Abstract
The present study examined the developmental trajectories of youth depression and anxiety symptoms from 6th through 12th grade in a low-income, urban sample (N = 141; mean age = 11.75 years; 88.7% African American). The study also tested the independent contribution of parent mood disorders, anxiety disorders, and substance use disorders assessed in early childhood to initial levels and rate of change in depression and anxiety symptoms from 6th through 12th grade. Possible gender differences in symptom course and strength of parent psychopathology predictors were examined using multiple-group analysis. Results indicated that depression symptoms declined over time for males, whereas depression symptoms initially declined, but then increased for females. In contrast, male and female adolescents each showed a decline in anxiety symptoms throughout adolescence. Findings also indicated that parent mood disorders were the only predictor of youth depression and anxiety symptoms for male and female adolescents in 6th grade. Parent anxiety disorders uniquely predicted the rate of change in depression symptoms among male adolescents. These results underscore the importance of targeting parents with mood and anxiety disorders in urban families in order to reduce the risk for internalizing difficulties in their adolescent youth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The urban environment is one with a multitude of adversities, including poverty, violence, and isolation [1]. While each of these circumstances alone is associated with significant risk, many urban youth experience these challenges in combination [2, 3]. Consequently, prior work has found that urban African American youth are at greater risk for psychological problems relative to youth in the general population [4, 5].
Although studies suggest that urban African American children are specifically at greater risk for externalizing problems [6, 7], several investigations have also indicated that these youth demonstrate elevated rates of internalizing problems. For instance, previous research has found anxiety symptoms and disorders among urban African American youth to equal or exceed rates among Caucasian youth [8–10]. Further, recent work indicates that the rate of suicidal behavior among African American youth is escalating [11] and markedly high among those who reside in urban areas [12, 13]. Despite the scale and significance of these problems, psychiatric disorders are persistently undertreated in this population [14, 15]. Moreover, identification of early factors that predispose urban African American youth to the development of internalizing problems may enable more timely and effective screening, recognition, and intervention.
Among predominantly Caucasian samples, a great deal of research has identified parent psychopathology as a critical factor in the development of youth internalizing problems [e.g., 16–19]. Although forms of parent psychopathology may differ considerably in clinical presentation and extent of impairment, several different types of parent psychopathology, including disorders of mood [16, 20–22], anxiety [18, 19, 23], and substance use [17, 24, 25], have mutually been found to increase the risk for youth internalizing problems.
An important question, however, is whether some forms of parent psychopathology have a greater impact on the development of specific types of internalizing problems among children relative to others. Knowledge of the differential impact of various forms of parent psychopathology on youth may guide where mental health resources should be allocated in environments where they are limited, such as low income, urban areas [14, 26]. Further, increased understanding of these risk factors may inform future prevention and intervention with children of psychologically-ill parents by guiding the scope of interventions and prioritizing both risk and need.
Specificity in Relations Between Parent and Child Internalizing Problems
According to the notion of specificity in the transmission of psychopathology [e.g., 27], children are at greatest risk for the type of psychopathology demonstrated by their parents. Whether due to biological (i.e., genetic vulnerability) or environmental mechanisms (i.e., parent modeling), the notion of specificity suggests that children of parents with mood and/or depressive disorders are more likely to experience mood problems relative to anxiety problems, and similarly but conversely, children of parents with anxiety disorders are at greater risk for anxiety problems relative to depression problems.
However, the majority of studies that have tested specificity in the expression of depression and anxiety problems have utilized a group comparison approach in which rates of disorder (i.e., when outcomes are dichotomous) or mean levels of symptoms (i.e., when outcomes are continuous) are examined across groups defined by parent diagnostic status. Although this approach may provide important information on observed differences between groups, it fails to control for the covariation that often occasions mood and anxiety disorders in adults [28]. In contrast, regression approaches allow investigators to examine the uniqueness of predictors in relation to a given outcome by including multiple predictors simultaneously and statistically controlling for their individual effects and covariation [29]. Regression approaches may also allow investigators to draw firmer conclusions with regard to the relative importance of a risk factor by revealing its independent contribution to an outcome.
Among the few studies that have utilized a regression approach to understand the specificity of relations between parent and youth internalizing problems, too little work has controlled for other highly comorbid conditions among parents. Of exception, Merikangas et al. [18] found that parent anxiety disorders predicted child anxiety disorders, after controlling for parent substance use disorders among families of Caucasian ethnicity. In addition, Biederman et al. [30] found that parent panic disorder and major depression each exerted independent effects on child anxiety disorders and major depression, respectively, after controlling for one another in a sample of primarily Caucasian families. Also of note, Chassin et al. [31] found that parent mood and alcohol use disorders predicted both child mood disorders and anxiety disorders, after controlling for each of parent mood, anxiety, and substance use disorders in a sample consisting predominantly of Caucasian families. Because comorbidity among mood, anxiety, and substance use disorders is highly prevalent [28, 32–34], and substance use disorders may be encountered at elevated rates among individuals of low income [35], it is of interest to consider all disorders in analyses to more accurately discern their independent effects on youth internalizing problems in this population.
Additionally, a number of areas merit further investigation in the study of specificity of relations between parent psychopathology and youth internalizing problems. First, because most studies, with few exceptions [e.g., 30, 31], have used concurrent or cross-sectional data to examine these relations, very little is known about the specificity of these predictors over time. Likewise, few studies have tested whether parent diagnoses longitudinally predict youth internalizing problems at a discrete time point as well as the rate of growth or decline in youth symptoms over time. Latent Growth Modeling (LGM) is a useful statistical approach that enables the modeling of both initial levels (intercept) and rate of change (slope) in problems over time, while also considering the individual variation in these parameters, in order to better elucidate longitudinal stability and change [36]. Knowledge of whether parent diagnoses impact the change in youth symptoms over time may yield additional information on the relative importance of a given predictor and provide clinically-relevant data on the most favorable time to intervene (i.e., intervention during stability or decline versus growth of symptoms).
Perhaps most important, almost all studies that have examined specificity in relations between parent psychopathology and youth internalizing problems have involved only Caucasian samples [e.g., 18, 37] or samples in which there were no African Americans represented [e.g., 31]. Indeed, even among studies in which African Americans were included, their representation was marginal [e.g., 19, 30, 38]. Further, with the exception of one study [i.e., 31], most work has examined this research question in predominantly middle to high income samples [e.g., 18, 30, 37, 38]. In view of evidence that the effects of parent psychopathology on youth internalizing problems may be strongest among populations of low socioeconomic status (SES) [38], it is necessary to examine how these risk factors operate in low income, urban communities in which African Americans predominate [6].
Developmental Course of Internalizing Problems Across Gender
Epidemiological studies involving primarily Caucasian youth that have examined the developmental course of depressive symptoms indicate that symptom levels may differ both by child gender and age. In particular, studies have found depressive symptoms to increase between the period of childhood and adolescence [39, 40], with some studies showing the elevation in symptoms to be more rapid among female adolescents relative to male adolescents [41]. These results have been replicated in several studies in which investigators have used LGM methodology to examine gender differences in the developmental trajectories of depressive symptoms throughout adolescence [42, 43].
Research examining the course of anxiety symptoms among predominantly Caucasian youth, in contrast, has generated mixed findings, with some studies showing increases during the period of adolescence [44], others showing decreases during this time [45, 46], and still others showing a stable pattern during the adolescent years [47]. Similar inconsistencies have been found among studies that have examined differences in anxiety problems across gender, with some studies finding female adolescents to display higher symptoms than male adolescents [46, 48], and others finding few, if any differences [49].
However, similar to research on relations between parent psychopathology and youth internalizing problems, the majority of this work has focused on exclusively Caucasian [e.g., 39, 40, 43, 45] or predominantly Caucasian samples [e.g., 41, 42, 47–49]. Likewise, many of these studies involved youth who lived in middle to high income households [e.g., 39, 45, 47, 48], although in some studies low to middle income families were included [e.g., 43] or individuals of low income were oversampled [e.g., 41, 49]. Notably, one study that examined developmental trajectories of adolescent depressive symptoms in a low-income, urban, exclusively African American sample found that symptoms were more likely to increase for female adolescents relative to male adolescents [50]. This study notwithstanding, additional longitudinal research on symptoms of depression and anxiety in low-income minority populations is needed to contribute to our empirical understanding of the developmental course of symptoms in these youth.
Goals and Hypotheses of Present Study
Given the evident rise in internalizing symptoms during the period of adolescence [51, 52], our aim was to examine parent psychopathology as a possible predisposing factor that might account for increases in youth internalizing symptoms during this developmental stage (6th–12th grade). Toward that end, the present study attempts to advance current knowledge of specificity in relations between parent psychopathology and youth internalizing problems among urban adolescent youth. Further, in consideration of documented disparities in symptom expression across adolescent gender [41, 48], we statistically tested differences both in growth trajectories and strength of parent psychopathology predictors across adolescent gender using multiple-group LGM analysis.
