize that both the SCQ and SRS will be elevated for our sample. Additionally, the researchers hypothesize that ASD traits will be associated with OCD severity, in that greater psychiatric impairment may yield more elevated scores on ASD measures. If this elevation and association occurs, the researchers believe that this may be a reflection of the shared topographical features of ASD and OCD symptoms and/or indicate that subclinical ASD traits are associated with OCD in young children.
Methods
Participants were 127 children, ages 5–8, with a primary diagnosis of OCD. Participants were recruited as part of a randomized controlled trial examining the efficacy of family-based cognitive behavior therapy (CBT) compared to family-based Relaxation Therapy (RT). Recruitment took place between 2006 and 2011 at three collaborating sites: The University of Pennsylvania (n = 44; 34.6 % of sample), Duke University (n = 35; 27.6 %), and Brown Medical School (n = 48; 37.8 %). Institutional Review Boards at each site approved the study and consent from parents and assent from child participants was obtained.
Participants were screened for eligibility using a three-gate assessment procedure. First, potential subjects participated in a telephone screen with a research assistant to assess their preliminary eligibility (Gate A). Next, those families who were interested and appeared eligible participated in an in-person intake assessment with a doctoral level clinician (Gate B1). If eligible following this assessment, participants proceeded to Gate B2, which included (1) a systematic diagnostic assessment with the parent(s) and child and (2) a team meeting to review all available data to establish caseness and suitability for study entry. Patients determined to be eligible were invited back for Gate C, a baseline visit with an independent evaluator (IE) who was blind to treatment condition.
Inclusion criteria were as follows: Participants must (a) be 5–8 years old, (b) have a DSM-IV-TR primary diagnosis of OCD, with a Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) score of 16 or greater, (c) have had stable symptoms for at least 3 months, (d) be appropriate for outpatient treatment, and (e) have a parent or guardian available to participate in treatment. Exclusion criteria were: (a) another primary psychiatric diagnosis, (b) a diagnosis of pervasive development disorder (PDD), intellectual disability, thought disorder/symptoms of psychosis, or conduct disorder, (c) acute suicidality (d) participation in concurrent psychotherapy, (e) treatment with medication for depression/mood disorder, (f) treatment with medication for ADHD, OCD, anxiety, or tic disorders that had not been stable for more than 8 weeks, (g) a prior failed trial of adequate CBT for OCD [defined as ten sessions of formalized exposure with response prevention (E/RP), and h] meeting criteria for pediatric autoimmune disorders associated with strep (PANDAS).
To further address the exclusion criterion (b) “a diagnosis of PDD”: At Gate A all families participated in a brief telephone screen asking about exclusion diagnoses, specifically PDD. At this gate 20 participants were excluded due to a known existing diagnosis of PDD or mental retardation. Upon the intake assessment at Gate B1 two participants were excluded due to a PDD diagnosis, and upon the further diagnostic assessments at Gate B2/C two more participants were excluded due to a PDD diagnosis. For further information regarding inclusion/exclusion criteria the reader is referred to the POTS Jr Outcomes paper [21].
Assessment measures included the baseline evaluation ratings and assessments by the psychologist assessing the participant at gates B1 and B2, ratings by the IE assessing the participant at gate C, and self-and parent-report measures administered at gate C. All evaluators were trained in making developmentally sensitive adaptations to the clinical interview process. The reader is referred to the POTS Jr Methods paper for more information on these adaptations [22].
OCD symptoms and severity were measured using the Child Yale-Brown Obsessive Compulsive Scale [CY-BOCS; 23]. Evaluators were trained to reliability on the CY-BOCS through monthly supervision, joint interviews, and videotape reviews. The reliability was checked frequently through random selection of videotapes. If an evaluator fell below 80 % agreement they were then retrained. The CY-BOCS is a “gold standard” clinician interview yielding a combined obsessions and compulsions total score (0–40) and demonstrating adequate reliability and validity [23]. Developmentally sensitive anchors and probes were developed. The literature supports the use of the measure in children as young as 6 years [24] and it was used successfully in our prior studies with 5 year olds [25]. Demographics were measured using the Conners March Developmental Questionnaire [CMDQ; 26], including age, grade level, gender, race, and socioeconomic status, and was completed by parents.
