Abstract
Oppositional defiant disorder in childhood is a predictor of later mood disorders. This study assessed whether groups of children can be identified by their course of co-occurring oppositional and depressive symptoms in childhood using group based trajectory modeling. Participants were a cohort of 932 4 or 5 year old offspring of women participating in the National Longitudinal Study of Youth whose symptom trajectories were modeled across ages 4–13 years. Three co-occurring trajectory groups were found: oppositional symptoms only (23%), oppositional symptoms preceding increasing depressive symptoms over time (16%) and absence of any symptoms (61%). Of all children who developed depressive symptoms, all had moderate or high levels of pre-existing oppositional symptoms. Oppositional symptoms typically precede, or co-occur with depressive symptoms in childhood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oppositional defiant disorder (ODD) is the second most prevalent psychiatric disorder of childhood and the most common reason for clinic referral [1]. Community prevalence rates of ODD are 2–14% across childhood and adolescence, with substantially higher rates in clinical settings (28–50%) [2, 3]. Compared to other disruptive behaviour disorders of childhood, there are no clear sex differences in prevalence of ODD after adolescence, although in childhood, there is a higher prevalence of ODD in boys [4].
Epidemiological and clinical studies show that youth with ODD have high rates of externalizing and internalizing comorbidity; 92.4% of those with a lifetime diagnosis of ODD met criteria for another lifetime DSM-IVTR disorder (45.8% mood, 62.3% anxiety, 68.2% impulse control and 47.2% substance abuse) [5]. Despite the high rates of symptom comorbidity, recent longitudinal studies have shown that ODD symptoms in childhood most strongly predict depression in young adulthood [6]. The process by which this pattern of symptom development occurs (from oppositional to depressive) is not known. Two hypotheses have been posed. The first is the Failure Hypothesis [7] where depression is a result of youth experiencing high levels of failure or rejection because of their ODD behaviours. The second hypothesis is that oppositionality and depression are part of a developmental trajectory in children who have a temperamental profile high in negative affect. The latter possibility has been supported by research showing a cluster of ODD symptoms denoted as “irritable” (tempers, irritable, angry) is more strongly linked to depression than other ODD symptoms (e.g., defiance, argumentativeness, and being spiteful) [8, 9].
The studies of comorbidity and longitudinal prediction between oppositional and depressive symptoms across childhood suggest that oppositional symptoms are risk factors for depression. Based on the modest strength of the predictive associations, however, it is most likely that there are sub-groups of oppositional children who are at even greater risk for depression than other children with ODD. By estimating the proportion of children with oppositionality who develop depressive symptoms, hypotheses linking ODD and depression that are general (i.e., temperament) or more specific (only in instances of family conflict or peer rejection) can be developed.
Sex Differences in Trajectories Between Oppositional and Depressive Symptoms
It is unknown whether ODD is an equally strong predictor of depression in girls and boys. It is also unclear whether the developmental course is similar in girls and boys. Epidemiologic studies have identified that there are two peaks in prevalence of ODD, at ages 7 and 11 [4, 10]. Whereas boys make up the majority of early onset cases, the prevalence of ODD is similar in boys and girls in adolescence. This is the result of an increase in ODD prevalence in girls after age 12 [4]. It may be that potential risk processes contributing to girls’ oppositional symptoms in adolescence are associated with the female-specific increase in prevalence of depressive and anxiety disorders in that developmental stage [3]. As such, it may be that early childhood ODD predicts depression in adolescent boys but not adolescent girls. Comparing how the developmental trajectories of these symptoms unfold between boys and girls may suggest the presence of age- or stage- specific processes which may differ by sex. This information would offer opportunities for better identification of risk for depression as well as interventions for oppositional behaviour.
The two aims of this study were to determine the developmental course of co-occurring oppositional and depressive symptoms in childhood using group-based trajectory modeling and to determine whether boys’ and girls’ symptoms unfold in a developmentally similar pattern.