Therefore, the objectives of the current study were to examine each of the following in a predominantly African American, urban sample: (1) gender differences in the developmental trajectories of youth depression and anxiety symptoms during adolescence; (2) the independent contribution of parent mood disorders, anxiety disorders, and substance use disorders to youth depression and anxiety symptoms for male versus female adolescents; (3) the predictive strength of parent diagnoses on the initial levels as well as the rate of change in youth depression and anxiety symptoms over time for male versus female adolescents.
In consideration of previous work concerning the course of depressive symptoms in adolescence among both primarily Caucasian [42, 43] and urban African American youth [50], we expected that females would show higher initial levels of depressive symptoms and more rapid increases over time relative to males. We made no predictions with regard to the course of anxiety symptoms over time and across gender due to inconclusive findings in this area. Consistent with the notion of specificity [27], we also hypothesized that parent mood disorders and anxiety disorders would predict the initial levels and rate of change in youth depression and anxiety symptoms, respectively, after controlling for one another as well as for parent substance use disorders. Because of limited studies on the topic, we did not propose any hypotheses as to differences in the strength of parent psychopathology predictors on adolescent internalizing symptoms across gender.
Method
Participants
Participants included 149 families who took part in a larger, longitudinal study of two school-based, preventive intervention trials targeting learning, aggression, and social participation in nine Baltimore City public elementary schools [53].Footnote 1
Of the 678 families in the original sample, approximately one-quarter of the families (n = 175) were selected to participate in a more intensive study that included additional assessments of parent psychological functioning. Families were selected using a stratified random sampling procedure in which both high-risk and low-risk children were identified based on the number of depressive symptoms children endorsed on the Baltimore How I Feel-Young Child Version, Child Report [BHIF-YC-C; 54] in the fall of first grade. All children who endorsed 4 or more depressive symptom criteria (high-risk; n = 131) and a random probability sample of those with less than 4 depressive symptom criteria (low-risk; n = 44) according to the criteria for major depressive disorder described in the Diagnostic and Statistical Manual-III-Revised [DSM-III-R; 55] were recruited to participate. Among the 175 families that were identified using this procedure, 149 (85.1%) agreed to participate in the more intensive study. Eight adolescents (5.3%) were missing data on all outcomes of interest and were therefore excluded from analyses in the present study.
The remaining sample of 141 families (n = 45 control children; n = 55 children assigned to the classroom-centered [CC] intervention; n = 41 children assigned to the family-school partnership [FSP] intervention) included 133 female parents (94.3%) and 8 male parents (5.7%)Footnote 2 who ranged in age from 23 to 63 years (M = 33.8; SD = 7.5) when children were entering second grade. Of the parents, 84.4% (n = 119) were the biological parent of the child, 3.5% (n = 5) were the adoptive, step, or foster parent of the child, 2.8% (n = 4) were the grandparent of the child, 5.7% (n = 8) were another relative of the child, and 3.5% (n = 5) were a non-relative. Annual household income among these families ranged between less than $5,000–$70,000, with approximately 77.8% of these parents earning an annual household income of $30,000 or less.
The 141 adolescents were 51.1% male (n = 72) and 48.9% female (n = 69). Youth ranged in age between 6 and 8 years (M = 7.4; SD = 0.6) at the time of the first parent assessment (baseline) and between 11 and 13 years (M = 11.8; SD = 0.4) at the first time point of the present study (6th grade; Time 1). Youth ethnicity was 88.7% African American and 11.3% European American and the majority (71.6%) obtained free or reduced-price school lunch. There were no significant differences between male and female youth on the following clinical and demographic variables: prevalence of parent mood, anxiety, and substance use disorders, youth age, youth ethnicity, relationship to parent, free lunch status, and annual household income (all ps > .05).
Procedures
Procedures of the preventive intervention trials are described in detail elsewhere [e.g., 53]. For the present study, assessment of parent psychopathology was completed in the summer of first grade or the fall of second grade (i.e., baseline), between July 16th, 1994 and December 30th, 1994. Assessment of adolescent outcomes was gathered annually in the spring of 6th through 12th grade (Times 1–7, respectively). Following written informed consent, assessments occurred within the schools as well as at the Baltimore Prevention and Research Center.
Measures
Parent Psychopathology Predictors
Parental diagnosis was assessed using the Core Composite International Diagnostic Interview, Version 1.1 (CIDI)Footnote 3 [56]. The CIDI is a structured diagnostic interview that assesses the criteria for 14 DSM-III-R diagnoses including mood disorders, anxiety disorders, and substance use disorders. The psychometric properties of the CIDI have been shown to be both reliable and valid [57]. Parents were administered the CIDI the summer after children completed the first grade. Of the one-hundred and forty-one CIDI assessments used in the present study, a minority of assessments (n = 42; 29.8%) were conducted subsequent to this time period, with assessments completed from one day to 3.9 months after the summer of first grade (M = 1.5 months; SD = 1.1 months).
Fifty-two (36.8%) parents met criteria for at least one psychiatric disorder during this time. Parent psychopathology variables were created by collapsing parent psychiatric diagnoses into 3 categories: Parent Mood Disorders, Parent Anxiety Disorders, and Parent Substance Use Disorders. All mood, anxiety, and substance use diagnoses assessed with the CIDI [56] were categorized to be consistent with current Diagnostic and Statistical Manual of Mental Disorder nosology [DSM-IV-TR; 58]. The Parent Mood Disorders variable included major depressive disorder (n = 17), dysthymic disorder (n = 3), and bipolar I disorder (n = 4). The Parent Anxiety Disorders variable included panic disorder with agoraphobia (n = 1), panic disorder without agoraphobia (n = 3), agoraphobia without history of panic disorder (n = 11), specific phobia (n = 17),Footnote 4 social phobia (n = 13), generalized anxiety disorder (n = 2), and obsessive-compulsive disorder (n = 0). The Parent Substance Use Disorders variable included alcohol abuse (n = 7), alcohol dependence (n = 9), cannabis abuse (n = 2), cannabis dependence (n = 4), cocaine abuse (n = 0), cocaine dependence (n = 4), hallucinogen abuse (n = 0), hallucinogen dependence (n = 0), inhalant abuse (n = 0), inhalant dependence (n = 0), opioid abuse (n = 0), opioid dependence (n = 2), amphetamine abuse (n = 0), amphetamine dependence (n = 0), sedative, hypnotic, and anxiolytic abuse (n = 0), sedative, hypnotic, and anxiolytic dependence (n = 2), stimulant abuse (n = 0), stimulant dependence (n = 0), pcp abuse (n = 0), and pcp dependence (n = 0).Footnote 5
Values of the parent psychopathology variables were created by taking a count of the number of diagnoses in each category (i.e., if a parent had only social phobia, Parent Anxiety Disorders = 1; if a parent had social phobia + generalized anxiety disorder, Parent Anxiety Disorders = 2). Therefore, the range of scores for each parent psychopathology variable reflects the minimum and maximum number of psychiatric diagnoses parents demonstrated within each psychiatric category. Parent Mood Disorders scores ranged from 0 to 2, Parent Anxiety Disorders scores ranged from 0 to 3, and Parent Substance Use Disorders scores ranged from 0 to 5.
Our rationale for using this measurement approach in lieu of a count of total parent psychopathology symptoms or diagnostic criteria was threefold. First, because prior work examining relations between parent and child psychopathology [e.g., 18, 30, 31] has utilized measures of parent psychiatric diagnoses rather than symptoms, we chose to use a similar measurement method in order to facilitate synthesis and integration with the larger body of literature. Second, inherent in our approach to measurement is the CIDI implementation of computerized algorithms for the differential diagnosis of mood, anxiety, and substance use disorders [59]. Therefore, measurement of parent psychiatric diagnoses controlled for possible inflated parent psychopathology values by discounting symptoms of a diagnosis that were better accounted for by another condition. Third, given the sizeable correlations often observed between symptoms of depression and anxiety [60] as well as the high degree of symptom overlap across the mood and anxiety disorders [61], the potential for problems of multicollinearity among parent psychopathology variables derived from symptoms or criteria was prohibitive. Employing parent psychiatric diagnoses allowed us to capture parent psychiatric comorbidity while also managing problems of multicollinearity due to the lower magnitude of correlations among parent psychiatric variables obtained from diagnoses.
Of the 52 parents with psychiatric disorders, there were 21 (40.4%) who met criteria for at least one mood disorder, 34 (65.4%) who met criteria for at least one anxiety disorder, and 21 (40.4%) who met criteria for at least one substance use disorder. Approximately 19 (36.5%) of the parents with psychiatric disorders met criteria for more than one type of disorder (i.e., mood and anxiety, n = 6; mood and substance use, n = 2; anxiety and substance use, n = 6; mood and anxiety and substance use, n = 5). Of the 101 parent diagnoses, the onset of 89 (88.1%) of the diagnoses was greater than 1 year prior to the assessment. The average age of onset was 26.2 years (SD = 8.0) for Parent Mood Disorders, 14.4 years (SD = 7.2) for Parent Anxiety Disorders, and 24.8 years (SD = 7.5) for Parent Substance Use Disorders. In account of research that has found greater recency in onset of parent psychopathology to predict poorer child outcomes [e.g., 17], chi-square analyses were performed to determine that the recency in onset of parent diagnoses (i.e., within last year vs. greater than 1 year ago) did not differ across parent psychopathology domains. No tests were significant at p < .05, indicating a similar degree of recency in onset across the three domains of parent psychopathology.
