Abstract
In a cross-sectional study, the prevalence rates of overall and specific mental health problems (MHP), as well as consequential impairments, were examined in a representative community sample of German preschoolers. MHP in 391 children were assessed by applying the Strength and Difficulties Questionnaire, as well as its impact supplement. Furthermore, the child behaviour checklist 1½–5 (CBCL 1½–5) and the IOWA-Conners behaviour rating scale were applied. Prevalence rates of MHP with 95 % confidence intervals (95 % CI) were determined. Odds ratios were calculated to analyse the relationships between MHP, age, gender, socioeconomic status, and geographical region using logistic regression. Overall, 7.4 % of the children showed symptoms of MHP. 12.9 % of the children were considered to be impaired by psychosocial problems. Depressive and anxiety symptoms were present in 4.2 % of the children; 11.8 % showed hyperactivity symptoms. The observed prevalence rates call for early mental health prevention in preschoolers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiological data on the prevalence of MHP in childhood can help to improve the scientific foundation for preventing mental disorders and for the planning of corresponding health services [1, 2]. Data from longitudinal studies indicate that mental disorders frequently persist from preschool age through mid-childhood to adolescence [3]. The 4-year longitudinal study by Beyer et al. [4] assessed MHP within a German general population sample and revealed a high level of persistence of behavioural and emotional problems from kindergarten to primary school. Studies using retrospective reports of adults with MHP showed that most MHP occurred much earlier in their life [5]. These results indicate that a substantial proportion of adult mental health disorders are an extension of childhood disorders and should be recognized and treated early in life. Therefore, information regarding the prevalence of psychopathology in preschoolers is of great importance.
In the US, the most common disorders in preschoolers assessed within representative studies, based on diagnostic parent interviews, were oppositional defiant disorder (ODD) (9.4–13.4 %), attention deficit hyperactivity disorder (ADHD) (12.8 %) and specific phobia (9.1 %) [6, 7]. In a Danish study Esbjorn et al. [8] identified that 5.7 % of preschool aged children referred to clinical psychiatric in- and outpatient wards showed anxiety disorders. Diagnoses of mental disorders were based on clinical judgement using the International Classification of Diseases (ICD-10) [9]. Based on representative data from the general Danish population, MHP were found in 4.8 % of preschoolers [10]. MHP were determined using the extended version of the SDQ administered in parents and preschool teachers [10]. Using parent diagnostic interviews and the SDQ Wichstrom et al. [11] showed a prevalence rate of 7.1 % for any psychiatric disorder within a community sample in Norway. The most common disorders were ADHD (1.9 %), ODD (1.8 %), conduct disorder (0.7 %), anxiety disorders (1.5 %), and depressive disorders (2.0 %). Diagnoses were generated using the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; fourth edition) [12]. In contrast to their American counterparts, these European studies display lower prevalence for externalizing problems, including ADHD (0.7–1.9 %) and ODD (1.8 %), and higher rates of depressive (2.0 %) and anxiety disorders (5.7 %) [10, 11]. The differences in estimates of prevalence rates can be partly attributed to methodological differences. In the American studies mental disorders were identified using diagnostic parent interviews, whereas diagnoses in the European studies were assigned by trained child and adolescent psychiatrists and by the judgements of parents as well as preschool teachers [8, 11]. This methodological difference may lead to lower prevalence rates in the European studies. Another likely explanation for the lower prevalence rates may be the geographical region in which the studies were conducted. The reported European studies were conducted in Denmark and Norway. These countries have a relatively low rate of poverty and a low rate of unemployment [11]. Children from these countries have a more equal access to social and educational facilities [10] which may lead to lower prevalence rates of mental disorders in North Europe [11]. Heiervang, Goodman, and Goodman analysed SDQ scores of a Norwegian sample in comparison to a British sample [13]. According to the authors, lower questionnaire scores in Norwegian children seemed to reflect under-recognition by Norwegian adults and not actual lower prevalence rates [13]. These results indicate that prevalence estimates assessed with screening instruments may be partly attributed to cross-cultural differences.