Comorbidity was assessed using the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime Version [K-SADS-P/L; 27, 28] is a semi-structured, clinician rated interview that yields DSM-IV diagnoses and has favorable psychometric properties. Interviews were administered to the parent(s) (or primary caretakers), and to children (although 5–6 year old children varied in their ability to participate actively in the interview). The K-SADS is routinely used to assess psychiatric diagnoses in children as young as 5 years [29, 30]. Evaluators were trained using the same process as the CY-BOCS training (i.e. through monthly supervision, joint interviews, and videotape reviews). Twenty percent of tapes were checked for cross-site and inter-rater reliability, and all evaluators were trained to acceptable inter-rater reliability (i.e., 0.85).
Because this version of the K-SADS did not assess PDD, the Childhood Autism Rating Scale [CARS; 31] was administered as a supplement. The CARS is a 15-item behavior observation scale that captures the key elements of autistic disorder. This measure has good reliability and validity. It yields a total score providing a continuous measure symptom severity [32]. In the case of diagnostic ambiguity, specifically if a diagnosis of PDD was suspected, the participant was referred out for further assessment of PDD-related differential diagnosis. Additionally, all cases were presented in cross-site supervision to obtain a team clinical impression and agreement on diagnoses.
Features of ASD were additionally assessed using the Social Communication Questionnaire (SCQ) and the Social Responsiveness Questionnaire (SRS). The SCQ is a 40-item parent report that measures behaviors characteristic of autism spectrum disorders including communication skills and social functioning for children over 4 years old. The measure has demonstrated good internal consistency and concurrent validity [7] For the current sample the SCQ demonstrated acceptable internal consistency (α = 0.712). The SRS is a 65-item parent report that assesses abilities and deficits in social reciprocity in children ages 4–18 years. It has good internal consistency, temporal stability, and concurrent and discriminant validity [8]. The current sample demonstrated a high level of internal consistency on the overall SRS total score (α = 0.835). Four out of the five subscales (Social Awareness, Social Cognition, Social Communication, and Social Motivation) demonstrated less than adequate internal consistency with the exception of the Autistic Mannerisms subscale which demonstrated acceptable internal consistency (α = 0.760). Consequently the researchers will only report on the overall SRS total score and the Autistic Mannerisms subscale. For score interpretation on the SRS, T-scores below 59 are within the normal range, T-scores ranging from 60 to 75 indicate mild to moderate ASD severity, and a T-score above a 76 indicates severe ASD symptomology.
Statistical Analyses
Descriptive statistics were used to summarize the study sample characteristics and are based on N = 127 Continuous variables are summarized using means, standard deviations, medians, and ranges. Categorical variables are described with frequencies and percentages. Relationships among questionnaires that were used in the study and demographic variables (age, sex, race, & ethnicity) were examined with Pearson product-moment correlation coefficient. Preliminary analyses revealed that the SCQ total score was negatively and significantly associated with sex but not the other demographic variables (results below). Therefore, sex was controlled for in subsequent analyses on the SCQ. The association between the CY-BOCS total severity score and the SRS and SCQ total T-scores and subscale T-scores were examined using the Pearson Product Moment Correlation. Additionally, the total severity score on the CY-BOCS were regressed using Multiple Linear Regression on two models: one employing the SRS total T-score and the other the SCQ total score (controlling for sex). In the event of missing data, n is the number of cases with data recorded (there was no missing CYBOCS data, the SRS had 5.51 % missing data and the SCQ had 9.45 % missing).
Results
General Results
Associations among study questionnaires and demographic variables (age, sex, race, & ethnicity) revealed that sex, but not other demographic variables, was negatively and statistically significant for the SCQ, r (115) = 0.198, p < 0.03.