Adolescent Internalizing Symptoms
Adolescents completed the Baltimore How I Feel-Adolescent Version Youth Report (BHIF-AY) as a measure of depressive and anxious symptoms each year from grades 6 through 12. The BHIF-AY is a 45-item measure in which adolescents report the frequency of depressive and anxious symptoms over the last 2 weeks on a four-point scale from “never” (0) to “most times” (3). The measure was created to serve as an initial stage instrument in a two-stage epidemiologic investigation of the prevalence of child and adolescent mental disorders as recognized in the DSM-III-R [55]. Because existing instruments did not directly parallel diagnostic criteria for the DSM-III-R mood and anxiety disorders, the BHIF-AY was designed and employed to meet this need. Items were derived from several sources, including from the DSM-III-R criteria for major depressive disorder, dysthymia, generalized anxiety disorder, separation anxiety disorder, social phobia, panic disorder, and agoraphobia, and from other psychometrically sound self-report instruments that measure the frequency of child emotional symptoms (i.e., the Children’s Depression Inventory [62], the Depression Self-Rating Scale [63], and the Spence Children’s Anxiety Scale [64]). Moreover, in the current study, the BHIF-AY was used as a broad assessment of symptoms consistent with several mood and anxiety disorders.
The BHIF-AY Depression and Anxiety subscales showed excellent internal consistency from 6th to 12th grade in the present study (i.e., Depression: α = .82 to α = .89; Anxiety: α = .86 to α = .90). In previous studies, the Depression and Anxiety subscales have demonstrated high internal consistency (i.e., α = .79 to α = .88) and excellent 2-week test-retest reliability (Depression: r = .83; Anxiety: r = .76) during the middle school years [54]. In terms of concurrent validity, Depression subscale scores were significantly associated with a diagnosis of major depressive disorder, whereas Anxiety subscale scores were significantly associated with a diagnosis of generalized anxiety disorder on the Diagnostic Interview Schedule for Children-IV when children were in the 6th grade (DISC-IV) [65]. With regard to predictive validity, scores on BHIF Depression subscale at 12 years of age significantly predicted a diagnosis of major depressive disorder on the DISC-IV 2 years later. The Depression and Anxiety Symptom variables at each time point consisted of the mean item score, with higher scores indicating a greater frequency of symptoms.
Data Analyses
A series of LGMs were estimated using the Mplus Version 5.1 software package [66] to identify the initial level and rate of change in adolescent depression and anxiety symptoms from 6th through 12th grade. Depression and anxiety symptoms were specified in separate LGMs to conserve statistical power and identify predictors unique to each outcome. The manifest variables were adolescent reports of these symptoms on the BHIF-AY at each of seven time points (i.e., spring of 6th through 12th grade). In every LGM, time was fixed incrementally and according to the spacing of assessment points, with a one unit difference between each successive time point (e.g., spring of 6th grade fixed at 1, spring of 7th grade fixed at 2, etc.).
Multiple-group analysis was used to examine differences across gender in initial levels of adolescent internalizing symptoms, changes in these symptoms over time, and the specificity and predictive strength of parent psychopathology domains. This approach was used rather than including gender as a covariate of the LGMs (i.e., Multiple Indicator Multiple Causes [MIMIC] approach) [67] because the covariate approach imposes strict assumptions concerning the equality of model measurement across gender (e.g., equal intercept and slope factor means, equal intercept and slope factor variances, equal residual variances, equal covariances) and structure (e.g., equal predictive relations). In contrast, the multiple-group framework imposes no assumptions with regard to measurement equality. In addition, whereas the covariate approach tests only for mean differences in variables across gender, the multiple-group approach determines whether relations among variables differ across gender.
Analysis proceeded in a number of steps. First, in order to accurately specify male and female LGMs in each multiple-group model, we created separate LGMs for males and females, conducting preliminary nested model comparisons to determine the appropriate trajectory shape of symptoms (i.e., intercept vs. intercept + linear slope vs. intercept + linear slope + quadratic slope). The two best-fitting models in each separate male and female LGM were used as a point of departure in our multiple-group base model.Footnote 6
Second, we examined whether the LGM measurement model was equal for males and females using an omnibus nested model comparison. This was achieved by comparing a model in which every parameter (i.e., intercept mean and variance, slope factor mean(s) and variance(s), covariance(s) among intercept and slope factor(s), and residual variances of manifest variables) was allowed to vary across gender groups (Model 1: All Free Measurement Model), to a nested model in which every parameter was constrained to be equal across gender groups (Model 2: All Constrained Measurement Model). Model 1 hypothesizes that males are different from females in every respect of symptom measurement, whereas Model 2 hypothesizes that males are similar to females in every respect of symptom measurement.
To compare the fit of the nested models, the difference between the chi-square values of models (\( \chi^{2}_{\text{diff}} \)) was examined in accordance with the formula recommended by Arbuckle and Wothke [68]. A significant chi-square difference value indicated that the more restrictive model (e.g., Model 2), fit significantly worse than did the less restrictive model (e.g., Model 1) [68].
If Model 2 fit significantly worse than did Model 1, we identified which parameter(s) differed across groups by constraining sets of parameters at a time, and comparing each constrained model to Model 1. In our Final Measurement Model, all parameters were constrained that did not result in a significant chi-square difference value when compared with Model 1.
We then tested whether parent psychopathology domains predicted initial levels and rate of change in internalizing symptoms across males and females. This was achieved by introducing the three parent psychopathology predictors (Parent Mood Disorders, Parent Anxiety Disorders, Parent Substance Use Disorders) simultaneously as correlated exogenous variables in the multiple-group LGM (see Fig. 1). Any possible intervention effects were controlled by including Intervention Group (1 = control group; 2 = CC intervention; 3 = FSP intervention) as an exogenous predictor that was free to vary across males and females in all models tested.
Both the intercept and slope factor(s) were regressed onto each of the four predictors and freely estimated across groups (Model 3: Free Parent Predictor Model). The resulting model was then compared to a model in which covariances among the parent psychopathology predictors and their regression paths to all outcomes were constrained to be equal across groups (Model 4: All Constrained Parent Predictor Model). Model 3 hypothesizes that there are differences in both the covariation among parent psychopathology predictors and the effect of parent psychopathology predictors on internalizing symptoms across gender, whereas Model 4 hypothesizes these parameters to be similar.
In addition to the chi-square difference tests, models were also evaluated using several different fit indices, including the chi-square to degree-of-freedom ratio (χ2/df; with values <3 and <5, indicating good and adequate fit, respectively), the Root Mean Square Error of Approximation (RMSEA; with values ≤.05 and ≤.08, indicating good and adequate fit, respectively), and the Tucker Lewis Index (TLI; with values ≥.95 and ≥.90 indicating good and adequate fit, respectively) [29]. Because the Root Mean Square Error of Approximation (RMSEA) may result in an underestimation of model fit in small samples [69], this criterion was not rigidly applied.
Missing Data
All observations were included in the analysis, consistent with the Full Information Maximum Likelihood approach used by Mplus. This approach, which treats data as missing at random [70, 71], is both well-accepted and has been shown to provide more accurate estimates than other methods such as casewise deletion, pairwise deletion, and data imputation [72–74]. Over 90% (n = 127) of these participants had at least four of the seven time points from grades 6–12. There were no significant differences between adolescents who were observed on all seven occasions (n = 97) and those who were missing data on one or more occasions (n = 47) on the following clinical and demographic variables: prevalence of parent mood, anxiety, and substance use disorders, youth anxious and depressive symptom levels, parent gender, parent age, youth ethnicity, youth gender, free lunch status (all ps > .05). Covariance coverage for the LGM measurement models ranged from .65 to .97, exceeding the minimum covariance coverage of 0.1 recommended for reliable model convergence [75].
Results
Descriptive Statistics
Skewness and kurtosis statistics for all youth symptom variables were within appropriate limits (<2 for skewness, <7 for kurtosis) [76]. The zero-order correlation matrices for all variables used in the analysis are displayed by adolescent gender in Tables 1 and 2. As is shown, Parent Mood Disorders were correlated with Parent Anxiety Disorders (rs = .32 to .39, ps < .05) and Parent Mood Disorders were correlated with Parent Substance Use Disorders (rs = .29 to .31, ps < .05). In addition, all parent psychopathology predictors were correlated with at least one measure of youth depression and anxiety symptoms over time. Measures of youth depression and anxiety symptoms were also correlated in successive years from 6th through 12th grade. Mean scores and standard deviations for all primary variables included in analyses are also presented by group in Table 3.