A meta-analysis of 33 studies conducted by Barkman and Schulte-Markwort [14] revealed a prevalence rate of 17.6 % for emotional and behavioural disorders in German children and teenagers between the ages two and 19. In Germany, a day-care centre survey conducted by Rudolph and colleagues [15] using a parental questionnaire and a screening test administered by trained kindergarten teachers revealed that 15.4 % of the 3–6 year olds showed abnormalities in their socio-emotional development. Comparable results were found by Furniss et al. [16] in the baseline assessment of a longitudinal study revealing a 6-month prevalence for emotional and behavioural issues of 12.4 %, in which 14.2 % of boys and 10.5 % of girls displayed problems.
However, representative epidemiological investigations in Germany on MHP in preschoolers are still lacking [17]. Thus, the aim of the current study was to determine the prevalence rates of general and specific MHP, defined as emotional and behavioural problems, and the impairment caused by the reported symptoms among German preschoolers. Studies assessing MHP in children and its correlates document statistically significant associations of MHP and several risk factors, including male gender and low SES [10, 18]. After the German re-unification in 1990, large differences of the labour market situation in East and West Germany persist and lead to socioeconomic differences between both regions, with lower wages and a higher unemployment rate in East Germany [19]. An additional aim of the present study was therefore to examine the relation of sociodemographic factors, including geographical region, SES, age, and gender to MHP.
Methods
Study Design, Recruitment and Sample
Detailed information on the conceptualization, design and procedure of the BELLA study is provided by Ravens-Sieberer and colleagues [20]. The BELLA study is the mental health module of the KiGGS [21], which was conducted by the Robert Koch-Institute. The BELLA study collected data on mental health in a representative sample, with ages ranging from 7 to 17 years.
Parents from the KiGGS study with children aged 3–6 years were asked to participate in the BELLA preschool study in the third round of data collection between 2005 and 2006. The BELLA preschool study examined data from 33 sample points that were distributed relatively equally across Germany. Overall, 24 of the sample points were located in the western German states; nine sample points were located in the states of former East Germany, including Berlin. Seven-hundred-ninety-two parents were asked to participate in the BELLA preschool study. After receiving parents’ informed consent, the questionnaires were sent to 450 families (49.4 %). Three-hundred-ninety-one parents (87 %) provided information on their children.
Measures
Measurements for the BELLA preschool study were selected in accordance with the BELLA study. However, some modifications were necessary, as not all measurements were suitable for preschool aged children. MHP were assessed applying the SDQ 4-16 version [SDQ; 22], as well as its impact supplement [SDQ-Impact; 23]. Additional to the assessment of overall MHP, externalised abnormalities were assessed using the subscale aggressive behaviour of the Child Behaviour Checklist 1½–5 [CBCL 1½–5;24] and the IOWA-Conners Behaviour Rating Scale [25]. Internalised abnormalities were operationalised with the anxiety/depression subscale of the CBCL 1½–5. All of the questionnaires were completed by parents.
Strength and Difficulties Questionnaire
The SDQ [22] is a behavioural screening instrument containing 25 items to assess overall MHP in children from the last 6 months. Each of the items is scored on a three-point Likert scale, with ‘0 = not true’, ‘1 = somewhat true’ or ‘2 = certainly true’. To assess overall MHP, the scores of the four problem dimensions, emotional symptoms, conduct problems, hyperactivity/inattention, and peer problems, are summed to create a total difficulties score. The total difficulties score ranges from 0 to 40 and is classified into ‘normal’, ‘borderline’ and ‘abnormal’. To avoid the overestimation of the prevalence rates, only children with ‘abnormal’ SDQ scores were considered to have MHP in the present study. Cut-off points were defined based on available German normative data [22]. Scores of 16–40 were classified into ‘abnormal’ SDQ scores. In Germany, studies have been conducted using the German version of the SDQ showing the internal consistency and discriminant validity of the instrument [26, 27]. The German translation of the SDQ showed good internal consistencies (Cronbach’s alpha) for the subscales ranging from 0.72 to 0.81 and a Cronbach’s alpha of 0.83 for the total difficulties score in a clinical sample of 543 children and adolescents. The total difficulties score of the SDQ was able to distinguish between children with and without any clinical diagnosis [26, 27]. The SDQ shows strong associations with other measures of MHP and acceptable screening abilities to discriminate between children with and without MHP [28, 29]. In the BELLA preschool study, the internal consistency (Cronbach’s alpha) was 0.77 for the total difficulties score and ranged from 0.46 (conduct symptoms) to 0.76 (hyperactivity symptoms) for the sub-scales. The low internal consistency of some SDQ sub-scales does not allow for reliable statements about specific MHP to be made. Therefore, only the total difficulties score was applied in the present study.