Identification of groups of children with different trajectories of co-occurring oppositional and depressive symptoms may be useful clinically depending on whether the trajectories differ in the temporal course of symptoms, and whether the trajectories are associated with differences in clinically identifiable predictors or outcomes. To this end, the third aim of the study was to compare how the trajectory groups were related to variables describing other aspects of children’s emotional and behavioural functioning. These variables included: whether the child was seen by a mental health professional for a behaviour or emotional problem, took medication for a behaviour problem, the severity of the mother’s depressive symptoms, child’s level of conduct or anxiety symptoms and a scale measuring motor and social development.
Methods
Participants
Data were drawn from the National Longitudinal Survey of Youth 1979—Child and Youth sample (NLSY79 CY; US Bureau of Labour and Statistics), a nationally representative sample of the offspring of 12,686 American women who were all between 14 and 21 years of age by December 31, 1978. Methods used in the study are explained in the NLSY User’s Guide [11]. Informed consent was obtained from these women in compliance with the policies of the US Bureau of Labour and Statistics. Assessments of each child as well as additional demographic and developmental information were collected from the mother. At the time of the child’s birth, 57% of mothers were married and their average age was 25.8 years (SD = 2.2) and 65.2% of women were living with the father of the child at the time of interview (1994). Forty-nine percent of the mothers were non-Black non-Hispanic, 22% were Hispanic and 29% were Black. The average family income in 1994 was $43,309 (SD = 21.212) and on average mothers had completed 12.6 years of formal schooling (SD = 2.3 years). Eight percent had a clinically elevated score (>11) on the Center for Epidemiologic Studies Depression Scale (CESD) [12].
The sample cohort included all children in the original NLSY sample (N = 385 girls and 444 boys) who were aged 4 years 1 month to 5 years 11 months in 1994 (N = 829) and had complete data on oppositional and depressive symptoms at 3 or more of the 5 assessment points (years 1994, 1996, 1998, 2000, and 2002, or Times 1, 2, 3, 4 and 5).
Missing Data
Of all participants eligible for inclusion in the analysis on the basis of age at Time 1 (N = 932), 88.9% (N = 829) had partial or complete data on oppositional and depressive symptoms at three or more time points across years 1994–2002. Missing data were handled with full information maximum likelihood (FIML) in PROC TRAJ [13], and data were assumed to be missing at random based on finding no significant association between the pattern of missing data between children with 5 waves of complete data (N = 508) and participants with 3 or 4 waves of complete data (N = 321) on any of the following baseline socio-demographic variables: maternal CESD score, maternal age at birth, years of education, family income, and single parent status.
Measures
Mothers of children aged 4 years 0 months to 5 years 11 months at Time 1 were interviewed biannually about their child’s problem behaviour in addition to other developmental, familial and social factors.
Depressive symptoms and oppositional behaviour were measured using the Behaviour Problems Index (BPI) [14]. The BPI has been used extensively in epidemiologic research and has been linked to many socio-demographic indicators including maternal depression, teenage parenting and marital disruption [15].
Unfortunately the BPI does not have separate sub-scales for oppositionality and depression. Specific items (N = 8) to represent depressive and oppositional constructs were selected from the BPI by the authors based on conceptual overlap with core symptoms of related psychiatric disorders [16]. The depression sub-scale included the four items: (1) child feels worthless or inferior, (2) child is unhappy/sad/depressed, (3) child is withdrawn, and (4) child complains no one loves them. The oppositional sub-scale also included four items: (1) child has a very strong temper, (2) child is stubborn/sullen/irritable, (3) child is disobedient at home, and (4) child argues too much. Parents reported on the frequency their child engaged in each of these behaviours during the past week using a three-point scale (1 = never to 3 = often) with scale scores ranging from 4 to 12. Internal consistencies were moderate, ranging from α = 0.62 (age 4–6) to α = 0.75 (age 12–14) for depressive symptoms, and from α = 0.75 (age 4–6) to α = 0.78 (age 12–14) for oppositional behavior. In a previous study, we showed that the oppositional and depressive symptom items loaded best on their respective factors and the factor structure of these items was stable over time using a longitudinal confirmatory factor analysis of maternal ratings across ages 6–10 [17].