Youth Depression Symptoms
Measurement Model
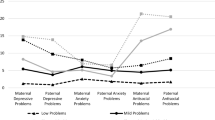
Preliminary nested model comparisons conducted separately for male and female adolescents indicated that an LGM with an intercept and linear slope factor provided the best fit to the data for male adolescents (χ2(23) = 27.49, p = .236; TLI = .967; RMSEA = .052), whereas an LGM with an intercept, linear slope factor, and quadratic slope factor provided the best fit to the data for female adolescents (χ2(22) = 27.14, p = .102; TLI = .953; RMSEA = .079). The observed and estimated depression symptom means from 6th through 12th grade are displayed by adolescent gender in Fig. 2. As is displayed, male depression symptoms exhibited a slight decreasing linear trajectory between 6th and 12th grade. In contrast, female depression symptoms displayed a quadratic trajectory, with depression symptoms decreasing from 6th through 9th grade, and then increasing from 10th to 12th grade.
These findings were incorporated into our baseline multiple-group model which tested differences in model parameters across gender. Given observed differences in trajectory shape across gender, the mean and variance of the quadratic slope factor were constrained to be zero among males in order to signify the absence of the quadratic slope factor. In addition, due to differences in linear factor interpretation when in the presence of a quadratic factor versus when in isolation, the linear slope factor parameters and covariances were allowed to vary across groups and only the intercept factor parameters were constrained to be equal in Model 2.
Model 1, in which all parameter estimates were allowed to vary across male and female adolescents, yielded a good fit to the data and provided a significantly better fit than did Model 2, in which residual variances, the intercept mean, and the intercept variance were constrained to be equal across groups (see Table 4). In order to identify how males and females differed, we conducted 3 nested model comparisons in which we constrained: (1) residual variances (Model 2a); (2) the intercept mean (Model 2b); and (3) the intercept variance (Model 3b). We compared these 3 resulting nested models to Model 1. Models 2b and 2c each resulted in a significantly worse model fit. However, Model 2a, in which all parameters but the residual variances were free to vary across groups, did not significantly differ from Model 1 (see Table 4). Therefore, Model 2a was retained as the Final Measurement Model in the interest of parsimony. In this model, among males, the mean of the intercept and linear slope factors were 0.633 (SE = 0.05) and −0.036 (SE = 0.01), respectively (all ps < .001). The variance of the intercept and linear slope factors were 0.126 (SE = 0.03, p < .001) and 0.006 (SE = 0.002, p < .01). The intercept and linear slope factors were also significantly correlated with one another (−0.016, SE = 0.01, p < .05), indicating that male adolescents with higher depression symptoms in 6th grade had a faster decline in depression symptoms over time. Among females, the mean of the intercept, linear slope, and quadratic slope factors were 0.971 (SE = 0.07), −0.131 (SE = 0.04), and 0.016 (SE = 0.01), respectively (all ps < .001). The variance of the intercept, linear slope and quadratic slope factors were 0.257 (SE = 0.06, p < .001), 0.078 (SE = 0.02, p < .001), and 0.002 (SE = 0.001, p < .01), respectively. The intercept and linear slope factors for females were also significantly correlated with one another (−0.079, SE = 0.03, p < .05), suggesting that female adolescents with higher 6th grade depression symptoms had a faster decline in depression symptoms over time.
In addition to differences in trajectory shape across gender, these results also indicate that female adolescents displayed higher mean levels of depression symptoms in 6th grade than did male adolescents (intercept mean: females = 0.971 vs. males = 0.633). Results also suggest that female adolescents showed greater variability in their depression symptom levels in 6th grade compared to male adolescents (intercept variance: females = 0.257 vs. males = 0.124).
Parent Predictor Model
As noted above, because of differences in the trajectory shape of depression symptoms across male and female adolescents, only the equality of covariances among parent psychopathology predictors and of regression paths from parent psychopathology predictors to the intercept factors were tested across gender groups. Model 3, in which these parameters were free to vary, provided an adequate fit to the data. Model 4, in which these parameters were constrained to be equal across groups, also provided an adequate fit to the data and did not significantly differ from Model 3 (see Table 4). Therefore, this model was retained as the Final Parent Predictor Model.
These results suggest that there were no significant differences in strength among covariances of parent psychopathology predictors across gender. In addition, males and females did not differ in the strength of regression paths between parent psychopathology predictors to depression symptoms in 6th grade (intercept). Consistent with the specificity hypothesis which suggests that Parent Mood Disorders will independently predict depression symptoms among youth, only Parent Mood Disorders predicted greater depression symptoms in 6th grade for male and female adolescents, after controlling for other parent psychopathology (β = 0.22, p < .05). However, counter to this hypothesis, only Parent Anxiety Disorders predicted a slower decline in depression symptoms among male adolescents (β = 0.03, p < .05). No parent psychopathology variable predicted change in depression symptoms over time among female adolescents. Specific parameter estimates of the Final Parent Predictor Model are displayed in Table 5.
Youth Anxiety Symptoms
Measurement Model
Preliminary nested model comparisons conducted separately for male and female adolescents indicated that LGMs including an intercept, linear slope, and quadratic slope factor provided the best fit to the data (Males: χ2(22) = 29.63, p = .128; TLI = .942; RMSEA = .069; Females: χ2(22) = 38.61, p = .016; TLI = .924; RMSEA = .105). Because the variance of the quadratic factor was zero and nonsignificant in both of these models, we treated it as a fixed effect. The observed and estimated anxiety symptom means from 6th through 12th grade are displayed by adolescent gender in Fig. 3. As is shown, male and female anxiety symptoms displayed a quadratic trajectory over time, with anxiety symptoms decreasing from 6th through 9th grade, and then remaining constant from 10th to 12th grade.
These separate models were used to inform our baseline multiple-group model. Model 1, in which parameter estimates were allowed to be different across male and female adolescents, yielded an acceptable fit to the data and did not significantly differ from Model 2, in which all parameters were constrained across groups. As such, Model 2 was retained as the Final Measurement Model in the interest of parsimony (see Table 4). In the Final Measurement Model, the means of the intercept, linear slope, and quadratic slope factor were 0.815 (SE = 0.05), −0.162 (SE = 0.02), and 0.016 (SE = 0.003), respectively (all ps <.001). The variances of the intercept and linear slope factors were 0.183 (SE = 0.03) and 0.005 (SE = 0.001), respectively (all ps <.001). The correlation between the intercept and linear slope factor was significant and negative (−0.019, SE = 0.005, p < .001), suggesting that children with higher anxiety symptoms in 6th grade had a faster decline in anxiety symptoms over time.
These results indicate that male and female adolescents exhibited similar levels of anxiety symptoms in 6th grade (intercept mean) and display similar rates of change in anxiety symptoms from 6th through 12th grade (linear slope and quadratic slope means). Results also suggest that male and female adolescents showed comparable degrees of variability in each of these parameters (intercept variance, linear slope variance, quadratic slope variance).
Parent Predictor Model
Model 3, in which covariances among the parent psychopathology predictors and relations from these predictors to the intercept, linear slope, and quadratic slope factor of the LGM were allowed to be different across male and female adolescents, provided an acceptable fit to the data and did not significantly differ from Model 4, in which these parameters were constrained across gender groups (see Table 4). Moreover, Model 4 was retained as the Final Parent Predictor Model.
These findings demonstrate that there were no significant differences in strength among covariances of parent psychopathology predictors across gender. There were also no differences across gender in the strength of predictive relations between parent psychopathology variables to anxiety symptoms in 6th grade (intercept) and to the rate of change in anxiety symptoms over time (linear and quadratic slope). Counter to the specificity hypothesis which suggests that Parent Anxiety Disorders will independently predict anxiety symptoms among youth, only Parent Mood Disorders predicted greater anxiety symptoms in 6th grade among male and female adolescents, after controlling for other comorbid parent psychopathology (β = 0.24, p < .05). No other parent psychopathology variable was a significant predictor of anxiety symptoms in 6th grade, nor did any parent psychopathology variable predict change in anxiety symptoms over time. Specific parameter estimates of the Final Parent Predictor Model are displayed in Table 5.
Discussion
The present study sought to expand previous work on internalizing problems in urban youth by: (1) examining the course of depression and anxiety symptoms during adolescence; (2) determining the independent contribution of parent mood, anxiety, and substance use disorders assessed in early childhood to youth depression and anxiety symptoms in adolescence; and (3) testing whether parent diagnoses predict initial levels as well as the rate of change in youth depression and anxiety symptoms over time. By utilizing a multiple-group analysis approach, we were able to examine gender differences among youth in each of these areas.
Developmental Course of Internalizing Problems Across Gender
As hypothesized, female adolescents showed higher mean levels of depression symptoms in 6th grade relative to male adolescents. These findings are consistent with an abundance of prior work involving both primarily Caucasian [42, 43, 77] and African American youth [50] that has found adolescent females to endorse greater depression symptoms relative to adolescent males. We also found that female adolescents evidenced greater variability in 6th grade depression symptoms than did male adolescents. Although we are aware of no previous studies that have tested gender differences in the variability of 6th grade depression symptoms, these results may be a function of female adolescents’ tendency to display a range of mild to moderate depression symptoms and male adolescents’ tendency to display only mild symptoms in 6th grade. Post-hoc examination of the range in 6th grade depression symptom scores across male and female adolescents supports the contention that females endorsed mild to moderate symptoms, while males endorsed only mild symptoms (i.e., females: 0–2.5; males: 0–1.79). Whether such differences in variance are due to genuine differences in symptom variability or broader sociocultural factors such as the tendency among males to underreport symptoms of depression [e.g., 78] may be an area for future work.