SDQ-Impact Supplement
The SDQ-Impact was developed to collect information relating to the impact of MHP [23]. It assess whether the child has a problem concerning his or her emotions, concentration, behaviour or whether the child is able to get on with other people. In case this question is confirmed, subsequent items focus on chronicity, distress, social impairment, and burden for others [23]. For purpose of illustration an example of a SDQ-impact supplement item is provided: “Overall, do you think that your child has difficulties in one of the following areas: emotions, concentration, behaviour or being able to get on with other people?”
The answers of the five item questionnaire are coded on a 4-point Likert Scale (‘not at all’ = 0, ‘only a little’ = 0, ‘quite a lot’ = 1, ‘a great deal’ = 2). The ‘impact score’ was generated by adding the scores on the distress and social incapacity items using a ‘0012’ scale for each item. This scoring disregards reports of smaller levels of distress or social incapacity as clinically irrelevant [23]. Children were considered to be impaired if the impact score was one or higher. There has been no study conducted in Germany that has evaluated the psychometric properties of the SDQ-Impact. Goodman [23] showed that the English version of the SDQ-Impact is able to discriminate between clinic and community subjects in a valid and reliable way [23]. In the present study, the internal consistency of the SDQ-Impact was acceptable (Cronbach’s alpha = 0.73).
Child Behaviour Checklist 1½–5
In the present study, the German version of the CBCL 1½–5 [24] was used. The scale comprises 99 items that each have three options (‘not true’ = 0, ‘somewhat or sometimes true’ = 1, ‘very true or often true’ = 2) and refers to the last two months. CBCL 1½–5 provides a total problem score, internalizing and externalizing disorder scores, and six problem scale scores on emotional reactivity, anxiety/depression, somatic difficulties, social withdrawal, sleeping problems, attention problems, and aggressive behaviour [30]. In the present study, data on the two subscales—aggressive behaviour (8 items) and anxiety/depression (19 items)—were collected. Scale sum scores were used in analyses and compared with norm samples using the cut-off according to the manual, with a cut-off score of 25 which is equivalent to a T score of 70 for aggressive behaviour and a cut-off score of 9 which is equivalent to a T score of 70 for anxious/depressive behaviour [30]. The internal consistency of most of the scales has been shown to be good to excellent (>0.80). The CBCL 1½–5 showed good validity by differentiating between the field and the clinical samples [31]. In the present study, the internal consistency of the two subscales that assessed aggressive and anxious/depressive behaviour was acceptable to good (Cronbach’s alpha = 0.69 for anxiety/depression and 0.87 for aggression).
IOWA-Conners Behaviour Rating Scale
The 10-item IOWA-Conners Behaviour Rating Scale [25] assesses the occurrence of the most important symptoms of ADHD within the last month and is based on the original version of the Conners Rating Scale [32]. This short version includes the most commonly marked items of the original version. The IOWA scale has been widely used in epidemiological studies and has shown good reliability, as assessed by test–retest and internal consistency reliability [33]. The IOWA scale was rated by the parents on a 4-point rating scale ranging from 0 to 3, in which zero indicates that the child has never shown any negative behaviour and 3 indicates the constant occurrence of appropriate behaviour. A score of 13 or more was considered to indicate MHP. The internal consistency in the present study was good, as evidenced by a Cronbach’s alpha of 0.83.
Statistical Analyses
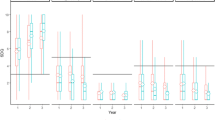
The prevalence rates of MHP with 95 % CI were calculated for the total sample and subgroups according to gender, age group, SES, and geographic region. OR with 95 % CI were calculated to analyse univariate and multivariate associations between MHP and sociodemographic characteristics using logistic regression [34]. To investigate the relationship between the prevalence of MHP (dependent variable) and gender, age, SES, and geographic region (indicators) univariate logistic regressions were conducted. In the univariate logistic regression only one indicator was considered at a time. Subsequently, a multivariate logistic regression was performed (Method: Enter) in which all indicators were considered simultaneously. As the validity of logistic models become problematic if the ratio of the numbers of events per predictor variable becomes too small, it was only calculated with a minimum of 10 events per cell in each predictor [35].