Sample Characteristics
Child demographics and baseline measures are outlined in Table 1. Children were 5–8 years of age (M = 7.22, SD = 1. 2; 52.8 % female), with 95.3 % of the sample describing themselves as non-Hispanic, and 4.7 % Hispanic/Latino. In terms of race, the sample was 89.9 % White, 2.4 % Asian, 1.6 % African American/Black, 3.1 % multi-racial, and 3.1 % not endorsed/missing. The majority of participants had parents living together (90.2 %) and modal yearly family income was above $100,000 (42.5 %), with 84.8 % making over $60,000. In addition, most parents reported a college degree or higher (71.0 % of fathers, 78.3 % of mothers). Almost one-third of sample had birth complications involving breathing problems/lack of oxygen (29.9 %), and 15.7 % were preterm at birth (M = 25.67, SD = 12.81 days early). All participants met criteria for a primary diagnosis of OCD. The CYBOCS mean total score was 25.55 (SD = 4.23), indicating severe OCD symptoms, and average age of onset of OCD symptoms was 5.06 (SD = 1.65, range 2–8). The mean SRS T-score showed elevated autistic traits in the sample (M = 58.29, SD = 11.21; clinical cutoff on the SRS is a T-score of 60) whereas the mean SCQ score (M = 5.74, SD = 4.25) did not indicate heightened ASD symptoms (clinical cut-off on the SCQ is a score of 15).
Correlations
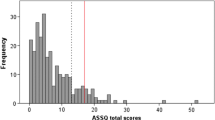
The CY-BOCS total severity score was positively and significantly associated to the SRS total T-score (Fig. 1) as well as the SRS subscale of Autistic Mannerisms (Table 2), indicating that OCD severity is associated with behaviors of ASD. Interestingly, the CY-BOCS total severity score did not correlate with the SCQ total score or its subscales; however, the SRS and SCQ total scores were significantly correlated with each other. Additionally the SRS total T-score demonstrated a relatively moderate correlation with all of the SCQ subscales, ranging in magnitude from 0.38 to 0.44. Sample effect size was interpreted in accordance with Cohen’s (1988) convention.
Regressions
Hierarchical multiple regression models indicated that the SRS total T-score, but not the SCQ total T-score, predicted higher total severity scores on the CY-BOCS, R 2 = 0.043, F (1, 117) = 5.32, p = 0.02. Additionally, the SRS total T-score had a significant weight, B = 0.208, SE = 0.034, suggesting that children who score higher on the SRS demonstrating increased ASD behaviors, will also score higher on the CY-BOCS, showing greater OCD severity.
Discussion
This study had two primary hypotheses: (1) that autistic traits measured by both the SCQ and SRS will be elevated for this sample of young children with OCD and (2) that ASD traits will be associated with OCD severity. These hypotheses were partially supported by this study’s findings. To address the first hypothesis, SRS scores were elevated for this sample (M = 58.29, SD = 11.21; clinical cutoff on the SRS is a T-score of 60), whereas SCQ scores were not (M = 5.74, SD = 4.25; clinical cut-off on the SCQ is a score of 15). Investigation of the second hypothesis is in line with this finding as autistic traits measured by the SRS but not the SCQ were associated with OCD severity as measured by the CY-BOCS. Combining the current study’s findings with previous literature on the ASD/OCD overlap, the researchers posit that overall higher ASD scores may (1) be an artifact of measurement and reflect the shared topography of the disorders and/or (2) indicate a continuum of severity of ASD features in those with OCD.
Young children with OCD in this study appear to score higher overall on the SRS, but not the SCQ. The mean total T-score on the SRS was 58.29 (SD = 11.21), with 36.2 % of the sample scoring a 60 or higher. The researchers note that a T-score of 58 is still within the “normal” range, though it is elevated and closely approaching the clinical cut-off. Conversely, on the SCQ only 2.4 % of the sample scored above the clinical cut-off. Higher scores on ASD measures are in line with previous research in adults and children with OCD, as well as research on other psychiatric populations [15–18]. In particular, Arildskov and colleagues [33] found in a large sample of children with OCD that subclinical ASD traits co-occurred with OCD symptoms for about 10–17 % of their sample. ASD and other psychiatric disorders, specifically OCD, overlap in symptom features (i.e. impaired social reciprocity, language deficits, and behavioral rigidity/stereotypy). Since it is impossible to ascertain behavioral function simply from the results of the SRS and SCQ, this study’s results may be that the SRS is capturing symptom overlap where the SCQ is not. The clinical implications of this finding are important for clinicians who may use the SRS as a diagnostic tool. In line with this study’s results and previous research on ASD measures, elevated scores on the SRS may be a reflection of other psychiatric conditions (i.e. OCD, as 36.2 % of this study’s sample was above the clinical cut-off). Clinicians should not rely solely on the SRS to inform an ASD diagnosis. Rather, clinicians should be informed through the use of good functional assessment techniques.