While we expected female youth to also demonstrate more rapid increases in depression symptoms relative to males, the growth functions of male and female youth were not directly comparable due to differences in trajectory shape across gender groups. In particular, whereas male depression symptoms consistently declined from 6th through 12th grade, female depression symptoms decreased from 6th through 10th grade, but increased thereafter. Though these findings differ from one investigation of primarily Caucasian youth that found linear increases in depression symptoms throughout adolescence for males and females, with more rapid increases among females [42], it is important to note that these authors employed a time frame of only 3 years for each growth model. If a longer time interval and/or more assessment occasions were included in each model, it is possible that our findings would be similar.
Our results do approximate the findings of one study involving mostly Caucasian youth that spanned a time interval of 9 years in which the investigators found mean depression symptoms to initially decrease and then increase for females, and to decline steadily for males, over the period of adolescence [41]. Also consistent with our results, another study of Caucasian youth involving four assessment points found a LGM including a quadratic factor to fit well among females, but not males [43]. Additional longitudinal research with multiple measurement occasions will be helpful in clarifying the shape of depression symptoms across males and females in other urban community samples.
Although developmental trajectories of youth depression symptoms differed by gender, male and female youth displayed similar trajectories of anxiety symptoms from 6th through 12th grade. In addition to showing similar mean levels and variability in anxiety symptoms in 6th grade, males and females also displayed a similar trajectory shape, mean rate of change, and variability in rate of change over time. While these results contrast with some studies including primarily Caucasian samples that have found females to show greater anxiety symptoms relative to males [46, 48], such discrepant results are likely due to differences in the ages of participants across studies. For example, several longitudinal studies involving predominantly Caucasian youth have found significant differences in anxiety symptoms to emerge only in late adolescence (i.e., 16 years) rather than early adolescence (i.e., 11–12 years) [45, 79]. Further, other research in mostly Caucasian samples has found no gender differences in levels of anxiety symptoms among younger adolescents [80, 81], whereas studies of older Caucasian [46, 48] and African American adolescents [82] have detected such differences. In consideration of this work, it is possible that we failed to observe differences in anxiety symptoms across gender because differences in mean levels and variation in anxiety symptoms were tested during the early adolescent years (i.e., M = 11.8).
With regard to the course of anxiety, we found anxiety symptoms to initially decrease over time from 6th through 10th grade and then to remain fairly stable from 10th through 12th grade. Although these results conflict with one prior study of Caucasian youth that has found anxiety problems to increase from childhood to adolescence [44], they are consistent with other research involving primarily Caucasian youth that has found anxiety symptoms to remain stable [47] or decline over time [45, 46]. Indeed, research with both Caucasian [83] and mixed ethnic samples [84] indicates that changes over time in anxiety problems may be more a matter of kind than degree. For instance, studies have found some types of anxiety symptoms (i.e., panic, school, separation, and social), to decline or remain stable during adolescence [45, 47, 85, 86]. Because the majority of items on the BHIF-AY (i.e., 60%) reflect panic, school, separation, and social concerns, the overall decrease in anxiety symptoms over time is appropriate to our assessment of youth anxiety. In the future, it will be important for longitudinal research to disaggregate subtypes of anxiety in order to better understand variations in the course of anxiety by symptom subtype.
With minimal exceptions [e.g., 42, 44], results of the course of youth depression and anxiety symptoms across gender in our sample were remarkably similar to studies that have examined this research question in predominantly Caucasian [e.g., 41, 43, 45–47] and middle to high income samples [45, 47]. Such similar findings are interesting given the disparities in ethnicity and sociocultural context in which each population is embedded. It is possible that the normative and gender-specific variations in internalizing symptoms throughout adolescence supercede differences that may be due to the sociocultural factors (i.e., ethnicity, income, urbanicity) commonly associated with greater risk. However, it is important to note that while the pattern of symptom change across these populations appears to be similar, levels of symptoms and the magnitude of change across sociocultural groups may differ. Future longitudinal research involving adolescent youth of various ethnicities, socioeconomic strata, and areas of residence are needed to allow direct comparisons of how the level and magnitude of change in internalizing symptoms may vary by these sociocultural features.
Specificity in Relations Between Parent and Youth Internalizing Problems
The current study found partial support for the specificity hypothesis. In accordance with this hypothesis, parent mood disorders uniquely predicted mean levels of depression symptoms in 6th grade for both male and female adolescents, after controlling for other comorbid parent psychopathology. On the contrary, findings did not support the specificity hypothesis with regard to youth anxiety symptoms. Though we expected parent anxiety disorders to independently predict youth anxiety symptoms in 6th grade, only parent mood disorders predicted mean levels of anxiety symptoms in 6th grade for male and female adolescents. In view of several studies that have found strong relations between parent and child anxiety problems [e.g., 18, 19, 30, 38, 87], these results are somewhat counterintuitive. However, it is important to note that almost all of these studies with the exception of one [i.e., 30], have utilized cross-sectional or concurrent data and none have controlled for each of parent mood, anxiety, and substance use disorders in analyses. These differences in experimental design and analytic approach may account for the observation of relations between parent and youth anxiety in previous studies and the failure to detect these relations in the current study.
Consistent with this notion, Chassin and colleagues [31] found only parent mood disorders and substance use disorders, not anxiety disorders, to longitudinally predict both youth depression and anxiety problems in a study in which all three forms of parent psychopathology were statistically controlled in analyses. Our failure to also observe relations between parent substance use disorders and youth outcomes may be due to the lower number of substance-abusing parents in our study relative to the study conducted by Chassin and others [31] (i.e., 40% of parents vs. 54% of parents). Alternatively, because many substance-abusing parents in the Chassin et al. [31] study were recruited via court records rather than sampled from the community, it is possible that they were more deviant in their substance use, leading to greater youth internalizing problems than those observed in the current study. Such differences in sample characteristics may have lead to the presence vs. absence of significant longitudinal relations between parent substance use disorders and youth internalizing symptoms across these two studies.
These findings may also be unique to our study population. That is, previous studies that have found parent anxiety disorders to predict similar problems in children [e.g., 18, 19, 30, 38, 87] have involved primarily Caucasian families from middle to high income households. Therefore, it is possible that parent mood disorders are more strongly related to youth depression and anxiety symptoms in 6th grade for urban African American youth relative to youth in the general population. For example, one large epidemiological study using a nationally representative sample found that adult mood disorders were classified as severe and impairing more frequently than were adult anxiety and substance use disorders [28]. Further, prior research has found adult psychopathology to be more persistent among African American adults relative to Caucasian adults [88]. Taken together, such clinical characteristics may have led to greater role dysfunction over longer periods for parents with mood disorders in the current sample, thereby accounting for the stronger impact of this diagnosis on youth depression and anxiety problems in 6th grade. Given the pervasive effect of parent mood disorders assessed in early childhood on levels of youth depression and anxiety symptoms in adolescence, it may be important to consider and address this diagnosis among urban minority parents early in their child’s developmental course. Such early identification and intervention with families may reduce the risk for later internalizing difficulties among urban adolescent children.
Although we expected both parent mood and anxiety disorders to predict changes in youth depression and anxiety symptoms from 6th through 12th grade, respectively, only parent anxiety was a significant predictor of the rate of change in youth depression symptoms over time. Further, this effect was limited to male youth. While these results were unanticipated, one prior study involving predominantly Caucasian youth also found parent anxiety to impact the rate of change in child internalizing symptoms among males, but not females [89]. It may be that parent anxiety has a greater impact on depression symptoms for male as opposed to female adolescents due to gender-role socialization practices. Toward this end, certain parenting behaviors observed among parents with anxiety disorders, such as overcontrol/overprotection [23] may undermine adolescent attempts at greater autonomy as they enter a developmental context that increasingly demands accomplishing this task [90]. While such parental restrictions may be of particular significance for males who are exposed to gender norms that emphasize independence over interpersonal relatedness [91], they may be of even greater significance for African American males who develop in a culture that highlights the importance of male strength and control [92]. Future work that focuses on these and other environmental factors may enable the identification of more powerful predictors of change in internalizing symptoms over time among urban adolescent youth.
Limitations
The results of this study should be considered within the context of several limitations. First, because the severity and duration of parent diagnoses were not assessed, it is possible that these clinical features had a greater impact on youth internalizing symptoms than did diagnosis type, per se. However, the average age of onset for all domains of parent psychopathology either predated or closely coincided with parents’ age at the time their children were born (i.e., between 25.8 and 27.8 years old), providing some evidence that children were exposed to parent psychopathology for a similar duration, regardless of the type of parent psychopathology. Additional research that considers such aspects of disorder as well as any environmental epiphenomena (i.e., impairments in parenting and/or family functioning) will be helpful in revealing why parent mood and anxiety disorders may predict poorer outcomes among low income, urban community samples.
Second, although our measure of parent psychopathology was derived from a dichotomous instrument, it is possible that a continuous measure of parent psychopathology would enable a broader representation of parent psychiatric severity and impairment. In the future, it will be useful for investigations to employ both dichotomous as well as continuous measures of parent psychopathology in order to provide a more refined assessment of parent pathology and symptom presentation.