To encounter sampling imbalances and differential non-response, we used post hoc case weights based on reference data from the German Federal Office of Statistics (31 Dec 2012). In order to calculate the post hoc case weights a mixed weighting method was used. In the first step, proportional weights were calculated by dividing the population percentage by the corresponding response percentage for each subgroup (gender, age, SES, geographic region). After multiplying these proportional weights, the mean of the product was calculated.
The final case weights were calculated by dividing the product by its mean value. After the data had been weighted the number of cases reported in each subgroup might deviate from the number of cases in the unweighted sample.
The weights were calculated to ensure the representativeness (indicated by similar univariate distributions) of the sample for the corresponding German population regarding gender, age (including two age groups of 3–4 and 5–6 years), SES (low, middle, high), and geographic region (eastern and western Germany).
As multiple statistical tests were performed on a single set of data, the Bonferroni correction was used to adjust significance level in order to avoid an increased risk of type I error. The significance level was adjusted based on the number of hypotheses being tested. In the Bonferroni-adjusted analyses, we considered the findings to be statistically significant at p < 0.013.
Missing values were estimated via indirect maximum likelihood estimation (EM algorithm) in the SPSS package. This method has been recommended for descriptive analyses [36]. All of the analyses were performed with PASW Statistics version 18 for Windows [37].
Results
Sample Characteristics
The demographic features of the sample were compared to representative data from the German Federal Office of Statistics (reference data 31 Dec 2012). A description of the sample and a comparison with the data from the Federal Office of Statistics is presented in Table 1.
Approximately 7.9 % of the families in the present study had a migration background. However, as the surveying of families was limited to the German language, families with a migration background participating in this study cannot be considered to be representative of migrant families living in Germany. Furthermore, families from large urban areas were underrepresented in the study. Therefore, analyses regarding migration background and community area were not conducted.
After the data had been weighted to be representative on a national level, the sample included children aged three to four (49.6 %) and children aged five to six (50.4 %). A total of 51.7 % of the participating children were girls, 26.8 % of the children had parents with a low SES, 43.1 % of the children had parents with a middle SES, and 30.1 % of the children had parents with a high SES. The majority of the children (80.8 %) lived in western Germany.
Prevalence of MHP and Impairment
Table 2 shows the prevalence and OR of MHP in preschoolers according to the SDQ, separately, for gender, age, SES, and geographic region.
The prevalence of MHP in preschoolers was 7.4 %. MHP were found in 9.0 % of the boys and 5.9 % of the girls. The prevalence of MHP was 9.8 % in children aged 3–4 years and 5.1 % in children aged 5–6 years. In families with low SES, 10.6 % of the children showed MHP; 4.2 % of the children with middle parental SES had MHP, and 9.3 % of the children with high parental SES had MHP. Eight percent of children from eastern Germany had MHP compared to 7.3 % of children from western Germany. Gender, age, and SES had no statistically significant influence on the prevalence of MHP in multivariate logistic regression analyses (χ 2 = 15.11, p = 0.06).
Table 3 depicts the impairment and prevalence of MHP with associated impairments according to the SDQ-Impact; 12.9 % of the children were judged as impaired by their parents. The prevalence of cases with MHP as well as cases of reported impairment was 3.9 %. Parents considered 14.8 % of the boys and 11.4 % of the girls to be impaired. The prevalence of MHP with associated impairment was reduced to 4.2 % for boys and 3.5 % for girls. In comparing age groups, 13.9 % of the children aged three to four and 11.7 % of the children aged five were judged as impaired. MHP with associated impairment were found in 4.6 % of the children aged 3–4 years and in 3.6 % of the children aged five to six. Impairment was assessed in 13.3 % of the children with lower parental SES, 10.7 % of the children with middle parental SES, and 15.4 % of the children with high parental SES. Regarding MHP with associated impairment, the prevalence rates reduced to 4.8 % in children with low parental SES, 2.4 % in children with middle parental SES and 5.9 % in children with high parental SES. With respect to impairment and MHP with associated impairment, comparable prevalence rates can be seen in children in both geographic regions. Gender, age, and SES had no statistically significant influence on the prevalence of impairment (χ 2 = 15.05, p = 0.06) as well as on the prevalence of MHP with associated impairment (χ 2 = 6.89, p = 0.55) in multivariate logistic regression analyses.