Covariates
Covariates were selected from the NLSY, which correspond to known risk factors or correlates of oppositional behaviour or depressed mood. Covariates were measured in 1992 when the children were preschoolers or in 2004 (age 14–15) (i.e., prior to, and following, the measurement of the trajectories). Anxiety and conduct symptoms variables were measured in 1994 as these data were not available on this cohort in 1992.
Predictors (Measured in Preschool Years 1992 or 1994)
Maternal depression was assessed using the Center for Epidemiologic Studies Depression Scale (CESD) [12]. The original 20-item CESD rating scale was designed to measure severity of depressive symptoms in epidemiologic studies. It was administered to mothers at several points in the study. Data for this analysis consisted of maternal report in 1992 when the children were preschoolers. Symptom severity was measured by asking about the frequency of occurrence of each item over the preceding week, with items scored on a scale of 0 (rarely/never) to 3 (most or all of the time). Scores ranged from 0 to 60. The scale had good internal consistency in the general population (a = 0.84) [18], and correlated with the BDI (r = 0.86) [19]. Reliability in this sample was α = 0.76.
Medication use for disruptive or other behaviour was queried by asking the mother “Does your child regularly take any medicine to help control activity level or behaviour?” Response options were yes (1) or no (0).
Motor and social development was assessed using the Motor and Social Development Scale (MSD) which was developed by the National Center for Health Statistics to measure dimensions of the motor, social and cognitive development of young children from birth to 3 years. Items were derived from the 3 reliable and valid scales of infant and toddler development: The Bayley Scales of Infant development, the Gesell Scale, the Denver Developmental Screening Test [20]. Based on the child’s age stratified into 3 groups, mothers answered 15 items from a total of 48. Each item was dichotomous and the total raw score was obtained by summation of the items (range 0–15).
Anxiety and conduct symptoms were assessed using sub-scales from the BPI. Mothers reported on the frequency their child engaging in each of these behaviours during the past week using a three-point scale (1 = never to 3 = often) with scale scores ranging from 4–12 for conduct and 5–15 for anxiety. The anxiety sub-scale included five items: (1) child is high-strung/tense/nervous, (2) child is too fearful or anxious, (3) child has difficulty keeping their mind off thoughts, (4) child is too dependent on others, and (5) child worries too much. The conduct sub-scale included the four items: (1) child bullies or is cruel/mean to others, (2) child does not feel sorry for misbehaving, (3) child breaks things deliberately, and (4) child cheats or tells lies. Internal consistencies were α = 0.64 (age 4–6) for anxiety and α = 0.62 (age 4–6) for conduct symptoms.
Outcomes Measured in Adolescence (2002 or 2004)
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression scale (CESD-7) [21]. This shortened version of the original 20 item CESD depression rating scale was administered to youth biannually as part of the Youth Self Report component of the study in 2004 when youth were aged 14–15. Seven items were scored on a scale of 0 (rarely; 1 days/wk) to 3 (most of the time; 5–7 days/wk) with a score range of 0–21. It has been demonstrated that this scale has good reliability and validity in a college sample [22].
Anxiety and conduct symptoms were measured using sub-scales of anxiety and conduct from the BPI as previously mentioned. The same sub-scales as reported by mothers above were used, but measured in 2002 when youth were 12–13 years old. Note that this information was not available after 2002 for this cohort given the age of the youth. Reliability for the anxiety sub-scale was α = 0.76 (age 12–14) and α = 0.67 (age 12–14) for conduct symptoms.
Medication use (2004) was assessed by asking the youth “Do you regularly take any medicine to help control activity level or behaviour?” Youth response options were yes or no.
Mental health support received (2004) was assessed by asking the youth “Have you received any help for an emotional, behavioural or family problem in the last 12 months?” Youth response options were yes or no.