Third, due to limited statistical power, it was not possible to test a parallel process of youth depression and anxiety symptoms, while controlling for their covariation in a single model. However, post-hoc Monte Carlo power analyses indicated that the current sample size was more than adequate to detect moderate to large effects with sufficiently high power (i.e., ≥.80) in the models we tested. In addition to replicating findings of the current study, it will be necessary for larger, longitudinal studies of urban youth to contribute to our understanding of the specificity of youth outcomes.
Fourth, it is possible that early reductions in aggression and problem behavior among children in the intervention groups indirectly decreased the risk for later depression and anxiety symptoms in adolescence [e.g., 93], thereby reducing the representativeness of these symptom trajectories for African American, urban youth at large. Yet, it is important to note that the symptom trajectories observed in measurement models were similar after we controlled for possible intervention effects in conditional models.
Finally, the selection and characteristics of the current study sample may limit the degree to which findings may generalize to other samples or populations. In particular, because the present sample consisted primarily of high-risk, urban African American youth, results of this study may not extend to the general population. Perhaps demonstrating this idea, the rates of psychiatric diagnoses among parents in our sample differ somewhat from rates found in general population samples that have employed the same diagnostic interview [e.g., 94], with higher lifetime rates of agoraphobia, bipolar I disorder, and substance dependence and lower rates of several mood (i.e., major depressive disorder), anxiety (i.e., social phobia, generalized anxiety disorder, obsessive compulsive disorder) and substance use disorders (i.e., alcohol abuse, alcohol dependence, drug abuse). However, similar to the psychiatric profile of our study sample, previous epidemiological studies have also found elevated rates of agoraphobia [95], bipolar I disorder [96] and substance dependence [97], and lower rates of other mood, anxiety, and substance use disorders [88, 94] among African American adults relative to Caucasian adults. Therefore, although our sample may not be representative of the larger population, it is likely representative of the urban African American population. Future studies including both general population and minority samples will be necessary to better understand whether the results of this study are universal or sample specific.
Clinical Implications
Over and above these limitations, the current study contributes to our empirical knowledge and clinical understanding of depression and anxiety symptoms in urban youth. It further provides data on the relations between parent psychopathology and youth depression and anxiety symptoms in adolescence. This study is among the first to examine the specificity of relations between parent mood, anxiety, and substance use disorders to youth depression and anxiety symptoms in this population. It is also among the first to examine whether parent psychopathology in early childhood impacts these symptoms throughout adolescence for male versus female youth. Although all forms of parent psychopathology may impose risk to children [98], findings of this study specifically suggest that parent mood disorders are a robust risk factor for the development of internalizing symptoms in this population. Findings also revealed that parent anxiety is a unique risk factor for depression symptoms among male adolescents. Because parent psychopathology can be assessed early in child development and mood and anxiety disorders can be effectively treated in low-income, minority populations [99–101], future intervention efforts targeting parents with internalizing disorders may be important in the prevention of later internalizing difficulties among low-income, urban youth.
Summary
The current study aimed to advance prior work that has investigated internalizing symptoms among urban, low-income youth by: (1) examining the developmental course of youth depression and anxiety symptoms from 6th through 12th grade; (2) testing the unique contribution of parent mood disorders, anxiety disorders, and substance use disorders assessed in early childhood to youth depression and anxiety symptoms in adolescence; and (3) determining the independent effect of parent mood, anxiety, and substance use disorders on initial levels as well as the rate of change in youth depression and anxiety symptoms throughout adolescence. The study employed a multiple-group LGM analysis in order to examine differences in both the course of youth internalizing symptoms as well as the predictive strength of parent diagnoses. Results demonstrated that male depression symptoms consistently declined from 6th through 12th grade, whereas female depression symptoms decreased from 6th through 10th grade, but increased thereafter. Results concerning the course of anxiety symptoms indicated that male and female youth displayed a similar decline in anxiety symptoms from 6th through 12th grade. Providing support for the notion of specificity [27], findings also indicated that parent mood disorders uniquely predicted youth depression symptom in 6th grade. In contrast to this hypothesis, however, parent mood disorders, not anxiety disorders, also predicted youth anxiety symptoms in 6th grade. Further, parent anxiety disorders independently predicted the rate of change in youth depression symptoms, but not anxiety symptoms, among male adolescents. Findings of this study suggest that reducing the risk for internalizing problems among urban adolescent youth may begin with early identification of these problems in their parents.
Notes
In each of the nine schools, three first-grade classrooms were randomly assigned to one of three conditions: (1) a classroom-centered (CC) intervention involving an enhanced curriculum, a classroom game in which student teams were contigently reinforced for exhibiting compliant, on-task, non-aggressive, and prosocial behavior (Good Behavior Game) [102], and weekly instruction in problem-solving skills; (2) a family-school partnership (FSP) intervention involving teacher training in parent-teacher communication [103], weekly home-school communication and learning activities, and nine parent workshops focused on both parent-school collaboration [104, 105] and enhancing parent discipline [106]; and (3) a standard setting or control condition. Interventions were provided over the course of first-grade. Relative to the control condition, children in the CC condition showed significantly higher academic achievement and fewer aggressive behaviors in second grade, and they were less likely to display conduct problems in sixth grade. Although children in the FSP condition also showed fewer problems than did children in the control condition, the effects of the FSP condition were more circumscribed and modest than the CC condition [53].
Nested model comparisons were also conducted without male parents. Because results were the same in either case, they are presented for the entire sample.
In order to reduce assessment burden, CIDI supplemental modules were not included in the interview. Therefore, diagnoses of posttraumatic stress disorder were not assessed.
Most parents diagnosed with a specific phobia also presented with one or more other anxiety disorders (n = 11; 64.7%), thereby weakening the possibility that the impact of Parent Anxiety Disorders on youth outcomes would be underestimated due to the inclusion of this diagnosis. However, in an attempt to reach a more comparable level of functional severity across parent diagnostic categories, analyses were also conducted without any specific phobia diagnoses. Findings were the same whether specific phobia diagnoses were included or omitted from the Parent Anxiety Disorders variable.
Because many parents had more than one diagnosis, frequency counts are not mutually exclusive.
Results of preliminary nested model comparisons conducted separately by adolescent gender are available upon request from the first author.
References
Leventhal T, Brooks-Gunn J (2000) The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull 126:309–337. doi:10.1037/0033-2909.126.2.309
Tuma JM (1989) Mental health services for children: the state of the art. Am Psychol 44:188–199. doi:10.1037/0003-066X.44.2.188
Day C, Roberts MC (1991) Activities of the child and adolescent service system program for improving mental health services for children and families. J Clin Child Psychol 20:340–350
Grant KE, O’Koon J, Davis T, Roache N, Poindexter L, Armstrong M, Minden JA, McIntosh JM (2000) Protective factors affecting low-income urban African American youth exposed to stress. J Early Adolesc 20:388–417. doi:10.1177/0272431600020004002
Tolan PH, Guerra NG, Montaini-Klovdahl L (1997) Staying out of harm’s way: coping and the development of inner-city children. In: Sandier I, Wolchik S (eds) Handbook of children’s coping with common stressors: Linking theory, research and interventions. Plenum, New York, pp 453–479
McLoyd VC (1998) Socioeconomic disadvantage and child development. Am Psychol 53:185–204. doi:10.1037/0003-066X.53.2.185