Prevalence of Specific MHP
The evaluation of specific MHP revealed that 4.2 % of children had depressive and anxiety symptoms according to the CBCL 1½–5 (see Table 4); 4.5 % of the girls showed depressive and anxiety symptoms compared to 3.7 % of the boys. Children of both age groups showed comparable prevalence rates, and 1.9 % of the children with low parental SES showed depressive and anxiety symptoms compared to 4.8 % of the children with middle parental SES and 5.1 % of the children with high parental SES. Depressive and anxiety symptoms where shown in 5.3 % of the children from eastern Germany and 4.1 % of the children from western Germany.
Aggressive behaviour, as measured by the CBCL 1½–5, was seldom seen and only exhibited in 0.8 % of the total population. Only boys showed aggressive behaviour (1.6 %). Because aggressive behaviour was rare amongst preschoolers, prevalence estimates of other sociodemographic characteristics could not be reliably obtained.
According to the IOWA Conner’s Rating Scale (see Table 5), 11.8 % of children showed hyperactive behaviour. The prevalence rates of hyperactivity behaviour were almost identical in both genders (12.2 vs. 11.4 %). Hyperactive behaviour was exhibited in 15.5 % of the children aged 3–4 years compared to 8.1 % of the children aged 5–6 years. Hyperactivity symptoms were demonstrated in 16.3 % of the children with low parental SES compared to 10.1 % of the children with middle parental SES and 9.4 % of the children with high parental SES. Regarding the geographic region, 16.0 % of the children from eastern Germany showed hyperactivity behaviour compared to 10.8 % from western Germany. Gender, age, SES, and global region had no statistically significant influence on the prevalence of hyperactivity behaviour in multivariate logistic regression analyses (χ 2 = 13.67, p = 0.09).
Discussion
MHP in preschoolers tend to continue into adolescence [1, 2] and pose risk factors for the development of mental disorders in adulthood [5]. Thus, the aim of the present study was to investigate the prevalence of MHP in children aged 3–6 years within a population-based sample in Germany.
A possible mental disorder was indicated for 7.4 % of the preschoolers who had abnormally high levels of MHP. Compared to other studies, the present study reported lower prevalence rates for general MHP in preschoolers [14, 15, 18]. However, in the present study, only children with ‘abnormal’ SDQ scores were considered to be actual cases to report conservative prevalence rates. Therefore, the reported prevalence rates of overall MHP may be lower than reported in other studies. A comparable case definition was applied in the BELLA study, which assessed MHP in children aged 7–17 years [38]. The results of both studies display a strong concordance, with prevalence rates of general MHP of approximately 7 %. When the impairment of the children was considered, the overall prevalence rates decreased from 7.4 to 3.9 % in the present study. The same effect has been shown repeatedly in studies of older children [38]. Therefore, not all children meeting the symptom criteria were impaired by their condition. Additionally, 12.9 % of the preschoolers were considered to be impaired according to the SDQ-Impact. Hence, some of the preschoolers were considered to be impaired by their parents, even though they did not show elevated symptoms scores. Goodman [23] showed that the impact supplement of the SDQ was better than the symptom scores of the SDQ at discriminating between the community and clinic samples. These results indicate that the assessment of impairment caused by MHP could provide more information than the assessment of mental health symptoms only. The SDQ-Impact may help to identify children who are at risk for developing mental health symptoms. This finding is consistent with other results by the BELLA study [39], which found children with undiagnosed impairment. However, it must be said that the findings of the BELLA preschool study are solely based on parental judgements. Besides, the SDQ-Impact does not use a standard definition for a minimum functional level of impairment. This may lead to an overestimation of children’s minor difficulties. Although the SDQ-Impact is able to differentiate clinical from community samples, the validity of such a differentiation is depending on many factors as for example the age and the kinds of problems manifested by the children [30]. Furthermore, Burns et al. [40] showed that it is harder to detect children with psychiatric problems in the community setting. The SDQ and its impact supplement may be able to distinguish between community and clinic samples; nevertheless it is harder to detect children with psychiatric disorders in the community [40].