Analytic Plan
Modeling Single and Co-occurring Developmental Trajectories of Oppositional and Depressive Symptoms
Semi-parametric group-based methods were used to identify the number and shape of distinct trajectories of oppositional and depressive symptoms across the ages of 4–14 using 5 cycles of data [23]. With this method, individual variation over time is considered to be normally distributed within groups which themselves have distinct growth patterns. This assumption is useful for conceptualization and prognostication of clinical problem behaviour where the presence of groups of children with differing patterns of behaviour over time is assumed.
Models were estimated using the PROC TRAJ macro in SAS 9.0 [13]. Estimation of the trajectories proceeded in two steps: (1) selecting the number of trajectory groups, followed by (2) estimating the shape (slope) of each trajectory. Models were first estimated independently for boys and girls to confirm that no differences in trajectory shapes by sex were identified (data available from authors). As no differences were identified, data were combined across sexes and sex differences in proportion of the sample in each trajectory were calculated. To determine the optimal number of trajectory groups within the data, we used a censored normal model and several recommended practical fit indicators [23]. Maximization of the Bayes Information Criterion (BIC) among any of 1–6 class full quadratic models was first used to identify the maximum number of groups [24]. Very strong differences between BIC scores were considered in the range of 10 or more units, [25] as supported by the Bayes’ criterion calculation (eΔBIC between comparator models). To select the shape of each group, quadratic, followed by linear and zero growth factor options were specified as possibilities. The best fitting model was then chosen where all growth and intercept terms for each trajectory in the model remained statistically significant, and maximization of the BIC score was achieved. When multiple alternate models presented with similar BIC scores, the best model was chosen where: (1) trajectory groups had the least classification error (i.e., the average posterior probability for each assigned trajectory group >0.7, (2) the odds of correct classification for each trajectory were greater than 5, and (3) parsimony was achieved [26]. These data are available from the authors.
The co-occurring trajectory model of oppositional and depressive symptoms was then estimated. This procedure in PROC TRAJ uses parameter estimates from the previously estimated single trajectories to estimate conditional and co-occurring probabilities of each oppositional and depressive trajectory group in relation to each other. The output from this procedure identifies the proportion/relative probabilities of each co-occurring trajectory group (i.e., Which types of joint trajectory patterns are there, and how commonly do they occur in the sample?).
For a final model with 4 oppositional groups and 3 depressive symptoms groups, for example, there would be potentially 12 (4 × 3) co-occurring trajectory combinations. To make the description of the co-occurring trajectory groups more meaningful and parsimonious, each co-occurring trajectory identified, regardless of its sample size, was grouped with other similar co-occurring trajectories according to their most identifying characteristic (e.g., sharing high levels of oppositional symptoms across time as well as above-average or increasing levels of depressive symptoms across time).
Covariates Associated with Trajectory Group Membership
ANOVA was used to compare the co-occurring trajectory groups in terms of mean differences in the level of covariates measured in preschool and adolescence. The χ2 difference test was used for categorical covariates. As this analysis was conducted post hoc, it was underpowered and only trends in group effects were identified. The approach used was to examine first for the presence of overall group effect for a particular covariate. If present, the nature of significant differences in post hoc tests across the covariates was examined. Given multiple testing, Bonferroni correction was set at P < 0.015. The presence of statistically significant Z scores (>1.96) were examined for evidence of post hoc differences in the categorical covariates across the trajectory groups.
Results
Descriptive Statistics
The average level of oppositional behaviour for the sample decreased between 1994 and 2002 (age range 8–14) [t(769) = 2.55, P = 0.01] but increased across years 1998–2000 (age range 8–10) [t(645) = −2.60, P = 0.01] (Table 1). The average level of depressive symptoms increased over time (1994–2002) [t(690) = −5.10, P < 0.01] but did not differ significantly between each successive year. Wave to wave correlations within construct ranged between 0.45 and 0.65, suggesting stability across 2 years, although the magnitude of these correlations decreased with increasing time between assessment intervals. Concurrent covariation was moderate and steadily increased over time (ranging from 0.34 at Time 1 to 0.53 at Time 5).