Tolan PH, Henry D (1996) Patterns of psychopathology among urban poor children: comorbidity and aggression effects. J Consult Clin Psychol 64:1094–1099. doi:10.1037/0022-006X.64.5.1094
Hawkes TH, Furst NF (1971) Race, socio-economic situation, achievement, IQ, and teacher ratings of students’ behavior as factors relating to anxiety in upper elementary school children. Sociol Educ 44:333–350. doi:10.2307/2111996
Nalven FB (1970) Manifest fears and worries of ghetto vs middle-class suburban children. Psychol Rep 27:285–286
Roberts RE, Roberts CR, Xing Y (2007) Rates of DSM-IV psychiatric disorders among adolescents in a large metropolitan area. J Psychiatr Res 41:959–967. doi:10.1016/j.jpsychires.2006.09.006
Centers for Disease Control and Prevention (1998) Suicide among black youths—United States, 1980–1995. Morb Mortal Wkly Rep 47:106–193
O’Donnell L, O’Donnell C, Wardlaw DM, Stueve A (2004) Risk and resiliency factors influencing suicidality among urban African American and Latino youth. Am J Community Psychol 33:37–49. doi:10.1023/B:AJCP.0000014317.20704.0b
Price JH, Dake JA, Kucharewski R (2001) Assets as predictors of suicide attempts in African American inner-city youths. Am J Health Behav 25:367–375
Griffin JA, Cicchetti D, Leaf PJ (1993) Characteristics of youths identified from a psychiatric case register as first-time users of services. Hosp Community Psychiatry 44:62–65
McMiller WP, Weisz JR (1996) Help-seeking preceding mental health clinic intake among African-American, Latino, and Caucasian youths. J Am Acad Child Adolesc Psychiatry 35:1086–1094. doi:10.1097/00004583-199608000-00020
Beardslee WR, Keller MB, Lavori PW, Staley JE (1993) The impact of parental affective disorder on depression in offspring: a longitudinal follow-up in a nonreferred sample. J Am Acad Child Adolesc Psychiatry 32:723–730
Chassin L, Rogosch F, Barrera M (1991) Substance use and symptomatology among adolescent children of alcoholics. J Abnorm Psychol 100:449–463. doi:10.1037/0021-843X.100.4.449
Merikangas KR, Dierker LC, Szatmari P (1998) Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: a high risk study. J Child Psychol Psychiatry 39:711–720. doi:10.1017/S0021963098002522
Turner SM, Beidel DC, Costello A (1987) Psychopathology in the offspring of anxiety disorders patients. J Consult Clin Psychol 55:229–235. doi:10.1037/0022-006X.55.2.229
Angold A, Weissman MM, John K, Merikangas KR (1987) Parent and child reports of depressive symptoms in children at low and high risk of depression. J Child Psychol Psychiatry 28:901–915. doi:10.1111/j.1469-7610.1987.tb00678.x
Garber J, Martin NC (2002) Negative cognitions in offspring of depressed parents: mechanisms of risk. 121-153. doi: 10.1037/10449-005
Weissman MM, Fendrich M, Warner V, Wickramaratne P (1992) Incidence of psychiatric disorder in offspring at high and low risk for depression. J Am Acad Child Adolesc Psychiatry 31:640–648. doi:10.1097/00004583-199207000-00010
Ginsburg GS, Schlossberg MC (2002) Family-based treatment of childhood anxiety disorders. Int Rev Psychiatr 14:143–154. doi:10.1080/09540260220132662
Kelley ML, Fals-Stewart W (2004) Psychiatric disorders of children living with drug-abusing, alcohol-abusing, and non-substance-abusing fathers. J Am Acad Child Adolesc Psychiatry 43:621–628. doi:10.1097/00004583-200405000-00016
Stanger C, Higgins ST, Bickel WK, Elk R, Grabowski J, Schmitz J, Amass L, Kirby KC, Seracini AM (1999) Behavioral and emotional problems among children of cocaine- and opiate dependent parents. J Am Acad Child Adolesc Psychiatry 38:421–428. doi:10.1097/00004583-199904000-00015
Cauce AM, Stewart A, Rodriguez MD, Cochran B, Ginzler J (2003) Overcoming the odds? Adolescent development in the context of urban poverty. In: Luthar SS (ed) Resilience and vulnerability: adaptation in the context of childhood adversities. Cambridge University Press, New York, pp 343–363
Merikangas KR (2002) Familial factors and substance use disorders. In: McMahon RJ, Peters RD (eds) The effects of parental dysfunction on children. Kluwer Academic/Plenum Publishers, New York, pp 17–40
Kessler RC, Chiu WT, Demler O, Walters EE (2005) Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 62:617–627. doi:10.1001/archpsyc.62.6.617
Kline RB (1998) Principles and practice of structural equation modeling. Guilford Press, New York
Biederman J, Petty C, Hirashfeld-Becker DR, Henin A, Faraone SV, Dang D, Jakubowski A, Rosenbaum JF (2006) A controlled longitudinal 5-year follow-up study of children at high and low risk for panic disorder and major depression. Psychol Med 36:1141–1152. doi:10.1017/S0033291706007781
Chassin L, Pitts SC, DeLucia C, Todd M (1999) A longitudinal study of children of alcoholics: predicting young adult substance use disorders, anxiety, and depression. J Abnorm Psychol 108:106–119. doi:10.1037/0021-843X.108.1.106
Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP (2004) The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United states, 1991–1992 and 2001–2002. Drug Alcohol Depend 74:223–234. doi:10.1016/j.drugalcdep.2004.02.004
Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ (1996) The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. Am J Orthopsychiatry 66:17–31. doi:10.1037/h0080151
Regier DA, Rae DS, Narrow WE, Kaelber CT, Schatzberg AF (1998) Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. Br J Psychiatry 173:24–28
Hasin DS, Stinson FS, Ogburn E, Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry 64:830–842. doi:10.1001/archpsyc.64.7.830
Bollen KA, Curran PJ (2006) Latent curve models: a structural equations perspective. Wiley, Hoboken, NJ, US
Biederman J, Rosenbaum JF, Bolduc EA, Faraone SV (1991) A high risk study of young children of parents with panic disorder and agoraphobia with and without comorbid major depression. Psychiatry Res 37:333–348. doi:10.1016/0165-1781(91)90068-Z
Beidel DC, Turner SM (1997) At risk for anxiety: I. psychopathology in the offspring of anxious parents. J Am Acad Child Adolesc Psychiatry 36:918–924. doi:10.1097/00004583-199707000-00013
Wichstrom L (1999) The emergence of gender difference in depressed mood during adolescence: the role of intensified gender socialization. Dev Psychol 35:232–245. doi:10.1037/0012-1649.35.1.232
van der Ende J, Verhulst FC (2005) Informant, gender and age differences in ratings of adolescent problem behaviour. Eur Child Adolesc Psychiatry 14:117–126. doi:10.1007/s00787-005-0438-y
Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ (2002) Depression scale scores in 8–17-year-olds: effects of age and gender. J Child Psychol Psychiatry 43:1052–1063. doi:10.1111/1469-7610.00232
Cole DA, Tram JM, Martin JM, Hoffman KB, Ruiz MD, Jacquez FM, Maschman (2002) Individual differences in the emergence of depressive symptoms in children and adolescents: a longitudinal investigation of parent and child reports. J Abnorm Psychol 111:156–165. doi:10.1037/0021-843X.111.1.156
Ge X, Lorenz FO, Conger RD, Elder GH, Simons RL (1994) Trajectories of stressful life events and depressive symptoms during adolescence. Dev Psychol 30:467–483. doi:10.1037/0012-1649.30.4.467
Ranta K, Kaltiala-Heino R, Koivisto A, Tuomisto MT, Pelkonen M, Marttunen M (2007) Age and gender differences in social anxiety symptoms during adolescence: the social phobia inventory (SPIN) as a measure. Psychiatry Res 153:261–270. doi:10.1016/j.psychres.2006.12.006
Hale WW III, Raaijmakers Q, Muris P, van Hoof A, Meeus W (2008) Developmental trajectories of adolescent anxiety disorder symptoms: a 5-year prospective community study. J Am Acad Child Adolesc Psychiatry 47:556–564. doi:10.1097/CHI.0b013e3181676583
Ollendick TH, King NJ (1994) Diagnosis, assessment, and treatment of internalizing problems in children: the role of longitudinal data. J Consult Clin Psychol 62:918–927. doi:10.1037/0022-006X.62.5.918
Hayward C, Wilson KA, Lagle K, Kraemer HC, Killen JD, Taylor CB (2008) The developmental psychopathology of social anxiety in adolescents. Depress Anxiety 25:200–206. doi:10.1002/da.20289
Lewinsohn PM, Gotlib IH, Lewinsohn M, Seeley JR, Allen NB (1998) Gender differences in anxiety disorders and anxiety symptoms in adolescents. J Abnorm Psychol 107:109–117. doi:10.1037/0021-843X.107.1.109
Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A (2003) Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 60:837–844. doi:10.1001/archpsyc.60.8.837
Repetto PB, Caldwell CH, Zimmerman MA (2004) Trajectories of depressive symptoms among high risk African-American adolescents. J Adolesc Health 35:468–477. doi:10.1016/j.jadohealth.2003.12.007
Clark DB, Smith MG, Neighbors BD, Skerlec LM (1994) Anxiety disorders in adolescence: characteristics, prevalence, and comorbidities. Clin Psychol Rev 14:113–137. doi:10.1016/0272-7358(94)90012-4
Twenge JM, Nolen-Hoeksema S (2002) Age, gender, race, socioeconomic status, and birth cohort difference on the children’s depression inventory: a meta-analysis. J Abnorm Psychol 111:578–588. doi:10.1037/0021-843X.111.4.578
Ialongo N, Poduska J, Werthamer L, Kellam S (2001) The distal impact of two first-grade preventive interventions on conduct problems and disorder in early adolescence. J Emot Behav Disord 9:146–160. doi:10.117/106342660100900301
Ialongo NS, Kellam SG, Poduska J (1999) Manual for the Baltimore how I feel. (Tech. Rep. No. 2). Johns Hopkins University, Baltimore, MD