OCD severity for young children, as indicated by the CY-BOCS, was significantly associated with the SRS total T-score but not the SCQ total score. The CY-BOCS also correlated with the SRS subscale of Autistic Mannerisms. Additionally, the SRS total T-score was predictive of higher total CY-BOCS scores.
It is interesting that the SRS and not the SCQ was associated with the CY-BOCS. Autistic traits in young children as indicated by the SRS were predictive of greater OCD severity; yet for this sample, scoring higher on an ASD symptom screener (i.e. the SCQ) was not related to OCD severity. Despite no correlation between the CYBOCS and SCQ, the SRS and SCQ were positively and significantly correlated with each other. The differing relationship with the CYBOCS may be due to differences in the structure of the SRS and SCQ. The SRS is more thorough than the SCQ, having more items and also more precise subscales. The SRS measures autistic traits with a four-point scale that allows for some variability in response, whereas the SCQ was designed to be a quick ASD symptom screener with simple “yes/no” responses. Consequently, the response choices on the SCQ may have led to floor and ceiling effects. These effects may be a factor accounting for different findings with these measures. This discrepancy is in line with previous research proposing that OCD itself may be associated with some lower level of ASD traits [2] and the milder spectrum of ASD traits may not be captured by the “yes/no” responses on the SCQ. Another potential reason for no relationship between the CYBOCS and the SCQ is an attenuated correlation due to low variance. The SRS may lend itself to less attenuation because it is a likert scale as opposed to behavior counts.
The CY-BOCS was also significantly associated with the Autistic Mannerisms subscale of SRS. This may be a result of the SRS’s inability to assess function of behavior and therefore it may not accurately discriminate between compulsions and stereotypies. Differential diagnosis in younger children may be challenging, as developmental limitations could hinder a child’s ability to report on the more cognitive aspects of OCD. Additionally, young children with more severe OCD may be preoccupied by their obsessive thoughts and compulsions, reducing their opportunities to practice and refine their social skills. As previously discussed, compulsions and stereotypies can share the same topographical features but serve very different functions. This further highlights the importance of incorporating other assessment strategies (e.g. functional assessment) into clinical interviews, especially with younger children. Once a differential diagnosis is established, a treatment path can be pursued.
The child’s developmental level is an added challenge to establishing a diagnostic picture. Typically developing young children may also share some ASD/OCD features such as a need for sameness and repetitive behaviors. In fact, Evans and colleagues [34] found “just right” behaviors like these are common in early childhood. Given that younger children may exhibit topographically similar symptoms to ASD, their scores on ASD measures could be elevated. Constantino and colleagues [35] divided children who took the SRS into two age groups, 4–7 year olds and 8–14 year olds, and found differences in SRS item factor loadings. Despite this finding, other studies have found SRS scores were not correlated with age [8, 36]. To add, Hus and colleagues [37] caution that non-ASD specific characteristics, including developmental level, can affect the SRS scores. Due to this influence, the researchers further advise clinicians to be cautious while using the SRS as a continuous measure of ASD severity and/or social deficits.
This study is not without limitations. The researchers propose two possible explanations for elevated scores on ASD measures for those with OCD: that it may either be an artifact of measurement and/or indicate an association with subclinical ASD features and OCD for young children; yet the results of this study cannot specifically point to one explanation or the other, as the explanation may vary on a case-by-case basis. Consequently, that is why the researchers strongly urge clinicians to perform thorough functional assessments of symptoms.