Trajectories
Oppositional Behaviour
Full quadratic estimation suggested that a 4-group model (BIC = −6773.76, E = 1.59) provided a description of the data, which maximized model fit but ensured parsimony. The four single groups depicted in Fig. 1 were: (1) no symptoms (20%), (2) low stable symptoms (37%), (3) moderate decreasing symptoms (35%), and (4) high persisting symptoms (8%).
Depressive Symptoms. A 3 group full quadratic model (BIC = −4,242.96, E = 1.75) provided maximum fit and proposed the most parsimonious solution: (1) no depressive symptoms (43%), (2) low stable symptoms (40%), and (3) moderate and increasing symptoms (17%). These trajectories are depicted in Fig. 2.
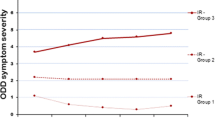
Co-occurring trajectories. The co-occurring trajectory model resulted in stable estimates of the original univariate trajectories, (BIC = −10,897.00, E = 1.75 for opposition and E = 1.75 for depressive symptoms) (data not shown). As can be seen in Table 2, a total of 12 possible co-occurring trajectory groups were identified (4 oppositional trajectories times 3 depressive trajectories). To facilitate presentation of the results and comparison across groups, three higher order joint trajectory clusters were identified by collapsing the 12 groups according to the dominant trajectory pattern observed:
Group 1: neither significant oppositional nor depressive symptoms (61%; none, low stable and moderate decreasing oppositional symptoms trajectories + none or low stable depressive symptoms trajectory),
Group 2: oppositional symptoms only (23%; high increasing oppositional symptoms + none or low stable depressive symptoms),
Group 3: both oppositional and depressive symptoms (16%; high increasing oppositional + high increasing depressive symptoms).
Sex Differences in Proportion of Sample in Each Trajectory
Although the shapes of trajectories did not differ across sex, there were differences in the proportion of boys and girls across oppositional (χ2(3) = 13.6, P = 0.003) and joint trajectory groups (χ2(2) = 12.1, P = 0.002) but not depressive symptom trajectory groups (X2(3) = 3.02, P = 0.22) (Table 3). There were significantly more girls in the low stable oppositional group 2 (34% boys vs. 43% girls) and significantly more boys in Group 3 (moderate symptoms; 36% boys vs. 29% girls) based on examination of standardized residuals in the differences in proportions across each trajectory group. Similarly, there were significantly more boys in the joint trajectory groups 2 (oppositional only; 29% boys vs. 21% girls) and 3 (both symptom types; 16% boys versus 11% girls), and more girls in Group 1 (no symptoms; 55% boys versus 67% girls).
Covariates Associated with Trajectory Membership
The mean scores or prevalence of covariates across the three co-occurring trajectory groups are presented in Table 4. For predictor variables measured prior to onset of trajectories, the level of psychological symptom variables (conduct, anxiety and maternal depressive symptoms) increased with severity of trajectories where levels of these symptoms were lowest in Group 1 and highest in Group 3. Motor and Social Development scores and frequency of medication use did not differentiate the trajectories at this age. For outcomes measured in adolescence, pairwise comparisons showed that the highest trajectory (Group 3) predicted significantly higher mean anxiety, conduct symptoms, youth-reported depression, and higher endorsement of medication use and visits to a mental health professional than other trajectories.
Discussion
In this study, longitudinal data collected from mothers about their children across the ages of 4–13 were used to identify single and co-occurring oppositional and depressive trajectories. Four oppositional and three depressive trajectories were identified along with three joint trajectory patterns.
The number and patterns of oppositional trajectories identified were similar to those found in another study which used a similar aged cohort [27], but with different oppositional items, attesting to the replicability of oppositional symptom trajectories in both boys and girls in childhood. The Bongers et al [27] study did identify an adolescent increasing oppositional trajectory which we did not. The fact that both studies identified similar trajectory shapes in boys and girls, (but admittedly overall higher symptom count in boys) suggests that the course of oppositional symptoms may not differ by sex; although boys are more likely to have higher levels of behaviour problems at any one time.