American Psychiatric Association (1987) Diagnostic and statistical manual of mental disorders (3rd ed., revised). American Psychiatric Association, Washington, DC
World Health Organization (1994) Composite international diagnostic interview (CIDI) researcher’s manual version 1.1. American Psychiatric Association, Albany, New York
Wittchen H (1994) Reliability and validity studies of the WHO-composite international diagnostic interview (CIDI): a critical review. J Psychiatr Res 28:57–84. doi:10.1016/0022-3956(94)90036-1
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders (4th ed., text revision). American Psychiatric Association, Washington, DC
Peters L, Andrews G (1995) Procedural validity of the computerized version of the composite international diagnostic interview (CIDI-Auto) in the anxiety disorders. Psychol Med 25(6):1269–1280
Dobson KS (1985) The relationship between anxiety and depression. Clin Psychol Rev 5(4):307
Barbee JG (1998) Mixed symptoms and syndromes of anxiety and depression: diagnostic, prognostic, and etiologic issues. Ann Clin Psychiatry 10(1):15
Kovacs M (1983) The children’s depression inventory: a self-rating depression scale for schoolaged youngsters. Unpublished manuscript. University of Pittsburgh, Pittsburgh
Asarnow JR, Carlson GA (1985) Depression self-rating scale: utility with child psychiatric inpatients. J Consult Clin Psychol 53:491–499. doi:10.1037/0022-006X.53.4.491
Spence SH (1998) A measure of anxiety symptoms among children. Behav Res Ther 36(5):545–566
Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME (2000) NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry 39:28–38. doi:10.1097/00004583-200001000-00014
Muthén LK, Muthén BO (2007) Mplus user’s guide, 5th edn. Muthén & Muthén, Los Angeles, CA
Joreskog KG, Goldberger AS (1972) Factor analysis by generalized least squares. Psychometrika 37:243–260. doi:10.1007/BF02306782
Arbuckle JL, Wothke W (1999) AMOS 4.0 user’s guide. Small Waters Corporation, Chicago
Chen F, Curran PJ, Bollen KA, Kirby JB, Paxton P (2008) An empirical evaluation of the use of fixed cutoff points in RMSEA test statistic in structural equation models. Sociol Method Res 36:462–494. doi:10.1177/0049124108314720
Arbuckle JL (1996) Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE (eds) Advanced structural equation modeling: issues and techniques. Erlbaum, Mahwah, NJ, pp 237–277
Little RJ (1995) Modeling the dropout mechanism in repeated-measures studies. J Amer Statistical Assoc 90(431):1112–1121
Muthén BO, Sheddon K (1999) Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics 6:463–469
Schafer JL, Graham (2002) Missing data: our view of the state of the art. Psychol Methods 7:147–177. doi:10.1037/1082-989X.7.2.147
Wothke W (2000) Longitudinal and multigroup modeling with missing data. In: Little TD, Schnabel KU, Baumert J (eds) Modeling longitudinal and multilevel data: practical issues, applied approaches, and specific examples. Lawrence Erlbaum Associates, Mahwah, NJ, US, pp 219–240
Muthén LK, Muthén BO (2004) Mplus: the comprehensive modeling program for applied researchers. User’s guide, 3rd edn. Muthén & Muthén, Los Angeles, CA
West SG, Finch JF, Curran PJ (1995) Structural equation models with nonnormal variables: problems and remedies. 56–75
Windle M, Windle RC (2001) Depressive symptoms and cigarette smoking among middle adolescents: prospective associations and intrapersonal and interpersonal influences. J Consult Clin Psychol 69:215–226. doi:10.1037/0022-006X.69.2.215
Sigmon ST, Pells J, Boulard N, Whitcomb-Smith S, Edenfield T, Hermann B, Schartel, LaMattina, Kubik (2005) Gender differences in self-reports of depression: the response bias hypothesis revisited. Sex Roles 53:401–411. doi:10.1007/s11199-005-6762-3
Bosquet M, Egeland B (2006) The development and maintenance of anxiety symptoms from infancy through adolescence in a longitudinal sample. Dev Psychopathol 18:517–550. doi:10.1017/S0954579406060275
Bell-Dolan DJ, Last CG, Strauss CC (1990) Symptoms of anxiety disorders in normal children. J Am Acad Child Adolesc Psychiatry 29:759–765. doi:10.1097/00004583-199009000-00014
Ohannessian CM, Lerner RM, Lerner JV, von Eye A (1999) Does self-competence predict gender differences in adolescent depression and anxiety? J Adolesc 22:397–411. doi:10.1006/jado.1999.0231
Palapattu AG, Kingery JN, Ginsburg GS (2006) Gender role orientation and anxiety symptoms among African American adolescents. J Abnorm Child Psychol 34:441–449. doi:10.1007/s10802-006-9023-1
Kashani JH, Orvaschel H (1990) A community study of anxiety in children and adolescents. Am J Psychiatry 147:313–318
Weems CF, Costa NM (2005) Developmental differences in the expression of childhood anxiety symptoms and fears. J Am Acad Child Adolesc Psychiatry 44:656–663. doi:10.1097/01.chi.0000162583.25829.4b
Ollendick TH, Matson JL, Helsel WJ (1985) Fears in children and adolescents: normative data. Behav Res Ther 23:465–467. doi:10.1016/0005-7967(85)90174-3
Ollendick TH, King NJ, Frary RB (1989) Fears in children and adolescents: reliability and generalizability across gender, age and nationality. Behav Res Ther 27:19–26. doi:10.1016/0005-7967(89)90115-0
Dierker LC, Merikangas KR, Szatmari P (1999) Influence of parental concordance for psychiatric disorders on psychopathology in offspring. J Am Acad Child Adolesc Psychiatry 38:280–288. doi:10.1097/00004583-199903000-00016
Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC (2005) Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med 35:317–327. doi:10.1017/S0033291704003514
Sterba SK, Prinstein MJ, Cox MJ (2007) Trajectories of internalizing problems across childhood: heterogeneity, external validity, and gender differences. Dev Psychopathol 19:345–366. doi:10.1017/S0954579407070174
Hill JP, Holmbeck G (1986) Attachment and autonomy during adolescence. In: White-hurst g (ed) Annals of child development, vol 3. JAI, Greenwich, CT, pp 145–189
Cross SE, Madson L (1997) Models of the self: self-construals and gender. Psychol Bull 122:5–37. doi:10.1037/0033-2909.122.1.5
Block CB (1981) Black American and the cross-cultural counseling and psychotherapy experience. In: Marsella AJ, Pederson PB (eds) Cross cultural counseling and psychotherapy. Pergamon, New York, pp 177–194
Kellam SG, Werthamer-Larsson L, Dolan LJ, Brown CH, Mayer LS, Rebok GW et al (1991) Developmental epidemiologically based preventive trials: baseline modeling of early target behaviors and depressive symptoms. Am J Community Psychol 19:563–584. doi:10.1007/BF00937992
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H, Kendler KS (1994) Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the national comorbidity survey. Arch Gen Psychiatry 51(1):8–19
Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC (1996) Agoraphobia, simple phobia, and social phobia in the national comorbidity survey. Arch Gen Psychiatry 53:159–168
Kessler RC, Rubinow DR, Holmes C, Abelson JM, Zhao S (1997) The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychol Med 27:1079–1089. doi:10.1017/S0033291797005333
Warner LA, Kessler RC, Hughes M, Anthony JC (1995) Prevalence and correlates of drug use and dependence in the United States: results from the national comorbidity survey. Arch Gen Psychiatry 52:219–229
McMahon RJ, Peters RD (eds) (2002) The effects of parental dysfunction on children. Kluwer Academic/Plenum Publishers, New York, NY, US
Chambless DL, Williams KE (1995) A preliminary study of African Americans with agoraphobia: symptom severity and outcome of treatment with in vivo exposure. Behav Ther 26:501–515
Miranda J, Chung G, Krupnick S, Revicki B (2003) Treating depression in predominantly low-income young minority women: a randomized controlled trial. JAMA 290:57–65. doi:10.1001/jama.290.1.57
Miranda J, Schoenbaum M, Sherbourne C, Duan N, Wells K (2004) Effects of primary care depression treatment on minority patients’ clinical status and employment. Arch Gen Psychiatry 61:827–834. doi:10.1001/archpsyc.61.8.827
Barrish HH, Saunders M, Wolf MD (1969) Good behavior game: effects of individual contingencies for group consequences on disruptive behavior in a classroom. J Appl Behav Anal 2:119–124. doi:10.1901/jaba.1969.2-119
Canter L, Canter M (1991) Parents on your side: a comprehensive parent involvement program for teachers. Lee Canter, Santa Monica, CA
Handel R, Goldsmith E (1990) Family-reading a home school partnership. Montclair State College, Montclair, NJ
Karweit N, Bond MA (1998) Manual for the story telling and retelling program. Center for Research on Elementary and Middle Schools, The Johns Hopkins University, Baltimore
Webster-Stratton C (1984) Randomized trial of two parent-training programs for families with conduct-disordered children. J Consult Clin Psychol 52:666–678. doi:10.1037/0022-006X.52.4.666
Acknowledgments
This research was supported by National Institute of Mental Health grants T32MH020033, K23MH63427-02, P30MH066247, R01MH057005 and National Institute of Drug Abuse grant R01DA011796. We gratefully acknowledge the generous assistance of Ms. Emily M. Becker for her help preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burstein, M., Ginsburg, G.S., Petras, H. et al. Parent Psychopathology and Youth Internalizing Symptoms in an Urban Community: A Latent Growth Model Analysis. Child Psychiatry Hum Dev 41, 61–87 (2010). https://doi.org/10.1007/s10578-009-0152-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-009-0152-y