Additionally, although ASD was an exclusion criterion of the study, assessing for ASD symptoms was not the primary focus of the assessment. The primary goal of the assessment was to establish an OCD diagnosis and evaluate OCD severity. Therefore, children received a structured clinical interview that did not thoroughly evaluate ASD features. However, if a participant’s diagnosis was unclear after the assessment, particularly if the clinician suspected possible ASD, the participant was referred out for more comprehensive testing. As a result of excluding participants with higher levels of ASD (those with an ASD diagnosis) this study truncated the range of ASD symptoms. Due to that exclusion criterion, this study was unable to look at the true co-occurrence of OCD and ASD. A further limitation is that the SRS and SCQ are parent-report measures. Unlike clinicians, parents are reporting on a topographical level of the symptoms they observe, not on a functional level. The study could also have benefited from more clinical impressions regarding ASD symptoms.
There is little research on evaluating social characteristics specific to OCD in younger children. As such, either further research is necessary to develop more precise measures differentiating the function of OCD and ASD symptoms, or these symptoms should be viewed in a more dimensional manner [e.g. NIHM Research Domain Criteria (RDoC)]. Other studies have provided support on the transdiagnostic nature of ASD features [15–18]. ASD traits clearly overlap with other psychiatric disorder symptoms (e.g. impaired social reciprocity, language deficits, and behavioral rigidity/stereotypy) and emerging research has shown elevated scores on ASD measures within psychiatric populations (e.g. mood disorders, anxiety disorders, ADHD) [1, 15–18]. This study adds a unique population to that literature.
Summary
This study investigated ASD measures, the SRS and the SCQ, in a population of young children with OCD. Higher scores were found on the SRS, but not the SCQ. For the SRS 36.2 % of the sample had a T-score of 60 or greater, whereas only 2.4 % of the sample met clinical cut-offs for the SCQ. Additionally the SRS was significantly correlated with the CY-BOCS, indicating that greater social impairment was associated with more severe OCD. Given that OCD and ASD overlap in symptom features (i.e. impaired social reciprocity, language deficits, and behavioral rigidity/stereotypy), the SRS may be capturing that overlap. The “yes/no” response choices on the SCQ may have led to floor and ceiling effects which may be a factor accounting for different findings on the SRS. The discrepancy between the SRS and SCQ is in line with previous research proposing that OCD itself may be associated with some lower level of ASD traits [2] and the milder spectrum of ASD traits may not be captured by the “yes/no” responses on the SCQ. Either additional research is needed to develop measures that more precisely delineate OCD and ASD symptoms, or these symptoms should be viewed in a more dimensional manner [e.g. NIHM Research Domain Criteria (RDoC)].
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Ivarsson T, Melin K (2008) Autism spectrum traits in children and adolescents with obsessive–compulsive disorder (OCD). J Anxiety Disord 22(6):969–978
Bejerot S, Nylander L, Lindström E (2001) Autistic traits in obsessive–compulsive disorder. Nord J Psychiatry 55(3):169–176
Ehlers S, Gillberg C, Wing L (1999) A screening questionnaire for Asperger syndrome and other high-functioning autism spectrum disorders in school age children. J Autism Dev Disord 29(2):129–141
Gillberg C et al (2001) The Asperger Syndrome (and high-functioning autism) Diagnostic Interview (ASDI): a preliminary study of a new structured clinical interview. Autism 5(1):57–66
Peters-Scheffer N et al (2011) A meta-analytic study on the effectiveness of comprehensive ABA-based early intervention programs for children with autism spectrum disorders. Res Autism Spectr Disord 5(1):60–69
Rutter M, Bailey A, Lord C (2003) The social communication questionnaire: manual. Western Psychological Services, Torrance
Constantino JN, Gruber CP (2005) Social responsiveness scale (SRS). Western Psychological Services, Los Angeles
Le Couteur A, Lord C, Rutter M (2003) The autism diagnostic interview-revised (ADI-R). Western Psychological Services, Los Angeles
Baird G et al (2006) Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP). Lancet 368(9531):210–215