Although children with low parental SES are often found to show higher rates of MHP, the present study did not find a significant association between low SES and MHP. This result might be due to the relatively conservative definition of MHP, which excludes children at risk. Furthermore, the impact of a low SES on MHP might be clearer in older children [41].
Emotional problems indicating internalizing symptoms were found in 4.2 % of the preschoolers. The lower frequency of internalizing symptoms in the present study may be a result of only including parent-based prevalence rates in the analysis. As externalizing symptoms are easier to recognize, parents may judge them as being more prevalent in their children [42]. It is therefore possible that the use of parent-based measurements, rather than a structured diagnostic interview, may have resulted in a substantial bias in favour of hyperactivity symptoms. This bias may have influenced the present results, as the highest frequencies for specific MHP were found for hyperactivity symptoms. Using the IOWA-Conners Rating Scale, 11.8 % of the children showed hyperactivity symptoms. With the exception of Scandinavian studies [8, 10, 11], this finding is consistent with studies conducted in the US, such as the prevalence of 12.8 % in the study by Carter et al. [18] for any type of ADHD. However, in the BELLA study [38] results assessed with IOWA-Conners Rating Scale seemed to overestimate hyperactivity symptoms comparing to screening instruments based on DSM-IV criteria. Prevalence rates of hyperactivity symptoms in the present study may be therefore highly dependent on the applied screening instrument.
Furthermore, these results are consistent with results showing higher prevalence rates of externalizing problems compared to internalizing problems in children younger than 13 years [43]. Generally, high prevalence estimates for externalizing problems in the present study indicate that disruptive behaviour is the main problem in preschoolers in Germany. Specifically, boys were more likely to suffer from general MHP and face a higher risk of developing hyperactivity symptoms. These findings are consistent with studies showing a higher tendency toward more disorders in boys in younger age groups, whereas these differences in prevalence estimates are much more apparent in externalizing problems [7].
Special attention should be paid to the limitations of the present study. In the present study screening instruments were applied in order to assess the occurrence of MHP and associated impairment. The applied screening instruments assess psychopathological problems and do not diagnose mental disorders. Therefore, the reported prevalence rates of MHP indicate the probability of a particular mental disorder and do not imply a clinical diagnosis.
Moreover, the reported prevalence estimates are highly dependent on the cut-off criteria of applied screening instruments. In order to avoid the overestimation of the prevalence rates, only children with clearly deviant scores from the normal population were considered to have general and specific MHP.
Results of the SDQ and its impact supplement indicated that considerably more children showed impairment than psychopathological problems. The observed differences may reflect reporting biases, as the findings of the present study are solely based on parental judgements.
Minor difficulties of the children may have been pathologised by their parents. Parents may be more likely to report perceived impairment of their children as clinically symptomatic. Therefore, additional information from another perspective, as for example nursery teachers, would be necessary.
A potential limitation of the study concerns the degree of representativeness of the study sample. This study sample appears to be representative of the general population of German preschool children with regard to the distribution of gender, age, SES, and geographical region. However, the study sample cannot be considered to be representative regarding the distribution of migration background and community area. Furthermore, the sample size is relatively moderate. Another limitation of the study is that no non-responder analysis was conducted as data of individuals who did not respond was not available. Therefore, differences between responders and non-responders regarding demographic characteristics could not be assessed.
Summary
The present study reports from a population based sample of German preschoolers aged 3–6 years. A possible mental disorder was indicated for 7.4 % of the preschoolers. Approximately 13 % of the preschoolers were judged as impaired by their parents. Regarding specific MHP, 4.2 % of the children had depressive and anxiety symptoms and 11.8 % showed hyperactive behaviour. Although low parental SES have been found to be associated with MHP in school age children, the present study could not find a significant association of SES with prevalence rates of overall and specific MHP, as well as impairment. The results of the BELLA preschool study showed that the prevalence estimates of MHP in preschoolers are similar to those assessed in later childhood, which supports the hypothesis of the continuity of MHP. As MHP may have a potentially persistent impact on the life of a child and thus may influence their education ability and social interaction [43], early identification of psychological problems and the promotion of mental health in early childhood institutions is needed [44].
This study highlights the importance of mental health promotion for all preschool aged children irrespective of sociodemographic characteristics.