The three depressive symptom trajectories identified were consistent with depressive symptom trajectories identified in studies that also used maternal report CBCL items and sampled younger children (ages 2–11) [28, 29]. One difference in the present study was a larger proportion of children being assigned as having “no significant” depressive symptoms. This was because we identified fewer depressive symptom trajectories than other researchers, and chose to consider the high trajectory as being the only trajectory demonstrating “clinically significant” depressive symptoms. Another difference in the present study was the absence of identifiable sex differences in the shape or proportion of children in each depression trajectory. Dekker et al [28] identified a high chronic trajectory in girls and no such trajectory in boys, and a decreasing trajectory in boys only. The main difference between Dekker et al. and our study, other than the measures of symptomatology, was their longer duration of followup (age 4–18) which may allow the modeling of greater heterogeneity in slope, particularly across the pubertal transition when sex differences in depressive symptom severity emerge most prominently [30].
In our study, joint trajectory groups were notable by the absence of a group of children who had a trajectory course of consisting of only high depressive symptoms. One quarter of boys and girls manifest only oppositional symptoms—either stable or decreasing in severity—during childhood. Developmental linkages between the symptoms are evident in two ways: all children with depressive symptoms had early onset and elevated levels of oppositional symptoms, 40% of those with significant trajectories of oppositionality had concurrent trajectories of depressed mood. These findings together suggest that when present, depressive symptoms in childhood always co-occur with oppositionality, and childhood oppositionality, particularly when severe, heralds the later development of depressed mood. These findings are consistent with the clinical literature regarding comorbidity of ODD and other disruptive behaviour disorders in children in mood disorders seen in clinics [31, 32]. Given that these data are epidemiological and not clinical, it attests to the robustness of the association outside of the clinic environment in children of this age. Further, both of these symptom types when present tend to persist across childhood, particularly in those with the highest levels of symptoms and these particular children appear to be at very high risk of experiencing depression in adolescence, and to use mental health services and psychotropic medications more frequently than all other oppositional trajectory groups. These findings should encourage researchers to try to identify differences between children with severe oppositional behaviours (oppositional Group 4) from those whose behaviours are likely to decrease over time (oppositional Group 3).
The covariate associations we explored do not provide much guidance to this end. Although the trajectory group with both ODD and depression had worse outcomes compared to the other groups in adolescence, and higher levels of psychopathology in childhood, the differences were not sufficiently robust for prediction. We did explore post hoc whether the children with modest but reducing oppositional behaviours (oppositional Group 3) who were assigned to the high depressive symptom trajectory (depressive Group 3) differed from those who were oppositional but did not have depressive symptoms. The Group 3 children who were at risk for depression had higher levels of childhood anxiety and maternal depressive symptoms but not childhood conduct symptoms or medication use. Whether childhood anxiety in the presence of oppositional behaviours is a stronger predictor of later depressive symptoms or depression requires further exploration.
The finding of oppositional symptoms preceding increases in depressive symptoms in children more often than not suggests that oppositional behaviour may be an early harbinger of depressive symptoms in many children, possibly by the hypothesized mechanism of shared negative affect symptoms or anxiety symptoms. This study did not allow us to examine this specific hypothesis, but given that most (if not all) of the children in this study with high levels of depressed mood had co-occurring oppositional symptoms suggests that whatever risk processes are at play, they are active in early childhood. While this does not argue against the applicability of the failure hypothesis, it suggests that there may be common risk processes influencing both types of symptom manifestation that occur independently of adverse interpersonal experiences. An intermediate formulation is that the process of depression occurring as a consequence of criticism or rejection in children with disruptive behaviour (i.e., the failure hypothesis) occurs most markedly in children with anxiety or anxious temperament. It would be important to explore the significance of the failure hypothesis as a mechanism for depressive symptoms, and indeed whether family or peer criticism of children’s oppositional behaviour is a mediator of incipient depressive symptoms or, alternatively, whether such interpersonal “failures” temporally precede the onset of oppositional behaviours.