Constantino JN et al (2003) Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord 33(4):427–433
Bishop DV, Norbury CF (2002) Exploring the borderlands of autistic disorder and specific language impairment: a study using standardised diagnostic instruments. J Child Psychol Psychiatry 43(7):917–929
Constantino JN et al (2004) The factor structure of autistic traits. J Child Psychol Psychiatry 45(4):719–726
Corsello C et al (2007) Between a ROC and a hard place: decision making and making decisions about using the SCQ. J Child Psychol Psychiatry 48(9):932–940
Pine DS et al (2008) Autism spectrum disorder scale scores in pediatric mood and anxiety disorders. J Am Acad Child Adolesc Psychiatry 47(6):652–661
Towbin KE et al (2005) Autism spectrum traits in children with mood and anxiety disorders. J Child Adolesc Psychopharmacol 15(3):452–464
Geurts HM et al (2004) Can the Children’s Communication Checklist differentiate between children with autism, children with ADHD, and normal controls? J Child Psychol Psychiatry 45(8):1437–1453
Gilmour J et al (2004) Social communication deficits in conduct disorder: a clinical and community survey. J Child Psychol Psychiatry 45(5):967–978
Fombonne E (2009) Epidemiology of pervasive developmental disorders. Pediatr Res 65(6):591–598
Grzadzinski R et al (2011) Examining autistic traits in children with ADHD: does the autism spectrum extend to ADHD? J Autism Dev Disord 41(9):1178–1191
Freeman J et al (2014) Family-based treatment of early childhood obsessive–compulsive disorder: the Pediatric Obsessive–Compulsive Disorder Treatment Study for Young Children (POTS Jr)–a randomozed controlled trial. JAMA 71:689–698
Freeman J et al (2012) The Pediatric Obsessive Compulsive Disorder Treatment Study for Young Children (POTS Jr): developmental considerations in the rationale, design, and methods. J Obsessive Compuls Relat Disord 1(4):294–300
Scahill L et al (1997) Children’s Yale-Brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36(6):844–852
March JS, Leonard HL (1998) Obsessive–compulsive disorder in children and adolescents. In: Swinson RP, Antony MM, Rachman S, Richter MA (eds) Obsessive–compulsive disorder: theory, research, and treatment. The Guilford Press, New York, pp 367–394
Freeman J, Flessner CA, Garcia A (2011) The Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity for use among 5 to 8 year olds with obsessive–compulsive disorder. J Abnorm Child Psychol 39(6):877–883
Conners C, March J (1996) The Conners/March Developmental Questionnaire. MultiHealth Systems Inc, Toronto
Chambers W (1985) The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode Version. Arch Gen Psychiatry 42(7):696–702
Kaufman J et al (1997) Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36(7):980–988
Hirshfeld-Becker DR, Biederman J (2002) Rationale and principles for early intervention with young children at risk for anxiety disorders. Clin Child Fam Psychol Rev 5(3):161–172
Youngstrom E et al (2003) Toward an integration of parent and clinician report on the Young Mania Rating Scale. J Affect Disord 77(2):179–190
Schopler E, Reichler RJ, Renner BR (1988) The childhood autism rating scale (CARS). Western Psychological Services, Los Angeles
Perry A et al (2005) Multi-site study of the Childhood Autism Rating Scale (CARS) in five clinical groups of young children. J Autism Dev Disord 35(5):625–634
Arildskov TW et al (2015) Subclinical autism spectrum symptoms in pediatric obsessive–compulsive disorder. Eur Child Adoles Psy. doi:10.1007/s00787-015-0782-5
Evans DW et al (1997) Ritual, habit, and perfectionism: the prevalence and development of compulsive-like behavior in normal young children. Child Dev 68(1):58–68
Constantino JN et al (2000) Reciprocal social behavior in children with and without pervasive developmental disorders. J Dev Behav Pediatr 21(1):2–11
Bölte S, Poustka F, Constantino JN (2008) Assessing autistic traits: cross-cultural validation of the social responsiveness scale (SRS). Autism Res 1(6):354–363
Hus V et al (2013) Factors influencing scores on the social responsiveness scale. J Child Psychol Psychiatry 54(2):216–224
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stewart, E., Cancilliere, M.K., Freeman, J. et al. Elevated Autism Spectrum Disorder Traits in Young Children with OCD. Child Psychiatry Hum Dev 47, 993–1001 (2016). https://doi.org/10.1007/s10578-016-0629-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-016-0629-4