References
Angold A, Egger HL (2007) Preschool psychopathology: lessons for the lifespan. J Child Psychol Psychiatry 48(10):961–966
Costello EJ, Egger H, Angold A (2005) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry 44(10):972–986
Anselmi L et al (2008) Continuity of behavioral and emotional problems from pre-school years to pre-adolescence in a developing country. J Child Psychol Psychiatry 49(5):499–507
Beyer T, Postert C, Mueller JM, Furniss T (2012) Prognosis and continuity of child mental health problems from preschool to primary school: results of a 4-year longitudinal study. Child Psychiatry Hum Dev 43(4):533–543
Kessler RC et al (2005) Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: results from the national comorbidity survey replication. Biol Psychiatry 57(11):1442–1451
Bufferd SJ, Dougherty LR, Carlson GA, Klein DN (2011) Parent-reported mental health in preschoolers: findings using a diagnostic interview. Compr Psychiatry 52(4):359–369
Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ (2009) The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. J Clin Child Adolesc Psychol 38(3):315–328
Esbjorn BH, Hoeyer M, Dyrborg J, Leth I, Kendall PC (2010) Prevalence and co-morbidity among anxiety disorders in a national cohort of psychiatrically referred children and adolescents. J Anxiety Disord 24(8):866–872
World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization, Geneva
Elberling H, Linneberg A, Olsen EM, Goodman R, Skovgaard AM (2010) The prevalence of SDQ-measured mental health problems at age 5–7 years and identification of predictors from birth to preschool age in a Danish birth cohort: the Copenhagen child cohort 2000. Eur Child Adolesc Psychiatry 19(9):725–735
Wichstrom L et al (2012) Prevalence of psychiatric disorders in preschoolers. J Child Psychol Psychiatry 53(6):695–705
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, vol 4. American Psychiatric Association, Washingtion
Heiervang E, Goodman A, Goodman R (2008) The Nordic advantage in child mental health separating health differences from reporting style in a cross-cultural comparison of psychopathology. J Child Psychol Psychiatry 49(6):678–685
Barkmann C, Schulte-Markwort M (2012) Prevalence of emotional and behavioural disorders in German children and adolescents: a meta-analysis. J Epidemiol Community Health 66(3):194–203
Rudolph S, Franze M, Gottschling-Lang A, Hoffmann W (2013) Developmental risks for social skills of 3-to 6-year-old children at day-care centers: prevalence and risk factors. Kindheit und Entwicklung 22(2):97–104
Furniss T, Beyer T, Guggenmos J (2006) Prevalence of behavioural and emotional problems among 6-years-old preschool children. Soc Psychiatry Psychiatr Epidemiol 41(5):394–399
McDonnell MA, Glod C (2003) Prevalence of psychopathology in preschool-age children. J Child Adolesc Psychiatr Nurs 16(4):141–152
Carter AS et al (2010) Prevalence of DSM-IV disorder in a representative, healthy birth cohort at school entry: sociodemographic risks and social adaptation. J Am Acad Child Adolesc Psychiatry 49(7):686–698
Smolny W (2009) Wage adjustment, competitiveness and unemployment—East Germany after unificaiton. J Econ Stat 229(2/3):130–145
Ravens-Sieberer U, Kurth B-M, KiGGS study group, Bella study group (2008) The mental health module (BELLA study) within the German health interview and examination survey of children and adolescents (KiGGS): study design and methods. Eur Child Adolesc Psychiatry 17:10–21
Kurth BM (2007) KiGGS—was kommt danach? Gesundheitswesen 69(10):548–554
Woerner W et al (2002) Normative data and evaluation of the German parent-rated Strengths and Difficulties Questionnaire (SDQ): results of a representative field study. Z Kinder Jugendpsychiatr Psychother 30(2):102–112
Goodman R (1999) The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry 40(5):791–799
Arbeitsgruppe Deutsche Child Behaviour Checklist (2002) Elternfragebogen für Klein- und Vorschulkinder (CBCL 1½–5). 2002, Köln: Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik (KJFD)
Atkins M, Milich R (1987) Iowa conners teacher rating scale. In: Hersen M, Bellack A (eds) Dictionary of behavioural assessment techniques. Pergamon Press, New York