There are three main limitations of the methodology, which constrain the inferences drawn from the study. First, the symptom items available to model the trajectories were chosen from a scale not designed for this purpose. As such, the BPI provided a limited pool of appropriate items to represent the constructs. This was particularly evident in the constructs of conduct and anxiety at early ages where reliability of the item scale was low. Although previous work showed the oppositional and depressive symptom items could be easily assigned to their respective factors [17], these factors had moderate reliability which could have been increased by the availability of a larger pool of items to describe mood lability or irritability. The limited item selection to model the symptom factors was a tradeoff for the large sample size and longitudinal follow up offered by the NLSY.
We also note that this work cannot identify children who would be diagnosed with ODD or depression. The purpose of this study was to examine longitudinal covariation across all levels of symptom severity with the expectation that outlier patterns of symptoms could be used to identify distinct groups on the basis of this covariation. A dimensional symptom approach is appropriate for this question as clusters or factors of psychological symptoms are, in general, highly correlated, may be difficult to distinguish phenomenologically and are themselves a manifestation of correlated risk processes.
Another limitation is the “common rater” (mother) contributing to the rating of both oppositional and depressive symptoms. The rating of oppositional behaviour and depressive symptoms may vary depending on their context, the perceived motives of the child the presence of internalizing problems and the characteristics of the rater. As such, it will be important to replicate these findings with data from multiple informants using multiple methods. Replication with a larger sample will also be important as there was insufficient power to test levels of some covariates across the joint trajectory groups. Further, these trajectories require stringent external validity testing with additional outcomes and predictors beyond those used in this study.
The finding that high levels of oppositional symptoms occurred prior to the onset of high levels of depressive symptoms suggests that interventions to reduce oppositional behaviours may prevent the onset or the severity of depressive symptoms in adolescence. The challenge that follows is how to intervene with children’s oppositional behaviour as treatment has been informed by studies consisting mostly of boys with ODD and ADHD, where the major focus has been on teaching parents better behaviour management skills. The findings of this study suggest that given the high likelihood of depressive symptoms as a symptom outcome, the treatment of oppositionality may follow a depression paradigm, with the use of family based treatments, cognitive behaviour therapy, or antidepressant medications. Much work remains to determine whether this shift provides much needed benefit to a group at high risk of poor long term outcomes.
Summary
The present study tested for heterogeneity in the developmental course of co-occurring oppositional and depressive symptoms across childhood using group-based trajectory methods. We identified an association between high levels of oppositional and depressive symptom trajectories, where neither trajectory exists independently of the other. This suggests that children with high levels of depressive symptoms have early and co-occurring oppositional symptoms. There were no obvious sex differences in the trajectory patterns observed. Although descriptive in nature, this study suggests that oppositional behaviour in childhood is commonly accompanied by depressive symptoms and that further study of oppositional children is warranted. Questions such as how their family seeks services, how depressive symptoms are identified and how these children respond to treatment are likely to be important for the prevention and treatment of depression in childhood and adolescence.
References
Loeber R, Burke JD, Lahey BB, Winters A, Zera M (2000) Oppositional defiant and conduct disorder: a review of the past 10 years, part I. J Am Acad Child Adolesc Psychiatry 39:1468–1484
Angold A, Costello EJ, Erkanli A (1999) Comorbidity. J Child Psychol Psychiatry 40:57–87
Boylan K, Vaillancourt T, Boyle M, Szatmari P (2007) Comorbidity of internalizing disorders in children with oppositional defiant disorder. Eur Child Adolesc Psychiatry 12:484–494
Maughan B, Rowe R, Messer J, Goodman R, Meltzer H (2004) Conduct disorder and oppositional defiant disorder in a national sample: developmental epidemiology. J Child Psychol Psychiatry 45:609–621