Becker A, Woerner W, Hasselhorn M, Banasscheewski T, Rothenberger A (2004) Validation of the parent and teacher SDQ in a clinical sample. Eur Child Adolesc Psychiatry Suppl 13(2):II/11–II/16
Klasen H et al (2000) Comparing the German versions of the Strengths and Difficulties Questionnaire (SDD-Deu) and the Child behavior checklist. Eur Child Adolesc Psychiatry 9(4):271–276
Ezpeleta L, Granero R, de la Osa N, Penelo E, Domenech JM (2013) Psychometric properties of the Strengths and Difficulties Questionnaire in 3-year-old preschoolers. Compr Psychiatry 54:282–291
Stone LL, Otten R, Engels RCME, Vermulst AA, Janssens JMAM (2010) Psychometric properties of the parent and teacher versions of the Strengths and Difficulites Questionnaires for the 4- to 12- year-olds: a review. Clin Child Fam Psychol Rev 13:254–274
Achenbach TM (2000) Manual for the child behaviour checklist 1½–5. University of Vermont, Burlington, VT
Elting P Überprüfung der psychometrischen Parameter von CBCL 1 ½–5 und C-TRF an einer deutschen Stichprobe. Frankfurt am Main. Dissertation. Johann Wolfgang Goethe University
Conners CK (1969) A teacher rating scale for use in drug studies with children. Am J Psychiatry 126:884–888
Conners CK, Sitarenios G, Parker JD, Epstein JN (1998) The revised conners’ parent rating scale (CPRS-R): factor structure, reliability, and criterion validity. J Abnorm Child Psychol 26(4):257–268
Hosmer D, Lemeshow S (2000) Applied logistic regression, 2nd edn. Wiley, New York
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the numer of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Lüdtke O, Robitzsch A, Trautwein U, Köller O (2007) Handling of missing data in psychological research: problems and solutions. Psychol Rundsch 58(2):103–117
SPSS Inc. (2009) PASW statistics for windows. SPSS Inc., Chicago
Ravens-Sieberer U et al (2008) Prevalence of mental health problems among children and adolescents in Germany: results of the BELLA study within the national health interview and examination survey. Eur Child Adolesc Psychiatry 17(SUPPL. 1):22–33
Wille N, Bettge S, Wittchen H-U, Ravens-Sieberer U, BELLA Study Group (2008) How impaired are children and adolescents by mental health problems? Results of the BELLA study. Eur Child Adolesc Psychiatry 17:42–51
Burns BJ et al (1995) Children’s mental health service use across service sectors. Health Aff 14(3):147–159
Laucht M, Esser G, Schmidt MH (2000) Longitudinal research on the developmental epidemiology of mental disorders: aims, concepts and major results of the mannheim study of risk children. Z Klin Psychol Psychother 29(4):246–262
Dopfner M et al (1997) Psychic disturbances of children and adolescents in Germany: results of respresentative survey: method, age, gender, and rater effects. Z Kinder Jugendpsychiatr Psychother 25:218–233
Ihle W, Esser G (2002) Epidemiology of mental disorders in childhood and adolescence: prevalence, course, comorbidity and gender differences. Psychol Rundsch 53(4):159–169
Froehlich-Gildhoff K, Roennau-Boese M (2012) Prevention of exclusion: the promotion of resilience in early childhoof institutions in disadvantaged areas. J Public Health 20:131–139
Winkler J, Stolzenberg H (1999) Der Sozialschichtindex im Bundesgesundheitssurvey. Gesundheitswesen 2:178–183
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declared conflicts of interest.
Ethical Statement
This study has been approved by the appropriate ethics committee of Medical Faculty of the Charité Berlin and has been performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments (see page 4).
Additional information
Olga Wlodarczyk and Silke Pawils are joint first authors.
The BELLA Study Group: Ulrike Ravens-Sieberer, Claus Barkmann, Susann Bettge, Monika Bullinger, Manfred Döpfner, Michael Erhart, Beate Herpertz-Dahlmann, Heike Hölling, Franz Resch, Aribert Rothenberger, Michael Schulte-Markwort, Nora Wille, Hans-Ulrich Wittchen.
Rights and permissions
About this article
Cite this article
Wlodarczyk, O., Pawils, S., Metzner, F. et al. Mental Health Problems Among Preschoolers in Germany: Results of the BELLA Preschool Study. Child Psychiatry Hum Dev 47, 529–538 (2016). https://doi.org/10.1007/s10578-015-0586-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-015-0586-3