Nock MK, Kazdin AE, Hiripi E, Kessler RC (2007) Lifetime prevalence, correlates, and persistence of oppositional defiant disorder: results from the national comorbidity survey replication. J Child Psychol Psychiatry 48:703–713
Copeland WE, Shanahan L, Costello EJ, Angold A (2009) Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry 66:764–772
Capaldi DM, Stoolmiller M (1999) Co-occurrence of conduct problems and depressive symptoms in early adolescent boys. IIII. prediction to young-adult adjustment. Dev Psychopathol 11:59–84
Stringaris A, Goodman R (2009) Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry 48:404–412
Burke JD, Hipwell AE, Loeber R (2010) Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. J Am Acad Child Adolesc Psychiatry 49:484–492
Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A (2003) Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 60:837–844
Center for Human Resource Research (2004) NLSY79 Child and young adult data users guide: a guide to the 1986–2002 child data and 1994–2002 young adult data. The Ohio State University, Columbus
Radloff L (1977) The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Jones BL, Nagin DS, Roeder K (2001) A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Method Res 29:374–393
Parcel TL, Menaghan ED (1988) Measuring behaviour problems in a large cross-sectional survey: reliability and validity of the NLS youth. Research report. Ohio State University Center for Human Resource Research, Columbus, OH
Peterson JL, Zill N (1986) Marital disruption, parent-child relationships, and behavior problems in children. J Marriage Fam 48:295–307
American Psychiatric Association (2001) Diagnostic and statistical manual of mental disorders. fourth edition - text revisions (DSM-IV-TR). American Psychiatric Association Press, Washington
Boylan K, Georgiades K, Szatmari P (2010) The longitudinal association of oppositional and depressive symptoms across childhood. J Am Acad Child Adolesc Psychiatry 49:152–159
Corcoran K, Fisher J (2000) Measures for clinical practice: a source book. Free Press: New York
Santor DA, Zuroff DC, Ramsay JO, Cervantes P, Palacios J (1995) Examining scale discriminability in the BDI and CES-D as a function of depressive severity. Psychol Assess 7:131–139
Poe GS (1986) Design and procedures for the 1981 child health supplement to the national health interview survey. Working paper series. National center for health statistics, Hyattsville
Ross CE, Mirowsky J, Huber J (1983) Dividing work, sharing work, and in-between: marriage patterns and depression. Am Sociol Rev 48:809–823
Santor D, Coyne J (1997) Shortening the CES-D to improve its ability to detect cases of depression. Psychol Assessment 9:233–243
Nagin DS (2001) Analyzing developmental trajectories: a semi-parametric, group-based approach. Psychol Method 4:139–157
D’Unger A, Land KC, McCall PL, Nagin DS (1998) How many latent classes of delinquent/criminal careers? Results from mixed poisson regression analyses of the London, Philadelphia and Racine cohort studies. Am J Sociol 103:1593–1960
Raftery AE (1995) Bayesian model selection in social research. Soc Method 25:111–163
Roeder K, Lynch K, Nagin D (1999) Modeling uncertainty in latent class membership: a case study in criminology. J Am Stat Assoc 94:766–776
Bongers IL, Koot HM, van der Ende J, Verhulst FC (2004) Developmental trajectories of externalizing behaviors in childhood and adolescence. Child Dev 75:1523–1537
Dekker MC, Ferdinand RF, van Lang ND, Bongers IL, van der Ende J, Verhulst FC (2007) Developmental trajectories of depressive symptoms from early childhood to late adolescence:gender differences and adult outcome. J Child Psychol Psychiatry 48:657–666
Sterba SK, Prinstein MJ, Cox MJ (2007) Trajectories of internalizing problems across childhood: heterogeneity, external validity, and gender differences. Dev Psychopathol 19:345–366
Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE (1998) Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol 107:128–140
Fristad MA, Verducci JS, Walters K, Young ME (2009) Impact of multifamily psychoeducational psychotherapy in treating children aged 8 to 12 years with mood disorders. Arch Gen Psychiatry 66:1013–1021
Luby JL (2009) Early childhood depression. Am J Psychiatry 166:974–979
Acknowledgments
This research was supported by a graduate fellowship from the Canadian Institutes of Health Research (KB) and a research training award from the Canadian Child Health Clinician Scientist Program (KB).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boylan, K., Vaillancourt, T. & Szatmari, P. Linking Oppositional Behaviour Trajectories to the Development of Depressive Symptoms in Childhood. Child Psychiatry Hum Dev 43, 484–497 (2012). https://doi.org/10.1007/s10578-011-0277-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-011-0277-7